Abstract
Various internal and external factors negatively affect the homeostatic equilibrium of organisms at the molecular to the whole-body level, inducing the so-called state of stress. Stress affects an organism's welfare status and induces energy-consuming mechanisms to combat the subsequent ill effects; thus, the individual may be immunocompromised, making them vulnerable to pathogens. The information presented here has been extensively reviewed, compiled, and analyzed from authenticated published resources available on Medline, PubMed, PubMed Central, Science Direct, and other scientific databases. Stress levels can be monitored by the quantitative and qualitative measurement of biomarkers. Potential markers of stress include thermal stress markers, such as heat shock proteins (HSPs), innate immune markers, such as Acute Phase Proteins (APPs), oxidative stress markers, and chemical secretions in the saliva and urine. In addition, stress biomarkers also play critical roles in the prognosis of stress-related diseases and disorders, and therapy guidance. Moreover, different components have been identified as potent mediators of cardiovascular, central nervous system, hepatic, and nephrological disorders, which can also be employed to evaluate these conditions precisely, but with stringent validation and specificity. Considerable scientific advances have been made in the detection, quantitation, and application of these biomarkers. The present review describes the current progress of identifying biomarkers, their prognostic, and therapeutic values.
Keywords: biomarkers, stress, diagnosis, prognosis, therapeutic values, acute phase proteins, heat shock proteins, miRNAs
Introduction
Conceptually, stress has been considered to have a negative connotation in the available literature. However, stress is an inevitable response in all mammals to maintain their homeostasis. Both human and animal health and animal production are hampered severely by different stresses (Martin et al., 2011; Takahashi A. et al., 2018. Strategies to counteract stress in humans and animals often rely on the early detection of stress-induced damage. Various indicators have been identified as potent markers of different biological processes, such as pathogenic or pharmacological responses, and are designated as biomarkers (Griffiths and Moller, 2002; Dadar et al., 2016; Abbas et al., 2017; Prajapati et al., 2017; Selleck et al., 2017; Ewert and Chang, 2018; Tampa et al., 2018). These include normal physiological biomarkers that are within the normal range in healthy subjects. However, a stress marker indicates that an individual is not in physiological comfort and different energy consuming mechanisms are operating inside their bodies to maintain the homeostasis (McEwen, 2015; Marco-Ramell et al., 2016), with the involvement of numerous biomarkers. Hence, a biomarker is a characteristic that can be objectively measured and evaluated as an indicator of a physiological as well as a pathological process or pharmacological response to a therapeutic intervention (Naylor, 2003). According to FDA, an ideal biomarker could be specific for a particular disease and should be able to differentiate between different physiological states, safe and easy to measure, rapid so as to enable faster diagnosis as well as able to give accurate results and consistent between different ethnic groups and genders (Jain, 2010; Sahu et al., 2011). Biomarkers help not only in disease diagnosis but also in tracking progression, regression, and outcome after the intervention. They should be quantified either in the body fluid or externally. Physiological parameters, such as the respiration rate, pulse rate, and core body temperature, are the best-observed markers depicting environmental, social, and psychological stresses (Carboni, 2013). Classical stress markers comprise endocrine changes, especially in the levels of hormones, such as cortisol and epinephrine (Martin et al., 2011; Ewert and Chang, 2018; Takahashi A. et al., 2018). It is the hypothalamic-pituitary-adrenal axis, along with autonomic nervous system, and the immune system that gets sensitized and responds immediately to the peripheral stresses through the commonly known stress biomarkers, such as cortisol, alpha-amylase, pro-inflammatory cytokines (Nater et al., 2013; Ewert and Chang, 2018; Takahashi A. et al., 2018). Deciphering the interaction of different immune cytokines with neuronal circuits of stress is critical to delineate the physiological and psychological stress responses and the prognosis of illness (Godoy et al., 2018). It is proved, experimentally, that hyperthermia and early life stresses in the murine model resulted in deregulation of hypothalamic-pituitary-adrenal (HPA) axis, skewing of hippocampal glucocorticoid receptor mRNA expression and defective neurogenesis indicated by the immature neuron marker doublecortin in an age-dependent manner (Umeoka et al., 2019). Advances in proteomic research have come up with various potential proteins as a panel of biomarkers for diagnosis and therapy related to immunity, blood coagulation, management of oxidative stress, energy metabolism, etc. (Silva-Costa et al., 2019).
From the stress induced physiological and endocrine alterations, disturbances in corresponding functional (e.g., clinical parameters), biochemical (e.g., hormones), metabolic systems become inevitable and hence alterations in metabolic biomarkers (metabolites, enzymes, hormones) also result (Fortunato et al., 2018; Hefnawy et al., 2018). This cascade influences other vital early responding (e.g., cardiovascular, CNS, renal) and late responding (e.g., hepato-biliary, pancreatic) systems. Thus, results in multisystem involvement and hence widespread disturbance in a range of biomarkers peculiar to each system or organ thereof (O'Brien et al., 2017; De Rosa et al., 2018; McGarrah et al., 2018; Nadkarni et al., 2019). The biomarkers concerning cardio-vascular-metabolic function and health include those of vascular function (FMD, BP, AIX), vasculature (cholesterol, HDL, LDL, SAA, sICAM, sVCAM), vascular cytokines (fasting), homocysteine, magnesium (urine), cardiac [(troponins, C-reactive protein, myeloperoxidase (MPO), natriuretic peptides] (Chacko et al., 2017; Dookhun et al., 2018) and corresponding metabolic parameters [(total, HDL, LDL cholesterol (fasting), TG (fasting), glucose, insulin (fasting), HbA1c)]. Similarly, biomarkers for health and function of liver (ketone bodies, central metabolism, ALAT, ASAT, ALP, GGT, CRP, TG, liver IR index, liver IS index), pancreas (disposition index, C-peptide, insulin, glucagon, HOMA-B), kidney (creatinine, Asp, Glu, Orn, urea, albumin), adipose tissue (glycerol, NEFA, and specific FFA, MG, DG, leptin, adiponectin, estimated SCD activity, C16:1 FFA, adipose IR index), gut (fructose, ribulose/xylulose, GIP, GLP-1, indole-3-proprionic acid), brain (secondary messengers, Trp, Tyr, Phe, Met), and muscle (lactate, beta-alanine, muscle IR index, branched chain amino acids and derivatives, 1-methylhistidine, 3-methylhistidine, 4-hydroxyproline, 4-oxoproline) have been enumerated (Chacko et al., 2017; Wopereis et al., 2017; Dookhun et al., 2018; Ho et al., 2018; Karwi et al., 2018; Kyle et al., 2018; Marcato et al., 2018; Pleil et al., 2018). Though these biomarkers constitute the routine health or function(s) detecting biomarkers of these systems, however the persistent alteration under a constant stimulus or etiology results in a disturbance in physio-biological-metabolic homeostatic mechanisms. This causes alteration in endpoint products or by-products of each physiological or metabolic process. Indirectly, the accumulation of these products causes a disturbance in the natural balance of systems and directly persistent stimulus, or etiology can influence normal health and functioning of vital organs (cardiovascular, CNS). All these events starting from disturbance to physiological, endocrine, multiorgan-metabolic to homeostatic mechanisms lead to a state of stress. This initiates a new series of reaction cascade involving oxidative, inflammatory and genomic and proteomic reactions giving origin to particular biomarkers of stress (Dhawan et al., 2014; Alicka and Marycz, 2018; Böbel et al., 2018; Fioranelli et al., 2018; Gómez-Serrano et al., 2018; Ho et al., 2018; Messina et al., 2018; van der Reest et al., 2018; Whongsiri et al., 2018).
These stress-induced reactions are so interlinked that generation of one species (e.g., oxidants, pro-inflammatory cytokines) influences the formation of others (e.g., anti-oxidants, anti-inflammatory cytokines). This, in turn, affects the levels of reactive oxygen species (ROS), and inflammatory mediators (Alicka and Marycz, 2018; Pickering et al., 2018; Saban et al., 2018; Sharma et al., 2018; Yatoo et al., 2019a). This interwoven homeostatic mechanism disturbance results alteration of protective defense mechanisms and result the stress of varying degrees and types. This further aggravates responsive cascade, activating genomic, and proteomic response expressing genes translating to proteins of interest. These all metabolomic, oxidative, inflammatory, genomic or proteomic alterations ultimately serve as biomarkers of stress (Alicka and Marycz, 2018; Nallagangula et al., 2018; Pickering et al., 2018; Sharma et al., 2018; van der Reest et al., 2018; Whongsiri et al., 2018).
Among various forms of stresses, endogenously oxidative and inflammatory stresses are the main generators of various biomarkers that correspond to alteration in different cellular systems they represent (Pickering et al., 2018; Virzì et al., 2018; Gabriela et al., 2019; Yatoo et al., 2019b). There exists a narrow margin of oxygen balance at the cellular level between the production of ROS and the effects of anti-oxidants. During different types of stress, powerful anti-oxidants in mammalian cells, such as glutathione peroxidase and catalase, scavenge these ROS and free radicals (Rahal et al., 2014). Highly reactive unpaired electrons present in ROS and free radicals are unleashed during oxidative stress and can be used as biomarkers at the cellular level (Ho et al., 2013). These free radicals stimulate an array of inflammatory reactions, generating numerous inflammatory mediators that also serve as stress biomarkers (Saban et al., 2018; Sharma et al., 2018; Yatoo et al., 2019b). Immunological stimulation of body defense systems by these alterations or the resulted products further extends the responsive cascade to molecular events including gene expression or protein translation (Yatoo et al., 2018, 2019b). In addition, various proteins get expressed under varying stresses and can be evaluated as biomarkers, e.g., heat shock proteins (HSPs), which are the molecular chaperonins that protect cells from misfolding of denatured proteins during heat-induced stress (Mori et al., 2016) or diseases (Lechner et al., 2018; Tang T. et al., 2018), may also represent useful biomarkers.
Along with the identification of potent biomarkers, the criteria for ideal markers recommend the provision of non-invasive biological samples, such as easily accessible external body secretions. Studies in the past few decades have identified biomarkers that have the potential to revolutionize medical science in terms of diagnosis, prognosis, and therapy (Chowdhury et al., 2013; Selleck et al., 2017; Cesano and Warren, 2018). Biomarkers have been identified for various diseases and disorders; for example, metabolic disorders (Boenzi and Diodato, 2018), cardiovascular disease (Ho et al., 2018), myocardial infarctions (Ge et al., 2018), gynecological diseases (Flores et al., 2018; Liu et al., 2018), neurological disorders (Lashley et al., 2018) and hepatic diseases (Wallace et al., 2016; Raghu et al., 2018). In the present era of high cancer prevalence, sensitive neoplastic biomarkers are a significant research focus, which could aid the early detection and prognosis of neoplastic changes (Tainsky, 2009; Admoni-Elisha et al., 2016; Andersen et al., 2017; Liu et al., 2018). In addition to conventional biomarkers, advances in molecular medicine have identified cell-free nucleic acids, including DNA, mRNA, and microRNAs (miRNAs) as potential markers for several diseases (Lo et al., 2007; Swarup and Rajeswari, 2007; Gilad et al., 2008; Shen et al., 2016; Hibner et al., 2018; Lin et al., 2018). There is an increasing demand for the evaluation of stress to reflect physiological well-being, nutritional status, disease progression, and the immune compromised state. Further, biomarkers can be of diagnostic, prognostic, or therapeutic value (FDA-NIH Biomarker Working Group, 2016). Diagnostic biomarkers help in diagnosing the stress and/or related disease when the prognostic biomarkers are being explored for studying progression or outcome of this stress-disease cascade and predict the likelihood of occurrence of disease. Similarly, therapeutic biomarkers help in monitoring the effect of therapy on stress or disease (Carlomagno et al., 2017; Verber et al., 2019).
Some biomarkers determine the extent of damage and serve as indicators of degradation by stress or disease, such as MDA, isoprostanes, while others, such as anti-oxidant markers reflect a status of body's defense mechanism against stress-induced alterations. Among them, some have dual nature of being both body's normal excretory or metabolic products and anti-oxidant defense, e.g., urates. Some hormones are the normal mediators of the stress process, such as cortisol and adrenaline, while as copeptin or chromogranin A (CgA) prohormones can indirectly determine renal, cardiovascular, or neuroendocrine dysfunction. Enzymes, such as alpha-amylase and lysozyme also serve as biomarkers of stress. Some proteins, such as secretory IgA and heat shock proteins (HSPs) serve as indicators of immunity or resistance mechanism to stress, while as acute phase proteins reflect body response to invading agents. So a broad range of areas concerning these biomarkers needs to be discussed.
Therefore, the present review focuses on the current progress of identifying biomarkers for different stresses in humans and animals, and their prognostic and therapeutic values in stress-mediated diseases and disorders, as well as discussing their futuristic perspectives. It has scope for identification of novel biomarkers with ease of evaluation and accuracy of determination, role in stress and disease, prediction, progression, and monitoring amelioration. The markers discussed include malondialdehyde (lipid peroxidation marker), isoprostanes, enzymatic anti-oxidants, blood urates, cortisol, copeptin, alpha-amylase, secretory IgA, chromogranin A (CgA), lysozyme, microRNAs (miRNAs), heat shock proteins (HSPs), and acute phase proteins. Their utility has been elaborated in various stresses, and related diseases and disorders (Vaishya et al., 2018; van't Erve, 2018; Pulvirenti et al., 2019).
Types of Biomarkers
Though biomarkers have been classified on various basis including characteristics, application, genetics and molecular biology methods, however biomarkers can be of dual nature or roles and fitting in diverse classifications. As per characteristics, they can be imaging biomarkers or non-imaging biomarkers (Huss, 2015). Imaging biomarkers are applied in identifying or visualizing a lesion or a disease as in computed tomography, positron emission tomography, or magnetic resonance imaging. Non-imaging biomarkers also considered as molecular biomarkers are biochemical type of biomarkers having biophysical properties, hence can be measured in biological samples. They include cellular structures or biophysical components, such as nucleic acid-based biomarkers including gene mutations or polymorphisms and quantitative gene expression analysis, peptides, proteins, lipids metabolites, and other small molecules.
According to the application, they can be classified as diagnostic, prognostic, and therapeutic biomarkers (Drucker and Krapfenbauer, 2013; Huss, 2015). Diagnostic biomarkers are those that help in disease diagnosis or determination. Prognostic biomarkers help in forecasting or likely prediction of disease outcome. Therapeutic biomarkers help in monitoring treatment progress of the disease.
According to genetics and molecular biology methods (Sahu et al., 2011), biomarkers can be categorized into three types, i.e., (1) Type 0, (2) Type 1, and (3) Type 2. Type 0 biomarkers are natural history biomarkers and help in measuring the natural history of the disease and correlate over time with known clinical indicators. Type 1 biomarkers are drug activity biomarkers and indicate the effect of drug intervention. They include efficacy biomarkers which indicate therapeutic effects of a drug, mechanism biomarkers which give information about the mechanism of action of a drug, and toxicity biomarkers that indicate the toxicological effects of a drug. Type 2 biomarkers are the surrogate markers and serve as a substitute for a clinical outcome of a disease. Type 2 also helps to predict the effect of a therapeutic intervention (Jain, 2010).
Another classification, as per Drucker and Krapfenbauer (2013), divides biomarkers into prognostic biomarkers that help in fore-knowing or foreseeing of disease and can tell likely outcome of a disease in an untreated individual. Predictive biomarkers are used to identify patients that can positively respond to a given treatment. Pharmacodynamic biomarkers help in determining the pharmacological effects of a drug. Surrogate endpoint biomarkers have been discussed previously.
As per Mayeux (2004) biomarkers are divided into biomarkers of exposure or antecedent biomarkers that are used in risk prediction and biomarkers of disease that are used in the diagnosis and tracking the progress of a disease.
Despite such classifications, biomarkers have their relevance to each stress mechanism or disease or the organ or system involved. Hence, the description of individual biomarker(s) can be useful in elucidating diagnostic, pathophysiological, and clinical significance.
Oxidative Stress as Biomarkers
Homeostasis is achieved by the timely maintenance of interactions among the various organ systems, as well as the balance between metabolic processes, their products, and by-products. Various chemical and biological processes elicited within active tissues and cells release oxidative by-products, such as ROS, which include hydrogen peroxides, superoxide anions, reactive chloride ions, and reactive nitrogen species (RNS), such as nitric oxide (Puppel et al., 2015). Normally, cells have several anti-oxidants to counter the damaging effects of oxidative chemicals, and a healthy biological balance should be maintained between ROS and anti-oxidants to prevent oxidative destruction of cells and tissues. Any oxidative imbalance resulting in the accumulation of oxidants will inflict oxidative damage on cells, such as alteration of cellular macromolecules, lethal changes in genetic materials, such as DNA and RNA, an increase in the rate of cell death by programmed- and non-programmed-cell death (apoptosis/pyroptosis/necroptosis/ferroptosis or necrosis), and structural damage to tissues and organs (Sordillo and Aitken, 2009). Accumulation of oxidants can also induce lipid peroxidation and disturbances in physiological adaptation and cellular signaling pathways; which, together, inflict oxidative stress (Yoshikawa and Naito, 2002; Puppel et al., 2015). Recent studies have come up with assessing the levels of and functional interactions between various reactive species interactome (RSI), such as ROS, RNS, etc. in arterial and venous circulation during metabolic and environmental stress. Such redox metabolic approaches were revealed with dynamic pattern of responses and variation in arterio-venous concentration of these metabolic signatures (Cumpstey et al., 2019).
Although oxidants are accumulated in the body primarily endogenously, especially via cellular respiration and the electron transport chain, their levels can be augmented from exogenous sources. The major exogenous sources of oxidative attack include radiation (both ionizing and non-ionizing), atmospheric pollutants, biological and chemical toxins, toxic gasses, such as ozone, and oxidizing disinfectants (Eaton, 2006). In addition, foreign microbes invading the body and ingested foods with low nutrient value can lead to the production of tissue/cell-damaging oxidants by disturbing immune responses (Chen et al., 2000; Lykkesfeldt and Svendsen, 2007; Ho et al., 2013). Metabolic disturbances also cause the generation of free radicals (Alicka and Marycz, 2018; Messina et al., 2018). Moreover, strongly indicated oxidative stress biomarkers out of protein oxidation, such as advanced oxidation protein products (AOPP) are also linked with polymorphonuclear neutrophil proliferation and function. This interaction points to the involvement of oxidative stress associated formation of carbonyls and dityrosine residues in uterine inflammations leading to low fertility (Gabai et al., 2019).
Oxidative stress mediated by reactive oxygen and nitrogen species affects vital physiology directly and at the same time, exerts a priming role in the progression of several degenerative conditions and disorders, including cancers, immune disorders, and cardiovascular changes (Lykkesfeldt and Svendsen, 2007; Sordillo and Aitken, 2009; Rahal et al., 2014). Several studies have noted the negative effects of oxidative stress on various pathological processes in animals, including pneumonia and bacterial sepsis in pigs, recurrent airway obstruction in horses, and parturition and lactation induced metabolic disorders in cattle (Basu and Eriksson, 2001; Deaton et al., 2004, 2005; Lauritzen et al., 2005; Castillo et al., 2006). Worldwide, studies in humans and animals indicate the relevance of the timely identification of oxidative stress to ensure the optimum production and health of individuals. Several biomarkers have been identified as cellular oxidative stress indicators in animals. These include the plasma and serum levels of malondialdehyde (MDA), isoprostanes, glutathione (GSH) (L-γ-glutamyl-L-cysteinylglycine), and ROS reduction catalyzing enzymes, such as superoxide dismutase, catalase, glutathione peroxidase, and thioredoxin reductase (Marchitti et al., 2008; Ho et al., 2013; Yatoo et al., 2019b). Both ROS and oxidative stress are very well-related to each other. Imbalances in ROS homeostasis, caused by impairments in anti-oxidant enzymes or non-enzymatic anti-oxidant networks, lead to an increase in oxidative stress. This further causes deleterious oxidation and chemical modification of biomacromolecules, such as lipids, DNA, and proteins. While many ROS are intracellular signaling messengers and most products of oxidative metabolisms are beneficial for normal cellular function, the elevation of ROS levels by light, hyperglycemia, peroxisomes, and certain enzymes causes oxidative stress-sensitive signaling, toxicity, oncogenesis, neurodegenerative diseases, and diabetes (Umeno et al., 2017; Yatoo et al., 2019a). Moreover, reactive oxygen and nitrogen radicals, which are the mediators of oxidative and nitrative stresses, respectively, are being directly linked to systemic metabolic disease, such as diabetes mellitus (Rani and Mythili, 2014; Srinivasan et al., 2018) and associated complications, such as arteriolar sclerosis and nodular glomerulosclerosis, cerebrovascular disease, and amyloid deposition in the pancreas and kidney (Johar and Bernstein, 2017). Hence they have clinical relevance also.
Enzymatic anti-oxidants mediate their beneficial effects via the selenocysteine residues in their active sites and have been studied extensively in humans and livestock, particularly in dairy cattle. In addition to anti-oxidant enzymes, non-enzymatic anti-oxidants, such as tocopherols, ascorbic acid, lipoic acid, and carotenoids, also exist, especially in the biological membranes, with vitamin E and α-tocopherols being predominant (Halliwell, 2007). Among the various cellular and tissue systems, red blood cells (RBCs) are uniquely vulnerable to oxidative stress due to the lack of nucleus and mitochondria, inability to synthesize fresh protein along with degradation of detoxifying enzymes, etc. So they are among the first cells to be affected by alterations in the redox status of the body and can be explored for the early detection of pathophysiological alterations of the body in early stages (Pandey and Rizvi, 2011).
Currently, methods are available to evaluate the total anti-oxidant status in animals instead of the individual assessment of each oxidative stress marker. Hence, evaluation of the total anti-oxidant status (TAS) provides critical information concerning the in vivo dynamic equilibrium between pro-oxidative and anti-oxidative molecules (Lykkesfeldt and Svendsen, 2007; Ziech et al., 2010; Rani and Mythili, 2014; Yatoo et al., 2019b).
Oxidative stress has been associated with many obesity-related conditions among children, such as cardiovascular disease (Sharma et al., 2018), diabetes mellitus (Pickering et al., 2018), and hypertension (Small et al., 2018). Most of the oxidative stress markers are associated with blood metabolites, such as LDL, cholesterol and other critical biochemical parameters, indicating their crucial influence in lifestyle diseases (Praticò et al., 2004; Patrono et al., 2005; Alicka and Marycz, 2018; Sharma et al., 2018). A prostaglandin-F2α isomer, 8-isoprostane (8-ISO), is created in vivo by free radical-catalyzed peroxidation of arachidonic acid. In patients with chronic obstructive pulmonary disease (COPD) and healthy smokers, exhaled 8-ISO is known as an in vivo biomarker of lung oxidative stress (Montuschi et al., 2000; Van't Erve et al., 2016). For example, elevated oxidative stress, as indicated by increased 8-ISO levels produced via estrogen-related mechanisms, could induce a condition of persistent platelet activation, which promotes the growth and progression of breast cancer through the release of bioactive stored molecules, ultimately contributing to tumor invasiveness (Ferroni et al., 2017). By contrast, in a birth cohort residing in an agricultural area of California, changes in the levels of urinary 8-ISO were associated positively with maternal prenatal urinary levels of phthalate metabolites for 258 participating children at 5, 9, and 14 years of age (Tran et al., 2017).
Protein carbonyl groups are reported as biomarkers of protein oxidation (Dalle-Donne et al., 2003). High levels of protein carbonyl (>C=O) groups have been observed in some diseases, including Alzheimer's disease (AD), rheumatoid arthritis, diabetes, sepsis, chronic renal failure, and respiratory distress syndrome (Pullaiah et al., 2018). In microbial infections (e.g., leptospirosis), induced oxidative stress like the protein carbonyls are of diagnostic value (Fernando et al., 2016). Also, it was reported that urinary 8-hydroxy-2-deoxyguanosine (8-OHdG), an oxidized nucleoside of DNA, is a DNA oxidative stress biomarker and a risk factor for cancer, atherosclerosis, and diabetes (Wu et al., 2004; Kawai et al., 2018). In diabetic patients with hyperglycemia, increased urinary 8-OHdG and leukocyte DNA has been reported, and the urinary 8-OHdG level in diabetes patients has been linked with the severity of diabetic nephropathy and retinopathy (Zhang G. et al., 2018; Zhang L. et al., 2018; Zhang X. G. et al., 2018). Various methods, including high-performance liquid chromatography (HPLC), with and without extraction, and enzyme-linked immunosorbent assays (ELISAs), are proposed to determine 8-OHdG in tissues and urine (Wu et al., 2004; Kawai et al., 2018). Recently, the nanotechnology-based method has been used for determination of 8-OHdG as a biomarker of oxidative stress (Manavalan et al., 2018). Contrastingly, exposure to carcinogens correlates with DNA oxidative damage and most associations of exposures are with urinary 8-OHdG (Franken et al., 2017). Furthermore, 8-OHdG and nuclear factor-kappa B (NF-κB) immunopositivity was reported in brain tissues of rainbow trout exposed to linuron, a herbicide used widely to control grasses and annual broadleaf weeds (Topal et al., 2017). Expression of oxidative stress biomarkers, namely hexanoyl-lysine (HEL), can be used for measurement of lipid peroxidation and 8-OHdG for measurement of DNA oxidation. These biomarkers can also be identified in human tears (Haworth and Chandler, 2017). Oxidation products of linoleic acid, such as hydroperoxides and hydroxides that constitutes hydroxyoctadecadienoic acid (HODE) in biological fluids and tissue samples are the potent lipid peroxidation biomarkers, and their levels will be much higher in conditions like lifestyle-related diseases, such as diabetes and others (Yoshida et al., 2015).
In oxidative stress, a potent biomarker is oxidized low-density lipoprotein (oxLDL) which is measured in relation to certain disease conditions including atherosclerosis (Stocker and Keaney, 2004; Itabe et al., 2018). Plasma is the most common source for measuring oxLDL. Monoclonal antibodies, i.e., 4E6, DLH3, and E06, are the most frequently used to isolate the oxLDL biomarker immunologically. The 4E6 antibody binds to lysine residues on LDL whereas DLH3 as well as E06 recognizes phosphatidylcholine. It is important to note that oxLDL level is high in plasma in patients suffering from cardiovascular diseases or in patients having increased resistance to insulin, diabetes or obesity (Frijhoff et al., 2015; Trpkovic et al., 2015).
Thiobarbituric acid-reactive substances (TBARS) is another biomarker, the level of which can be measured in plasma as well as sera and blood cells, such as RBCs and leukocytes (Cristalli et al., 2012; Moretti et al., 2018) or tissue samples (Yatoo et al., 2016; Moretti et al., 2018). With the help of meta-analysis, the levels of TBARS in Alzheimer's disease (AD) as well as cognitive impairment (mild) have been measured and found to be high in the sera of the patients suffering from AD (Schrag et al., 2013).
Sports sessions produce oxidative stress, and recent studies have found that an increase in ALT level can be employed as a biomarker for athletes to measure the stress level (Mello et al., 2017). Multiple candidate biomarkers for exercise, such as oxidative stress along with brain-derived neurotrophic factor are the main promising components for assessing the anti-depressant effect of exercise, rendering promising adjunct treatment for mood disorders (Gu et al., 2016; Hearing et al., 2016). Oxidative damage of placenta in early gestation can contribute to the progression of pregnancy-associated complications, such as pre-eclampsia, gestational-diabetes mellitus, preterm birth, and intrauterine growth restriction in the later stage of pregnancy. Based on this fact, few of the biomarkers, such as peroxilipids, malondialdehyde, etc. have been suggested to aid in disease diagnosis during early stages in gestation (Cuffe et al., 2017).
Furthermore, decreased concentrations of bilirubin, a significant anti-oxidant, reveal an increase in oxidative stress and have been proposed as a stress biomarker in some epidemiological studies (Vaishnav et al., 2015; Estrada et al., 2016). Similarly, other non-enzymatic natural antioxidants, such as ascorbic acid (vitamin C), alpha tocopherol (vitamin E), glutathione, and uric acid (Bartoli et al., 2018) have been evaluated as oxidative markers (Kawamura and Muraoka, 2018). Another study revealed that hydroxylated polybrominated diphenyl ethers (PBDEs) and their possible metabolites promote oxidative stress in cellular studies (Costa et al., 2014; Yuan et al., 2017). Also, other in vivo and in vitro studies demonstrated that some PBDEs could induce oxidative stress and inflammation (Fernie et al., 2005; He et al., 2008; Costa et al., 2014). N-3 polyunsaturated fatty acids (PUFAs) can alleviate oxidative stress, as measured by the ratios of late-stage lipid peroxidation markers [malondialdehyde (MDA), 4-hydroxy-2-nonenal (4-HNE), and 8-ISO] to an early-stage marker, lipid hydroperoxide (LPH), which is common in coronary artery disease, and might contribute to depressive symptoms (Mazereeuw et al., 2017). The role of oxidative stress markers in the pathophysiology of asthma has been recognized and reported by Aldakheel et al. (2016), revealing that an elevated level of exhaled hydrogen ions, nitric oxide products, hydrogen peroxide, and 8-isoprostanes in the exhaled breath condensate (EBC) can be reliable markers for asthma and lower airway functions.
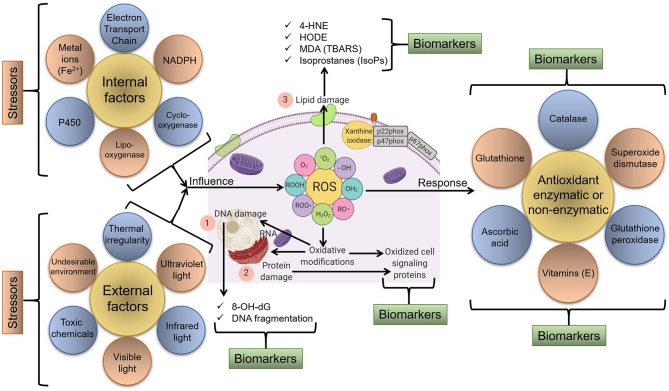
Figure 1 illustrates a schematic representation of various factors that can act as stressors and lead to the generation of ROS and oxidative stress/modifications that can be tracked as biomarkers of oxidative stress.
Figure 1.
Schematic representation of various endogenous and exogenous factors that act as stressors and lead to the generation of ROS and oxidative stress/modification. In response, various molecular and cellular redox-sensitive processes start that can be tracked as biomarkers of oxidative stress. For instance, major biomarkers include (1) markers of DNA/RNA damage/oxidation, (2) markers of protein damage/oxidation, and (3) markers of lipid damage via the oxidation of membrane components and available lipids, etc.
Oxidative stress can be physiological to maintain biological processes or pathological to facilitate disease process or stress response (Tan et al., 2018). In either case, alteration in biomarkers can reflect the severity of deviation from normality or degree of damage. A total change in oxidative or anti-oxidative markers through a reliable indicator of alteration but the individual interpretation of each oxidative stress marker will be more accurate for diagnosis and beneficial for understanding the overall process.
Malondialdehyde (MDA)
One of the most important and extensively studied oxidants is MDA. It is the aldehyde by-product derived from intracellular lipid peroxidation through the action of ROS upon PUFAs. MDA has a longer half-life than ROS; therefore, it can diffuse out to act on both intracellular and extracellular targets, exacerbating oxidative stress in animals (Marchitti et al., 2008; Sordillo and Aitken, 2009; Singh et al., 2013). MDA, along with another aldehyde by-product of lipid peroxidation, trans-4-hydroxy-2-nonenal (HNE), can be detrimental to homeostasis by disturbing the synthesis of essential biomolecules, such as nucleotides and proteins (Barrera et al., 2018). MDA and HNE accelerate the depletion of glutathione, increase proinflammatory cytokines, and activate stellate cells for collagen deposition, which ultimately increases oxidative stress to induce cell/tissue damage (Browning and Horton, 2004). In the field of modern biology to assess oxidative stress, MDA is an extensively utilized biomarker. To predict the pattern of various diseases, such as diabetes, hypertension, cancer, heart failure and atherosclerosis, MDA has been used as a potent biomarker in both in vivo as well as in vitro studies (Kulkarni et al., 2018). In patients suffering from osteo-arthritis, MDA can be detected in the sections of joint tissue. In both patients suffering from lung cancer as well as glaucoma, the concentration of MDA is high; thereby validating the reliability of MDA assay to find out oxidative stress in relation to the pathology of various diseases (Tiku et al., 2007; Singh Z. et al., 2014). Quantification of the plasma MDA level is evaluated mainly via a colorimetric reaction with thiobarbituric acid (TBA) (Meagher and FitzGerald, 2000). Novel antibody-based tests are possible using standard ELISA kits validated against high-performance liquid chromatography (HPLC), which have produced reliable and specific results (Bevan et al., 2003). Recently, a non-invasive method of quantification of MDA biomarker in human exhaled breath condensate using self-assembled organic-inorganic nanohybrid was used, and it has shown promise for diagnosing lung diseases being appropriate, reliable, inexpensive, fast, and user-friendly diagnostic tool (Jafari et al., 2019).
Investigations in dairy cattle indicated that the highest levels of plasma MDA reflected metabolic disturbances, especially around parturition and the early stages of lactation (Turk et al., 2004; Castillo et al., 2005). MDA and total anti-oxidant status (TAS) values are suggested as effective indicators for the oxidant-antioxidant balance and could be employed to generate complementary measures of animal homeostasis (Castillo et al., 2006; Ho et al., 2013). HPLC with diode-array detection (HPLC-DAD) was revealed as a selective, reproducible, and sensitive method to measure MDA in goat plasma as an oxidative stress biomarker (Yonny et al., 2016). In addition, gas chromatography coupled with tandem mass spectrometry (GC/MS/MS) is a useful method in long-term clinical studies of circulating MDA as a biomarker of lipid peroxidation, and its relevance to F2-isoprostane 15(S)-8-iso-prostaglandin F2α and nitric oxide (NO) has been demonstrated (Tsikas et al., 2016). Another study reported that GC-electron-capture negative ion chemical ionization (ECNICI)-MS measurement of nitrite and malondialdehyde in human urine is important as a surrogate internal standard for MDA (Hanff et al., 2016). A recent study demonstrated malondialdehyde-modified low-density lipoprotein (MDA-LDL) to be a good candidate for predicting the endovascular therapy outcome in patients affected with peripheral artery disease (Takamura et al., 2017). Acute stroke can be identified using levels of MDA (Liu Z. et al., 2017). Recently, MDA has been evaluated as an oxidative stress diagnostic biomarker in diabetes (Yatoo et al., 2016; Ma et al., 2018), ketosis, ovarian cyst, mastitis and lameness (Kapusta et al., 2018). Its elevated concentration in milk and meat has shown deleterious effects on milk (Yatoo et al., 2015; Kapusta et al., 2018), and meat (Cimmino et al., 2018) quality and hence can serve as a quality biomarker in foods.
As MDA is a lipid peroxidation product and determines the extent of damage of biological membranes, it can suitably be evaluated as a biomarker for degradative processes/stresses or diseases.
Isoprostanes
These are prostaglandin-like compounds released from the peroxidation of arachidonic acid, independently of the normal cyclo-oxygenase pathway, which are subsequently released for circulation by phospholipases (Griffiths and Moller, 2002; Stafforini et al., 2006; Czerska et al., 2016). The presence of isoprostanes, especially F2-isoprostane (F2-Isops), can be quantified from various biological sources, such as blood (Siti Hajar et al., 2018), urine (Roy et al., 2015), cerebrospinal fluid (Finno et al., 2018), or other fluids or tissues (Annelies et al., 2018; Finno et al., 2018; Jadoon and Malik, 2018). F2-Isops, being the most stable among the isoprostanes, is the most potent isoprostane biomarker and its level can reflect the oxidative status of vital organs, such as liver or kidneys (Morrow, 2005; Musiek et al., 2005). In both humans and animals, increased plasma and urine concentrations of F2-Isops correlate significantly with oxidative stress, revealing its potency as a stress marker (Fam and Morrow, 2003; Van't Erve et al., 2016). F2-Isops can be quantified using gas/liquid chromatography associated with mass spectrometry, immunological assays, including ELISA/radioimmunoassays (RIAs), and using commercial assay kits (Musiek et al., 2005; Smith et al., 2011). In addition, elevated levels of the oxidative stress biomarker 8-iso-prostaglandin F2α (8-iso-PGF2α) in wastewater is associated with tobacco use and represents a powerful wastewater biomarker to evaluate community public health (Ryu et al., 2016). Interestingly, it is reported that long-term supplementation with vitamin E reduces oxidative stress in smokers, which is determined by 8-iso-PGF2α detection (Guertin et al., 2016). Isoprostanes have been evaluated as biomarkers in equine neuroaxonal dystrophy (Finno et al., 2018), Creutzfeldt-Jakob disease, Huntington's disease, Alzheimer's disease, multiple sclerosis (Jadoon and Malik, 2018), Attention-Deficit/Hyperactivity Disorder (ADHD) (Annelies et al., 2018), and in passive smokers (Siti Hajar et al., 2018).
Some isoprostanes have found clinical applications in obesity, ischemia-reperfusion injury, the central nervous system, cancer, and genetic disorders (Milne et al., 2015). CSF isoprostane levels have been beneficial in evaluating oxidative stress in multiple sclerosis in humans (Mir et al., 2014) whereas plasma or milk isoprostane levels were diagnostic for oxidative stress in lactating dairy cows (Vernunft et al., 2014).
Enzymatic Anti-oxidants
Most potent anti-oxidant actions are mediated by enzymes, especially superoxide dismutase, glutathione peroxidase, and catalase, which mediate the direct reduction of ROS (Carocho et al., 2018). Glutathione peroxidase is a selenoenzyme that can reduce large quantities of hydroperoxide radicals in association with thiols like glutathione. The level of serum glutathione peroxidase is an excellent measure of the oxidative status of an individual and is most often employed in diagnostics (Gheita and Kenawy, 2014). Superoxide dismutase (SOD) and catalases reduce ROS directly into metabolic water and oxygen molecules, thereby preventing oxidative damage to tissues. Thioredoxin reductase is another selenoprotein-based antioxidant enzyme that has a critical role in reducing ROS into the less reactive water and alcohol, preventing their oxidant action (Hara, 2001; Grignard et al., 2005; Trigona et al., 2006). At present various reliable commercial assay kits are available to assess these biomarkers effectively (Blankenberg et al., 2003). Fluorometric assays for GSH/GSSG ratio (GSH/GSSG Ratio Assay Kit) and Total Antioxidant Capacity (Total Anti-Oxidant Capacity Assay Kit) from Abnova USA, Abcam USA, Sigma-Aldrich USA, Cayman Chemical USA or Bioassay Systems USA, Immunoassay for ArborAssays USA and Cell Biolabs USA, spectrophotometric method for aconitase (BIOXYTECH® Aconitase-340 Assay) are available. These have been used in numerous oxidative stress-related studies (Ijomone et al., 2014; Chauhan et al., 2017; Zhang Y. et al., 2017; Dada et al., 2018; Peng K. T. et al., 2018). They have been used in clinical applications, e.g., evaluating total anti-oxidant status in diabetic patients (Rani and Mythili, 2014).
Myeloperoxidase is a heme-based enzyme from proinflammatory cells that generate ROS, especially during phagocytosis in response to microbial attack, resulting in modification of biomolecules if not regulated. Spectrometric evaluation of its plasma concentration is a reliable method to assess the oxidative status and subsequent damage in vivo (Nicholls and Hazen, 2005). Myeloperoxidase is released into circulation, and its level in serum has been suggested as a useful measure of atherosclerotic plaque vulnerability in cardiac patients (Sugiyama et al., 2004). An elevated myeloperoxidase concentration is documented in various studies of coronary artery diseases, indicating the prognostic significance of myeloperoxidase in these conditions (Sugiyama et al., 2001; Zhang et al., 2001; Tsimikas, 2006). Myeloperoxidase has found clinical applications in rheumatoid arthritis, cardiovascular diseases, liver diseases, diabetes, and cancer (Coculescu et al., 2018; Khan et al., 2018).
A crucial role is played by oxidative stress in periodontitis. The level of SOD is found to be high in periodontitis. Periodontal ligament possesses this enzyme; thereby neutralizing the activity of reactive oxygen species (ROS). The SOD is introduced due to the release of superoxide stimulated by polysaccharide of bacteria. Recently clinical significance of SOD in gastric cancers has been summarized (Li et al., 2019). In chronic cases of periodontitis, the enzyme glutathione peroxidase shows variation in concentration. There may be an increase or decrease in the level of this enzyme (Aziz et al., 2012; Jeeva et al., 2015). In patients suffering from oral cancer, there is a reduction in the activity of catalase enzyme which is attributed to high amount of superoxide anion or reduction in enzymatic scavenging activity (Patel et al., 2009).
Glutathione reductase is another enzymatic anti-oxidant that catalyzes the reduction of glutathione disulfide (GSSG) to the sulfhydryl form glutathione (GSH) (Maciejczyk et al., 2018a). The levels of oxidized glutathione (GSSH) and reduced glutathione (GSH) predict oxidative stress and hence the ratio of GSH/GSSG is used as an oxidative index (Zitka et al., 2012; Giustarini et al., 2016). However, there are concerns regarding the use of this index as a measure of oxidative stress (Sentellas et al., 2014). Still, there are numerous efficient methods of expressing this index (Sentellas et al., 2014). Some prooxidant enzymes (xanthine oxidase and NADPH oxidase) that help in generation of ROS and aggravate oxidative stress, can also serve as diagnostic biomarkers in oxidative stress to evaluate severity (Maciejczyk et al., 2018b; Simioni et al., 2018). In the case of systemic oxidative stress, tissues respond diversely with respect to glutathione concentration. Barry-Heffernan et al. (2019) have reported that the GSH levels in erythrocyte and plasma are not correlated to that in liver biopsy tissues of dogs, which are clinically indicated for liver biopsy, suggesting that the GSH levels in circulatory system may not be ideal for assessing the redox status of the liver.
Blood Urates
Urates are the major end products of purine metabolism in mammals and have inherent anti-oxidant action. Blood plasma and cerebrospinal fluid (CSF) urate concentrations are associated with cellular models of neurodegeneration, which might be due to their capacity to reduce oxidative stress, mitochondrial damage, and cellular apoptosis (Guerreiro et al., 2009). Peroxyl (ROO•) and hydroxyl (OH•) radicals, which are capable of inducing DNA damage in cells, are inhibited powerfully by the anti-oxidant potential of urates. Urates' shielding action has also been linked to its capacity to form complexes with metal ions in cells under attack by oxidative damage. Unabated elevation of the ROS and hemoprotein/H2O2 systems in cells causes oxidation of urates to inactive forms, reducing their potency and efficacy. Laboratory-based epidemiological and clinical investigations in neurological diseases, especially Parkinson's diseases, revealed a negative correlation between blood and CSF urate concentrations and disease progression (Cipriani et al., 2010). Biochemical evidence indicated that the urate level is a promising biomarker to assess the incidence, diagnosis, and therapeutic prognosis of various neurodegenerative conditions, and suggested the possible therapeutic efficacy of endogenous urate molecules. Notably, under normal conditions, the kidneys continuously excrete uric acid out of the body, and the presence of circulating uric acids in the body is an important determinant of renal impairment (Stamp et al., 2011). In addition to being the routine biomarkers of kidney (Klein et al., 2018; Lu et al., 2018) and liver diseases (Drolz et al., 2018), urates or its related products are also proving to have diagnostic value in other important diseases, such as Parkinson's disease (Cova and Priori, 2018), diabetes (Xie et al., 2018), cardiovascular diseases (Murata et al., 2018), obstructive sleep apnea (Fleming et al., 2018), and bone inflammation (Beyazit and Pek, 2018). Urates or urea derivatives have also shown applicable values in clinical diagnosis of renal diseases (Yang et al., 2018), gastrointestinal and hepatic diseases (Siddiqui et al., 2016), using advanced technologies like self-powered implantable electronic-skin and non-invasive breath test, respectively.
Cortisol
The primary mediator of the physiological changes during stress is the neuroendocrine axis. In this process, the hypothalamic-pituitary-adrenocortical (HPA) system regulates the secretion of cortisol, and the sympathetic adrenomedullary (SAM) system regulates catecholamine secretion. Significant correlations have been observed between salivary cortisol and blood cortisol concentrations, especially during stress. In response to various stresses, the HPA system is activated, which induces the secretion of cortisol into the blood, and in this regard, salivary cortisol can be a reliable estimate of stress-induced HPA activity. Salivary cortisol mostly exists in the unbound (free) form, accounting for ~70% of the total unbound cortisol in the body (Jung et al., 2014). This unbound cortisol, because of its low molecular weight and liposolubility, diffuses through the acinar cells of the salivary gland and is secreted into the saliva (Ivković et al., 2015).
The urinary cortisol concentration cannot be exactly correlated with the blood concentration because of renal tubular reabsorption and secretion; therefore, salivary cortisol represents a good alternative and has become the most frequently studied stress biomarker in salivary samples (Hellhammer et al., 2009). Studies on stress-related depressive disorders revealed that such disorders could be diagnosed through cortisol levels (Islam et al., 2018; Xu Y. Y. et al., 2018). Another study revealed that patients with the lowest cortisol concentrations showed the least improvement in agoraphobic avoidance after psychotherapy (Wichmann et al., 2017), demonstrating an inverse association of the cortisol stress response with agoraphobic avoidance after psychotherapy. Also, in 198 Rhesus macaques (89 male) with demonstrated extensive alopecia (>30% hair loss), alopecia, hair loss, and hair cortisol concentrations were associated with elevated chronic cortisol concentrations (Novak et al., 2017). Furthermore, major depression is related to long-term attenuation of cortisol secretion (Steudte-Schmiedgen et al., 2017). Recently, a study was conducted to know the diagnostic value of oxidative stress markers, namely cortisol and α-amylase, in saliva to identify preterm birth in women. Results showed that increased cortisol level during pregnancy could be used as a tool to predict preterm birth (García-Blanco et al., 2017a).
Another way of monitoring stress is the assessment of cortisol from hair samples. This can be a complementary mode of analyzing systemic cortisol over longer periods in comparison to the cortisol concentration in saliva and urine samples which reveal only real-time data. This method finds application in cortisol quantification in chronic inflammations as well as acute conditions like myocardial infarctions (Russell et al., 2012). Stress hormones, like glucocorticoids along with cytokines, act as master homeostatic regulators in circulation, which mediate several conditions like post-traumatic stress disorder (PTSD) along with key vital pathways both peripherally and centrally, and represent promising functional biomarkers of stress responses in human as well as animal subjects; thus can be targeted for developing novel therapeutics (Michopoulos et al., 2015; Daskalakis et al., 2016). Though novel biomarkers are being explored for stress, however, still various recent studies have focused on cortisol of various origins (Egawa et al., 2018; Suh, 2018). Oxidative injury by other oxidants like MDA also causes the release of cortisol and hence both in the association can serve as diagnostic oxidative markers in diseases (Islam et al., 2018; Xu Y. Y. et al., 2018).
Evaluations of novel cortisol in hair or sweat has shown diagnostic value in various forms of stress or diseases, and has found clinical applications in Cushing syndrome (particularly Cyclical Cushing), Adrenal insufficiency (including Addison's disease), therapy monitoring, cardiovascular disease, stress, and mental illness (Meyer and Novak, 2012; Jia et al., 2016; Greff et al., 2019).
Copeptin
Copeptin is a polypeptide derived from the hypothalamo-pituitary axis-system, as a pre-prohormone along with vasopressin and neurophysin II. This C-terminal derivate of the arginine vasopressin mainly regulates water and electrolyte balance, hence has a diagnostic role in cardio-renal dysfunction (Tan and Sethi, 2014). Even though vasopressin is a major hypothalamic stress hormone, application of circulating vasopressin as a stress biomarker is challenging due to its pulsatile release, instability in plasma and rapid clearance (Morgenthaler et al., 2008). Copeptin, being a co-component of pre-pro-hormone and released as a more stable protein in an equimolar ratio to vasopressin, can be finely employed for assessing the individual stress level in comparison to cortisol (Katan and Christ-Crain, 2010). Clinically the prognostic accuracy of copeptin in acute illness, such as sepsis, pneumonia, lower respiratory tract infections, stroke, has been analyzed successfully (Katan and Christ-Crain, 2010). Because of the molecular stability, easier and faster test procedures and results, copeptin are used as a replacement along with cardiac troponins for faster diagnosis of myocardial infarction. Heart failure (HF) can be predicted well by using copeptin as a biomarker in combination with brain-type natriuretic peptide (BNP). There is a rise in the levels of copeptin in cardiovascular shock (Kristyagita and Siswanto, 2015). In recent times though copeptin is diagnostic biomarker for kidney (Tasneem et al., 2018) and heart (Berezin, 2018; Xu L. et al., 2018) related ailments mainly, but in future has good scope for evaluation of other systems or diseases as these systems are interdependent and affect one another, e.g., cardio-pulmonary or hepato-renal disorders. It has found clinical applications in acute myocardial infarction (Ay et al., 2017; Aydin et al., 2019), polycystic kidney disease (Tasneem et al., 2018), insulin resistance and metabolic syndrome (Saleem et al., 2009).
Alpha-Amylase
Although the stress-induced sympathetic adrenomedullary system regulates catecholamine secretion, the salivary enzyme α-amylase has been estimated as a marker for sympathetic stimuli (Rai and Kaur, 2011). In normal conditions, the level of this adrenalin-induced enzyme is lowest in the early morning hours and highest in the late afternoon (Takai et al., 2004). In response to stress, the α-amylase concentration increases drastically, indicating that this can be considered as a potent salivary biomarker of stress (O'Donnell et al., 2009; Strahler et al., 2010). Due to the stress (acute) caused during venipuncture, the concentration of α-amylase in saliva increases (Koh et al., 2014). It was suggested that the α-amylase level in saliva could reflect nervous system activity exercise responses in elite male wheelchair athletes, with or without cervical spinal cord injury (Leicht et al., 2017). In recent findings, salivary amylase has been found to be diagnostic in oral disease (Lorenzo-Pouso et al., 2018), renal diseases (Maciejczyk et al., 2018b), cardiovascular and psychological diseases (Mishra, 2017).
Salivary amylase has been used as biomarkers for clinical evaluation of stress in pigs (Escribano et al., 2019), acute abdominal disease in horses (Contreras-Aguilar et al., 2019), neurobehavioral activity (Pajcin et al., 2019) and radiation exposure in humans (Balog et al., 2019).
Secretory IgA
Various studies have shown interactions between the neuroendocrine system and the immune system, and this also occurs in stress conditions. The induction of stress hormones, especially cortisol, harms immunoglobulin secretion, thereby decreasing the concentration of immunoglobulins in body fluids (Mocci and Bullitta, 2006; Lee et al., 2010). Furthermore, higher salivary IgA, as well as decreased anxiety, were linked with fewer potentially pathogenic oral bacteria and enhanced oral immunity (Lamb et al., 2017). IgA has a diagnostic role in gastrointestinal diseases (Siddiqui et al., 2017), stress-immunity link diseases (Staley et al., 2018), maintenance of the intestinal epithelial barrier, gut health and microbiota regulation (Donaldson et al., 2018; Ducatelle et al., 2018), besides playing role in gut nutrition and immunity (Celi et al., 2018), Hence, IgA is considered as a non-invasive biomarker of gastrointestinal functionality, microbiota, health and immunity (Celi et al., 2018; Ducatelle et al., 2018).
Chromogranin A (CgA)
CgA is an acidic protein prohormone that is present in the secretory granules of different neuroendocrine tissues, and has been recognized as a marker of mental stress (Yamakoshi et al., 2009). It is stored primarily in adrenal gland vesicles and is released into the circulation, along with catecholamines, via exocytosis (Ivković et al., 2015). In normal subjects, higher levels of CgA are observed during the night, and lower levels are seen in the morning (Giampaolo et al., 2002); however, significantly higher concentrations of CgA were observed in saliva samples collected immediately after exposure to various stresses (Ng et al., 2003; Takatsuji et al., 2008). CgA was also proposed as an important biomarker in diabetes (Broedbaek and Hilsted, 2016). Recent studies evaluated CgA as a valuable biomarker in various stressful diseases including neuroendocrine tumors (Di Giacinto et al., 2018), cardiovascular disorders (Ottesen et al., 2017; Mahata et al., 2018), atopic dermatitis (Cai et al., 2018), ulcerative colitis (Magnusson et al., 2018) and diabetes mellitus (Herold et al., 2018).
Serum CgA is considered as the diagnostic biomarker for gastroenteropancreatic neuroendocrine neoplasms and has been utilized in clinical applications (Pulvirenti et al., 2019; Zhang et al., 2019). However, it has not been found effective as a biomarker for diagnosis or management of bronchopulmonary neuroendocrine tumors/neoplasms (Matar et al., 2019). Also, in pancreatic neuroendocrine tumors, CgA as a clinical biomarker has found limited role. Salivary CgA could be used as a potential biomarker in animal production systems to monitor the severity of social stress and behavioral aggression. Chromogranin A is highly correlated with the skin lesions due to fighting in weaning piglets as it is an indicator of activation of sympathetic adrenomedullary stress pathway (Escribano et al., 2019).
Lysozyme
Lysozyme is a prominent anti-bacterial peptide in the external secretory fluids of humans and animals. This cationic protein shows potent bactericidal actions by hydrolyzing bacterial cell walls (peptidoglycan), especially those of Gram-positive bacteria. Studies have reported that there is a negative correlation between lysozyme concentration and stress exposure, which is in accordance with increased susceptibility to bacterial invasion during stress (Yang et al., 2002; Allgrove et al., 2008). Another study revealed that lysozyme is related to circulating RNA, extracellular vesicles, and chronic stress (Abey et al., 2017). Currently lysozyme as diagnostic biomarker has found applications in chronic stress (Abey et al., 2016), cancer metastasis (Brzozowski et al., 2018), cardiovascular markers, psychological research (Mishra, 2017), oral diseases (Lorenzo-Pouso et al., 2018), diabetes (Maciejczyk et al., 2017), wound healing (Abey et al., 2016), infectious diseases (Ghosh et al., 2018; Stjärne Aspelund et al., 2018), Graves' disease and orbitopathy (Zhang L. et al., 2018). Serum lysozyme has been used as a clinical biomarker for diagnosing sarcoidosis with high specificity (Ramos-Casals et al., 2019). Similarly, plasma lysozyme has been used as a putative biomarker of atherosclerosis (Abdul-Salam et al., 2010).
Conventional biomarkers generally are weak in their sensitivity, specificity, and poor reflectors of the complex interactions underpinning the cellular and molecular changes during stress related disorder and diseases. Complex biological networks delineated through computational algorithms can forecast impending molecular alterations, which may further results in stress disorder or clinical diseases. In this regard, stress response or a clinical illness may be perceived very early through probing the emergent skewing of molecular pathways. At the same context conventional serum, cellular and molecular markers may take enough time to reflect its detectable level in the respective diagnostic fluid, so that computational algorithms tailored for mining the omics data trespassed the many conventional approaches.
MicroRNAs (miRNAs)
MicroRNAs, short sequences of RNA (~22 nucleotides), are a class of small non-coding RNA segments that are regulated and transcribed like protein-coding genes (Bartel, 2000; Trzybulska et al., 2018). MicroRNAs regulate gene expression post-transcriptionally and influence normal biological processes, as well as various pathological conditions (Gilad et al., 2008). They are also present in cell-free body fluids like serum, suggesting their utility as non-invasive clinical biomarkers for prediabetes, diabetes, and related complications (Vaishya et al., 2018). MicroRNAs in serum was demonstrated to be stable and are sufficiently robust to serve as practicable clinical biomarkers to differentiate the patients with autoimmune disease from healthy individuals (Jin et al., 2018). Easily accessible biomarkers to evaluate and predict pregnancy complications are required urgently; serum levels of miRNAs reflecting critical physiological conditions, such as pregnancy and its associated complications, could be exploited as useful markers, suggesting their clinical utility to determine pregnancy stages and related abnormalities (Liang et al., 2007). Many miRNAs are present in maternal serum and their level increase with gestational age. Recently, distinctive expression of miRNAs in the placenta in association with pre-eclampsia was observed, which highlighted the possibility that serum levels of particular miRNAs might serve as future diagnostic biomarkers for pre-eclampsia (Walker, 2000; Pineles et al., 2007). Further detailed investigations on miRNAs revealed the potential of cell-free miRNAs in body fluids to serve as practical and reliable molecular markers to assess diverse physiological and pathological conditions. Among these conditions, the possible critical roles of miRNAs in tumor diagnosis, disease progression, and prognosis have received increased research attention (Yan et al., 2016). Accumulating data suggest the application of abnormally expressed miRNAs in blood and serum as promising candidates to predict hepatocellular carcinoma (Jiang et al., 2015; Shen et al., 2016). Circulating miRNAs in blood could serve as novel diagnostic markers for various disease conditions owing to their evolutionary conservation and stability. The potential of serum miRNAs as non-invasive biomarkers for assessing the progression of subarachnoid hemorrhage has been recently explored by Lai et al. (2017). Studies are being demanded in elucidating the critical role of circulatory miRNAs as coagulation and thrombosis biomarker in order to find their clinical application in predicting complications like stroke (Vijayan and Reddy, 2016). Their usage as potential biomarkers in equine medicine has been recently reviewed by van der Kolk et al. (2015). MicroRNAs might be exploited as novel diagnostic markers for myopathies, recurrent exertional rhabdomyolysis, and osteochondrosis. MicroRNAs in blood could also be important in glucose metabolism pathway of the equine. Further investigations and validations are required for these novel molecular markers, particularly to determine better reliable body fluid miRNA profiles to exploit their clinical utilization, thereby paving the way for their wider application in the future.
Currently, miRNAs are being studied as potential diagnostic biomarkers in both epidemiological (He et al., 2018) and clinical studies (Pogribny, 2018). They are proving helpful in all fields of medicine, be it for elucidating disease associations (He et al., 2018), etiology (Liguori et al., 2018), diagnosis (Wang H. et al., 2018; Zhou Q. et al., 2018), typing (Pérez-Sánchez et al., 2018), therapeutics (Roy et al., 2018; Zhou, S. S. et al., 2018), progression (Clark et al., 2018), perioperative medicine (Kreth et al., 2018) and much more. In diagnosis, they have been found to possess great applications. They are being used for diagnosis of cancers (Wang H. et al., 2018; Zhou Q. et al., 2018), cardiovascular diseases (Pérez-Sánchez et al., 2018; Zhou, S. S. et al., 2018), hepatic diseases (Schueller et al., 2018), renal diseases (Shaffi et al., 2018), sporadic amyotrophic lateral sclerosis (Liguori et al., 2018), Parkinson's disease (Roser et al., 2018), etc.
Heat Shock Proteins (HSPs)
Heat shock proteins (HSPs) are molecular chaperones with multiple physiological roles. HSPs comprise highly conserved protein families across different species of animals. The HSP family comprises various critical proteins, such as HSP60, HSP70, and HSP90, among which HSP70 is the most prominent, with significant effects on diverse biological systems and therapeutic potential (Shrestha et al., 2016; Khandia et al., 2017). Various HSPs are induced in response to short-term stress, such as thermal stress, osmotic stress, heavy metal toxicity, and ecological stress from pollutants (Hecker and McGarvey, 2011). Environmental stress acts as predisposing factors for the synthesis and secretion of various heat shock proteins at greater concentration. Such stresses include infection and inflammation, exercise, the cell being exposed to various toxic substances, dearth of water, etc. This is the reason why these proteins are also termed as stress proteins (Santoro, 2000). The mechanisms of activation of heat shock factor by heat shock have been well-described in bacteria. There is no unfolding of outer membrane proteins (OMPs) during stress; thereby insertion of these proteins occurs inappropriately in the outer membrane; ultimately accumulation occurs between the inner cytoplasmic membrane and outer membrane (periplasmic space). A protease of the inner membrane detects these OMPs and the signal is passed to a transcription factor sigmaE (Walsh et al., 2003). Upregulation of certain heat shock proteins of bacteria occurs through RNA thermometers, such as HSP90 cis-regulatory element (Narberhaus, 2010). Post-transcription and translation studies revealed that the expression of HSPs increases dramatically in response to other stresses and degenerative conditions, such as hypoxia-induced tissue injuries, ischemia, and CNS degeneration (Li et al., 2004; Mariucci et al., 2007). These HSPs ultimately serve as the endogenous mediators that initiate intracellular cascades to provide cellular protection from the stresses mentioned above. HSP70 was first reported in the fruit fly, Drosophila melanogaster, where it was found to have a half-life of 2 h, after which its activity decreases rapidly (Li and Duncan, 1995). Continuous secretion of HSP70 is induced by ongoing exposure to thermal, osmotic, hypoxic, or toxic stresses. Besides, the co-localization of HSP70 with early indicators of cellular stress, such as the cytokines c-fos and c-jun, has been observed; however, the HSP response is specific to the type of stress and cellular factors. HSPs are governed tightly by cellular regulatory mechanisms, such that those tissues with thermal tolerance can restrict its responses to stresses by eliciting feedback signals that regulate both transcription and translation (Van Eden et al., 2010). Certain non-classical secretory pathways also exist for the active secretion of HSP70, especially those proteins concerned with the stress response in lipid rafts (Multhoff, 2007). This demonstrated the presence of HSP70 in the cellular membranes of tumor–affected cells and by its association with lipid raft receptor complexes (Bausero et al., 2005; Mambula et al., 2007). HSPs, especially HSP70, also induce anti-inflammatory responses, in particular through regulatory T lymphocytes (Tregs) (Mariucci et al., 2007). Role of HSP70 as a biomarker in monitoring environmental diseases, such as mycotoxicoses has been explored and reported to be of potential application (El Golli-Bennour and Bacha, 2011).
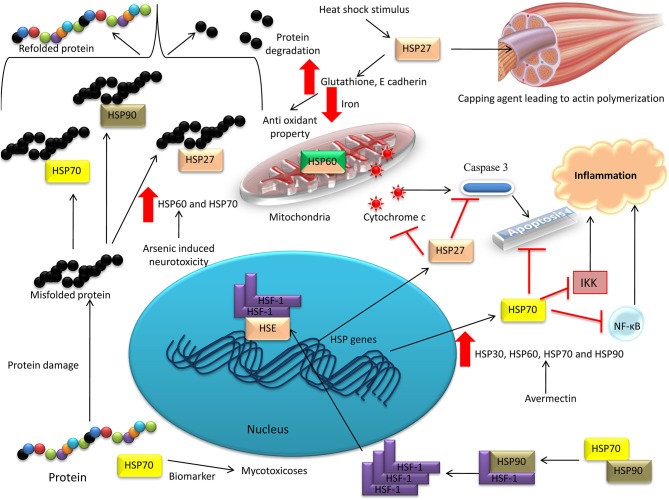
Another member of the HSP family, HSP27, belonging to the small molecular weight HSP family, mediates canonical roles in response to various stresses (Vidyasagar et al., 2012). Initially, HSP27 was characterized as a potent marker for thermal stress, facilitating the effective re-orientation of misfolded proteins (Rogalla et al., 1999; Lelj-Garolla and Mauk, 2006). HSP27 responds to heat shock stimulus in muscle tissues, regulating actin-mediated cytoskeletal dynamics, especially as a capping agent that aids actin polymerization. Furthermore, HSP27-based studies reported that this protein could be a marker not only for thermal stress but also for oxidative and chemical stresses (Vidyasagar et al., 2012). Oxidative stress mediated through the actions of ROS can be resisted effectively by HSP27, which plays a role as a potent anti-oxidant by elevating intracellular glutathione concentrations and limiting the intracellular iron concentration (Arrigo et al., 2005). HSP27 also interacts with apoptosis pathways, thereby mediating an anti-apoptotic effect. It influences the extrinsic pathway of apoptosis by preventing the interaction of activation of apoptosis signal-regulating kinase 1 (Ask 1) with death domain-associated protein (DAXX) (Charette and Landry, 2000). In addition, HSP27 inhibits the intrinsic and mitochondrial apoptotic pathways via its action on Bax (apoptotic regulator protein) and cytochrome c (Bruey et al., 2000; Havasi et al., 2008). HSP27 also exerts an anti-apoptotic effect by inhibiting the caspase pathway (Calderwood et al., 2006). These mechanisms can be effective in preventing chemical stress in vital tissues, especially in response to high doses of new generation chemotherapies (Nakashima et al., 2011). Figure 2 depicts the role of HSPs as stress biomarkers.
Figure 2.
Heat shock proteins as stress biomarkers. HSP70 has been reported as a biomarker in monitoring environmental diseases, such as mycotoxicoses. HSP27 was characterized as a potent marker for thermal stress, facilitating the effective re-orientation of misfolded proteins. HSP27 inhibits the intrinsic and mitochondrial apoptotic pathways via its action on Bax and cytochrome c. HSP60 and HSP70 was demonstrated to have neuroprotective function in arsenic-induced neurotoxicity in red jungle fowl. HSP30, HSP60, HSP70, and HSP90 were elevated in an Avermectin toxicity model in the cardiac tissues of pigeons.
Elevated levels of HSP60 and HSP70 demonstrated a neuroprotective function in arsenic-induced neurotoxicity in red jungle fowl, Gallus gallus (Zhao et al., 2017). The mRNA transcriptional and protein levels of HSP30, HSP60, HSP70, and HSP90 were elevated in an Avermectin (anthelmintic drug) toxicity model in the cardiac tissues of pigeons (Liu C. et al., 2017). Furthermore, elevated levels of HSP90 and HSP70, and glucose-related protein 78 (GRP78), in medullary thyroid carcinoma revealed their potential role in medullary thyroid carcinoma tumor biology, suggesting that they could be developed as biomarkers in the future (Soudry et al., 2017).
Besides heat stress (Baena et al., 2018; Sales et al., 2018), heat shock proteins (HSP) are being evaluated in apoptosis, oxidative stress, inflammatory diseases, cancer (Ikwegbue et al., 2017), virus infection (Shan et al., 2018), bacterial infection (Kim et al., 2018), as immunomodulators (Edkins et al., 2017; Zininga et al., 2018), therapeutics (Skórzynska-Dziduszko et al., 2018), and diagnostics (Lechner et al., 2018; Tang T. et al., 2018). HSPs have diagnostic role in ischemic injury of cardiomyocytes (Santos et al., 2018), inflammatory process of multiple sclerosis (Lechner et al., 2018), early diagnosis of lung cancer (Tang T. et al., 2018), proteome stress (Liu and Zhang, 2018), bipolar disorder (Cheng et al., 2018), and anti-apoptotic agent (Jang et al., 2018).
Acute Phase Proteins
The innate immune system elicits certain key and prompt responses to defend the body against infection, inflammation, stress, tumor progression, or tissue injury. These systemically activated complex early defensive responses, termed acute phase responses, are promoted by acute phase proteins (APPs), which are serum components, produced primarily by hepatocytes (Jain et al., 2011). Acute phase response (APR) organs include the brain (involved in the increased synthesis of corticotropin-releasing hormone (CRH) and adrenocorticotropic hormone (ACTH), liver (involved in the increased synthesis of metallothionein and antioxidants to restore homeostasis of plasma proteins), bone marrow (increased thrombocytosis and reduced erythropoiesis), adrenal gland (increased cortisol production), and muscle (proteolysis) and adipose cells (altered lipid metabolism) (Robinson et al., 2016). The APR is regulated via interleukin 1 receptor antagonist (IL-1RA), IL-10, suppressor of cytokine signaling (SOCS) proteins, and transient expression of APP and their mRNA half-lives (McCormick et al., 2016; Chakrabarti et al., 2018). There are ~200 different APPs in animals. Classification of APPs and their role as diagnostic tool have been reviewed (Jain et al., 2011). APPs are normally secreted under the influence of innate immunity or stress and whose concentrations change upon secretory stimuli. The serum concentrations of positive APPs, such as C-reactive proteins (CRP) and serum amyloid A (SAA), are elevated significantly in response to infections and inflammations (Mittelman et al., 2018). While the serum concentrations of negative APPs, such as albumin and transferrin, decrease in response to infection, inflammation, and stress (Cray et al., 2009). The protein with the highest concentration in serum is albumin, and its reduction or selective loss in biological fluids indicate degenerative conditions of the renal/gastrointestinal system or hepatic insufficiency (Paltrinieri, 2008).
In the 1930s, CRP was the first APP to be described scientifically. This was followed by the discovery of other APPs, including SAA, serum amyloid P (SAP), haptoglobin, ceruloplasmin, fibrinogen, major acute phase protein (MAP), lipopolysaccharide-binding protein (LBP), and α1-acid glycoprotein (AGP) (Kushner, 1982; Petersen et al., 2004; Shamay et al., 2005; Cheung et al., 2008; Ceciliani et al., 2012). Various researchers revealed the influence of these proteins on human health and animal physiology, resulting in them being termed “molecular thermometers” (Murata et al., 2004; Ceron et al., 2005; Cray et al., 2009; Jain et al., 2011). Human CRP is regarded as the primary detector for autoimmune/traumatic/neoplastic conditions (Eckersall et al., 2007). Recent studies in animals indicated the sensitivity of different APPs, suggesting them as strong markers of herd health in large animals (Ganheim et al., 2007; Ceciliani et al., 2012).
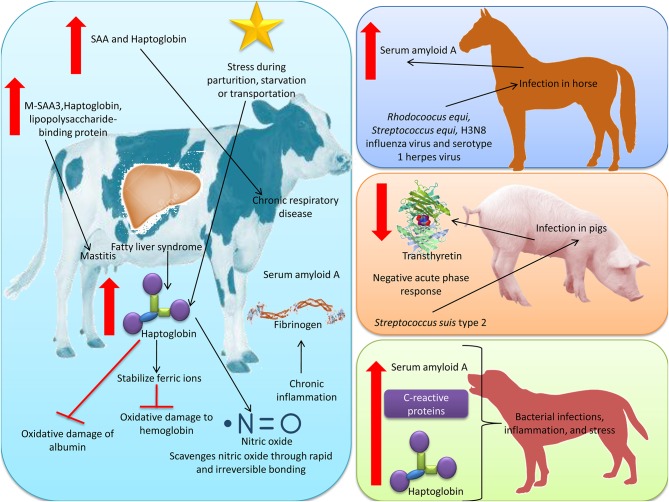
APPs have been studied immensely in pets and companion animals. In these species, they have been suggested as the optimum markers for the prognosis of stress conditions and various diseases. Advances in canine and feline medicines have identified several APPs as biomarkers in the prognosis of inflammatory, degenerative, or septic conditions, such as pancreatitis, septic acute kidney injury, mammary tumor, autoimmune disorders, reproductive complications, pyometra, and cardiovascular changes (Hori, 2006; Bayraml and Ulutas, 2008; Gebhardt et al., 2009; Hollinger et al., 2018). Similar to humans, CRP is the primary APP in canines, along with haptoglobin and SAA, whose concentrations are elevated in bacterial infections, inflammation, and stress (Martinez-Subiela et al., 2002; Ceron et al., 2005; McGrotty et al., 2005). In feline species, the serum concentration of α1-acid glycoprotein and SAA are valuable markers of stress, infection, and other inflammations (Verbrugghe et al., 2014). Figure 3 depicts the role of APPs (SAA) as stress biomarkers.
Figure 3.
Acute phase proteins as stress biomarkers. Increased level of haptoglobin was noticed in cattle in conditions like fatty liver syndrome and stress induced by parturition, starvation, or transportation. There was also increase in SAA and fibrinogen in cattle during chronic inflammation and associated stress. Haptoglobin exerts its anti-oxidant role by stabilizing ferric irons to prevent oxidative damage to hemoglobin. Haptoglobin protects albumin from oxidative damage by inhibiting the exchange of heme between hemoglobin and albumin. Haptoglobin scavenges nitric oxide through rapid and irreversible bonding, thereby limiting its bioavailability and preventing oxidative damage from reactive nitrogen species. Haptoglobin and SAA are synthesized in the bovine mammary epithelium, and the substantial increase in their secretion into milk was observed during mastitis. SAA has been found to increase in sera of foals during infections with bacteria, i.e., Rhodocoocus equi and Streptococcus equi and viruses, i.e., H3N8 influenza virus and serotype 1 herpes virus. Streptococcus suis type 2 infection in pigs, transthyretin showed a negative acute phase response. CRP is the primary APP in canines, along with haptoglobin and SAA, whose concentrations are elevated in bacterial infections, inflammation, and stress.
APPs have been proposed as useful indicators for social stresses, such as transportation, mixing, and abrupt weaning, which elicit an acute phase response, especially in young ruminants (Gupta et al., 2007; Herskin et al., 2007). The serum concentrations of ruminant APPs show considerable differences from other animal species, with haptoglobin being the primary ruminant APP. Its already high serum concentration of 20 mg/L can be increased up to 2 g/L within 2–3 days in response to infection, inflammation, and stress (Ceciliani et al., 2012). Increases in haptoglobin levels have been observed in conditions like fatty liver syndrome and stress induced by parturition, starvation, or transportation (Murata et al., 2004; Petersen et al., 2004). Studies on stress-induced variations in APPs in cattle indicated that the concentrations of other APP, such as SAA and fibrinogen, also increase in cattle, especially when exposed to chronic inflammation and associated stress. These APPs were also proposed as indicators of transportation and commingling induced stress in calves (Conner et al., 1998; Arthington et al., 2003). Later, Lomborg et al. (2008) reinforced the findings that APPs, especially SAA and haptoglobin, are potent markers to evaluate transportation or mixing-induced stress in both calves and adult cattle.
Haptoglobin has an anti-oxidant role, especially in ruminant species, preventing them from undergoing oxidative stress, in addition to its standard immune functions including free hemoglobin scavenging and anti-inflammatory actions (Ceciliani et al., 2012). Haptoglobin exerts its anti-oxidant role by stabilizing ferric irons to prevent oxidative damage to hemoglobin. Thus, haptoglobin can protect albumin from oxidative damage by inhibiting the exchange of heme between hemoglobin and albumin (Lim et al., 1998; Buehler et al., 2009). It can also prevent lipid peroxidation damage of vital tissues, particularly in the kidney (Melamed-Frank et al., 2001). Haptoglobin scavenges nitric oxide through rapid and irreversible bonding, thereby limiting its bioavailability and preventing oxidative damage from reactive nitrogen species (Rother et al., 2005).
The well-established influence of APPs upon stimuli resulting from infection, inflammation, and proinflammatory cytokine-mediated responses paved the way for research into their involvement in bovine medicine as markers of various diseases (Eckersall and Bell, 2010). Since certain APPs were detected in milk, their influence has been studied extensively in bovine mastitis, a major bovine inflammation causing considerable economic losses. Haptoglobin and SAA are synthesized in the bovine mammary epithelium, and the substantial increase in their secretion into milk was observed during mastitis (Eckersall et al., 2001). Increases in the milk concentration of the mammary isoform of SAA in ruminants (M-SAA3) have been reported in cows and ewes with mastitis (Winter et al., 2003; Nielsen et al., 2004; Jacobsen et al., 2005; Eckersall and Bell, 2010). In cows with experimentally induced mastitis (using specific microbes, such as Staphylococcus uberis), the level of M-SAA3 in milk reached a peak at 6 h, and haptoglobin reached a peak at 10 h after infection (Pedersen et al., 2003; Nielsen et al., 2004). There is an increase in APPs, particularly SAA and haptoglobin in chronic respiratory diseases in calves; in sick calves, concentrations of these parameters were significantly higher in died or euthanized calves compared with calves in improved health status during therapy (Tothova et al., 2010).
SAA has been found to increase in sera of foals during infections with bacteria, i.e., Rhodocoocus equi and Streptococcus equi and viruses, i.e., H3N8 influenza virus and serotype 1 herpes virus. There was also a statistically significant correlation between SAA serum concentration and severity of clinical signs of the respiratory disease as well as the rectal temperature of the infected animals (Jain et al., 2011).
Following Streptococcus suis type 2 infection in pigs, transthyretin (a serum protein which is a negative acute phase reactant) showed a negative acute phase response with serum concentrations reaching a significantly lower level at 2 days following infection compared to serum samples of the healthy pigs (Campbell et al., 2005).
Another potent APP, lipopolysaccharide-binding protein (LBP) which is a liver-derived acute phase protein, has also been reported to show increased concentration in milk during bovine mastitis compared with normal conditions (Zeng et al., 2009). Bovine APPs, such as SAA and haptoglobin, are elevated in the serum during other extra-mammary inflammations, e.g., metritis and interdigital dermatitis. During these extra-mammary inflammation or degenerative changes, no significant alterations in the concentration of these APPs in milk were observed, indicating their specificity in assessing mammary inflammation (Ceciliani et al., 2012). These observations indicated strongly that milk APPs are potent and reliable biomarkers in bovine medicine for the most endemic condition, mastitis, particularly attention subclinical mastitis, which can barely be detected from clinical evidence.
In addition, the effect of transport stress on APPs gene expression in turkey (Meleagris gallopavo) revealed upregulation of α1-acid glycoprotein (AGP) and CRP and downregulation SAA and PIT54 in the liver (Marques et al., 2016).
Modern studies are exploring the roles of APPs in both health and productivity, and simultaneously being correlating to stress (Joshi et al., 2018; Miglio et al., 2018). Their diverse roles have enabled them to be potential candidates in theronostics, disease pathogenesis and progression, and prevention. They have been associated with the diagnosis of both infectious and non-infectious diseases including viral diseases (Reczynska et al., 2018), bacterial diseases (tuberculosis) (Santos et al., 2019), cardiovascular diseases (Asleh et al., 2018), acute pulmonary embolism (Zhang Y. X. et al., 2018), pulmonary arterial hypertension (Nakamura et al., 2018), respiratory diseases (Joshi et al., 2018), metabolic disorders in obese children and adolescents (Cura-Esquivel et al., 2018), vascular disorders (Wang S. et al., 2018), chronic inflammatory and neurodegenerative diseases (Luan and Yao, 2018).
These findings revealed the ubiquitous nature of APPs, such that their applications should not be restricted to inflammatory and infectious disease progression and diagnosis. They could be used in a wider range of applications, including monitoring and prognosis of treatment efficacy in humans and animals, and evaluation of the health status of production animals for optimum output; thereby ensuring overall well-being from a public health perspective. However, properly standardized and systematically validated APP assays, such as the Acute Phase Index, are warranted in both the human and animal clinical sectors.
The Role of Interleukin-22 in the Expression of APR Proteins
Interleukin-22 (IL-22) is implicated in the expressions of acute phase proteins (Liang et al., 2010). IL-22 induced acute-phase protein expression from a HepG2 hepatocellular carcinoma-derived cell line and the liver, with a subsequent increase in the circulating SAA levels (Wolk et al., 2004). IL-22 induced rapid hepatic expression of chemokine ligand, i.e., CXCL1, associated with transient mobilization of neutrophils for systemic ramifications. IL-22 is produced by a subset of T cells, including TH17 and NKT cells. The IL-22 receptor is a heterodimer composed of IL-22R1 and IL-10R2. The expression of IL-22R1 is limited to epithelial and pancreatic acinar cells (Xue et al., 2012). By contrast, IL-10R2 expression is ubiquitous (Sabat et al., 2014; Dudakov et al., 2015). In a recent finding in a mouse model of colitis, an increased expression of serum amyloid A3 has been shown to play a protective role against acute injury through TLR2-dependent induction of neutrophil IL-22 expression (Zhang G. et al., 2018). Expression of anti-microbial peptides for anti-microbial action has also been credited to IL-22 (Narazaki and Kishimoto, 2018).
The detailed mechanism of the role of IL-22 in the expression of acute phase response proteins is shown in Figure 4. IL-22 acts on the cells of various organs, including pancreatic cells, liver cells, intestinal epithelial cells, epidermal keratinocytes, respiratory epithelial cells, and synovial fibroblasts (Sabat et al., 2014). In epithelial cells, IL-22 induces the production of anti-bacterial proteins, including β-defensin 2 (BD2), BD3, S100A7, S100A8, S100A9, lipocalin 2, matrix metalloproteinase 1 (MMP1), and MMP3. In hepatocytes and pancreatic cells, IL-22 increases the expression of B-cell lymphoma 2 (Bcl-2), Bcl-xL, myeloid cell leukemia sequence 1 (MCL-1), cyclin D1, p21 (a negative regulator of cell cycle), and CDK4. Specifically, in hepatocytes, it promotes the expression of haptoglobin, LBP, and SAA. In synovial fibroblasts, IL-22 induces CC-chemokine ligand 2 (CCL2) and receptor activator of NF-κB ligand (RANKL) (Sabat et al., 2014). IL-22 expression can act as a sensitive biomarker for identification of allergic children vulnerable to polychlorinated biphenyls (Tsuji et al., 2012).
Figure 4.
IL-22 signaling pathway for expression of acute phase response proteins. 1. IL-22 receptor is a heterodimer of IL-22R1 and IL-10R2. Initially IL-22 binds to IL-22R1. 2. Upon binding, conformational change in IL-22 enhances its affinity toward IL-10R2. 3. leading to formation of heterodimeric receptor intracellularly, IL-22R1 is associated with JAK1 and STAT3 (STAT3 is recruited through tyrosine-independent recruitment) and IL-10R2 is associated with tyrosine kinase 2 (TYK2). 4. Binding of ligand with receptor initiates the phosphorylation of JAK1 and TYK2. 5. Receptor bound STAT3 is phosphorylated by JAK1. 6. Phosphorylation of STAT3 leads to dimerization of STAT3. 7. Dimerized STAT3 translocates to nucleus; in nucleus, it binds to response elements and regulate associated proteins. 8. STAT3 binds to different genes coding for acute phase proteins by different cells, viz. to viz. a). Epithelial cell (β-defensin 2, β-defensin 3, lipocalin 2, MMP1 and MMP3, S100A7, S100A8, S100A9 b). tracheal epithelial cells (CXCL5); c). synovial fibroblast (CCL2/RANKL); d). hepatic and pancreatic cells (Bcl-2, Bcl-xL, MCL-1, Cyclin D1, p21, CDK4).
So, these hormonal, enzymatic or protein biomarkers serve as indicators of inflammation, immunity, stress or related diseases. An overview of these biotic stress markers along with their detection methods is presented in Table 1.
Table 1.
Biotic stress markers, the associated ailments and their detection methods.
| S. No. | Name of molecule | Molecule prelude | Functions of the molecule | Marker to ascertaining | Type of stress | Diagnosis method | Reference(s) |
|---|---|---|---|---|---|---|---|
| 1. | Malondialdehyde (MDA) | Present in plasma samples; positively correlated to stress | Highly cytotoxic, mutagenic, inhibitors of various enzymes, inhibitor of DNA replication | Ischemic conditions, ocular pathologies, hypertension, Cancer, Alzheimer's disease, respiratory disease | Oxidative stress | Thiobarbitoric acid (TBA) assay | Sordillo and Aitken, 2009; Singh et al., 2013; Wispriyono et al., 2016; Peña-Bautista et al., 2019 |
| 2. | Protein carbonyl groups | Chemically stable moieties generated through oxidative cleavage of proteins | Lipid oxidation of cell membrane results in formation of reactive aldehydes and ketone called protein carbonyl groups | Increased levels observed in Alzheimer's disease (AD), rheumatoid arthritis, diabetes, sepsis, chronic renal failure, and respiratory distress syndrome | Oxidative stress | Spectrophotometric assay, ELISA, and one-dimensional or two-dimensional electrophoresis followed by Western blot assay | Dalle-Donne et al., 2003 |
| 3. | Isoprostanes | Prostaglandin-like compounds present in plasma, urine or vital tissue samples, formed via the free radical-mediated oxidation of arachidonic acid | Reliable in-vivo marker of lipid peroxidation | Coronary heart disease, obesity, cancer, genetic disorders, chronic obstructive pulmonary disease (COPD), and acute coronary syndrome | Oxidative stress | Gas chromatography–mass spectrometry, RIA, ELISA | Musiek et al., 2005; Smith et al., 2011; Ferroni et al., 2017; Su et al., 2019 |
| 4. | Blood urates | Final product of metabolic breakdown of purine nucleotides | A correlation between blood uric acid level and risk for complications | Gout, kidney stones, cardiovascular disease (CVD), and type 2 diabetes, Parkinson's disease | Oxidative stress (diagnostic and prognostic stress) | Near-infrared (NIR) spectroscopy (use of infrared wavelengths between 1,400 and 1,700 nm) | Cipriani et al., 2010; Stamp et al., 2011; Kim, 2015 |
| 5. | 3-Nitrotyrosine peptides | Reactive nitrogen intermediates attack on protein bound tyrosine to form 3-nitrotyrosine peptides; a biomarker of nitrogen free-radical species | Expose tissue to reactive nitrogen species | Alzheimer's, Parkinson's, multiple sclerosis, stroke, and cardiovascular (atherosclerosis, myocardial infarction, coronary artery disease, hypertension, and diabetic vasculopathy) diseases | Nitroxidative stress | HPLC Separation and Electrochemical (EC) Detection | Malinski, 2007; Nuriel et al., 2008; Radi, 2013 |
| 6. | Liver-type fatty acid-binding protein (L-FABP) | Express in the proximal tubules of the human kidney participating in fatty acid metabolism | Reduce cellular oxidative stress through binding to fatty acid oxidation products, and limiting the toxic effects of oxidative intermediates | Acute kidney injury | Oxidative stress | Sandwich ELISA kit | Ferguson et al., 2010; Kamijo-Ikemori and Kimura, 2015 |
| 7. | Endothelin-2 | A potent vasoconstrictor | Mainly secreted from endothelial cells | Essential hypertension, hepatorenal dysfunction | Oxidative stress | EIA kit/PCR | Dhawan et al., 2014; Qureshi et al., 2016 |
| 8. | Advanced glycation end-products (AGE) | Nucleic acids, proteins or lipids glycated as a result of exposure to reducing sugars | Downstream mediators of tissue injury | Diabetic retinopathy, nephropathy, cataract, neuropathy, cardiomyopathy | Oxidative stress | Fluorescence high-performance liquid chromatography | Calabrese et al., 2007; Singh V. P. et al., 2014 |
| 9. | Glutathione peroxidase | Antioxidant selenoprotein enzyme, directly concerned with reduction of free radicals, reducing the oxidative attack | catalyzes the oxidation of glutathione (GSH) | Cancer and cardiovascular disease, systemic lupus erythematosus and anti-phospholipid syndrome | Functional indicator of selenium status | Colorimetric assay | Gheita and Kenawy, 2014; Barry-Heffernan et al., 2019 |
| 10. | Superoxide dismutase | Metalloenzyme against reactive oxygen species (ROS) regulating the bioactivity of nitric oxide | Concerned with the direct reduction of ROS into metabolic water and oxygen molecules, thereby preventing the oxidative damages of tissues | Cardiovascular disease, atherosclerosis, ischemia–reperfusion injury | Oxidative stress | ELISA kits using WST method | Fukai et al., 2002; Chen et al., 2018 |
| 11. | Heme oxygenase-1 (HO-1) | An increase in HO-1 protein occurs during pro-inflammatory conditions | Up-regulated during selenium (Se) deficiency and suggestive of its role as anti-oxidant compensating for the loss of Se-dependent antioxidants | Ischemia–reperfusion, graft rejection and atherosclerosis | Oxidative stress | ELISA | Trigona et al., 2006; Rücker and Amslinger, 2015 |
| 12. | Catalase | Anti-oxidant enzyme | Decompose hydrogen peroxide to water and oxygen | Diabetes mellitus, hypertension, and vitiligo, acatalasemia | Oxidative stress | Formation of a stable and colored carbonato-cobaltate (III) complex | Góth et al., 2004; Hadwan, 2018 |
| 13. | Myeloperoxidase | Heme-containing peroxidase expressed mainly in neutrophils | In the presence of H2O2 and halides, formation of reactive oxygen intermediates, including hypochlorous acid | Diabetes/diabetic retinopathy, obesity, atherosclerosis, cardiovascular diseases | Inflammation | ELISA | Nicholls and Hazen, 2005; Khan et al., 2018 |
| 14. | Heat shock proteins (HSPs) | Molecular chaperonins | Stress induced protein denaturation is corrected by refolding and remodeling | Infectious diseases and autoimmune diseases | Indicator of short-term stress like thermal stresses, osmotic stresses, toxicity due to heavy metals, ecological stress due to pollutants | ELISA | Hecker and McGarvey, 2011; Khandia et al., 2017; Tang T. et al., 2018; Silva et al., 2019 |
| 15. | Cortisol | Secretion is regulated by the hypothalamo-pituitary-adrenocortical (HPA) system | Stressed conditions increase salivary and blood cortisol | Cardiovascular, metabolic, immunologic, and homeostatic functions | Generalized stress | Competitive lateral flow immunoassay | Ivković et al., 2015; Apilux et al., 2018 |
| 16. | Acute phase proteins (APPs) | Innate immune proteins, secreted by hepatocytes | APPS are increased or decreased in response to inflammation | Prostate cancer, bronchopneumonia, chronic inflammation | Apart diseases, environmental stress | RIA and ELISA | Jain et al., 2011 |
| 17. | Copeptin | Polypeptide derived from the hypothalamo-pituitary axis-system, as a pre-pro-hormone along with vasopressin and neurophysin II. Employed for assessing the individual stress level in comparison to cortisol. Prognostic accuracy of copeptin in acute illness like sepsis, pneumonia, lower respiratory tract infections and stroke has been analyzed successfully | 39-amino acid glycopeptide | Acute myocardial infarction, heart failure, acute exacerbation of chronic obstructive pulmonary disease, lower respiratory tract infections, acute dyspnea, sepsis, hemorrhagic and septic shock, diabetes mellitus, metabolic syndrome, hyponatremia, vasodilatory shock, diabetes insipidus, autosomal dominant polycystic kidney disease (ADPKD), intracerebral hemorrhage, ischemic stroke and traumatic brain injury | Even mild to moderate stress situations alter copeptin level | Sandwich immunoassay | Morgenthaler et al., 2008; Katan and Christ-Crain, 2010; Dobsa and Edozien, 2013 |
However, their evaluation and interpretation is cumbersome and varies in various conditions or diseases. Sampling, determination, or expression process is relatively tedious. Further, there probable specificity to stress or disease process less likely determines reliability to be used for constant accuracy.
Since biomarkers of stress or related diseases usually vary from condition to condition or organ to organ, efforts are being made to identify a specific and sensitive biomarker that can remarkably diagnose a particular condition or may be characteristic to a group of conditions (Singh et al., 2018). Besides, ease of investigation, safe sampling, and accurate determination can add to the reliability of the biomarker. Though yet in infancy and early stages of investigation, still few specific samples or organ oriented biomarkers are being explored for uniformity and accuracy including salivary, renal, sweat, tears, breath or feces biomarkers. Thus, a detailed account of these salivary or renal biomarkers will be helpful in understanding importance and extent of the diagnostic circumference (Chou et al., 2015; Drozdz et al., 2016; Mortha et al., 2018; Silva et al., 2019).
Stress Biomarkers in Saliva
Saliva provides an optimum and non-invasive biological source for the quantitative and qualitative assessment of chemical and physiological mediators associated with various conditions, such as stresses, diseases, and injury (Rai and Kaur, 2011). The role of saliva as a mediator can be elucidated from its components, such as digestive enzymes (α-amylase), secretory immunoglobulins for mucosal defense (secretory IgA), innate immune components, such as anti-microbial peptides (lysozyme), and signaling molecules (such as steroidal and peptide hormones) (Wong, 2006; Turner and Ship, 2008). Recent technical advances in the processing and evaluation of salivary components have produced reliable results that increase the possibility of exploiting this biological source, which is comparatively safer, cheaper, and less invasive than its traditional counterparts, such as blood, urine, and peritoneal fluid (Groschl, 2008). Studies suggest that salivary components can be analyzed accurately using specific and sensitive immunological and biochemical techniques, such as RIA, ELISA, and chromatography (Ivković et al., 2015). Reports suggest an intense correlation between exposure to stress and the level of various salivary components, including cortisol, secretory immunoglobulins, enzymes like α-amylase, and chromogranin A. All of the above-mentioned salivary components can be considered as salivary biomarkers of stress in animals (Takai et al., 2004; Takatsuji et al., 2008; Clow et al., 2010). Being a widely accepted salivary biomarker of stress, rapid quantification of cortisol in saliva was investigated as a non-invasive measure to check modulation in stress responses. Apilux et al. (2018) reported the development of a lateral flow immunoassay facility using cortisol-BSA conjugate containing gold nanoparticle labeling in a silver enhancement system to detect cortisol associated with stress from saliva. In addition, oxidative stress markers, including ROS and their mediators, are reported to have been evaluated in salivary samples (Su et al., 2009; Gümüş et al., 2015). Chromogranin A and haptoglobin in saliva are potent candidates for assessing the stress of pigs caused by restraining (Huang et al., 2017).
So far salivary biomarkers have been found to play profound role in diagnosis of many diseases or stressful conditions including cancers (Arantes et al., 2018; Kaur et al., 2018; Khurshid et al., 2018), liver diseases (Abe et al., 2018; Morán and Cubero, 2018), kidney diseases (Maciejczyk et al., 2018b), neurological (Farah et al., 2018) and cardiovascular diseases (Gohel et al., 2018), psoriasis (Asa'ad et al., 2018), systemic lupus erythematosus (Stanescu et al., 2018), and rheumatoid arthritis (Äyräväinen et al., 2018). In one of the very recent review, it has been enumerated that majority of the biomarkers in saliva have diagnostic potential for neoplasms, followed by detection of metabolic disorders and least for systemic disorders (Mortha et al., 2018). A recent study in humans during enduring hot temperature indicated significantly higher levels of biomarkers, such as α-amylase, cortisol, and total proteins in saliva and suggested intensified stressful responses upon exercise during such conditions (Silva et al., 2019). The most commonly used method for estimating these biomarkers is enzyme-linked immunosorbent assay, the most common analytes are immunoglobulins; however, in the recent past, proteomic approaches have enabled discovery of novel salivary biomarkers (Mortha et al., 2018).
Table 2 summarizes the prominent salivary biomarkers associated with stress along with salient research findings indicating their diagnostic potential. Figure 5 depicts various stresses affecting the salivary stress biomarkers.
Table 2.
Salivary biomarkers and assessment of stress.
| S. No. | Salivary marker used to assess the stress | Subject(s) | Age group | Design to evaluate the stress | Statistics used/outcome of study | Reference |
|---|---|---|---|---|---|---|
| 1. | Salivary chromogranin A | 20 males | 21–24 years | White noise at 90 dB for 15 min with 15-min-rest periods before and after noise exposure | Friedman's test (p = 0.001) | Miyakawa et al., 2006 |
| 5 children | 3–5 years | Dental treatment followed by a questionnaire | Two sided Wilcoxon signed rank test (p < 0.05) | Mitsuhata et al., 2012 | ||
| Professional elite 9 swimmers (6 men and 3 women) | 22 ± 2 and 22 ± 4 years, for men and women, respectively | Before and after competition level of stress marker in success and failure athlete | Mann-Whitney comparisons (p < 0.05) | Chennaoui et al., 2016 | ||
| 40 patients | 25–60 years | Test of patients with aggressive periodontitis before and after non-surgical periodontal therapy | post hoc test (p < 0.001) | Lihala et al., 2019 | ||
| 62 (34 males, 28 females) |
57.6 ± 13.4 | To fill the SF-36 questionnaire indicative of quality of life (QOL)including the parameters of Peak Expiratory Flow, role physical and role emotional in patients with Bronchial Asthma | Kruskal-Wallis rank test (p < 0.05) | Hoshino et al., 2008 | ||
| 56 preprimary school students | 2.5–5 years | Stress marker correlation with self-structured preprimary stress questionnaire (PPSQ) | One-way ANOVA (p < 0.001) | Jena and Mohanty, 2016 | ||
| 2. | Salivary IgA and lysozyme | 132 female emergency department and general ward nurses | Not given | Stress marker correlation with mental health professionals stress scale (PSS) | Test not given (p = 0.001) | Yang et al., 2002 |
| 3. | Salivary IgA | 514 nurses | 22–43 years | 33 data points collected for immunological measures to find out association with stress and job in a voluntary job stress survey | ANOVA (p < 0.01) | Lee et al., 2010 |
| 130 dental students | 22.4 ± 2.5 | A 38-item dental environmental stress (DES) questionnaire and a 4-point perceived stress scale to identify self-perceived stress levels (stress due to academic pressure) | A two sample independent t-test, Scheffe's test, partial correlation coefficient (Pearson's r = −0.30, p = 0.0001) |
Ng et al., 2004 | ||
| 4. | Salivary amylase and cortisol | 20 participants | 20–44 years | Exposure to naturalistic traffic noise samples containing 75 dB (LA, eq) for 20 min via a loudspeaker system | Test not given (p < 0.01) | Wagner et al., 2010 |
| 5. | α-amylase | 30 healthy young men | 19–28 years | Participants subjected to Trier Social Stress Test (TSST) consisting of a mental arithmetic task and free speech in front of an audience | Analyses of variance (ANOVA) (p < 0.001) | Nater et al., 2006 |
| 83 healthy volunteers | 20–27 years | Stress induced by showing scenes of injection into the eyeball and incision of the cornea with scissors for 15 min | Unpaired t-test; Pearson's correlation coefficient (r); Positive correlation between the amylase level and the State-Trait Anxiety Inventory (personal anxiety test) score (r = 0.535; p < 0.01) | Takai et al., 2004 | ||
| 100 subjects (50 chronic stressed + 50 healthy) | Over 18 years | Subjects were asked to fill a psychometric questionnaire | Non-parametric Mann-Whitney U Test (p = 0.002) | Vineetha et al., 2014 | ||
| 6. | Cortisol | 170 children | 11–14 years | Revised Children's Manifest Anxiety Scale (RCMAC) Questionnaire was filled to evaluate child anxiety in connection to oral environment and its connection to the general psychological status of children | T-standard evaluation (X50; SD10) by linear transformation of the data, step algorithm and Single correlations (p < 0.05) | Rashkova et al., 2010 |
| 20 children | 4–8 years | Evaluation of fear and pain stress during dental procedure (10 min before, during the procedure, and 30 min after excavation of caries with rotary hand piece an tooth extraction) | Paired t-test, two independent sample t-tests, and analysis of variance (ANOVA) (p < 0.05) | Patil et al., 2015 | ||
| 30 patients with clinically and histopathologically proven cases of oral lichen planus with matched healthy individual | 19–69 years | Assessment of intensity of burning sensation was determined using a Visual Analog Scale with psychological evaluation was done with depression, anxiety, and stress scale | Student's t-test (p < 0.001) | Shah et al., 2009 | ||
| 1,755 adolescents | 13–18 years | The National Comorbidity Survey-Adolescent Supplement questionnaire to measure stress reactivity in adolescents with psychiatric disorders | Quantile regression models; adolescents with mood and/or anxiety disorders have high cortisol levels | Brown, 2016 | ||
| 65 rescue workers | 34–59 years | Workers subjected to Psychiatric self-rating scale General Health Questionnaire (GHQ-28) measuring psychiatric health, Impact of Events Scale (IES) and Post-Traumatic Symptom Scale (PTSS) measuring post-traumatic symptoms | Non-parametric Spearman rank correlation coefficients; correlation between evening salivary cortisol and anxiety (p < 0.005), depressive symptoms (p < 0.01), post-traumatic symptoms with avoidance behavior (p < 0.005) | Aardal-Eriksson et al., 1999 | ||
| 7. | Salivary lysozyme | 17 participants in final year examination (7 males + 10 females) | 20–26 years | Sample taken before and after the examination and assessed for study | paired student's t-test (p < 0.05) | Perera et al., 1997 |
| 8. | Chromogranin A and salivary lysozyme, Salivary amylase | 26 female professors | 7.2 ± 3.0 years | State-trait anxiety inventory (STAI) was used to assess personal anxiety while delivering lecture in front of 200 students | Two-way repeated measures ANOVA; Salivary lysozyme (p < 0.05); Chromogranin A (p < 0.05); Salivary amylase (p < 0.05) | Filaire et al., 2010 |
| 9. | Chromogranin A and IgA | 15 female students appearing in nursing exam | 21–26 years | Sample taken 10 min before exam, and immediately after the exam and 2 h post-exam | Student's t-test (p < 0.05) |
Figure 5.
Various stresses affecting the salivary stress biomarkers: cortisol, chromogragranin A and α-amylase are increased whilst salivary IgA and lysozyme are decreased with an increase in level of stress.
Renal Stress Biomarkers
Blood urea nitrogen (BUN) and creatinine are the most commonly used biomarkers to assess the functional status of the kidney and can be measured easily and inexpensively in serum. Urea and creatinine are the normal metabolic end products of dietary and tissue-derived proteins in healthy humans and animals. They are cleared from the circulation via the kidneys. Even though they are potent markers for assessing renal insufficiency in mammals, a range of serum levels reflecting different pathophysiological statuses resulting from many non-renal etiologies have been observed (Tesch, 2010). Urea and creatinine levels in the serum are influenced by non-renal causes, such as dietary intake of protein, dehydration due to temperature and humidity stresses, defective liver function, bleeding in the gastrointestinal tract, and chronic steroid use. BUN is customarily quantified in serum by an enzyme/oxidation-reduction assay; however, BUN assays often misjudge renal function because of interfering chromogens (Waikar and Bonventre, 2006). Different assays are employed to quantify creatinine levels in serum and urine, such as the creatininase method and HPLC; however, the Jaffe rate reaction is used most commonly because it is cheap and easy to perform (Schwartz et al., 2009).
Renal oxidative stress responses can also be measured using serum and urine biomarkers in human patients and animal models. One such renal oxidative stress marker is 8-OH-dG, which is a metabolically stable product of the oxidation of guanine from nucleic acids. The 8-OH-dG level increases in urine following renal oxidative stress, which can be detected by standard enzyme immunoassays (Dounousi et al., 2006). Cystatin-C, a cysteine protease inhibitor, is another reliable biomarker to assess renal function. Cystatin-C is released regularly into the circulation from nucleated cells and is reabsorbed normally by kidney tubules, followed by its catabolism (Curhan, 2005). Thus, the increased concentration of cystatin-C in blood and serum samples is highly sensitive to assess renal impairment and compared with creatinine, it is a very potent indicator of acute renal injuries because of its shorter half-life (Herget-Rosenthal et al., 2004). Although its quantification can be affected by steroid therapy and thyroid dysfunctions, immunonephelometry and enzyme immunoassays can be used effectively to measure the serum cystatin-C concentration.
Increased lipid peroxidation during oxidative stress leads to the production of several chemo-mediators, in which 8(F2a)-isoprostane and 4-hydroxy-2-nonenal can be detected not only in serum but also in urine samples by HPLC or immunoassays. Their increased serum concentrations are indicative of chronic renal disorders (Calabrese et al., 2007; Tesch, 2010). Besides these conditions, urinary excretion levels of 8-iso-prostaglandin (PG) F2α has also been described for a strong association with coronary problems and diabetes. Higher urinary 8-iso-PGF2α levels are being correlated to an increase in necrotic plaque formation and coronary culprit lesions in diabetes patients, especially with acute coronary problems (Su et al., 2019). Also, renal oxidative stress can be measured using markers, such as 3-nitrotyrosine peptides, which are stable nitrated peptides produced through the action of peroxynitrites upon protein tyrosine residues (Radi, 2013). The effectiveness of 3-nitrotyrosine peptides, present in urine and serum samples, as potential biomarkers of renal oxidative and nitrosative stress, has been reported in several studies (Nemirovskiy et al., 2009). Their levels can be determined accurately using liquid chromatography and mass spectroscopy (Radabaugh et al., 2008).
Certain modified proteins, such as advanced glycation end products (AGEs) are increased in the circulation as a consequence of oxidative stress, especially in diabetes and uremia. AGEs, together with pentosidine, can also be deposited in kidneys, resulting in renal cellular dysfunction and/or renal damage (Calabrese et al., 2007). Thus, elevated levels of these compounds, which can be assessed by ELISA/HPLC, are effective markers of oxidative stress and help to predict the development of nephropathic conditions in diabetic patients. Liver-type fatty acid-binding protein (L-FABP), released by proximal tubular cells, has been identified as a potent marker of hypoxic stress-induced renal damage. Increased urinary secretion of L-FABP correlates with a declining renal function that might be caused by acute or chronic renal tubular injury (Portilla et al., 2008; Ferguson et al., 2010; Kamijo-Ikemori and Kimura, 2015).
Potent biomarkers for sensitizing renal injury include albumin, N-acetyl-β-D-glucosaminidase, kidney injury molecule-1, and exosomal transcription factors (Coca et al., 2008). The excretion rate of albumin into urine is considered as a routine early biomarker to assess the renal injury, such that an increase in the urinary albumin level (albuminuria) indicates the possibility of renal dysfunction (Meijer et al., 2010). N-acetyl-beta-D-glucosaminidase is a proximal renal tubule-derived lysosomal enzyme that has been identified as a sensitive marker for both acute and chronic renal injury (Han et al., 2008; Jungbauer et al., 2011). Potential sourcing of urinary biomarkers that can be employed for the improved diagnostic tests is identified as pathways involved in kidney damage, oxidative stress and low-grade inflammatory changes associated with atherosclerosis/vascular damage (Matheson et al., 2010). Several studies have revealed that in case of chronic kidney diseases the level of various stress markers/oxidative stress markers, such as products of oxidation of protein (advanced products), isoprostanes, and malondialdehyde increase along with a reduction in the concentration of anti-oxidants. Such markers are valuable to detect atherosclerosis (and the rate of its progress) associated with disturbed kidney functions (Gosmanova and Le, 2011; Sung et al., 2013; Tucker et al., 2013; Drozdz et al., 2016).
Biomarkers of renal dysfunction, such as transferrin, type IV collagen, N-acetyl-beta-D-glucosaminidase, etc., inflammatory markers, such as orosomucoid, tumor necrosis factor-alpha, monocyte chemoattractant protein-1 (MCP-1), vascular endothelial growth factor, as well as oxidative stress markers, such as 8-OH-dG can be superior candidates in the detection of renal disorders including nephropathy and associated cardiovascular disease (Matheson et al., 2010; Chou et al., 2015). Valuable biomarkers indicative of acute kidney injury (AKI) are insulin-like growth factor-binding protein 7 (IGFBP7), tissue inhibitor of metalloproteinases-2 (TIMP-2); their levels in urine need to be monitored on urgent basis (Kimmel et al., 2016). Another proximal renal tubule expressed transmembrane protein is kidney injury molecule-1; its increased concentrations in urine, which can be detected effectively using immuno-enzymatic and immunochromatographic techniques, correlate highly with proximal renal tubular injury (Van Timmeren et al., 2007; Vaidya et al., 2009). Several pathological invasions activate the expression of exosomal transcription factors (ETFs) that are contained in the exosomal vesicles of renal tubular epithelial cells. Assessment of these ETFs in urine by transcriptome sequencing and Western blotting could be effective to diagnose acute renal injuries, as well as in monitoring disease progression (Zhou et al., 2008). Taken together, the accumulated biochemical and immunological data for stress-induced renal dysfunctions and associated biomarkers provide a sound foundation for further study of the molecular mechanisms of disease progression, prognosis, and therapeutic evaluation.
Certain biomarkers including estimated glomerular filtration rate (eGFR), serum creatinine, blood urea, cystatin-C, and proteinuria or albuminuria can be employed for diagnosis of diabetic nephropathy (DN) (Campion et al., 2017; Moledina, 2019). Urinary heat shock protein 72 (uHSP72) was recently found to be a novel biomarker for detection of DN and was also known to be a biomarker for acute kidney injury (El-Horany et al., 2017). Other novel renal biomarkers are neutrophil gelatinase-associated lipocalin, urinary activin A, kidney injury molecule-1, monocyte chemotactic peptide-1, IL-18, netrin-1, cycle arrest markers, endogenous ouabain, selenium-binding protein 1, and BPIFA2 marker (Arsalan et al., 2018; Beker et al., 2018; Takahashi S. et al., 2018; Yimer et al., 2018). An overview of renal stress biomarkers to assess the status of the renal system is depicted in Figure 6.
Figure 6.
An overview on renal stress biomarkers: various biomarkers, such as urea, creatinine, 8-hydroxy-2-deoxyguanosine, cystatin-C, and others are used to assess the status of renal system.
Hence, salivary and urinary biomarkers have found promising scope for future applications in biomedical science in diagnosing stress related and pathophysiological diseases and disorders. Being natural secretory or excretory products and not involving any invasive protocols makes diagnostic procedure convenient besides overcoming ethical issues of sampling or investigation procedures. Though numerous biomarkers have already been identified in these natural secretions and many proving beneficial of diagnostic value, still much needs to be investigated for covering broad range problems with accuracy and repeatability so that they can be utilized in stresses, diseases or disorders. Many may prove effective as prognostic and therapeutic markers enabling forecasting or progression of the disease and monitoring the effect of therapy on the management of disease as discussed ahead.
The Utility of Biomarkers in the Clinical Illness: Prognosis and Therapy Guidance/Selection
Various critical molecular signatures have been identified in relation with stress associated ailments clinical, but for their recommendation as a unique biomarker for each condition depends on the clinical relevance as well as cost-effectiveness, sensitivity, and specificity of diagnostic tools. Table 3 depicts an overview of various biomolecules partaking diagnostic/prognostic values along with their association with various ailments. Scientific advances mainly paved for the exploration of oxidative stress related biomarkers for using clinically, but nowadays more focus are being paid on the use of non-invasive biological samples wherein numerous studies have proposed the use of saliva and urine stress biomarkers in the prognosis and diagnosis of infectious, non-infectious and metabolic diseases (Frustaci et al., 2012; Lindsay and Costello, 2017).
Table 3.
Overview of various biomolecules having diagnostic/prognostic values along with their association with various ailments.
| S. No. | Molecular marker | Molecule category | Vita of the molecule | Association with ailment | Marker for diagnosis/prognosis | Detection module | Reference(s) |
|---|---|---|---|---|---|---|---|
| 1. | Glutamate | Mitochondrial phosphate-dependent glutaminase converts glutamine to glutamate and ammonia | Essential to protein synthesis, muscle growth, regulation of acid-base balance in the kidney, ureagenesis in the liver, hepatic and renal gluconeogenesis, oxidative fuel for the intestine and cells of the immune system, precursors of neurotransmitter synthesis, of nucleotide and nucleic acid synthesis and of glutathione production | Visceral obesity and associated metabolic alterations | Diagnostic marker for visceral obesity and altered metabolism | Targeted metabolomics using the Absolute IDQ kit p180 | Maltais-Payette et al., 2018 |
| 2. | Chromogranin-A (CgA) | Present in the secretory granules of most endocrine and many neuroendocrine cells | Considered to serve as precursor molecule for biologically active peptides | Neuroendocrine tumor | Diagnostic and prognostic marker for survival | Solid-phase, two-site immuno-radiometric assay, the CGA-RIA kit | Deftos, 1991; Bílek et al., 2019 |
| 3. | Urinary 8-hydroxy-2-deoxyguanosine (8-OH-dG) | An oxidized nucleoside of DNA | Excreted in the urine upon DNA repair | Cancer, atherosclerosis, diabetes, diabetic nephropathy and retinopathy | Diagnostic and prognostic marker | Alkaline comet assay | Wu et al., 2004; Franken et al., 2017 |
| 4. | Liver-type fatty acid-binding protein (L-FABP) | Express in the proximal tubules of the human kidney participating in fatty acid metabolism | Reduce cellular oxidative stress through binding to fatty acid oxidation products, and limiting the toxic effects of oxidative intermediates | Acute kidney injury | Diagnostic marker effective in estimating severity of renal injury/oxidative stress biomarker | Sandwich enzyme-linked immunosorbent assay (ELISA) kit | Ferguson et al., 2010; Kamijo-Ikemori and Kimura, 2015 |
| 5. | Renal Wilms' tumor-1 (WT-1) | WT-1 is constitutively expressed on podocytes in healthy adult kidneys | Maintain normal podocyte function | Focal segmental glomerulosclerosis, steroid-sensitive nephrotic syndrome, acute kidney injury | Prognostic marker of podocyte injury | Differential centrifugation followed by lysis and immunoblotting | Zhou et al., 2008, 2013 |
| 6. | N-acetyl-beta-D-glucosaminidase | Lysosomal enzyme abundantly present proximal kidney tubule cells | Indicative of renal tubular function, patients with tubular and interstitial renal impairment, the total activity of urinary NAG is elevated | Chronic heart failure, acute kidney injury | Prognostic for mortality and rehospitalization for heart failure, renal impairment | Fluorimetric assay based on the fluorescent 4-methylumbelliferyl-N-acetyl-β-D-glucosaminide substrate or spectrophotometric method is based on highly soluble and stable 4-nitrophenyl-N-acetyl-β-D-glucosaminide as substrate | Skálová, 2005; Han et al., 2008; Jungbauer et al., 2011 |
| 7. | D-serine | Formed through serine racemase enzyme mediated conversion of L-serine | Anti-depressant properties | Schizophrenia, Alzheimer's disease | Prognostic biomarker for anti-depressant response to ketamine | High performance liquid chromatography/ amperometric, biosensor-based method |
Papouin and Haydon, 2018; MacKay et al., 2019 |
| 8. | Osteocalcin | Secreted solely by osteoblasts | Pro-osteoblastic, responsible for bone mineralization and calcium ion homeostasis | Chronic rheumatic diseases, bone metastases | Prognostic marker for skeletal metastasis marker | ELISA | Arai et al., 1992; Mishra, 2017; Anderson et al., 2018 |
| 9. | Cathepsin-D | Ubiquitously expressed lysosomal aspartic protease | Protein degradation and cell death and regulation of trypsinogen activation | Cystic fibrosis, pancreatitis via inflammatory cells | Prognostic marker for poor prognosis in glioma patients | Real-time -reverse transcription-PCR analysis | Fukuda et al., 2005; Mishra, 2017 |
| 10. | Urease, ammonia/urea (breath) | Neutralize stomach acid by producing ammonia from urea diffusing from the blood | Hydrolyze urea, to form ammonia and carbon dioxide | Gastritis, peptic ulcer and gastric cancer | Diagnostic marker for the presence of H. pylori | Rapid urease test, urea breath test | Mishra, 2017; Graham and Miftahussurur, 2018 |
| 11. | Calcitonin gene-related peptide (CGRP), and substance P (SP) | Pronociceptive role | Involved in development of pain and hyperalgesia | Colonic hypersensitivity | Diagnostic Marker of neurogenic inflammation | Capillary Isoelectric Focusing (CIEF) immunoassay | Delafoy et al., 2006; Mishra, 2017; Jasim et al., 2018 |
| 12. | Brain-derived neurotropic factor (BDNF) | Neurotrophin having role in neuronal survival and development | Involved in mechanism of hyperalgesia | Upregulated and associated with pain in chronic pancreatitis | Diagnostic marker of chronic pancreatitis | Immunohistochemistry | Zhu et al., 2001 |
| 13. | Galectin-3 | A member of β-galactoside binding lectins | Activates a variety of profibrotic factors, promotes fibroblast proliferation and transformation, and mediates collagen production | Fibrotic diseases, cardiac disorders, asthma, atherosclerosis, atopic dermatitis | Prognostic biomarker in patients with heart failure | ELISA, BGM Gal-3 assay; RCHITECT Gal-3 assay | Gehlken et al., 2018; Sciacchitano et al., 2018 |
| 14. | Mucin | Prolines, threonines and serine rich proteins that contain tandem repeat motifs | A physical barrier limiting damage to the epithelium and attenuates activation of innate and adaptive immune responses | Deficiency causes inflammation of the colon and superficial erosions consistent with ulcerative colitis | Diagnostic and prognostic marker of gastrointestinal disease, cancer | Solid-phase sandwich ELISA | Kufe, 2009; Chen et al., 2015; Celi et al., 2018; Bademler et al., 2019 |
| 15. | Neutrophil gelatinase associated lipocalin and cystatin C | Expression is induced in liver, spleen and immune cells in response to ischemic damage or other kidney insult; cysteine protease inhibitor expressed by nucleated cells | – | Indicative of kidney damage | Diagnostic biomarker for tubular damage markers | ELISA | Siddiqui et al., 2017 |
| 16. | Lactoferrin | Member of the transferrin family of iron-binding glycoproteins | Component of the innate immune system, binds to iron with high affinity and thus control inflammation | Obesity, type 2 diabetes, and cardiovascular diseases | Non-specific diagnostic marker of inflammation | Immunoassay | Mayeur et al., 2016 |
| 17. | Tumor M2-pyruvate kinase (Tumor M2-PK)/M2-pyruvate kinase | Tissue-specific isoenzymes are replaced by M2-PK | In tumor cells is a shift from the tetrameric form to a nearly inactive dimeric form occurs | Increased in some human cancers, diabetes mellitus, coronary heart disease, chronic renal failure | Prognostic biomarker for pancreatic cancer, GIT stress/diseases | ELISA | Siddiqui et al., 2017; Bandara et al., 2018 |
| 18. | Catestatin (CST) | Peptide derived from the neuroendocrine protein chromogranin A | Autocrine inhibitor of catecholamine secretion, regulates hypertension | Cardiovascular disorders | Diagnostic marker of psychological stress associated with increased mortality in heart patients | ELISA | Mahata et al., 2018 |
| 19. | Fecal secretogranin | Proteins present in secretory cells of the enteric, endocrine, and immune systems | Reflect activity of enteric, endocrine, and immune systems | Ulcerative colitis, irritable bowel syndrome | Prognostic marker | Commercial radioimmunoassay | Ohman et al., 2012; Magnusson et al., 2018 |
| 20. | Cystatin-C | Member of group of cysteine protease inhibitors | Produced mainly through nucleated cells | Chronic kidney disease | Diagnostic marker for glomerular filtration | Particle-enhanced turbidmetric immunoassay | Onopiuk et al., 2015; Ogawa-Akiyama et al., 2018 |
| 21. | Urinary activin A | Member of the TGF-beta superfamily, is correlated with the degree of tubular damage | stimulated by inflammatory mediators | Ischemic kidneys | Diagnostic biomarker for acute kidney injury | ELISA | Takahashi S. et al., 2018 |
| 22. | Cardiac troponin (cTn) | Cardiac-specific proteins that are part of the troponin complex part of contractile apparatus | Released in blood followed by an acute myocardial infarction (AMI) and other types of acute myocardial injury | Cardiac injury | Diagnostic biomarker for acute myocardial infarction | Troponin I assay | Hammarsten et al., 2018 |
| 23. | Visfatin | An endocrine, autocrine as well as paracrine peptide | Participate in enhancement of cell proliferation, biosynthesis of nicotinamide mono- and dinucleotide and hypoglycemic effect. | Endometrial cancer, diabetes | Diagnostic marker | Multiplex fluorescent bead-based immunoassays | Adeghate, 2008; Baldassarre et al., 2018; Cymbaluk-Płoska et al., 2018 |
| 24. | Interleukin-6 | A pleiotropic, pro-inflammatory cytokine | Play an important role in inflammation, immunity, reproduction, metabolism, hematopoiesis, neural development, bone remodeling and angiogenesis | Albuminuria, retinopathy, and cardiovascular disease | Diagnostic and prognostic marker | SignaturePLUS Protein Array Imaging and Analysis System | Baker et al., 2018; Vainer et al., 2018 |
| 25. | Fibrinogen | A glycoprotein that enzymatically converted to fibrin and subsequently forms fibrin-based blood clot | Traditional markers of inflammation | Chronic kidney disease | Prognostic marker | Immunonephelometry | Baker et al., 2018 |
| 26. | C-reactive protein (CRP) | An acute phase reactant of the pentraxin family | During pathogen-independent inflammation, CRP binds to DNA and histones and scavenges the nuclear materials released from damaged circulating cells to activate innate immune cells | Solid tumor | Prognostic marker | Turbidmetric immunoassay | Baldassarre et al., 2018; Shrotriya et al., 2018 |
| 27. | Natriuretic peptide | A polypeptide hormone secreted by heart muscle cells | Reduce blood pressure, diuretic, sympathetic outflow, and vascular smooth muscle and endothelial cell proliferation | Acute (decompensated) and chronic heart failure, renal disease, hyperthyroidism, pulmonary diseases | Diagnostic and prognostic marker | Single-epitope sandwich assay | Tamm et al., 2008; Pandit et al., 2011; Vodovar et al., 2018 |
| 28. | Carbohydrate antigen 125 (CA 125) | A glycoprotein, product of MUC16 gene | Produced as a consequence of mechanical stress, such as fluid overload/serosal effusions and/or inflammation | Ovarian cancer, heart failure | Prognostic marker | Quantitative ELISA kit | Polineni et al., 2018; Stanciu et al., 2018 |
| 29. | Endothelin-1 | A potent vasoconstrictor peptide | Mainly secreted from endothelial cells | Systemic sclerosis, spontaneous cardiac or respiratory diseases | Diagnostic and prognostic marker | Radioimmunoassay (RIA) | Tessier-Vetzel et al., 2006; Odler et al., 2018 |
| 30. | Angiogenin | Member of the vertebrate-specific secreted ribonuclease A superfamily | Induce blood vessel formation | Colorectal cancer, acute myeloid leukemia, multiple myeloma, myelodysplastic syndromes cardiovascular diseases | Diagnostic and prognostic marker | ELISA | Yu et al., 2018 |
| 31. | β2-Microglobulin | 100-amino acid protein encoded by gene present on chromosome 15 in human | Tertiary structure is similar to the constant domain of the immunoglobulins and associate with human leukocyte antigen I (HLA-I) on the surface of all nucleated cells. The interaction is essential to antigen presentation | Acute kidney Injury, familial hypercatabolic hypoproteinemia, solid organ malignancies, lymphoproliferative disorders, such as myeloma and chronic lymphoblastic leukemia, and many autoimmune diseases, tubulointerstitial nephritis and uveitis (TINU) syndrome | Diagnostic marker | BN ProSpec Nephelometer | Hettinga et al., 2015; Lu et al., 2018 |
Oxidative stress-related biomarkers are important to detect autism in patients with autism spectrum disorders (ASDs). A decline in blood levels of reduced glutathione (27%), glutathione peroxidase (18%), methionine (13%), and cysteine (14%), and increased concentrations of oxidized glutathione (45%) relative to controls were indicative; whereas, superoxide dismutase, homocysteine, and cystathionine showed no association with ASDs (Frustaci et al., 2012). Furthermore, oxidative stress has been postulated as a key factor in the pathogenesis of neurodegenerative disorders, such as amyotrophic lateral sclerosis (ALS), Parkinson's disease (PD) (Medeiros et al., 2016), and Alzheimer's disease (AD) (Mander et al., 2016; Niedzielska et al., 2016). The presence of neurodegenerative diseases is revealed by elevated levels of oxidative stress biomarkers and by decreased levels of anti-oxidant defense biomarkers in the brain and peripheral tissues. Some oxidative stress markers, including, F2-isoprostanes and isofurans in plasma, are related to excess cardiovascular risk and are very common in patients with end-stage renal disease (Rivara et al., 2017). In addition, lipid oxidation could be a promising stress biomarker to diagnose systemic lupus erythematosus (Hu et al., 2016). Assessment of lipid peroxidation markers in non-invasive biological samples, especially saliva, has been validated through novel methods including ultrasound-assisted liquid-liquid semi-microextraction (UA-LLsME), tandem mass spectrometry and ultra performance liquid chromatography. The findings strongly recommend the adoption of such analytical methods in determining the level of lipid peroxidation as well as its potential as a potent oxidative stress marker and correlation with neurodegenerative changes (Peña-Bautista et al., 2019).
Furthermore, levels of the stress biomarker, MDA were significantly selective for cases of extrapulmonary tuberculosis compared with healthy controls (p < 0.05) (Goyal et al., 2016). Besides, the therapeutic efficacy of various molecules, such as coenzyme Q10 upon systemic diseases, such as coronary artery disease is also being assessed based on their impact over oxidative stress biomarkers (Jorat et al., 2019). Moreover, salivary MDA has been recognized as an important stress biomarker in systemic and oral diseases (Khoubnasabjafari et al., 2016). In another study, in the first month after birth, elevated F2-isoprostanes, produced through two distinct pathways simultaneously in the disease state predict poor respiratory outcomes and neuro-developmental risk in very preterm infants (Matthews et al., 2016). IL-6 and IL-8 have been reported to be used as potential biomarkers for diagnosis of oral pre-malignant lesion and oral carcinoma (Khyani et al., 2017).
Stress biomarker research reported that oxidative biomarkers could be promising approaches for enantioselective toxicity control of chiral pesticides (Ye et al., 2017). By contrast, the enzymatic anti-oxidant defense system, which is damaged in recurrent aphthous stomatitis patients with active lesions, has been proposed to have an important role in its pathogenesis and could represent the best stress biomarker in this situation (Zhang Z. et al., 2017). Plasma protein-bound di-tyrosines were designed as oxidative stress biomarkers in patients with end-stage renal disease on maintenance hemodialysis (Colombo et al., 2017). Also, a strong association between oxidative stress and anti-oxidant biomarkers in the circulating, cellular, and urinary anatomical compartments in Guatemalan children from the western highlands was reported (Soto-Mendez et al., 2016). The study revealed that excessive oxidation is suggested to be associated with an increase in the urinary biomarkers of oxidative stress F2-Iso and 8-OHdG andurinary excretion of oxidative biomarkers associates directly with the activity of antioxidant enzymes and inversely with the vitamin concentration. Studies on the relationship between lipid peroxidation biomarkers offer a promising research line that need to be developed with the aim to help clinicians in early disease diagnosis, effective treatment initiation and reliable disease monitoring (García-Blanco et al., 2017b).
Oxidative stress enhanced lipid peroxidation (LPO) leads to the accumulation of 4-hydroxy-2-nonenal that ultimately produces exocyclic etheno-DNA adducts, which are strong pro-mutagenic DNA lesions. Biomonitoring of etheno-DNA adducts from tissues, white blood cells and urine using ultra-sensitive detection methods are promising tools for the prognosis of malignancy, the efficacy of chemopreventive and outcome of therapeutic interventions (Bartsch et al., 2011).
Dietary anti-oxidants are inversely related to oxidative stress biomarkers among men with prostate cancer (Vance et al., 2016). Men diagnosed with prostate cancer are reported to have increased oxidative stress and lower antioxidant enzyme activity (Arsova-Sarafinovska et al., 2009). Furthermore, increased levels of urinary oxidative biomarkers, such as 8-hydroxydeoxyguanosine (8-OH-dG), could be considered the best oxidative stress biomarkers in metal oxides nanomaterial-handling workers (Liou et al., 2016). Increased level of oxidative stress markers, such as malondialdehyde and a decreased level of anti-oxidative markers, such as superoxide dismutase and glutathione peroxidase in the serum or the aqueous humor is suggested to be reliable aids in the diagnosis of glaucoma as reported by Benoist d'Azy et al. (2016), through a systematic review and meta-analysis. Therapeutic efficacy of molecules, e.g., ascorbic acid in ameliorating oxidative stress has been evaluated based on the plasma levels of markers including albumin, malondialdehyde, and superoxide dismutase (Yimcharoen et al., 2019).
Biomarkers associated with post-traumatic stress disorder (PTSD) include endocrine as well as molecular biomarkers. Assessment can be done at the genetic level (DNA or single nucleotide polymorphism biomarkers), at the level of expression of a gene, e.g., RNA biomarkers, the protein levels, such as peptide as well as proteins as biomarkers, etc. (Schmidt et al., 2013). Assessment can also be done at the epigenome level to program the genomic activity by various ways, such as methylation of DNA, modifications of histone, and RNA interference, otherwise termed as epigenetic biomarkers. Imaging biomarkers are also associated with PTSD whose assessment can be done by either structural method, such as magnetic resonance imaging (MRI) or functional method, such as MRI/fMRI (Berger et al., 2009; Schmidt et al., 2013; Bisson et al., 2015). Certain common biomarkers are critical in inducing morphological alteration in tissues, for instance, experimentally induced febrile seizures were reported with morphological changes in the brain, such as dentate gyrus which is mainly elicited by corticosterone, the simple stress hormone (van Campen et al., 2018). Table 4 shows an overview of various biological markers associated with numerous physical, emotional and environmental stresses.
Table 4.
Various biological markers associated with numerous physical, emotional and environmental stresses.
| S. No. | Biomarker molecule | Brief introduction | Efficacy of the molecule | Associated ailment(s) | Marker intended for | Diagnostic assay | Reference(s) |
|---|---|---|---|---|---|---|---|
| 1. | α-amylase | A salivary enzyme, estimated as the marker for sympathetic stimuli. In stress response the α-amylase concentration increases | Hydrolysis of internal α-1,4-glycosidic linkages in starch | Stress associated with periodontal disease | Physiologic and behavioral stress | Enzyme Immunoassay (EIA) kit | Rai and Kaur, 2011 |
| 2. | Chromogranin A (CgA) | A protein prohormone with acidic nature, present in the secretory granules of different neuroendocrine tissues | Influence endocrine, cardiovascular, and immune systems and glucose or calcium homeostasis | Indicative of endocrine tumors, cardiovascular, inflammatory, and neuropsychiatric diseases | Mental stress marker during monotonous driving | ELISA, immunoradiometric assay (IRMA) and RIA | Yamakoshi et al., 2009; D'amico et al., 2014; Gut et al., 2016; Mishra, 2017 |
| 3. | Secretory IgA | Present in external body secretions like saliva. The induction of stress hormones, especially cortisol, have an adverse impact on immunoglobulin secretion | Participate in immune function of mucous membrane | Immunosuppressive effects | Job stress | Immunofluorescence staining and flow-cytometry analysis | Lee et al., 2010 |
| 4. | MicroRNA-29c | Expressed in the human prefrontal cortex | Involved in psychopathologies, such as schizophrenia and bipolar disorder and Alzheimer's, Huntington's and Parkinson's diseases | Indicate stress-induced functional neural alterations | Social stress task | TaqMan Low Density array/TaqMan real-time PCR assay | Vaisvaser et al., 2016 |
| 5. | miR-16 | Acute psychological stress-responsive miRNAs | Play a role in the inhibition of inflammatory cytokine response | Indicate positive correlation with anxiety | Chronic academic stress | miRNA microarray/TaqMan® MicroRNA assays | Honda et al., 2013 |
| 6. | miR-146a and−212 expression | Responsive to inflammatory stimuli | Deficiency result in an excessive IL-6 and TNF-α production, myeloproliferative syndrome, chronic inflammation and a decrease in the number and quality of hematopoietic stem cells | Postpartum psychosis | Postpartum psychotic stress | TaqMan array human microRNA A Cards v2.0 | Weigelt et al., 2013; Testa et al., 2017 |
| 7. | Relative telomere length | Repetitive DNA sequences present at the ends of eukaryotic chromosomes that undergoes attrition after every somatic cell division | Shorter telomeres are indicative of accelerated aging | Fear disorders including generalized anxiety disorder (GAD), panic disorder, agoraphobia, and social and other phobia | High phobic anxiety in women | Real-time polymerase chain reaction | Okereke et al., 2012 |
| 8. | Sigma-1 receptor | An endoplasmic reticulum chaperone involved in regulation of bioenergetics, free radical generation, oxidative stress, unfolded protein response, cytokine signaling, morphogenesis of neuronal cells | Its ligands exhibit antidepressant-like and neuroprotective actions | Mental disorders | Psychological stress | Single-cell reverse transcription-polymerase chain reaction (scRT-PCR) and immunofluorescence staining | Hayashi, 2015; Zhang K. et al., 2017 |
| 9. | Biopyrrins (bilirubin oxidative metabolites) | Biosynthesized from heme | Considered as harmful and useless substance | Associated with the risk of bilirubin encephalopathy and neuronal injury | Psychological stress | ELISA | Miyaoka et al., 2005 |
| 10. | Glycated hemoglobin (HbA1C) | HbA1c is considered as a possible substitute to fasting blood glucose for diagnosis of diabetes. | Independent risk factor for coronary heart disease and stroke | Anxiety, irritability, mood swings, insomnia, depression, and a sense of failure | Physical and emotional exhaustion mediated stress | Hexokinase assay and turbidimetric immunoinhibition methods by automatic analyzer | Sherwani et al., 2016; Deneva et al., 2019 |
| 11. | Cardiac troponin I | Considered as gold-standard biomarker for detecting acute myocardial necrosis and acute myocardial infarction | Cardiac damage during HS recovery | Multi-organ failure | Heat stroke stress | Handheld iSTAT clinical analyzer | Quinn et al., 2014; Park et al., 2017 |
| 12. | Osteopontin | A phosphoglycoprotein marker of hypoxic conditions | Involved in biomineralization, immune regulation and inflammation | Acute mountain sickness, high-altitude cerebral edema, high-altitude pulmonary edema | High altitude stress | ELISA | Basnyat, 2018; Tang X. G. et al., 2018 |
HSPs are being accepted widely as potent biomarkers with multiple applications wherein lower HSP expressions have been linked to the manifestation of neurological disorders, cardiovascular disease, and cancer (Charmpilas et al., 2017). HSP90 and proinsulin are recognized as a stress biomarker of beta-cell stress in the early period of type 1 diabetes; HSP90 increases about four times in the islets from non-obese diabetics relative to those from controls (Watkins et al., 2016). Another study reported that salivary and circulatory HSP70 showed a significant increase in a renal dialysis patient, confirming that salivary and circulatory HSP70 is an efficient stress marker in chronic renal disease condition (Hegde and Nireeksha, 2016).
Prognostic biomarkers are getting much focus these days, owing to their importance in determining the outcome of a disease/condition as well as the therapy. Various APPs have also long been used as general prognostic and diagnostic biomarkers in a variety of injuries, independently of their location and cause. Proteomic techniques have demonstrated that APPs favor the systemic regulation of defense, coagulation, proteolysis, and tissue repair (Schrödl et al., 2016). Recently, the usefulness of biomarkers in cancer development, diagnosis, and prognostic accuracy has been reviewed by Dadar et al. (2016). DNA methylation has also been utilized as a biomarker for the prognosis and diagnosis of several cancers including breast, colon, liver, and lung (Hao et al., 2017). A glycoprotein having molecular mass of 40 kDa harboring three N-terminal amino acids namely tyrosine (Y), lysine (K), and leucine (L) known better as YKL-40 is considered as an ideal biomarker in serum for diseases indicated by inflammation, fibrosis, remodeling of the extracellular matrix and malignancy (Johansen, 2006). YKL-40 is proved to be a diagnostic marker with better sensitivity, specificity, and accuracy for detecting pleural effusion with malignancy (Shahanaze et al., 2018) and breast cancer prognosis in human subjects (Wan et al., 2017).
Promising results are observed in recent literature regarding the prospects of circulating pro-angiogenic miRNAs, such as miR-17-5p, miR-18a, miR-19b-1, miR-20a, miR-210, miR-296, and let-7f as novel biomarkers for predicting the risk and severity of gastric malignancy in human subjects (Peng W. et al., 2018). Scientists have developed a novel and cost-effective solid phase extraction process using magnetic β-cyclodextrin for the extraction and enrichment of the potential markers of gastric tumor, such as p-hydroxybenzoic acid and p-cresol which is eliminated in traces in the urine of human gastric tumor patients (Shi et al., 2019). Use of circulating miRNA in diagnostics of brain tumor is promising since other protein biomarkers, such as glial fibrillary acidic protein (GFAP) are restricted to CSF or other brain tissue. From the meta-analysis of different studies conducted in the last years, it can be concluded that six mi RNAs, such as miR-9, miR-15a, miR-16, miR-21, miR-23a, and miR-124 have better accuracy to consider as circulating biomarker for gliomas (Santangelo et al., 2017) Different serum exosomal miRNAs including miR-638 could be utilized for diagnosis and prognosis of hepatocellular carcinoma (Shi et al., 2018; Xue et al., 2019).
Another emerging candidate for clinical biomarker is the exosomes, which are the secretory vesicles released from cells and contain multiple compounds, such as lipids, proteins, RNAs, etc. (Théry et al., 2002). These vesicles were initially regarded as garbage bags of cells but later after intense exploration, were found to have critical roles in cell communication, physiological events as well as pathological changes (Bang and Thum, 2012; Sun et al., 2013). The findings on exosomes that they are released by multiple cell types and present in almost all body fluids, paved the way for identifying exosomes specific to cells of origin as novel biomarkers for clinical conditions also (Lin et al., 2015). It is the miRNAs present in exosomes that are largely evaluated for diagnosis of various conditions like cancer since exosomal miRNAs are resistant to RNase-mediated degradation (Hunter et al., 2008). In human ovarian cancer, eight miRNAs from the biopsy specimen which are previously recognized as specific biomarkers for the condition could be detected from the serum exosomes also, suggesting the scope of developing these exosomal miRNAs as surrogate diagnostic candidates as well as for biopsy profiling (Taylor and Gercel-Taylor, 2008). Another report on esophageal squamous cell carcinoma indicated the specificity of exosomal miR-21 as biomarker from serum which is detected in patients with benign tumor without any systemic inflammation and its level in serum was proportionate to the tumor progression, suggesting its role in prognosis also (Tanaka et al., 2013; Lin et al., 2015). Besides cancer, exosomal miRNAs were identified in predicting cardiovascular conditions, metabolic disorders, and renal dysfunctions (Hong et al., 2009; Kuwabara et al., 2011).
Most of the physiological markers are late to reflect their serum or urine levels in chronic kidney patients, so it is a herculean task to identify a urinary biomarker in patients suffering from chronic kidney disease at an early stage. Urinary exosomes are gaining importance among researchers as a potential bioactive fluid which can be targeted as a source of biomarkers in patients suffering from chronic kidney disease. In a recent study, it has been found that 30 non-coding (nc) RNAs are differentially expressed in the urinary exosomes at an early stage of kidney disease. Out of these, miRNA-181a is the most promising as it is shown a 200-fold difference in comparison to healthy subjects (Khurana et al., 2017).
Studies on neurological conditions like Alzheimers disease reported the involvement of exosomes in secreting out the disease-related β-amyloid peptides (Rajendran et al., 2006) as well as the phosphorylation of exosome-associated tau during early stages of the condition (Saman et al., 2012), thereby indicating the critical role of exosomes in cerebrospinal fluid as biological signatures. The ultimate product of metabolism of purine, i.e., urate has been identified in the recent past as an influential neuroprotectant to treat Parkinson's disease (PD) apart from being an important biomarker/predictor of the PD (Chen et al., 2012).
Identification and validation of disease-associated biomarkers play a crucial role in detecting diseases before their symptoms are observed, as well as in monitoring the outcome of therapies. Much focus is needed in designing point of care diagnostics based on biomarkers which need detailed and specific molecular profiling and specific screening using enough sample/population sizes. In conclusion, the important roles of stress biomarkers, their prognostic factors, and drug target properties represent a significant resource for future clinical applications and therapeutic approaches. Biomarkers in the prognosis of stress-related diseases/disorders are summarized in Figure 7.
Figure 7.
Biomarkers in prognosis of stress related diseases/disorders.
Clinical Significance of Biomarkers in Stress-Related Diseases—Highlights
Engineering robust biomarkers, either prognostic or predictive, is imperative for the advancement of clinical-related treatment strategies. Several successful research efforts have been made or being made to identify the relative usefulness of various biomarkers, including HSPs and APPs either in their pristine or combinational way in discriminating various stress-related diseases and disorders. The key scientific advances have revealed the uniqueness of biomarkers with special reference to the clinical arena. However, the prognostic or predictive values of the biomarkers mentioned above could not be ascertained in a statistically significant way and also to highlight the clinical manifestation, in-depth futuristic studies with larger clinical subjects may be warranted.
Stress is an inevitable response in all organisms at the molecular to the whole-body level to maintain their homeostasis.
Potential stress biomarkers act as molecular signatures found useful as non-invasive biological approaches for diagnosis, prognosis and treatment guidance.
Diagnostic, prognostic and therapeutic values of valuable biomarkers have been highlighted in stress-mediated diseases and disorders.
Various biomarkers have been proven as effective tools to diagnose the stress status as well as pathophysiological aspects of human/animal subjects.
Identifying highly reliable biomarker is critical because the most promising markers need to be correlated with the particular conditions to facilitate prognosis and specificity of the therapy.
Some of the potent biomarkers which can be explored clinically are:
Plasma and serum levels of malondialdehyde (MDA), isoprostanes, glutathione (GSH), and ROS reduction catalyzing enzymes, such as superoxide dismutase, catalase, myeloperoxidase, glutathione peroxidase, and thioredoxin reductase.
Urate level as a promising biomarker to assess the incidence, diagnosis, and therapeutic prognosis of various neurodegenerative, hepatic, and renal diseases.
APPs as indicators for social stresses, such as transportation, mixing, and abrupt weaning, which elicit an acute phase response.
Sensitive neoplastic biomarkers can aid in the early detection and prognosis of neoplastic changes.
Advances in molecular medicine have identified cell-free nucleic acids, including DNA, mRNA, and miRNAs as novel diagnostic markers for myopathies, recurrent exertional rhabdomyolysis, and osteochondrosis.
Biocompounds, such as peroxilipids, malondialdehyde, etc. have been suggested to aid in disease diagnosis during early stages of gestation.
HSPs are being accepted widely as potent biomarkers with multiple applications wherein lower HSP expressions have been linked to the manifestation of neurological disorders, cardiovascular disease, and cancer.
Potent biomarkers for sensitizing renal injury include albumin, N-acetyl-β-D-glucosaminidase, kidney injury molecule-1, and exosomal transcription factors.
Potent mediators of cardiovascular, CNS, hepatic, and nephrological disorders could be involved in the prognosis and treatment strategies.
Stress biomarker research identified that oxidative biomarkers could be potential approaches for enantioselective toxicity control of pesticides.
Non-invasive biological sources, such as saliva, urine, sweat, etc. provide optimum sources for the quantitative and qualitative assessment of chemical and physiological mediators associated with various conditions, such as stresses, diseases, and injury.
Presently, quantitation of biomarkers is mostly based on immunological, chromatographical, and mass spectrophotometric assessments.
Potent biomarkers which are efficiently validated can be employed in various reliable commercial assay kits.
Advances in clinical techniques to assess various vital stages, as well as their underlying processes, will help to unravel the roles played by much more as-yet-undiscovered potent biomarkers, which ultimately will benefit the treatment and outcomes of patients.
Further scientific and technical advances are yet to be explored, particularly regarding proteomic approaches, providing a wider chance to identify optimal and specific markers in any physiological/pathological disorder.
Conclusion and Future Perspectives
In humans and animals, homeostasis is influenced highly by the physiological disturbances and molecular instabilities inflicted by various stressors, ultimately affecting their productivity, psychological health, and social welfare. According to the globally accepted one-health concept, where human health is highly intertwined with that of domestic and wild animals, there is a high demand to identify stress markers in the human and veterinary medicine sectors. There may be various biomarkers for each type of stress; however, identifying the best and most reliable biomarker(s) is critical, because the most promising markers need to be highly correlated with the specific pathophysiological aspects of the particular stress. They may include proteins, enzymes, hormones, chemicals, metabolites, genes, or by-products. Notable ones are malondialdehyde, isoprostanes, enzymatic antioxidants, blood urates, cortisol, copeptin, alpha-amylase, secretory IgA, chromogranin A (CgA), lysozyme, microRNAs (miRNAs), long non-coding RNAs (lnRNAs), heat shock proteins (HSPs), and acute phase proteins. Potent markers identified so far have been proven as effective tools to diagnose the stress status and have been applied to assess the prognosis and specificity of the therapy.
Diverse data from nature related to the identification of various types of physiological stresses and their associated molecular and systemic mediators, are still accumulating. Other novel technologies also could enable the development of non-molecular, functional, or biophysical tissue-based biomarkers. Moreover, the impact of sex differences and associated sex hormones over the expression of certain biomarkers need to be addressed. Therefore, the convergence of these biological, ecological, epidemiological, and zoonotic data, will lead their scientific scrutiny to identify promising markers to assess disease risk, diagnosis, prognosis, and therapeutic efficacy of drugs. Advances in clinical techniques to assess various vital stages, as well as their underlying processes, will help to unravel the roles played by many more as-yet-undiscovered potent biomarkers, which ultimately will benefit the treatment and outcomes of patients.
Stress is an inevitable culmination of all mammalian metabolism, which will be regulated normally within the physiological limits may skew exorbitantly following certain disturbances or diseases. This skewing or stress response may upshoot the concentration of different biochemical compounds within the cells or body fluids which could be potentially exploited as biomarkers for diagnosis, prognosis, and for therapy selection. Subcellular modification prevails during the stress response and disease progress –at the microarchitecture of the cell could facilitate positive clinical interpretations and remedial strategies. But the major deterrent in the practical use of stress biomarkers are uncertainty as to whether the reported response is a steady-state adaptation stage or the initial phase of a stress response. On the other hand, comparisons between experimental variants, plots, or species should only be made since an equal steady-state is marked. Another hitch in the exploitation of biomarkers clinically is the uncertainty that whether these are part of the stress-related diseases and disorders, and anti-oxidative defense systems or not. As the most of the known stress biomarkers as of date, such as thermal stress markers like heat shock proteins (HSPs), innate immune markers like acute phase proteins (APPs), oxidative stress markers, and chemical secretions in the saliva and urine are the part of anti-oxidant defense system of the body, a highly sensitive cut off value to differentiate their levels in different biological samples at different stages of stress or disease with respect to healthy condition is warranted. According to the results reported in this review, it is significant to involve multiple parameters, possibly covering potent mediators of cardiovascular, central nervous system, hepatic, and nephrological disorders, energy dissipation, and anti-oxidative defense, in human and animal-stress physiological studies. For example, in studies on animal tissues there is, at present, an attempt to measure as many systems related to cascade influences of vital early responding (e.g., cardiovascular, CNS, renal) and late responding (e.g., hepato-biliary, pancreatic) systems as possible.
Promising attempts to use several components of anti-oxidative and protective defense systems in human and animal tissues revealed different statistical approaches, which were profitably used to reveal typical arrangements of stress biomarker responses of animal and human at field plots. The first attempt toward the combination of such data proposes the metabolic modeling studies, which potentially gives perspective about multisystem involvement and hence widespread disturbance in a range of biomarkers through protective and stress pathways. From this perspective, the accurate evaluation of stress markers in saliva, urine, tears, and feces will turn to a critical part in measuring of the stress response of human and animal, although it is necessary to include a wide range of stress–physiological parameters.
Identification of many more useful markers is warranted because their clinical application as universal biomarkers demands the following properties:
The ease of collecting and processing the related biological specimen.
Stability and durability of the marker throughout the storage and evaluation period.
The availability of assays with sufficient specificity and sensitivity for the particular marker.
Moreover, identifying non-invasive methods to assess biomarkers has the potential to provide accurate data related to exercise-induced physiological and psychological stress. Furthermore, multiple stress biomarkers are detectable in ambulatory individuals and add prognostic value to standard risk factors for predicting death. So far, considerable advancements have been achieved in identifying and standardizing biomarkers of various origins. However, salivary and renal/urinary biomarkers are proving quite convenient. Present quantitation mostly based on immunological, chromatographical, and mass spectrophotometric assessments, have produced reliable results. However, some variability, and low reproducibility are also reported. Further scientific and technical advances are necessary, particularly regarding proteomic approaches, so that profiling of the markers in each biological sample becomes possible, providing a wider chance to identify optimal and specific markers in any physiological/pathological disorder. Hopefully, future advances will provide us with precise, multidimensional biological molecules that can address many of the current diagnostic and therapeutic deficiencies.
Author Contributions
KD, SL, MD, HS, and RT initiated this review compilation. RK, RT, SC, MY, PB, and KK updated the current progress of identifying biomarkers. RK designed the table. AM and KK designed the figures. KD, HI, AM, SJ, KS, and WC reviewed, analyzed, and edited the final version. All the authors substantially contributed to the conception, design, analysis, interpretation of data, checking and approving the final version of the manuscript, and agree to be accountable for its contents.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
All the authors acknowledge and thank their respective Institutes and Universities for providing literature facilities.
Glossary
Abbreviations
- AKI
acute kidney injury
- APPs
acute phase proteins
- Adipo-IR
adipose tissue insulin resistance index
- ACTH
adrenocorticotropic hormone
- AGEs
advanced glycation end products
- AOPP
advanced oxidation protein products
- ALAT
alanine-aminotransferase
- ALP
alkaline phosphatase
- AD
Alzheimer's disease
- ALS
amyotrophic lateral sclerosis
- ASAT
aspartate-aminotransferase
- Asp
aspartic acid
- ADHD
Attention-Deficit/Hyperactivity Disorder
- AIx
augmentation index
- ASDs
autism spectrum disorders
- Bcl-2
B-cell lymphoma 2
- Bcl-xL
B-cell lymphoma extralarge
- BP
blood pressure
- BUN
blood urea nitrogen
- BNP
brain-type natriuretic peptide
- CCL2
CC-chemokine ligand 2
- CNS
central nervous system
- CgA
chromogranin A
- COPD
chronic obstructive pulmonary disease
- CRH
corticotropin-releasing hormone
- CRP
C-reactive proteins
- DAXX
death domain associated protein
- DN
diabetic nephropathy
- DG
diacylglycerols
- ELISAs
enzyme-linked immunosorbent assays
- eGFR
estimated glomerular filtration rate
- EBC
exhaled breath condensate
- ETFs
exosomal transcription factors
- F2-Isops
F2-isoprostane
- FMD
Flow Mediated Dilation
- FFA
free fatty acid
- GC/MS/MS
gas chromatography coupled with tandem mass spectrometry
- GIP
gastric inhibitory polypeptide
- GLP-1
glucagon-like peptide-1
- GRP78
glucose-related protein 78
- Glu
glutamic acid
- GSH
glutathione
- GSSG
glutathione disulfide
- GPX
glutathione peroxidase
- HF
heart failure
- HSPs
heat shock proteins
- HbA1c
hemoglobin A1c
- HEL
hexanoyl-lysine
- HPLC
high performance liquid chromatography
- HDL
high-density lipoprotein
- HPLC-DAD
HPLC with diode-array detection
- HODE
hydroxyoctadecadienoic acid
- HPA
hypothalamic-pituitary-adrenocortical
- IGFBP7
insulin-like growth factor-binding protein 7
- IL-1RA
interleukin 1 receptor antagonist
- IL-22
Interleukin-22
- LPO
lipid peroxidation
- LBP
lipopolysaccharide-binding protein
- LDL
lipoprotein
- liver IR
liver insulin resistance
- liver IS index
liver somatic index
- L-FABP
liver-type fatty acid-binding protein
- LDL
low-density lipoprotein
- MRI
magnetic resonance imaging
- MAP
major acute phase protein
- MDA
malondialdehyde
- MDA-LDL
malondialdehyde-modified low-density lipoprotein
- Met
methionine
- miRNAs
microRNAs
- MG
monoacylglycerol
- MCP-1
monocyte chemoattractant protein-1
- MCL1
myeloid cell leukemia sequence 1
- MPO
myeloperoxidase
- PUFAs
N-3 polyunsaturated fatty acids
- NO
nitric oxide
- NEFA
non-esterified fatty acids
- Orn
Ornithine
- oxLDL
oxidized low density lipoprotein
- HOMA-B
pancreatic B-cell function
- PD
Parkinson's disease
- PHE
phenylalanine
- PTSD
post-traumatic stress disorder
- PTSD
post-traumatic stress disorder
- RNS
reactive nitrogen species
- ROS
reactive oxygen species
- RSI
reactive species interactome
- RBCs
red blood cells
- Tregs
regulatory T lymphocytes
- SAA
serum amyloid A
- SAP
serum amyloid P
- Ask 1
signal-regulating kinase 1
- sICAM
soluble intercellular adhesion molecule
- SCD
stearoyl-CoA-desaturase
- SOD
superoxide dismutase
- SOCS
suppressor of cytokine signaling
- SAM
sympathetic adreno-medullary
- TBARS
thiobarbituric acid-reactive substances
- TAS
total anti-oxidant status
- TAS
total anti-oxidant status
- HNE
trans-4-hydroxy-2-nonenal
- TRP
transient receptor potential
- TG
Triglyceride
- Tyr
Tyrosine
- UA-LLsME
ultrasound-assisted liquid-liquid semi-microextraction
- uHSP72
urinary heat shock protein 72
- sVCAM
vascular cell adhesion molecule-1
- AGP
α1-acid glycoprotein
- BD2
β-defensin 2
- GGT
γ-glutamyltransferase
- 4-HNE
4-hydroxy-2-nonenal
- 8-OH-dG
8-hydroxydeoxyguanosine
- 8-iso-PGF2α
8-iso-prostaglandin F2α
- 8-ISO
8-isoprostane
- NF-κB
nuclear factor-kappa B.
References
- Aardal-Eriksson E., Eriksson T. E., Holm A. C., Lundin T. (1999). Salivary cortisol and serum prolactin in relation to stress rating scales in a group of rescue workers. Biol. Psychiatry 46, 850–855. 10.1016/s0006-3223(98)00381-3 [DOI] [PubMed] [Google Scholar]
- Abbas M., Habib M., Naveed M., Karthik K., Dhama K., Shi M., et al. (2017). The relevance of gastric cancer biomarkers in prognosis and pre- and post-chemotherapy in clinical practice. Biomed. Pharmacother. 95, 1082–1090. 10.1016/j.biopha.2017.09.032 [DOI] [PubMed] [Google Scholar]
- Abdul-Salam V. B., Ramrakha P., Krishnan U., Owen D. R., Shalhoub J., Davies A. H., et al. (2010). Identification and assessment of plasma lysozyme as a putative biomarker of atherosclerosis. Arterioscler. Thromb. Vasc. Biol. 30, 1027–1033. 10.1161/ATVBAHA.109.199810 [DOI] [PubMed] [Google Scholar]
- Abe K., Takahashi A., Fujita M., Imaizumi H., Hayashi M., Okai K., et al. (2018). Dysbiosis of oral microbiota and its association with salivary immunological biomarkers in autoimmune liver disease. PLoS ONE 13:e0198757. 10.1371/journal.pone.0198757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abey S. K., Yuana Y., Joseph P. V., Kenea N. D., Fourie N. H., Sherwin L. B., et al. (2016). Lysozyme association with circulating RNA, extracellular vesicles, and chronic stress. BBA Clin. 7, 23–35. 10.1016/j.bbacli.2016.12.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abey S. K., Yuana Y., Joseph P. V., Kenea N. D., Fourie N. H., Sherwin L. B., et al. (2017). Data supporting the effects of lysozyme on mRNA and protein expression in a colonic epithelial scratch wound model. Data Brief. 11, 15–18. 10.1016/j.dib.2016.12.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adeghate E. (2008). Visfatin: structure, function and relation to diabetes mellitus and other dysfunctions. Curr. Med. Chem. 15, 1851–1862. 10.2174/092986708785133004 [DOI] [PubMed] [Google Scholar]
- Admoni-Elisha L., Nakdimon I., Shteinfer A., Prezma T., Arif T., Arbel N., et al. (2016). Novel biomarker proteins in chronic lymphocytic leukemia: impact on diagnosis, prognosis and treatment. PLoS ONE 11:e0148500. 10.1371/journal.pone.0148500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aldakheel F. M., Thomas P. S., Bourke J. E., Matheson M. C., Dharmage S. C., Lowe A. J. (2016). Relationships between adult asthma and oxidative stress markers and pH in exhaled breath condensate: a systematic review. Allergy 71, 741–757. 10.1111/all.12865 [DOI] [PubMed] [Google Scholar]
- Alicka M., Marycz K. (2018). The effect of chronic inflammation and oxidative and endoplasmic reticulum stress in the course of metabolic syndrome and its therapy. Stem Cells Inter. 2018:4274361. 10.1155/2018/4274361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allgrove J. E., Gomes E., Hough J., Gleeson M. (2008). Effects of exercise intensity on salivary antimicrobial proteins and markers of stress in active men. J. Sports Sci. 26, 653–661. 10.1080/02640410701716790 [DOI] [PubMed] [Google Scholar]
- Andersen A. D., Binzer M., Stenager E., Gramsbergen J. B. (2017). Cerebrospinal fluid biomarkers for Parkinson's disease–a systematic review. Acta Neurol. Scand. 135, 34–56. 10.1111/ane.12590 [DOI] [PubMed] [Google Scholar]
- Anderson S. T., Kidd L. J., Barton A. J., Greer R. M. (2018). Serum bone biomarkers osteocalcin and pyridinoline in mares during pregnancy and lactation, and in foals during early post-natal life. Res. Vet. Sci. 118, 34–40. 10.1016/j.rvsc.2018.01.007 [DOI] [PubMed] [Google Scholar]
- Annelies V., Harry R., Ines W., Annelies B., Tess D. B., Nina H. (2018). Evaluation of biomarkers of oxidative stress in attention-deficit/hyperactivity disorder (ADHD). J. Mol. Biomark. Diagn. 9:390 10.4172/2155-9929.1000390 [DOI] [Google Scholar]
- Apilux A., Rengpipat S., Suwanjang W., Chailapakul O. (2018). Development of competitive lateral flow immunoassay coupled with silver enhancement for simple and sensitive salivary cortisol detection. EXCLI J. 17, 1198–1209. 10.17179/excli2018-1824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arai Y., Takeuchi H., Oishi K., Yoshida O. (1992). Osteocalcin: is it a useful marker of bone metastasis and response to treatment in advanced prostate cancer? Prostate 20, 169–177. 10.1002/pros.2990200302 [DOI] [PubMed] [Google Scholar]
- Arantes L. M. R. B., De Carvalho A. C., Melendez M. E., Lopes Carvalho A. (2018). Serum, plasma and saliva biomarkers for head and neck cancer. Expert Rev. Mol. Diag. 18, 85–112. 10.1080/14737159.2017.1404906 [DOI] [PubMed] [Google Scholar]
- Arrigo A. P., Virot S., Chaufour S., Firdaus W., Kretz-Remy C., Diaz-Latoud C. (2005). Hsp27 consolidates intracellular redox homeostasis by upholding glutathione in its reduced form and by decreasing iron intracellular levels. Antioxid. Redox Signal 7, 414–422. 10.1089/ars.2005.7.414 [DOI] [PubMed] [Google Scholar]
- Arsalan M., Ungchusri E., Farkas R., Johnson M., Kim R. J., Filardo G., et al. (2018). Novel renal biomarker evaluation for early detection of acute kidney injury after transcatheter aortic valve implantation. Proc. Bayl. Univ. Med. Cent. 31, 171–176. 10.1080/08998280.2017.1416235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arsova-Sarafinovska Z., Eken A., Matevska N., Erdem O., Sayal A., Savaser A., et al. (2009). Increased oxidative/nitrosative stress and decreased antioxidant enzyme activities in prostate cancer. Clin. Biochem. 42, 1228–1235. 10.1016/j.clinbiochem.2009.05.009 [DOI] [PubMed] [Google Scholar]
- Arthington J. D., Eicher S. D., Kunkle W. E., Martin F. G. (2003). Effect of transportation and commingling on the acute-phase protein response, growth, and feed intake of newly weaned beef calves. J. Anim. Sci. 81, 1120–1125. 10.2527/2003.8151120x [DOI] [PubMed] [Google Scholar]
- Asa'ad F., Fiore M., Alfieri A., Pigatto P. D. M., Franchi C., Berti E., et al. (2018). Saliva as a future field in psoriasis research. BioMed. Res. Int. 2018:7290913. 10.1155/2018/7290913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asleh R., Briasoulis A., Berinstein E. M., Wiener J. B., Palla M., Kushwaha S. S., et al. (2018). Meta-analysis of the association of the haptoglobin genotype with cardiovascular outcomes and the pharmacogenomic interactions with vitamin E supplementation. Pharmacogen. Person. Med. 11, 71–82. 10.2147/PGPM.S159454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ay M. O., Erenler A. K., Dogan T., Yetim M. (2017). Diagnostic value of copeptin in acute myocardial infarction. Eur. Rev. Med. Pharmacol. Sci. 21, 1576–1582. [PubMed] [Google Scholar]
- Aydin S., Ugur K., Aydin S., Sahin I., Yardim M. (2019). Biomarkers in acute myocardial infarction: current perspectives. Vasc. Health Risk Manag. 15, 1–10. 10.2147/VHRM.S166157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Äyräväinen L., Heikkinen A. M., Kuuliala A., Ahola K., Koivuniemi R., Laasonen L., et al. (2018). Inflammatory biomarkers in saliva and serum of patients with rheumatoid arthritis with respect to periodontal status. Ann. Med. 50, 333–344. 10.1080/07853890.2018.1468922 [DOI] [PubMed] [Google Scholar]
- Aziz A. S., Kalekar M. G., Benjamin T., Suryakar A. N., Milsee Mol J. P. (2012). Chronic periodontitis and oxidative stress – a biochemical study. Indian J. Dent. Sci. 4, 22–26. [Google Scholar]
- Bademler S., Zirtiloglu A., Sari M., Ucuncu M. Z., Dogru E. B., Karabulut S. (2019). Clinical significance of serum membrane-bound mucin-2 levels in breast cancer. Biomolecules 9:E40. 10.3390/biom9020040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baena M. M., Tizioto P. C., Meirelles S. L. C., Regitano L. C. A. (2018). HSF1 and HSPA6 as functional candidate genes associated with heat tolerance in Angus cattle. R. Bras. Zootec. 47:e20160390 10.1590/rbz4720160390 [DOI] [Google Scholar]
- Baker N. L., Hunt K. J., Stevens D. R., Jarai G., Rosen G. D., Klein R. L., et al. (2018). Association between inflammatory markers and progression to kidney dysfunction: examining different assessment windows in patients with type 1 diabetes. Diabetes Care 41, 128–135. 10.2337/dc17-0867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baldassarre M. P. A., Andersen A., Consoli A., Knop F. K., Vilsbøll T. (2018). Cardiovascular biomarkers in clinical studies of type 2 diabetes. Diabetes Obes. Metab. 20, 1350–1360. 10.1111/dom.13247 [DOI] [PubMed] [Google Scholar]
- Balog R. P., Bacher R., Chang P., Greenstein M., Jammalamadaka S., Javitz H., et al. (2019). Development of a biodosimeter for radiation triage using novel blood protein biomarker panels in humans and non-human primates. Int. J. Radiat. Biol. 10.1080/09553002.2018.1532611. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- Bandara I. A., Baltatzis M., Sanyal S., Siriwardena A. K. (2018). Evaluation of tumor M2-pyruvate kinase (Tumor M2-PK) as a biomarker for pancreatic cancer. World J. Surg. Oncol. 16:56. 10.1186/s12957-018-1360-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bang C., Thum T. (2012). Exosomes: new players in cell–cell communication. Int J Biochem. Cell Biol. 44, 2060–2064. 10.1016/j.biocel.2012.08.007 [DOI] [PubMed] [Google Scholar]
- Barrera G., Pizzimenti S., Daga M., Dianzani C., Arcaro A., Cetrangolo G. P., et al. (2018). Lipid peroxidation-derived aldehydes, 4-hydroxynonenal and malondialdehyde in aging-related disorders. Antioxidants 7:102. 10.3390/antiox7080102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barry-Heffernan C., Ekena J., Dowling S., Pinkerton M. E., Viviano K. (2019). Biomarkers of oxidative stress as an assessment of the redox status of the liver in dogs. J. Vet. Intern. Med. 33, 611–617. 10.1111/jvim.15443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartel D. P. (2000). MicroRNAs: genomics, biogenesis, mechanism, and function. Cell 116, 281–297. 10.1016/s0092-8674(04)00045-5 [DOI] [PubMed] [Google Scholar]
- Bartoli F., Crocamo C., Trotta G., Bava M., Capuzzi E., Castagna G., et al. (2018). Testing the role of the antioxidant uric acid as a biomarker of suicidal ideation in subjects with major affective disorders: an exploratory study. Gen. Hosp. Psychiatry 51, 128–129. 10.1016/j.genhosppsych.2017.09.002 [DOI] [PubMed] [Google Scholar]
- Bartsch H., Arab K., Nair J. (2011). Biomarkers for hazard identification in humans. Environ. Health 10:S11. 10.1186/1476-069X-10-S1-S11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basnyat B. (2018). The potential usefulness of serum biomarkers in high-altitude medicine. J. Travel Med. 25, 1–2. 10.1093/jtm/tay083 [DOI] [PubMed] [Google Scholar]
- Basu S., Eriksson M. (2001). Retinol palmitate counteracts oxidative injury during experimental septic shock. Ann. Acad. Med. Singapore 30, 265–269. [PubMed] [Google Scholar]
- Bausero M., Gastpar R., Multhoff G., Asea A. (2005). Alternative mechanism by which IFN-γ enhances tumor recognition: active release of heat shock protein 72. J Immunol. 175, 2900–2912. 10.4049/jimmunol.175.5.2900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bayraml G., Ulutas B. (2008). Acute phase protein response in dogs with experimentally induced gastric mucosal injury. Vet. Clin. Pathol. 37, 312–316. 10.1111/j.1939-165X.2008.00060.x [DOI] [PubMed] [Google Scholar]
- Beker B. M., Corleto M. G., Fieiras C., Musso C. G. (2018). Novel acute kidney injury biomarkers: their characteristics, utility and concerns. Int. Urol. Nephrol. 50, 705–713. 10.1007/s11255-017-1781-x [DOI] [PubMed] [Google Scholar]
- Benoist d'Azy C., Pereira B., Chiambaretta F., Dutheil F. (2016). Oxidative and anti-oxidative stress markers in chronic glaucoma: asystematic review and meta-analysis. PLoS ONE 11:e0166915 10.1371/journal.pone.0166915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berezin A. (2018). Circulating biomarkers in heart failure: diagnostic and prognostic importance. J. Lab. Precis. Med. 3:36 10.21037/jlpm.2018.03.13 [DOI] [Google Scholar]
- Berger W., Mendlowicz M. V., Marques-Portella C., Kinrys G., Fontenelle L. F., Marmar C. R., et al. (2009). Pharmacologic alternatives to antidepressants in posttraumatic stress disorder: a systematic review. Prog. Neuropsychopharmacol. Biol. Psychiatry 33, 169–180. 10.1016/j.pnpbp.2008.12.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bevan R. J., Durand M. F., Hickenbotham P. T., Kitas G. D., Patel P. R., Podmore I. D., et al. (2003). Validation of a novel ELISA for measurement of MDA-LDL in human plasma. Free Radic. Biol. Med. 35, 517–527. 10.1016/s0891-5849(03)00359-9 [DOI] [PubMed] [Google Scholar]
- Beyazit F., Pek E. (2018). Effects of vitamin B12, folate, uric acid, and serum biomarkers of inflammation on bone mineral density in postmenopausal women. Prz. Menopauzalny 17, 69–76. 10.5114/pm.2018.77305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bílek R., Vlček P., Šafarík L., Michalský D., Novák K., Dušková J., et al. (2019). Chromogranin A in the laboratory diagnosis of Pheochromocytoma and Paraganglioma. Cancers (Basel) 11:E586. 10.3390/cancers11040586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bisson J. I., Cosgrove S., Lewis C., Robert N. P. (2015). Post-traumatic stress disorder. BMJ 351:h6161 10.1136/bmj.h6161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blankenberg S., Rupprecht H. J., Bickel C., Torzewski M., Hafner G., Tiret L., et al. (2003). Glutathione peroxidise activity and cardiovascular events in patients with coronary artery disease. N. Engl. J. Med. 349, 1605–1613. 10.1056/NEJMoa030535 [DOI] [PubMed] [Google Scholar]
- Böbel T. S., Hackl S. B., Langgartner D., Jarczok M. N., Rohleder N., Rook G. A., et al. (2018). Less immune activation following social stress in rural vs. urban participants raised with regular or no animal contact, respectively. Proc. Natl. Acad. Sci. U.S.A. 115, 5259–5264. 10.1073/pnas.1719866115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boenzi S., Diodato D. (2018). Biomarkers for mitochondrial energy metabolism diseases. Essays Biochem. 62, 443–454. 10.1042/EBC20170111 [DOI] [PubMed] [Google Scholar]
- Broedbaek K., Hilsted L. (2016). Chromogranin A as biomarker in diabetes. Biomarkers Med. 10, 1181–1189. 10.2217/bmm-2016-0091 [DOI] [PubMed] [Google Scholar]
- Brown C. W. (2016). Salivary cortisol as a measure of stress reactivity, in Adolescents with psychiatric disorders. Yale Medicine Thesis Digital Library, 2041. Available online at: https://elischolar.library.yale.edu/ymtdl/2041
- Browning J. D., Horton J. D. (2004). Molecular mediators of hepatic steatosis and liver injury. J. Clin. Invest. 114, 147–152. 10.1172/JCI22422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruey J. M., Ducasse C., Bonniaud P., Ravagnan L., Susin S. A., Diaz-Latoud C., et al. (2000). Hsp27 negatively regulates cell death by interacting with cytochrome C. Nat. Cell Biol. 2, 645–652. 10.1038/35023595 [DOI] [PubMed] [Google Scholar]
- Brzozowski J. S., Bond D. R., Jankowski H., Goldie B. J., Burchell R., Naudin C., et al. (2018). Extracellular vesicles with altered tetraspanin CD9 and CD151 levels confer increased prostate cell motility and invasion. Sci. Rep. 8:8822. 10.1038/s41598-018-27180-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buehler P. W., Abraham B., Vallelian F., Linnemayr C., Pereira C. P., Cipollo J. F., et al. (2009). Haptoglobin preserves the CD163 hemoglobin scavenger pathway by shielding hemoglobin from peroxidative modification. Blood 113, 2578–2586. 10.1182/blood-2008-08-174466 [DOI] [PubMed] [Google Scholar]
- Cai L., Kaneko S., Morita E. (2018). Changes in salivary chromogranin A levels in adults with atopic dermatitis are correlated with changes in their condition. J. Dermatol. 45, 554–559. 10.1111/1346-8138.14277 [DOI] [PubMed] [Google Scholar]
- Calabrese V., Mancuso C., Sapienza M., Puleo E., Calafato S., Cornelius C., et al. (2007). Oxidative stress and cellular stress response in diabetic nephropathy. Cell Stress Chaperones 12, 299–306. 10.1379/csc-270.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calderwood S. K., Khaleque M. A., Sawyer D. B., Ciocca D. R. (2006). Heat shock proteins in cancer: chaperones of tumorigenesis. Trends Biochem. Sci. 31, 164–172. 10.1016/j.tibs.2006.01.006 [DOI] [PubMed] [Google Scholar]
- Campbell F. M., Waterston M., Andresen L. O., Sorensen N. S., Heegaard P. M., Eckersall P. D. (2005). The negative acute phase response of serum transthyretin following Streptococcus suis infection in the pig. Vet. Res. 36, 657–664. 10.1051/vetres:2005017 [DOI] [PubMed] [Google Scholar]
- Campion C. G., Sanchez-Ferras O., Batchu S. N. (2017). Potential role of serum and urinary biomarkers in diagnosis and prognosis of diabetic nephropathy. Can. J. Kidney Health Dis. 4:2054358117705371. 10.1177/2054358117705371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carboni L. (2013). Peripheral biomarkers in animal models of major depressive disorder. Dis. Markers 35, 33–41. 10.1155/2013/284543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlomagno N., Incollingo P., Tammaro V., Peluso G., Rupealta N., Chiacchio G., et al. (2017). Diagnostic, predictive, prognostic, and therapeutic molecular biomarkers in third millennium: a breakthrough in gastric cancer. BioMed. Res. Int. 2017:7869802. 10.1155/2017/7869802 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carocho M., Ferreira I., Morales P., Soković M. (2018). Antioxidants and prooxidants: effects on health and aging. Oxid. Med. Cell Longev. 2018:1472708. 10.1155/2018/1472708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castillo C., Hernandez J., Bravo A., Lopez-Alonso M., Pereira V., Benedito J. L. (2005). Oxidative status during late pregnancy and early lactation in dairy cows. Vet. J. 169, 286–292. 10.1016/j.tvjl.2004.02.001 [DOI] [PubMed] [Google Scholar]
- Castillo C., Hernandez J., Valverde I., Pereira V., Sotillo J., Alonso M. L., et al. (2006). Plasma malonaldehyde (MDA) and total antioxidant status (TAS) during lactation in dairy cows. Res. Vet. Sci. 80, 133–139. 10.1016/j.rvsc.2005.06.003 [DOI] [PubMed] [Google Scholar]
- Ceciliani F., Ceron J. J., Eckersall P. D., Sauerwein H. (2012). Acute phase proteins in ruminants. J. Proteomics 75, 4207–4231. 10.1016/j.jprot.2012.04.004 [DOI] [PubMed] [Google Scholar]
- Celi P., Verlhac V., Pérez Calvo E., Schmeisser J., Kluenter A. M. (2018). Biomarkers of gastrointestinal functionality in animal nutrition and health. Anim. Feed Sci. Tech. 250, 9–31. 10.1016/j.anifeedsci.2018.07.012 [DOI] [Google Scholar]
- Ceron J. J., Eckersall P. D., Martynez-Subiela S. (2005). Acute phase proteins in dogs and cats: current knowledge and future perspectives. Vet. Clin. Pathol. 34, 85–99. 10.1111/j.1939-165X.2005.tb00019.x [DOI] [PubMed] [Google Scholar]
- Cesano A., Warren S. (2018). Bringing the next generation of immuno-oncology biomarkers to the clinic. Biomedicines 6:14. 10.3390/biomedicines6010014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chacko S., Haseeb S., Glover B. M., Wallbridge D., Harper A. (2017). The role of biomarkers in the diagnosis and risk stratification of acute coronary syndrome. Fut. Sci. 4:FSO251. 10.4155/fsoa-2017-0036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chakrabarti S., Jana M., Roy A., Pahan K. (2018). Upregulation of suppressor of cytokine signaling 3 in microglia by cinnamic acid. Curr. Alzheimer Res. 15, 894–904. 10.2174/1567205015666180507104755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charette S. J., Landry J. (2000). The interaction of HSP27 with Daxx identifies a potential regulatory role of HSP27 in Fas-induced apoptosis. Ann. N. Y. Acad. Sci. 926, 126–131. 10.1111/j.1749-6632.2000.tb05606.x [DOI] [PubMed] [Google Scholar]
- Charmpilas N., Kyriakakis E., Tavernarakis N. (2017). Small heat shock proteins in ageing and age-related diseases. Cell Stress Chaperones 22, 481–492. 10.1007/s12192-016-0761-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chauhan R. N., Kapoor M., Prabha Singh L., Gupta R., Chand Meena R., Tulsawani R., et al. (2017). Heat stress induced neuroinflammation and aberration in monoamine levels in hypothalamus is associated with temperature dysregulation. Neuroscience 358, 79–92. 10.1016/j.neuroscience.2017.06.023 [DOI] [PubMed] [Google Scholar]
- Chen G. D., Zhang J. L., Chen Y. T., Zhang J. X., Wang T., Zeng Q. Y. (2018). Insulin alleviates mitochondrial oxidative stress involving upregulation of superoxide dismutase 2 and uncoupling protein 2 in septic acute kidney injury. Exp. Ther. Med. 15, 3967–3975. 10.3892/etm.2018.5890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen J., Tellez G., Richards J. D., Escobar J. (2015). Identification of potential biomarkers for gut barrier failure in broiler chickens. Front. Vet. Sci. 2:14. 10.3389/fvets.2015.00014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen K., Suh J., Carr A. C., Morrow J. D., Zeind J., Frei B. (2000). Vitamin C suppresses oxidative lipid damage in vivo, even in the presence of iron overload. Am. J. Physiol. Endocrinol. Metab. 279, E1406–E1412. 10.1152/ajpendo.2000.279.6.E1406 [DOI] [PubMed] [Google Scholar]
- Chen X., Wu G., Schwarzschild M. A. (2012). Urate in Parkinson's disease: more than a biomarker? Curr. Neurol. Neurosci. Rep. 12, 367–375. 10.1007/s11910-012-0282-7 [DOI] [PubMed] [Google Scholar]
- Cheng Y., Li Z., He S., Tian Y., He F., Li W. (2018). Elevated heat shock proteins in bipolar disorder patients with hypothalamic pituitary adrenal axis dysfunction. Medicine 97, e11089. 10.1097/MD.0000000000011089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chennaoui M., Bougard C., Drogou C., Langrume C., Miller C., Gomez-Merino D., et al. (2016). Stress biomarkers, mood states, and sleep during a major competition: success and failure athlete's profile of high-level swimmers. Front. Physiol. 7:94. 10.3389/fphys.2016.00094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheung E. Y., de Willige S. U., Vos H. L., Leebeek F. W., Dippel D. W., Bertina R. M., et al. (2008). Fibrinogen gamma' in ischemic stroke: a case-control study. Stroke 39, 1033–1035. 10.1161/STROKEAHA.107.495499 [DOI] [PubMed] [Google Scholar]
- Chou R., Gore J. L., Buckley D., Fu R., Gustafson K., Griffin J. C., et al. (2015). Urinary biomarkers for diagnosis of bladder cancer: asystematic review and meta-analysis. Ann. Intern. Med. 163, 922–931. 10.7326/M15-0997 [DOI] [PubMed] [Google Scholar]
- Chowdhury P., Kehl D., Choudhary R., Maisel A. (2013). The use of biomarkers in the patient with heart failure. Curr. Cardiol. Rep. 15:372. 10.1007/s11886-013-0372-4 [DOI] [PubMed] [Google Scholar]
- Cimmino R., Barone C., Claps S., Varricchio E., Rufrano D., Caroprese M., et al. (2018). Effects of dietary supplementation with polyphenols on meat quality in Saanen goat kids. BMC Vet. Res. 14:181. 10.1186/s12917-018-1513-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cipriani S., Chen X., Schwarszchild M. A. (2010). Urate: a novel biomarker of Parkinson's disease risk, diagnosis and prognosis. Biomarkers Med. 4, 701–712. 10.2217/bmm.10.94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark R. J., Craig M. P., Agrawal S., Kadakia M. (2018). MicroRNA involvement in the onset and progression of Barrett's esophagus: a systematic review. Oncotarget 9, 8179–8196. 10.18632/oncotarget.24145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clow A., Hucklebridge F., Thorn L. (2010). The cortisol awakening response in context. Int. Rev. Neurobiol. 93, 153–175. 10.1016/S0074-7742(10)93007-9 [DOI] [PubMed] [Google Scholar]
- Coca S. G., Yalavarthy R., Concato J., Parikh C. R. (2008). Biomarkers for the diagnosis and risk stratification of acute kidney injury: systematic review. Kidney Int. 73, 1008–1016. 10.1038/sj.ki.5002729 [DOI] [PubMed] [Google Scholar]
- Coculescu B. I., Dincă G. V., Bălăet C., Manole G., Bălăet M., Stocheci C. M. (2018). Myeloperoxidase, a possible biomarker for the early diagnosis of cardiac diastolic dysfunction with preserved ejection fraction. J. Enzyme Inhib. Med. Chem. 33, 1292–1298. 10.1080/14756366.2018.1499626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colombo G., Reggiani F., Cucchiari D., Portinaro N. M., Giustarini D., Rossi R., et al. (2017). Plasma protein-bound di-tyrosines as biomarkers of oxidative stress in end stage renal disease patients on maintenance hemodialysis. BBA Clin. 7, 55–63. 10.1016/j.bbacli.2016.12.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conner J. G., Eckersall P. D., Wiseman A., Aitchison T. C., Douglas T. A. (1998). Bovine acute phase response following turpentine injection. Res. Vet. Sci. 44, 82–88. 10.1016/0034-5288(88)90018-5 [DOI] [PubMed] [Google Scholar]
- Contreras-Aguilar M. D., Martínez-Subiela S., Cerón J. J., Martín-Cuervo M., Tecles F., Escribano D. (2019). Salivary alpha-amylase activity and concentration in horses with acute abdominal disease: association with outcome. Equine Vet. J. 51, 569–574. 10.1111/evj.13066 [DOI] [PubMed] [Google Scholar]
- Costa L. G., de Laat R., Tagliaferri S., Pellacani C. (2014). A mechanistic view of polybrominated diphenyl ether (PBDE) developmental neurotoxicity. Toxicol. Lett. 230, 282–294. 10.1016/j.toxlet.2013.11.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cova I., Priori A. (2018). Diagnostic biomarkers for Parkinson's disease at a glance: where are we? J. Neural. Transm. (Vienna) 125, 1417–1432. 10.1007/s00702-018-1910-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cray C., Zaias J., Altman N. H. (2009). Acute phase response in animals: a review. Comp. Med. 59, 517–526. [PMC free article] [PubMed] [Google Scholar]
- Cristalli D. O., Arnal N., Marra F. A., De Alaniz M. J. T., Marra C. A. (2012). Peripheral markers in neurodegenerative patients and their first-degree relatives. J. Neurol. Sci. 314, 48–56. 10.1016/j.jns.2011.11.001 [DOI] [PubMed] [Google Scholar]
- Cuffe J. S., Xu Z. C., Perkins A. V. (2017). Biomarkers of oxidative stress in pregnancy complications. Biomark. Med. 11, 295–306. 10.2217/bmm-2016-0250 [DOI] [PubMed] [Google Scholar]
- Cumpstey A. F., Minnion M., Fernandez B. O., Mikus-Lelinska M., Mitchell K., Martin D. S., et al. (2019). Pushing arterial-venous plasma biomarkers to new heights: a model for personalised redox metabolomics? Redox. Biol. 21:101113. 10.1016/j.redox.2019.101113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cura-Esquivel I., Cordero-Pérez P., Torres-González L., Muñoz-Espinosa L. E. (2018). Acute phase markers in obese children and adolescents with metabolic disorders. Arch. Argent Pediatr. 116, 275–282. 10.5546/aap.2018.eng.275 [DOI] [PubMed] [Google Scholar]
- Curhan G. (2005). Cystatin C: a marker of renal function or something more? Clin. Chem. 51, 293–294. 10.1373/clinchem.2004.044388 [DOI] [PubMed] [Google Scholar]
- Cymbaluk-Płoska A., Chudecka-Głaz A., Pius-Sadowska E., Sompolska-Rzechuła A., Machalinski B., Menkiszak J. (2018). Circulating serum level of visfatin in patients with endometrial cancer. BioMed. Res. Int. 2018:8576179. 10.1155/2018/8576179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czerska M., Zielinski M., Gromadzinska J. (2016). Isoprostanes – a novel major group of oxidative stress markers. Int. J. Occup. Med. Environ. Health 29, 179–190. 10.13075/ijomeh.1896.00596 [DOI] [PubMed] [Google Scholar]
- Dada T., Mittal D., Mohanty K., Faiq M. A., Bhat M. A., Yadav R. K., et al. (2018). Mindfulness meditation reduces intraocular pressure, lowers stress biomarkers and modulates gene expression in glaucoma: a randomized controlled trial. J. Glaucoma 27, 1061–1067. 10.1097/IJG.0000000000001088 [DOI] [PubMed] [Google Scholar]
- Dadar M., Dhama K., Iqbal H., Munjal A., Khandia R., Karthik K., et al. (2016). Molecular signatures of biomarkers in cancer development, diagnosis, and its prognostic accuracy. Curr. Biomarkers 6, 89–96. 10.2174/2468422807666170210164253 [DOI] [Google Scholar]
- Dalle-Donne I., Rossi R., Giustarini D., Milzani A., Colombo R. (2003). Protein carbonyl groups as biomarkers of oxidative stress. Clin. Chim. Acta 329, 23–38. 10.1016/s0009-8981(03)00003-2 [DOI] [PubMed] [Google Scholar]
- D'amico M. A., Ghinassi B., Izzicupo P., Manzoli L., Di Baldassarre A. (2014). Biological function and clinical relevance of chromogranin A and derived peptides. Endocr. Connect. 3, R45–R54. 10.1530/EC-14-0027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daskalakis N. P., Cohen H., Nievergelt C. M., Baker D. G., Buxbaum J. D., Russo S. J., et al. (2016). New translational perspectives for blood-based biomarkers of PTSD: from glucocorticoid to immune mediators of stress susceptibility. Exp. Neurol. 284, 133–140. 10.1016/j.expneurol.2016.07.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Rosa S., Arcidiacono B., Chiefari E., Brunetti A., Indolfi C., Foti D. P. (2018). Type 2 diabetes mellitus and cardiovascular disease: genetic and epigenetic links. Front Endocrinol. 9:2. 10.3389/fendo.2018.00002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deaton C. M., Marlin D. J., Smith N. C., Harris P. A., Schroter R. C., Kelly F. J. (2004). Antioxidant supplementation in horses affected by recurrent airway obstruction. J Nutr. 134, S2065–S2067. 10.1093/jn/134.8.2065S [DOI] [PubMed] [Google Scholar]
- Deaton C. M., Marlin D. J., Smith N. C., Roberts C. A., Harris P. A., Schroter R. C., et al. (2005). Antioxidant and inflammatory responses of healthy horses and horses affected by recurrent airway obstruction to inhaled ozone. Equine Vet. J. 37, 243–249. 10.2746/0425164054530605 [DOI] [PubMed] [Google Scholar]
- Deftos L. J. (1991). Chromogranin A: its role in endocrine function and as an endocrine and neuroendocrine tumor marker. Endocr. Rev. 12, 181–187. 10.1210/edrv-12-2-181 [DOI] [PubMed] [Google Scholar]
- Delafoy L., Gelot A., Ardid D., Eschalier A., Bertrand C., Doherty A. M., et al. (2006). Interactive involvement of brain derived neurotrophic factor, nerve growth factor, and calcitonin gene related peptide in colonic hypersensitivity in the rat. Gut 55, 940–945. 10.1136/gut.2005.064063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deneva T., Ianakiev Y., Keskinova D. (2019). Burnout Syndrome in physicians-psychological assessment and biomarker research. Medicina (Kaunas) 55:E209. 10.3390/medicina55050209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhawan V., Sharma I., Mahajan N., Sangwan S. M., Jain S. (2014). Implication of endothelin-2 and oxidative stress biomarkers in essential hypertension. J. Hypertens. 3:170 10.4172/2167-1095.1000170 [DOI] [Google Scholar]
- Di Giacinto P., Rota F., Rizza L., Campana D., Isidori A., Lania A., et al. (2018). Chromogranin A: from laboratory to clinical aspects of patients with neuroendocrine tumors. Int. J. Endocrinol. 2018:8126087. 10.1155/2018/8126087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dobsa L., Edozien K. C. (2013). Copeptin and its potential role in diagnosis and prognosis of various diseases. Biochem. Med. 23, 172–190. 10.11613/BM.2013.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donaldson G. P., Ladinsky M. S., Yu K. B., Sanders J. G., Yoo B. B., Chou W. C., et al. (2018). Gut microbiota utilize immunoglobulin A for mucosal colonization. Science 360, 795–800. 10.1126/science.aaq0926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dookhun M. N., Sun Y., Zou H., Cao X., Lu X. (2018). Classification of new biomarkers of dilated cardiomyopathy based on pathogenesis-an update. Health 10, 300–312. 10.4236/health.2018.103024 [DOI] [Google Scholar]
- Dounousi E., Papavasiliou E., Makedou A., Ioannou K., Katopodis K. P., Tselepis A., et al. (2006). Oxidative stress is progressively enhanced with advancing stages of CKD. Am. J. Kidney Dis. 48, 752–760. 10.1053/j.ajkd.2006.08.015 [DOI] [PubMed] [Google Scholar]
- Drolz A., Horvatits T., Roedl K., Rutter K., Brunner R., Zauner C., et al. (2018). Acid-base status and its clinical implications in critically ill patients with cirrhosis, acute-on-chronic liver failure and without liver disease. Ann. Int. Care 8:48. 10.1186/s13613-018-0391-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drozdz D., Kwinta P., Sztefko K., Kordon Z., Drozdz T., Łatka M., et al. (2016). Oxidative stress biomarkers and left ventricular hypertrophy in children with chronic kidney disease. Oxid Med. Cellular Long. 2016:7520231. 10.1155/2016/7520231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drucker E., Krapfenbauer K. (2013). Pitfalls and limitations in translation from biomarker discovery to clinical utility in predictive and personalised medicine. EPMA J. 4:2013. 10.1186/1878-5085-4-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ducatelle R., Goossens E., De Meyer F., Eeckhaut V., Antonissen G., Haesebrouck F., et al. (2018). Biomarkers for monitoring intestinal health in poultry: present status and future perspectives. Vet. Res. 49:43. 10.1186/s13567-018-0538-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dudakov J. A., Hanash A. M., van den Brink M. R. (2015). Interleukin-22: immunobiology and pathology. Annu. Rev. Immunol. 33, 747–785. 10.1146/annurev-immunol-032414-112123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton P. (2006). Protein thiol oxidation in health and disease: techniques for measuring disulfides and related modifications in complex protein mixtures. Free Rad. Biol. Med. 40, 1889–1899. 10.1016/j.freeradbiomed.2005.12.037 [DOI] [PubMed] [Google Scholar]
- Eckersall P. D., Bell R. (2010). Acute phase proteins: biomarkers of infection and inflammation in veterinary medicine. Vet. J. 2010, 18523–18527. 10.1016/j.tvjl.2010.04.009 [DOI] [PubMed] [Google Scholar]
- Eckersall P. D., Lawson F. P., Bence L., Waterston M. M., Lang T. L., Donachie W., et al. (2007). Acute phase protein response in an experimental model of ovine caseous lymphadenitis. BMC Vet. Res. 3:35. 10.1186/1746-6148-3-35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eckersall P. D., Young F. J., McComb C., Hogarth C. J., Safi S., Fitzpatrick J. L., et al. (2001). Acute phase proteins in serum and milk from dairy cows with clinical mastitis. Vet. Rec. 148, 35–41. 10.1136/vr.148.2.35 [DOI] [PubMed] [Google Scholar]
- Edkins A. L., Price J. T., Pockley A. G., Blatch G. L. (2017). Heat shock proteins as modulators and therapeutic targets of chronic disease: an integrated perspective. Philos. Trans. R. Soc. Lond. B Biol. Sci. 373:20160521. 10.1098/rstb.2016.0521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egawa M., Haze S., Gozu Y., Hosoi J., Onodera T., Tojo Y., et al. (2018). Evaluation of psychological stress in confined environments using salivary, skin, and facial image parameters. Sci. Rep. 8:8264. 10.1038/s41598-018-26654-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- El Golli-Bennour E., Bacha H. (2011). Hsp70 expression as biomarkers of oxidative stress: mycotoxins exploration. Toxicology 287, 1–7. 10.1016/j.tox.2011.06.002 [DOI] [PubMed] [Google Scholar]
- El-Horany H. E., Abd-Ellatif R. N., Watany M., Hafez Y. M., Okda H. I. (2017). NLRP3 expression and urinary HSP72 in relation to biomarkers of inflammation and oxidative stress in diabetic nephropathy patients. IUBMB Life 69, 623–630. 10.1002/iub.1645 [DOI] [PubMed] [Google Scholar]
- Escribano D., Ko H. L., Chong Q., Llonch L., Manteca X., Llonch P. (2019). Salivary biomarkers to monitor stress due to aggression after weaning in piglets. Res. Vet. Sci. 123, 178–183. 10.1016/j.rvsc.2019.01.014 [DOI] [PubMed] [Google Scholar]
- Estrada V., Monge S., Gómez-Garre M. D., Sobrino P., Masia M., Berenguer J., et al. (2016). Relationship between plasma bilirubin level and oxidative stress markers in HIV-infected patients on atazanavir vs. efavirenz-based antiretroviral therapy. HIV Med. 17, 653–661. 10.1111/hiv.12368 [DOI] [PubMed] [Google Scholar]
- Ewert A., Chang Y. (2018). Levels of nature and stress response. Behav. Sci. 8:49. 10.3390/bs8050049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fam S. S., Morrow J. D. (2003). The isoprostanes: unique products of arachidonic acid oxidation – a review. Curr. Med. Chem. 10, 1723–1740. 10.2174/0929867033457115 [DOI] [PubMed] [Google Scholar]
- Farah R., Haraty H., Salame Z., Fares Y., Ojcius D. M., Said Sadier N. (2018). Salivary biomarkers for the diagnosis and monitoring of neurological diseases. Biomed. J. 41, 63–87. 10.1016/j.bj.2018.03.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- FDA-NIH Biomarker Working Group (2016). BEST (Biomarkers, EndpointS, and other Tools) Resource. Silver Spring, MD; Bethesda, MD: Food and Drug Administration (US); National Institutes of Health (US). [PubMed] [Google Scholar]
- Ferguson M. A., Vaidya V. S., Waikar S. S., Collings F. B., Sunderland K. E., Gioules C. J., et al. (2010). Urinary liver-type fatty acid-binding protein predicts adverse outcomes in acute kidney injury. Kidney Int. 77, 708–714. 10.1038/ki.2009.422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernando N., Wickremesinghe S., Niloofa R., Rodrigo C., Karunanayake L., de Silva H. J., et al. (2016). Protein carbonyl as a biomarker of oxidative stress in severe leptospirosis, and its usefulness in differentiating leptospirosis from dengue infections. PLoS ONE 11:e0156085. 10.1371/journal.pone.0156085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernie K. J., Shutt J. L., Mayne G., Hoffman D., Letcher R. J., Drouillard K. G., et al. (2005). Exposure to polybrominated diphenyl ethers (PBDEs): changes in thyroid, vitamin A, glutathione homeostasis, and oxidative stress in American kestrels (Falco sparverius). Toxicol. Sci. 88, 375–383. 10.1093/toxsci/kfi295 [DOI] [PubMed] [Google Scholar]
- Ferroni P., Santilli F., Cavaliere F., Simeone P., Costarelli L., Liani R., et al. (2017). Oxidant stress as a major determinant of platelet activation in invasive breast cancer. Int. J. Cancer 140, 696–704. 10.1002/ijc.30488 [DOI] [PubMed] [Google Scholar]
- Filaire E., Massart A., Nourrit D., Rama L., Teixeira A. (2010). Lecturing to 200 students and its effects on saliva flow rate, immunoglobulin a, lysozyme and salivary markers of adrenal activation. Biomed. Res. 21, 33–44. [Google Scholar]
- Finno C. J., Estell K. E., Winfield L., Katzman S., Bordbari M. H., Burns E. N., et al. (2018). Lipid peroxidation biomarkers for evaluating oxidative stress in equine neuroaxonal dystrophy. J. Vet. Int. Med. 32, 1740–1747. 10.1111/jvim.15241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fioranelli M., Bottaccioli A. G., Bottaccioli F., Bianchi M., Rovesti M., Roccia M. G. (2018). Stress and inflammation in coronary artery disease: a review psychoneuroendocrineimmunology-based. Front. Immunol. 9:2031. 10.3389/fimmu.2018.02031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fleming W. E., Holty J. C., Bogan R. K., Hwang D., Ferouz-Colborn A. S., Budhiraja R., et al. (2018). Use of blood biomarkers to screen for obstructive sleep apnea. Nat. Sci. Sleep 10, 159–167. 10.2147/NSS.S164488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flores V. A., Vanhie A., Dang T., Taylor H. S. (2018). Progesterone receptor status predicts response to progestin therapy in endometriosis. J. Clin. Endocrinol. Metab. 103, 4561–4568. 10.1210/jc.2018-01227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fortunato A. K., Pontes W. M., De Souza D. M. S. D., Prazeres J., Marcucci-Barbosa L. S., Santos J., et al. (2018). Strength training session induces important changes on physiological, immunological, and inflammatory biomarkers. J. Immunol. Res. 2018:9675216. 10.1155/2018/9675216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franken C., Koppen G., Lambrechts N., Govarts E., Bruckers L., Den Hond E., et al. (2017). Environmental exposure to human carcinogens in teenagers and the association with DNA damage. Environ. Res. 152, 165–174. 10.1016/j.envres.2016.10.012 [DOI] [PubMed] [Google Scholar]
- Frijhoff J., Winyard P. G., Zarkovic N., Davies S. S., Stocker R., Cheng D., et al. (2015). Clinical relevance of biomarkers of oxidative stress. Antioxid. Redox. Signal. 23, 1144–1170. 10.1089/ars.2015.6317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frustaci A., Neri M., Cesario A., Adams J. B., Domenici E., Dalla Bernardina B., et al. (2012). Oxidative stress-related biomarkers in autism: systematic review and meta-analyses. Free Radic. Biol. Med. 52, 2128–2141. 10.1016/j.freeradbiomed.2012.03.011 [DOI] [PubMed] [Google Scholar]
- Fukai T., Folz R. J., Landmesser U., Harrison D. G. (2002). Extracellular superoxide dismutase and cardiovascular disease. Cardiovasc. Res. 55, 239–249. 10.1016/s0008-6363(02)00328-0 [DOI] [PubMed] [Google Scholar]
- Fukuda M. E., Iwadate Y., Machida T., Hiwasa T., Nimura Y., Nagai Y., et al. (2005). Cathepsin D is a potential serum marker for poor prognosis in glioma patients. Cancer Res. 65, 5190–5194. 10.1158/0008-5472.CAN-04-4134 [DOI] [PubMed] [Google Scholar]
- Gabai G., De Luca E., Miotto G., Zin G., Stefani A., Da Dalt L., et al. (2019). Relationship between protein oxidation biomarkers and uterine health in dairy cows during the postpartum period. Antioxidants (Basel) 8:E21. 10.3390/antiox8010021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gabriela G., Belén M. M., Romina D., Jose C. M., Susana L., Juan B., et al. (2019). Biomarkers of oxidative stress and inflammation in Chagasic myocardiopathy. Open Biomarkers J. 9, 17–23. 10.2174/1875318301808010017 [DOI] [Google Scholar]
- Ganheim C., Alenius S., Persson Waller K. (2007). Acute phase proteins as indicators of calf herd health. Vet. J. 173, 645–651. 10.1016/j.tvjl.2006.01.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- García-Blanco A., Baquero M., Vento M., Gil E., Bataller L., Chafer-Pericas C. (2017b). Potential oxidative stress biomarkers of mild cognitive impairment due to Alzheimer disease. J. Neurol. Sci. 373, 295–302. 10.1016/j.jns.2017.01.020 [DOI] [PubMed] [Google Scholar]
- García-Blanco A., Diago V., De La Cruz V. S., Hervás D., Cháfer-Pericás C., Vento M. (2017a). Can stress biomarkers predict preterm birth in women with threatened preterm labor? Psychoneuroendocrinology 83, 19–24. 10.1016/j.psyneuen.2017.05.021 [DOI] [PubMed] [Google Scholar]
- Ge W. H., Lin Y., Li S., Zong X., Ge Z. C. (2018). Identification of biomarkers for early diagnosis of acute myocardial infarction. J. Cell Biochem. 119, 650–658. 10.1002/jcb.26226 [DOI] [PubMed] [Google Scholar]
- Gebhardt C., Hirschberger J., Rau S., Arndt G., Krainer K., Schweigert F. J., et al. (2009). Use of C-reactive protein to predict outcome in dogs with systemic inflammatory response syndrome or sepsis. J. Vet. Emerg. Crit. Care 19, 450–458. 10.1111/j.1476-4431.2009.00462.x [DOI] [PubMed] [Google Scholar]
- Gehlken C., Suthahar N., Meijers W. C., de Boer R. A. (2018). Galectin-3 in heart failure: an update of the last 3 years. Heart Fail Clin. 14, 75–92. 10.1016/j.hfc.2017.08.009 [DOI] [PubMed] [Google Scholar]
- Gheita T. A., Kenawy S. A. (2014). Measurement of malondialdehyde, glutathione and glutathione peroxidase in SLE patients. Methods Mol. Biol. 1134, 193–199. 10.1007/978-1-4939-0326-9_14 [DOI] [PubMed] [Google Scholar]
- Ghosh S., Khan N. I., Tsavalas J. G., Song E. (2018). Selective detection of lysozyme biomarker utilizing large area chemical vapor deposition-grown graphene-based field-effect transistor. Front. Bioeng. Biotechnol. 6:29. 10.3389/fbioe.2018.00029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giampaolo B., Angelica M., Antonio S. (2002). Chromogranin ‘A' in normal subjects, essential hypertensives and adrenalectomized patients. Clin. Endocrinol. (Oxf). 57, 41–50. 10.1046/j.1365-2265.2002.01557.x [DOI] [PubMed] [Google Scholar]
- Gilad S., Meiri E., Yogev Y., Benjamin S., Lebanony D., Yerushalmi N., et al. (2008). Serum microRNAs are promising novel biomarkers. PLoS ONE 3:e3148. 10.1371/journal.pone.0003148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giustarini D., Tsikas D., Colombo G., Milzani A., Dalle-Donne I., Fanti P., et al. (2016). Pitfalls in the analysis of the physiological antioxidant glutathione (GSH) and its disulfide (GSSG) in biological samples: an elephant in the room. J. Chromatogr. B Analyt. Technol. Biomed. Life Sci. 1019, 21–28. 10.1016/j.jchromb.2016.02.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Godoy L. D., Rossignoli M. T., Pereira P. D., Garcia-Cairasco N., Umeoka E. H. D. L. (2018). A comprehensive overview on stress neurobiology: basic concepts and clinical implications. Front. Behav. Neurosci. 12:127. 10.3389/fnbeh.2018.00127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gohel V., Jones J. A., Wehler C. J. (2018). Salivary biomarkers and cardiovascular disease: a systematic review. Clin. Chem. Lab. Med. 56, 1432–1442. 10.1515/cclm-2017-1018 [DOI] [PubMed] [Google Scholar]
- Gómez-Serrano M., Camafeita E., Loureiro M., Peral B. (2018). Mitoproteomics: tackling mitochondrial dysfunction in human disease. Oxid. Med. Cell Longev. 2018:1435934. 10.1155/2018/1435934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gosmanova E. O., Le N.-A. (2011). Cardiovascular complications in CKD patients: role of oxidative stress. Cardiol. Res. Pract. 2011:156326. 10.4061/2011/156326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Góth L., Rass P., Páy A. (2004). Catalase enzyme mutations and their association with diseases. Mol. Diagn. 8, 141–149. 10.1007/BF03260057 [DOI] [PubMed] [Google Scholar]
- Goyal N., Kashyap B., Singh N. P., Kaur I. R. (2016). Neopterin and oxidative stress markers in the diagnosis of extrapulmonary tuberculosis. Biomarkers 7, 1–6. 10.1080/1354750X.2016.1265005 [DOI] [PubMed] [Google Scholar]
- Graham D. Y., Miftahussurur M. (2018). Helicobacter pylori urease for diagnosis of Helicobacter pylori infection: a mini review. J. Adv. Res. 13, 51–57. 10.1016/j.jare.2018.01.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greff M. J. E., Levine J. M., Abuzgaia A. M., Elzagallaai A. A., Rieder M. J., van Uum S. H. M. (2019). Hair cortisol analysis: an update on methodological considerations and clinical applications. Clin. Biochem. 63, 1–9. 10.1016/j.clinbiochem.2018.09.010 [DOI] [PubMed] [Google Scholar]
- Griffiths H. R., Moller L. (2002). Biomarkers. Mol Aspects Med. 23, 101–208. 10.1016/S0098-2997(02)00017-1 [DOI] [PubMed] [Google Scholar]
- Grignard E., Morin J., Vernet P., Drevet J. R. (2005). GPX5 orthologs of the mouse epididymis-restricted and sperm-bound selenium-independent glutathione peroxidase are not expressed with the same quantitative and spatial characteristics in large domestic animals. Theriogenology 64, 1016–1033. 10.1016/j.theriogenology.2005.01.008 [DOI] [PubMed] [Google Scholar]
- Groschl M. (2008). Current status of salivary hormone analysis. Clin. Chem. 54, 1759–1769. 10.1373/clinchem.2008.108910 [DOI] [PubMed] [Google Scholar]
- Gu S., Wang W., Wang F., Huang J. H. (2016). Neuromodulator and emotion biomarker for stress induced mental disorders. Neural Plast. 2016:2609128. 10.1155/2016/2609128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guerreiro S., Ponceau A., Toulorge D., Martin E., Alvarez-Fischer D., Hirsch E. C., et al. (2009). Protection of midbrain dopaminergic neurons by the end-product of purine metabolism uric acid: potentiation by low-level depolarization. J. Neurochem. 109, 1118–1128. 10.1111/j.1471-4159.2009.06040.x [DOI] [PubMed] [Google Scholar]
- Guertin K. A., Grant R. K., Arnold K. B., Burwell L., Hartline J., Goodman P. J., et al. (2016). Effect of long-term vitamin E and selenium supplementation on urine F 2-isoprostanes, a biomarker of oxidative stress. Free Rad. Biol. Med. 95, 349–356. 10.1016/j.freeradbiomed.2016.03.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gümüş P., Emingil G., Öztürk V. Ö., Belibasakis G. N., Bostanci N. (2015). Oxidative stress markers in saliva and periodontal disease status: modulation during pregnancy and postpartum. BMC Infect. Dis. 15:261. 10.1186/s12879-015-1003-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta S., Earley B., Crowe M. A. (2007). Effect of 12-h road transportation on physiological, immunological and hematological parameters in bulls housed at different space allowances. Vet. J. 173, 605–616. 10.1016/j.tvjl.2006.03.002 [DOI] [PubMed] [Google Scholar]
- Gut P., Czarnywojtek A., Fischbach J., Baczyk M., Ziemnicka K., Wrotkowska E., et al. (2016). Chromogranin A–unspecific neuroendocrine marker. Clinical utility and potential diagnostic pitfalls. Arch. Med. Sci. 12, 1–9. 10.5114/aoms.2016.57577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hadwan M. H. (2018). Simple spectrophotometric assay for measuring catalase activity in biological tissues. BMC Biochem. 19:7. 10.1186/s12858-018-0097-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halliwell B. (2007). Biochemistry of oxidative stress. Biochem. Soc. Trans. 035, 1147–1150. 10.1042/BST0351147 [DOI] [PubMed] [Google Scholar]
- Hammarsten O., Mair J., Möckel M., Lindahl B., Jaffe A. S. (2018). Possible mechanisms behind cardiac troponin elevations. Biomarkers 23, 725–734. 10.1080/1354750X.2018.1490969 [DOI] [PubMed] [Google Scholar]
- Han W. K., Waikar S. S., Johnson A., Betensky R. A., Dent C. L., Devarajan P., et al. (2008). Urinary biomarkers in the early diagnosis of acute kidney injury. Kidney Int. 73, 863–869. 10.1038/sj.ki.5002715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanff E., Eisenga M. F., Beckmann B., Bakker S. J., Tsikas D. (2016). Simultaneous pentafluorobenzyl derivatization and GC-ECNICI-MS measurement of nitrite and malondialdehyde in human urine: close positive correlation between these disparate oxidative stress biomarkers. J. Chromatogr. B Analyt. Technol. Biomed. Life Sci. 1043:167–175. 10.1016/j.jchromb.2016.07.027 [DOI] [PubMed] [Google Scholar]
- Hao X., Luo H., Krawczyk M., Wei W., Wang W., Wang J., et al. (2017). DNA methylation markers for diagnosis and prognosis of common cancers. Proc. Natl. Acad. Sci. U.S.A. 114, 7414–7419. 10.1073/pnas.1703577114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hara S. (2001). Effects of selenium deficiency on expression of selenoproteins in bovine arterial endothelial cells. Biol. Pharmaceut. Bull. 24, 754–759. 10.1248/bpb.24.754 [DOI] [PubMed] [Google Scholar]
- Havasi A., Li Z., Wang Z., Martin J. L., Botla V., Ruchalski K., et al. (2008). Hsp27 inhibits Bax activation and apoptosis via a phosphatidylinositol 3-kinase-dependent mechanism. J Biol Chem. 283, 12305–12313. 10.1074/jbc.M801291200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haworth K. M., Chandler H. L. (2017). Oxidative stress measures of lipid and DNA damage in human tears. Invest. Ophthalmol. Vis. Sci. 58, BIO151–BIO157. 10.1167/iovs.17-21436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayashi T. (2015). Conversion of psychological stress into cellular stress response: roles of the sigma-1 receptor in the process. Psychiatry Clin. Neurosci. 69, 179–191. 10.1111/pcn.12262 [DOI] [PubMed] [Google Scholar]
- He B. S., Qu J., Zhao Q. (2018). Identifying and exploiting potential miRNA-disease associations with neighborhood regularized logistic matrix factorization. Front. Genet. 9, 303. 10.3389/fgene.2018.00303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- He P., He W., Wang A., Xia T., Xu B., Zhang M., et al. (2008). PBDE-47-induced oxidative stress, DNA damage and apoptosis in primary cultured rat hippocampal neurons. Neurotoxicol. 9, 124–129. 10.1016/j.neuro.2007.10.002 [DOI] [PubMed] [Google Scholar]
- Hearing C. M., Chang W. C., Szuhany K. L., Deckersbach T., Nierenberg A. A., Sylvia L. G. (2016). Physical exercise for treatment of mood disorders: a critical review. Curr. Behav. Neurosci. Rep. 3, 350–359. 10.1007/s40473-016-0089-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hecker J. G., McGarvey M. (2011). Heat shock proteins as biomarkers for the rapid detection of brain and spinal cord ischemia: a review and comparison to other methods of detection in thoracic aneurysm repair. Cell Stress Chaperones 16, 119–131. 10.1007/s12192-010-0224-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hefnawy A., Helal M. A. Y., Sabek A., Shousha S. (2018). Clinical, behavioral and biochemical alterations due to shearing stress in Ossimi sheep. J. Vet. Med. Sci. 80, 1281–1286. 10.1292/jvms.18-0150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hegde M. N., Nireeksha S. S. (2016). Saliva as a biomarker of heat shock protein in chronic renal disease. J. Interdiscipl. Med. Dent. Sci. 4:2 10.4172/2376-032X.1000195 [DOI] [Google Scholar]
- Hellhammer D. H., Wust S., Kudielka M. B. (2009). Salivary cortisol as a biomarker in stress research. Psychoneuroendocrinology 34, 163–171. 10.1016/j.psyneuen.2008.10.026 [DOI] [PubMed] [Google Scholar]
- Herget-Rosenthal S., Marggraf G., Hüsing J., Göring F., Pietruck F., Janssen O., et al. (2004). Early detection of acute renal failure by serum cystatin C. Kidney Int. 66, 1115–1122. 10.1111/j.1523-1755.2004.00861.x [DOI] [PubMed] [Google Scholar]
- Herold Z., Doleschall M., Kovesdi A., Patocs A., Somogyi A. (2018). Chromogranin A and its role in the pathogenesis of diabetes mellitus. Endokrynol. Pol. 69, 598–610. 10.5603/EP.a2018.0052 [DOI] [PubMed] [Google Scholar]
- Herskin M., Munksgaard L., Andersen J. B. (2007). Effects of social isolation and restraint on adrenocortical responses and hypoalgesia in loose-housed dairy cows. J. Anim. Sci. 85, 240–247. 10.2527/jas.2005-346 [DOI] [PubMed] [Google Scholar]
- Hettinga Y. M., Scheerlinck L. M., Lilien M. R., Rothova A., de Boer J. H. (2015). The value of measuring urinary β2-microglobulin and serum creatinine for detecting tubulointerstitial nephritis and uveitis syndrome in young patients with uveitis. JAMA Ophthalmol. 133, 140–145. 10.1001/jamaophthalmol.2014.4301 [DOI] [PubMed] [Google Scholar]
- Hibner G., Kimsa-Furdzik M., Francuz T. (2018). Relevance of micrornas as potential diagnostic and prognostic markers in colorectal cancer. Int. J. Mol. Sci. 19:2944. 10.3390/ijms19102944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho E., Galougahi K. K., Liu C. C., Bhindi R., Figtree G. A. (2013). Biological markers of oxidative stress: applications to cardio-vascular research and practice. Redox. Biol. 1, 483–491. 10.1016/j.redox.2013.07.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho J. E., Lyass A., Courchesne P., Chen G., Liu C., Yin X., et al. (2018). Protein biomarkers of cardiovascular disease and mortality in the community. J. Am. Heart Assoc. 7:e008108. 10.1161/JAHA.117.008108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollinger A., Wittebole X., François B., Pickkers P., Antonelli M., Gayat E., et al. (2018). Proenkephalin A 119-159 (Penkid) is an early biomarker of septic acute kidney injury: the kidney in sepsis and septic shock (Kid-SSS) study. Kidney Int. Rep. 3, 1424–1433. 10.1016/j.ekir.2018.08.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Honda M., Kuwano Y., Katsuura-Kamano S., Kamezaki Y., Fujita K., Akaike Y., et al. (2013). Chronic academic stress increases a group of microRNAs in peripheral blood. PLoS ONE 8:e75960. 10.1371/journal.pone.0075960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong B. S., Cho J. H., Kim H., Choi E. J., Rho S., Kim J., et al. (2009). Colorectal cancer cell-derived microvesicles are enriched in cell cycle-related mRNAs that promote proliferation of endothelial cells. BMC Genomics 10:556. 10.1186/1471-2164-10-556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hori Y. (2006). The time course of C-reactive protein in a dog suffering acute pancreatitis. J. Jap. Vet. Med. Assoc. 59, 619–622. 10.12935/jvma1951.59.619 [DOI] [Google Scholar]
- Hoshino K., Suzuki J., Yamauchi K., Inoue H. (2008). Psychological stress evaluation of patients with bronchial asthma based on the chromogranin a level in saliva. J. Asthma 45, 596–599. 10.1080/02770900802126966 [DOI] [PubMed] [Google Scholar]
- Hu C., Zhou J., Yang S., Li H., Wang C., Fang X., et al. (2016). Oxidative stress leads to reduction of plasmalogen serving as a novel biomarker for systemic lupus erythematosus. Free Rad. Biol. Med. 101, 475–481. 10.1016/j.freeradbiomed.2016.11.006 [DOI] [PubMed] [Google Scholar]
- Huang Y., Liu Z., Liu W., Yin C., Ci L., Zhao R., et al. (2017). Salivary haptoglobin and chromogranin A as non-invasive markers during restraint stress in pigs. Res. Vet. Sci. 114, 27–30. 10.1016/j.rvsc.2017.02.023 [DOI] [PubMed] [Google Scholar]
- Hunter M. P., Ismail N., Zhang X., Aguda B. D., Lee E. J., Yu L., et al. (2008). Detection of microRNA expression in human peripheral blood microvesicles. PLoS ONE 3:e3694. 10.1371/journal.pone.0003694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huss R. (2015). Biomarkers, in Chapter 19: Translational Regenerative Medicine, eds Atala A., Allickson J. G. (London: Academic Press; ), 235–241. [Google Scholar]
- Ijomone O. M., Olaibi O. K., Nwoha P. U. (2014). Effects of chronic nicotine administration on body weight, food intake and nitric oxide concentration in female and male rats. Pathophysiology 21, 185–190. 10.1016/j.pathophys.2014.08.003 [DOI] [PubMed] [Google Scholar]
- Ikwegbue P. C., Masamba P., Oyinloye B. E., Kappo A. P. (2017). Roles of heat shock proteins in apoptosis, oxidative stress, human inflammatory diseases, and cancer. Pharmaceuticals 11:2. 10.3390/ph11010002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Islam M. R., Islam M. R., Ahmed I., Moktadir A. A., Nahar Z., Islam M. S., et al. (2018). Elevated serum levels of malondialdehyde and cortisol are associated with major depressive disorder: a case-control study. SAGE Open Med. 6:2050312118773953. 10.1177/2050312118773953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Itabe H., Kato R., Sasabe N., Obama T., Yamamoto M. (2018). Significance of oxidized low-density lipoprotein in body fluids as a marker related to diseased conditions. Curr. Med. Chem. 26, 1576–1593. 10.2174/0929867325666180307114855 [DOI] [PubMed] [Google Scholar]
- Ivković N., BoŽović Ã., Račić M., Popović-Grubač D., Davidović B. (2015). Biomarkers of stress in saliva. Acta Facult. Med. Nis. 32, 91–99. 10.1515/afmnai-2015-0010 [DOI] [Google Scholar]
- Jacobsen S., Niewold T. A., Kornalijnslijper E., Toussaint M. J., Gruys E. (2005). Kinetics of local and systemic isoforms of serum amyloid A in bovine mastitic milk. Vet. Immunol. Immunopathol. 104, 21–31. 10.1016/j.vetimm.2004.09.031 [DOI] [PubMed] [Google Scholar]
- Jadoon S., Malik A. (2018). A comprehensive review article on isoprostanes as biological markers. Biochem. Pharmacol. 7:246 10.4172/2167-0501.1000246 [DOI] [Google Scholar]
- Jafari M., Solhi E., Tagi S., Hasanzadeh M., Jouyban-Gharamaleki V., Jouyban A., et al. (2019). Non-invasive quantification of malondialdehyde biomarker in human exhaled breath condensate using self-assembled organic-inorganic nanohybrid: a new platform for early diagnosis of lung disease. J. Pharm. Biomed. Anal. 164, 249–257. 10.1016/j.jpba.2018.10.048 [DOI] [PubMed] [Google Scholar]
- Jain K. K. (2010). The Handbook of Biomarkers. New York, NY: Springer, 1–457. [Google Scholar]
- Jain S., Gautam V., Naseem S. (2011). Acute-phase proteins: as diagnostic tool. J. Pharm. Bioallied Sci. 3, 118–127. 10.4103/0975-7406.76489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jang J., Oh H., Nam D., Seol W., Seo M. K., Park S. W., et al. (2018). Increase in anti-apoptotic molecules, nucleolin, and heat shock protein 70, against upregulated LRRK2 kinase activity. Anim. Cells Syst. 22, 273–280. 10.1080/19768354.2018.1518262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jasim H., Carlsson A., Hedenberg-Magnusson B., Ghafouri B., Ernberg M. (2018). Saliva as a medium to detect and measure biomarkers related to pain. Sci. Rep. 8:3220. 10.1038/s41598-018-21131-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeeva J. S., Sunitha J., Ananthalakshmi R., Rajkumari S., Ramesh M., Krishnan R. (2015). Enzymatic antioxidants and its role in oral diseases. J. Pharm. Bioallied Sci. 7, S331–S333. 10.4103/0975-7406.163438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jena S. K., Mohanty B. (2016). Stress in preschool children and its correlation with salivary chromogranin A. Muller J. Med. Sci. Res. 7, 105–110. 10.4103/0975-9727.185007 [DOI] [Google Scholar]
- Jia M., Chew W. M., Feinstein Y., Skeath P., Sternberg E. M. (2016). Quantification of cortisol in human eccrine sweat by liquid chromatography–tandem mass spectrometry. Analyst 141, 2053–2060. 10.1039/c5an02387d [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang L., Cheng Q., Zhang B. H., Zhang M. Z. (2015). Circulating microRNAs as biomarkers in hepatocellular carcinoma screening: a validation set from China. Medicine 94:e603. 10.1097/MD.0000000000000603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jin F., Hu H., Xu M., Zhan S., Wang Y., Zhang H., et al. (2018). Serum microRNA profiles serve as novel biomarkers for autoimmune diseases. Front. Immunol. 9:2381. 10.3389/fimmu.2018.02381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johansen J. S. (2006). Studies on serum YKL-40 as a biomarker in diseases with inflammation, tissue remodelling, fibroses and cancer. Dan. Med. Bull. 53, 172–209. [PubMed] [Google Scholar]
- Johar D. R., Bernstein L. H. (2017). Biomarkers of stress-mediated metabolic deregulation in diabetes mellitus. Diabetes Res. Clin. Pract. 126, 222–229. 10.1016/j.diabres.2017.02.023 [DOI] [PubMed] [Google Scholar]
- Jorat M. V., Tabrizi R., Kolahdooz F., Akbari M., Salami M., Heydari S. T., et al. (2019). The effects of coenzyme Q10 supplementation on biomarkers of inflammation and oxidative stress in among coronary artery disease: a systematic review and meta-analysis of randomized controlled trials. Inflammopharmacology 27, 233–248. 10.1007/s10787-019-00572-x [DOI] [PubMed] [Google Scholar]
- Joshi V., Gupta V. K., Bhanuprakash A. G., Mandal R. S. K., Dimri U., Ajith Y. (2018). Haptoglobin and serum amyloid A as putative biomarker candidates of naturally occurring bovine respiratory disease in dairy calves. Microb. Pathog. 116, 33–37. 10.1016/j.micpath.2018.01.001 [DOI] [PubMed] [Google Scholar]
- Jung C., Greco S., Nguyen H. H., Ho J. T., Lewis J. G., Torpy D. J., et al. (2014). Plasma, salivary and urinary cortisol levels following physiological and stress doses of hydrocortisone in normal volunteers. BMC Endocr. Disord. 14:91. 10.1186/1472-6823-14-91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jungbauer C. G., Birner C., Jung B., Buchner S., Lubnow M., von Bary C., et al. (2011). Kidney injury molecule-1 and N-acetyl-ß-d-glucosaminidase in chronic heart failure: possible biomarkers of cardiorenal syndrome. Eur. J. Heart Failure 13, 1104–1110. 10.1093/eurjhf/hfr102 [DOI] [PubMed] [Google Scholar]
- Kamijo-Ikemori A., Kimura K. (2015). Urinary liver-type fatty acid binding protein and chronic kidney disease. Indian J Nephrol. 25, 263–264. 10.1007/s11010-005-9047-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kapusta A., Kuczynska B., Puppel K. (2018). Relationship between the degree of antioxidant protection and the level of malondialdehyde in high-performance Polish Holstein-Friesian cows in peak of lactation. PLoS ONE 13:e0193512. 10.1371/journal.pone.0193512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karwi Q. G., Uddin G. M., Ho K. L., Lopaschuk G. D. (2018). Loss of metabolic flexibility in the failing heart. Front. Cardiovasc. Med. 5:68. 10.3389/fcvm.2018.00068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katan M., Christ-Crain M. (2010). The stress hormone copeptin: a new prognostic biomarker in acute illness. Swiss Med. Wkly. 140:w13101. 10.4414/smw.2010.13101 [DOI] [PubMed] [Google Scholar]
- Kaur J., Jacobs R., Huang Y., Salvo N., Politis C. (2018). Salivary biomarkers for oral cancer and pre-cancer screening: a review. Clin. Oral Invest. 22, 633–640. 10.1007/s00784-018-2337-x [DOI] [PubMed] [Google Scholar]
- Kawai K., Kasai H., Li Y. S., Kawasaki Y., Watanabe S., Ohta M., et al. (2018). Measurement of 8-hydroxyguanine as an oxidative stress biomarker in saliva by HPLC-ECD. Genes Environ. 40:5. 10.1186/s41021-018-0095-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawamura T., Muraoka I. (2018). Exercise-induced oxidative stress and the effects of antioxidant intake from a physiological viewpoint. Antioxidants 7:119. 10.3390/antiox7090119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan A. A., Alsahli M. A., Rahmani A. H. (2018). Myeloperoxidase as an active disease biomarker: recent biochemical and pathological perspectives. Med. Sci. 6:E33. 10.3390/medsci6020033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khandia R., Munjal A. K., Iqbal H. M. N., Dhama K. (2017). Heat shock proteins: therapeutic perspectives in inflammatory disorders. Recent Pat. Inflamm. Allergy Drug Discov. 10, 94–104. 10.2174/1872213X10666161213163301 [DOI] [PubMed] [Google Scholar]
- Khoubnasabjafari M., Ansarin K., Jouyban A. (2016). Salivary malondialdehyde as an oxidative stress biomarker in oral and systemic diseases. J. Dental Res. Dent. Clin. Dent. Prospects 10:71. 10.15171/joddd.2016.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khurana R., Ranches G., Schafferer S., Lukasser M., Rudnicki M., Mayer G., et al. (2017). Identification of urinary exosomal noncoding RNAs as novel biomarkers in chronic kidney disease. RNA 23, 142–152. 10.1261/rna.058834.116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khurshid Z., Zafar M. S., Khan R. S., Najeeb S., Slowey P. D., Rehman I. U. (2018). Role of salivary biomarkers in oral cancer detection. Adv. Clin. Chem. 86, 23–70. 10.1016/bs.acc.2018.05.002 [DOI] [PubMed] [Google Scholar]
- Khyani I. A. M., Qureshi M. A., Mirza T., Farooq M. U. (2017). Detection of interleukins-6 and 8 in saliva as potential biomarkers of oral pre-malignant lesion and oral carcinoma: a breakthrough in salivary diagnostics in Pakistan. Pak. J. Pharm. Sci. 30, 817–823. [PubMed] [Google Scholar]
- Kim J. (2015). Noninvasive uric acid monitoring device using near-infrared spectroscopy. J. Biosens. Bioelectron. 6:188 10.4172/2155-6210.1000188 [DOI] [Google Scholar]
- Kim W. S., Jung I. D., Kim J. S., Kim H. M., Kwon K. W., Park Y. M., et al. (2018). Mycobacterium tuberculosis GrpE, a heat-shock stress responsive chaperone, promotes TH1-biased T cell immune response via TLR4-mediated activation of dendritic cells. Front. Cell Infect. Microbiol. 8:95 10.3389/fcimb.2018.00095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimmel M., Shi J., Latus J., Wasser C., Kitterer D., Braun N., et al. (2016). Association of renal stress/damage and filtration biomarkers with subsequent AKI during hospitalization among patients presenting to the emergency department. Clin. J. Am. Soc. Nephrol. 11, 938–946. 10.2215/CJN.10551015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein S. J., Brandtner A. K., Lehner G. F., Ulmer H., Bagshaw S. M., Wiedermann C. J., et al. (2018). Biomarkers for prediction of renal replacement therapy in acute kidney injury: a systematic review and meta-analysis. Intensive Care Med. 44, 323–336. 10.1007/s00134-018-5126-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koh D., Ng V., Naing L. (2014). Alpha amylase as a salivary biomarker of acute stress of venepuncture from periodic medical examinations. Front. Public Health 2:121. 10.3389/fpubh.2014.00121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kreth S., Hübner M., Hinske L. C. (2018). MicroRNAs as clinical biomarkers and therapeutic tools in perioperative medicine. Anesth. Analg. 126, 670–681. 10.1213/ANE.0000000000002444 [DOI] [PubMed] [Google Scholar]
- Kristyagita A., Siswanto B. B. (2015). The role of copeptin as a novel cardiovascular biomarker. Med. J. Indonesia 24, 59–66. 10.13181/mji.v24i1.1208 [DOI] [Google Scholar]
- Kufe D. W. (2009). Mucins in cancer: function, prognosis and therapy. Nat. Rev. Cancer 9, 874–885. 10.1038/nrc2761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kulkarni N. B., Ganu M. U., Godbole S. G., Deo S. S. (2018). Assessment of potential biomarkers of atherosclerosis in Indian patients with type 2 diabetes mellitus. Indian J. Med. Res. 147, 169–176. 10.4103/ijmr.IJMR_852_16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kushner I. (1982). The phenomenon of the acute phase response. Ann. N. Y. Acad. Sci. 389, 39–48. 10.1111/j.1749-6632.1982.tb22124.x [DOI] [PubMed] [Google Scholar]
- Kuwabara Y., Ono K., Horie T., Nishi H., Nagao K., Kinoshita M., et al. (2011). Increased microRNA-1 and microRNA-133a levels in serum of patients with cardiovascular disease indicate myocardial damage. Circ. Cardiovasc. Genet. 4, 446–454. 10.1161/CIRCGENETICS.110.958975 [DOI] [PubMed] [Google Scholar]
- Kyle S. M., Vashi N., Justice M. J. (2018). Rett syndrome: a neurological disorder with metabolic components. Open Biol. 8:170216. 10.1098/rsob.170216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai N. S., Zhang J. Q., Qin F. Y., Sheng B., Fang X. G., Li Z. B. (2017). Serum microRNAs are non-invasive biomarkers for the presence and progression of subarachnoid hemorrhage. Biosci. Rep. 37:BSR20160480 10.1042/BSR20160480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamb A. L., Hess D. E., Edenborn S., Ubinger E., Carrillo A. E., Appasamy P. M. (2017). Elevated salivary IgA, decreased anxiety, and an altered oral microbiota are associated with active participation on an undergraduate athletic team. Physiol. Behav. 169, 169–177. 10.1016/j.physbeh.2016.12.004 [DOI] [PubMed] [Google Scholar]
- Lashley T., Schott J. M., Weston P., Murray C. E., Wellington H., Keshavan A., et al. (2018). Molecular biomarkers of Alzheimer's disease: progress and prospects. Dis. Models Mech. 11:dmm031781. 10.1242/dmm.031781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauritzen B., Lykkesfeldt J., Friis C. (2005). Evaluation of a single dose versus a divided dose regimen of amoxicillin in treatment of Actinobacillus pleuropneumoniae infection in pigs. Res. Vet. Sci. 79, 61–67. 10.1016/j.rvsc.2004.09.011 [DOI] [PubMed] [Google Scholar]
- Lechner P., Buck D., Sick L., Hemmer B., Multhoff G. (2018). Serum heat shock protein 70 levels as a biomarker for inflammatory processes in multiple sclerosis. Mult. Scler. J. Exp. Transl. Clin. 4:2055217318767192. 10.1177/2055217318767192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee K. M., Kang D., Yoon K., Kim S. Y., Kim H., Yoon H. S., et al. (2010). A pilot study on the association between job stress and repeated measures of immunological biomarkers in female nurses. Int. Arch. Occup. Environ. Health 83, 779–789. 10.1007/s00420-010-0544-0 [DOI] [PubMed] [Google Scholar]
- Leicht C. A., Paulson T. A., Goosey-Tolfrey V. L., Bishop N. C. (2017). Salivary alpha amylase not chromogranin A reflects sympathetic activity: exercise responses in elite male wheelchair athletes with or without cervical spinal cord injury. Sports Med. Open 3:1 10.1186/s40798-016-0068-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lelj-Garolla B., Mauk A. G. (2006). Self-association and chaperone activity of Hsp27 are thermally activated. J. Biol. Chem. 281, 8169–8174. 10.1074/jbc.M512553200 [DOI] [PubMed] [Google Scholar]
- Li D., Duncan R. F. (1995). Transient acquired thermotolerance in Drosophila, correlated with rapid degradation of Hsp70 during recovery. Eur. J. Biochem. 231, 454–465. 10.1111/j.1432-1033.1995.tb20719.x [DOI] [PubMed] [Google Scholar]
- Li J., Lei J., He L., Fan X., Yi F., Zhang W. (2019). Evaluation and monitoring of superoxide dismutase (SOD) activity and its clinical significance in gastric cancer: a systematic review and meta-analysis. Med. Sci. Monit. 25, 2032–2042. 10.12659/MSM.913375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Z., Zhao X., Wei Y. (2004). Regulation of apoptotic signal transduction pathways by the heat shock proteins. Sci. China C Life Sci. 47, 107–114. 10.1360/02yc0263 [DOI] [PubMed] [Google Scholar]
- Liang S. C., Nickerson-Nutter C., Pittman D. D., Carrier Y., Goodwin D. G., Shields K. M., et al. (2010). IL-22 induces an acute-phase response. J. Immunol. 185, 5531–5538. 10.4049/jimmunol.0904091 [DOI] [PubMed] [Google Scholar]
- Liang Y., Ridzon D., Wong L., Chen C. (2007). Characterization of microRNA expression profiles in normal human tissues. BMC Genomics 8:166. 10.1186/1471-2164-8-166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liguori M., Nuzziello N., Introna A., Consiglio A., Licciulli F., D'Errico E., et al. (2018). Dysregulation of microRNAs and target genes networks in peripheral blood of patients with sporadic amyotrophic lateral sclerosis. Front. Mol. Neurosci. 11:288 10.3389/fnmol.2018.00288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lihala R., Jayaram P., Chatterjee A., Joshi A. (2019). Effect of non-surgical periodontal therapy on stress and salivary Chromogranin-A levels: a clinico-biochemical study. Indian J. Dent. Res. 30, 213–218. 10.4103/ijdr.IJDR_273_17 [DOI] [PubMed] [Google Scholar]
- Lim S. K., Kim H., Lim S. K., bin Ali A., Lim Y. K., Wang Y., et al. (1998). Increased susceptibility in Hp knockout mice during acute hemolysis. Blood 92, 1870–1877. [PubMed] [Google Scholar]
- Lin J., Li J., Huang B., Liu J., Chen X., Chen X. M., et al. (2015). Exosomes: novel biomarkers for clinical diagnosis. Sci. World J. 2015:657086. 10.1155/2015/657086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin L. H., Chang K. W., Kao S. Y., Cheng H. W., Liu C. J. (2018). Increased plasma circulating cell-free dna could be a potential marker for oral cancer. Int. J. Mol. Sci. 19:3303. 10.3390/ijms19113303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindsay A., Costello J. T. (2017). Realising the potential of urine and saliva as diagnostic tools in sport and exercise medicine. Sports Med. 47, 11–31. 10.1007/s40279-016-0558-1 [DOI] [PubMed] [Google Scholar]
- Liou S. H., Chen Y. C., Liao H. Y., Wang C. J., Chen J. S., Lee H. L. (2016). Increased levels of oxidative stress biomarkers in metal oxides nanomaterial-handling workers. Biomarkers 21, 600–606. 10.3109/1354750X.2016.1160432 [DOI] [PubMed] [Google Scholar]
- Liu C., Cao Y., Zhou S., Khoso P. A., Li S. (2017). Avermectin induced global DNA hypomethylation and over-expression of heat shock proteins in cardiac tissues of pigeon. Pesticide Biochem. Physiol. 135, 52–58. 10.1016/j.pestbp.2016.06.005 [DOI] [PubMed] [Google Scholar]
- Liu X., Yu H., Qiao Y., Yang J., Shu J., Zhang J., et al. (2018). Salivary glycopatterns as potential biomarkers for screening of early-stage breast cancer. EBioMedicine 28, 70–79. 10.1016/j.ebiom.2018.01.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y., Zhang X. (2018). Heat shock protein reports on proteome stress. Biotechnol. J. 13:1800039. 10.1002/biot.201800039 [DOI] [PubMed] [Google Scholar]
- Liu Z., Zhu Z., Zhao J., Ren W., Cai Y., Wang Q., et al. (2017). Malondialdehyde: a novel predictive biomarker for post-stroke depression. J. Affect. Disord. 220, 95–101. 10.1016/j.jad.2017.05.023 [DOI] [PubMed] [Google Scholar]
- Lo Y. D., Tsui N. B., Chiu R. W., Lau T. K., Leung T. N., Heung M. M., et al. (2007). Plasma placental RNA allelic ratio permits noninvasive prenatal chromosomal aneuploidy detection. Nat. Med. 13, 218–223. 10.1038/nm1530 [DOI] [PubMed] [Google Scholar]
- Lomborg S. R., Nielsen L. R., Heegaard P. M., Jacobsen S. (2008). Acute phase proteins in cattle after exposure to complex stress. Vet. Res. Commun. 32, 575–582. 10.1007/s11259-008-9057-7 [DOI] [PubMed] [Google Scholar]
- Lorenzo-Pouso A. I., Pérez-Sayáns M., Bravo S. B., López-Jornet P., García-Vence M., Alonso-Sampedro M., et al. (2018). Protein-based salivary profiles as novel biomarkers for oral diseases. Dis. Markers 2018:6141845. 10.1155/2018/6141845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu H. Y., Ning X. Y., Chen Y. Q., Han S. J., Chi P., Zhu S. N., et al. (2018). Predictive value of serum creatinine, blood urea nitrogen, uric acid, and β2-microglobulin in the evaluation of acute kidney injury after orthotopic liver transplantation. Chinese Med. J. 131, 1059–1066. 10.4103/0366-6999.230726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luan Y. Y., Yao Y. M. (2018). The clinical significance and potential role of c-reactive protein in chronic inflammatory and neurodegenerative diseases. Front. Immunol. 9:1302. 10.3389/fimmu.2018.01302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lykkesfeldt J., Svendsen O. (2007). Oxidants and antioxidants in disease: Oxidative stress in farm animals. Vet. J. 173, 502–511. 10.1016/j.tvjl.2006.06.005 [DOI] [PubMed] [Google Scholar]
- Ma X., Chen Z., Wang L., Wang G., Wang Z., Dong X., et al. (2018). The pathogenesis of diabetes mellitus by oxidative stress and inflammation: Its inhibition by berberine. Front. Pharmacol. 9:782. 10.3389/fphar.2018.00782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maciejczyk M., Kossakowska A., Szulimowska J., Klimiuk A., Knás M., Car H., et al. (2017). Lysosomal exoglycosidase profile and secretory function in the salivary glands of rats with streptozotocin-induced diabetes. J. Diabetes Res. 2017:9850398. 10.1155/2017/9850398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maciejczyk M., Szulimowska J., Skutnik A., Taranta-Janusz K., Wasilewska A., Wiśniewska N., et al. (2018b). Salivary biomarkers of oxidative stress in children with chronic kidney disease. J. Clin. Med. 7:E209. 10.3390/jcm7080209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maciejczyk M., Zebrowska E., Zalewska A., Chabowski A. (2018a). Redox balance, antioxidant defense, and oxidative damage in the hypothalamus and cerebral cortex of rats with high fat diet-induced insulin resistance. Oxid. Med. Cell Longev. 2018:6940515. 10.1155/2018/6940515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKay M. B., Kravtsenyuk M., Thomas R., Mitchell N. D., Dursun S. M., Baker G. B. (2019). D-serine: potential therapeutic agent and/or biomarker in schizophrenia and depression? Front. Psychiatry 10:25 10.3389/fpsyt.2019.00025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magnusson M. K., Lasson A., Stridsberg M., Isaksson S., Strid H., Öhman L. (2018). Faecal secretogranin and chromogranin levels persist over time and are unrelated to disease history and outcome in patients with ulcerative colitis. Cogent. Med. 5:1484602 10.1080/2331205X.2018.1484602 [DOI] [Google Scholar]
- Mahata S. K., Kiranmayi M., Mahapatra N. R. (2018). Catestatin: a master regulator of cardiovascular functions. Curr. Med. Chem. 25, 1352–1374. 10.2174/0929867324666170425100416 [DOI] [PubMed] [Google Scholar]
- Malinski T. (2007). Nitric oxide and nitroxidative stress in Alzheimer's disease. J. Alzheimers Dis. 11, 207–218. 10.3233/JAD-2007-11208 [DOI] [PubMed] [Google Scholar]
- Maltais-Payette I., Boulet M. M., Prehn C., Adamski J., Tchernof A. (2018). Circulating glutamate concentration as a biomarker of visceral obesity and associated metabolic alterations. Nutr. Met. 15:78. 10.1186/s12986-018-0316-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mambula S. S., Stevenson M. A., Ogawa K., Calderwood S. K. (2007). Mechanisms for Hsp70 secretion: crossing membranes without a leader. Methods 43, 168–175. 10.1016/j.ymeth.2007.06.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manavalan S., Rajaji U., Chen S. M., Selvin S. S. P., Govindasamy M., Chen T. W., et al. (2018). Determination of 8-hydroxy-2′-deoxyguanosine oxidative stress biomarker using dysprosium oxide nanoparticles@reduced graphene oxide. Inorg. Chem. Front. 5, 2885–2892. 10.1039/C8QI00727F [DOI] [Google Scholar]
- Mander B. A., Winer J. R., Jagust W. J., Walker M. P. (2016). Sleep: a novel mechanistic pathway, biomarker, and treatment target in the pathology of Alzheimer's disease? Trends Neurosci. 39, 552–566. 10.1016/j.tins.2016.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcato F., van den Brand H., Kemp B., van Reenen K. (2018). Evaluating potential biomarkers of health and performance in veal calves. Front. Vet. Sci. 5:133. 10.3389/fvets.2018.00133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marchitti S. A., Brocker C., Stagos D., Vasiliou V. (2008). Non-P450 aldehyde oxidizing enzymes: thealdehyde dehydrogenase superfamily. Expert Opin. Drug Metab. Toxicol. 4, 697–720. 10.1517/17425255.4.6.697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marco-Ramell A., de Almeida A. M., Cristobal S., Rodrigues P., Roncada P., Bassols A. (2016). Proteomics and the search for welfare and stress biomarkers in animal production in the one-health context. Mol. Biosyst. 12, 2024–2035. 10.1039/c5mb00788g [DOI] [PubMed] [Google Scholar]
- Mariucci G., Tantucci M., Giuditta A., Ambrosini M. V. (2007). Permanent brain ischemia induces marked increments in hsp72 expression and local protein synthesis in synapses of the ischemic hemisphere. Neurosci. Lett. 415, 77–80. 10.1016/j.neulet.2006.12.047 [DOI] [PubMed] [Google Scholar]
- Marques A. T., Lecchi C., Grilli G., Giudice C., Nodari S. R., Vinco L. J., et al. (2016). The effect of transport stress on turkey (Meleagris gallopavo) liver acute phase proteins gene expression. Res. Vet. Sci. 104, 92–95. 10.1016/j.rvsc.2015.11.014 [DOI] [PubMed] [Google Scholar]
- Martin L. B., Andreassi E., Watson W., Coon C. (2011). Stress and animal health: physiological mechanisms and ecological consequences. Nat. Educ. Knowl. Project 3:11. [Google Scholar]
- Martinez-Subiela S., Tecles F., Cerón J. J., Eckersall P. D. (2002). Serum concentrations of acute phase proteins in dogs with leishmaniasis. Vet. Rec. 150, 241–244. 10.1136/vr.150.8.241 [DOI] [PubMed] [Google Scholar]
- Matar S., Malczewska A., Oberg K., Bodei L., Aslanian H., Lewczuk-Myślicka A., et al. (2019). Blood chromogranin A is not effective as a biomarker for diagnosis or management of bronchopulmonary NET/NET. Neuroendocrinology. 10.1159/000500202. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matheson A., Willcox M. D., Flanagan J., Walsh B. J. (2010). Urinary biomarkers involved in type 2 diabetes: a review. Diabetes Metab. Res. Rev. 26, 150–171. 10.1002/dmrr.1068 [DOI] [PubMed] [Google Scholar]
- Matthews M. A., Aschner J. L., Stark A. R., Moore P. E., Slaughter J. C., Steele S., et al. (2016). Increasing F2-isoprostanes in the first month after birth predicts poor respiratory and neurodevelopmental outcomes in very preterm infants. J. Perinatology 36, 779–783. 10.1038/jp.2016.74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayeur S., Spahis S., Pouliot Y., Levy E. (2016). Lactoferrin, a pleiotropic protein in health and disease. Antioxid. Redox Signal 24, 813–836. 10.1089/ars.2015.6458 [DOI] [PubMed] [Google Scholar]
- Mayeux R. (2004). Biomarkers: potential uses and limitations. J. Am. Soc. Exp. Neuro. Ther. 1, 182–188. 10.1602/neurorx.1.2.182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazereeuw G., Herrmann N., Andreazza A. C., Scola G., Ma D. W., Oh P. I., et al. (2017). Oxidative stress predicts depressive symptom changes with omega-3 fatty acid treatment in coronary artery disease patients. Brain. Behav. Immun. 60, 136–141. 10.1016/j.bbi.2016.10.005 [DOI] [PubMed] [Google Scholar]
- McCormick S. M., Gowda N., Fang J. X., Heller N. M. (2016). Suppressor of cytokine signaling (SOCS)1 regulates interleukin-4 (IL-4)-activated insulin receptor substrate (IRS)-2 tyrosine phosphorylation in monocytes and macrophages via the proteasome. J. Biol. Chem. 291, 20574–20587. 10.1074/jbc.M116.746164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEwen B. S. (2015). Biomarkers for assessing population and individual health and disease related to stress and adaptation. Metabolism 64, S2–S10. 10.1016/j.metabol.2014.10.029 [DOI] [PubMed] [Google Scholar]
- McGarrah R. W., Crown S. B., Zhang G. F., Shah S. H., Newgard C. B. (2018). Cardiovascular metabolomics. Circ. Res. 122, 1238–1258. 10.1161/CIRCRESAHA.117.311002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGrotty Y. L., Arteaga A., Knottenbelt C. M., Ramsey I. K., Eckersall P. D. (2005). Haptoglobin concentrations in dogs undergoing trilostane treatment for hyperadrenocorticism. Vet. Clin. Pathol. 34, 255–258. 10.1111/j.1939-165X.2005.tb00050.x [DOI] [PubMed] [Google Scholar]
- Meagher E. A., FitzGerald G. A. (2000). Indices of lipid peroxidation in vivo: strengths and limitations. Free Radic. Biol. Med. 28, 1745–1750. 10.1016/s0891-5849(00)00232-x [DOI] [PubMed] [Google Scholar]
- Medeiros M. S., Schumacher-Schuh A., Cardoso A. M., Bochi G. V., Baldissarelli J., Kegler A., et al. (2016). Iron and oxidative stress in Parkinson's disease: an observational study of injury biomarkers. PLoS ONE 11:e0146129. 10.1371/journal.pone.0146129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meijer E., Boertien W. E., Nauta F. L., Bakker S. J., van Oeveren W., Rook M., et al. (2010). Association of urinary biomarkers with disease severity in patients with autosomal dominant polycystic kidney disease: across-sectional analysis. Am. J. Kidney Dis. 56, 883–895. 10.1053/j.ajkd.2010.06.023 [DOI] [PubMed] [Google Scholar]
- Melamed-Frank M., Lache O., Enav B. I., Szafranek T., Levy N. S., Ricklis R. M., et al. (2001). Structure-function analysis of the antioxidant properties of haptoglobin. Blood 98, 3693–3698. 10.1182/blood.v98.13.3693 [DOI] [PubMed] [Google Scholar]
- Mello R., Mello R., Gomes D., Paz G. A., Nasser I., Miranda H., et al. (2017). Oxidative stress and antioxidant biomarker responses after a moderate-intensity soccer training session. Res. Sports Med. 25, 322–332. 10.1080/15438627.2017.1345738 [DOI] [PubMed] [Google Scholar]
- Messina A., Monda V., Sessa F., Valenzano A., Salerno M., Bitetti I., et al. (2018). Sympathetic, metabolic adaptations, and oxidative stress in autism spectrum disorders: how far from physiology? Front. Physiol. 9:261. 10.3389/fphys.2018.00261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer J. S., Novak M. A. (2012). Minireview: hair cortisol: a novel biomarker of hypothalamic-pituitary-adrenocortical activity. Endocrinology 153, 4120–4127. 10.1210/en.2012-1226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michopoulos V., Norrholm S. D., Jovanovic T. (2015). Diagnostic biomarkers for posttraumatic stress disorder: promising horizons from translational neuroscience research. Biol. Psychiatry 78, 344–353. 10.1016/j.biopsych.2015.01.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miglio A., Moscati L., Scoccia E., Maresca C., Antognoni M. T., Felici A. (2018). Reference values for serum amyloid A, haptoglobin, lysozyme, zinc and iron in healthy lactating Lacaune sheep. Acta Vet. Scand. 60:46. 10.1186/s13028-018-0400-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milne G. L., Dai Q., Roberts L. J., II. (2015). The isoprostanes−25 years later. Biochim. Biophys. Acta 1851, 433–445. 10.1016/j.bbalip.2014.10.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mir F., Lee D., Ray H., Sadiq S. A. (2014). CSF isoprostane levels are a biomarker of oxidative stress in multiple sclerosis. Neurol. Neuroimmunol. Neuroinflamm. 1:e21. 10.1212/NXI.0000000000000021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mishra A. (2017). Saliva biomarkers: the unsung hero of diagnostics. J. Mol. Genet. Med. 11:288 10.4172/1747-0862.1000288 [DOI] [Google Scholar]
- Mitsuhata C., Ohara Y., Tachikake M., Iwamoto Y., Kozai K. (2012). Effectiveness of salivary chromogranin A as a stress index in young children during dental treatment. Pediatr. Dental J. 22, 163–169. 10.1016/S0917-2394(12)70267-7 [DOI] [Google Scholar]
- Mittelman N. S., Stefanovski D., Johnson A. L. (2018). Utility of C-reactive protein and serum amyloid A in the diagnosis of equine protozoal myeloencephalitis. J. Vet. Inter. Med. 32, 1726–1730. 10.1111/jvim.15254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miyakawa M., Matsui T., Kishikawa H., Murayama R., Uchiyama I., Itoh T., et al. (2006). Salivary chromogranin A as a measure of stress response to noise. Noise Health 8, 108–113. 10.4103/1463-1741.33951 [DOI] [PubMed] [Google Scholar]
- Miyaoka T., Yasukawa R., Yasuda H., Shimizu M., Mizuno S., Sukegawa T., et al. (2005). Urinary excretion of biopyrrins, oxidative metabolites of bilirubin, increases in patients with psychiatric disorders. Eur. Neuropsychopharmacol. 15, 249–252. 10.1016/j.euroneuro.2004.11.002 [DOI] [PubMed] [Google Scholar]
- Mocci F., Bullitta M. A. (2006). Perception of stress in the nursing profession: study of the behavior of s-IgA. Ital. Med. Lav. Ergon. 28, 219–221. [PubMed] [Google Scholar]
- Moledina D. G. (2019). Penkid: a novel biomarker of reduced GFR in sepsis. Kidney Int. Rep. 4, 17–19. 10.1016/j.ekir.2018.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montuschi P., Collins J. V., Ciabattoni G., Lazzeri N., Corradi M., Kharitonov S. A., et al. (2000). Exhaled 8-isoprostane as an in vivo biomarker of lung oxidative stress in patients with COPD and healthy smokers. Am. J. Respir. Crit. Care Med. 162, 175–177. 10.1164/ajrccm.162.3.2001063 [DOI] [PubMed] [Google Scholar]
- Morán L., Cubero F. J. (2018). Extracellular vesicles in liver disease and beyond. World J. Gastroenterol. 24, 4519–4526. 10.3748/wjg.v24.i40.4519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moretti S., Mrakic-Sposta S., Roncoroni L., Vezzoli A., Dellanoce C., Monguzzi E., et al. (2018). Oxidative stress as a biomarker for monitoring treated celiac disease. Clin. Transl. Gastroenterol. 9:157. 10.1038/s41424-018-0031-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgenthaler N. G., Struck J., Jochberger S., Dünser M. W. (2008). Copeptin: clinical use of a new biomarker. Trends Endocrinol. Metab. 19, 43–49. 10.1016/j.tem.2007.11.001 [DOI] [PubMed] [Google Scholar]
- Mori K., Toiyama Y., Otake K., Fujikawa H., Saigusa S., Hiro J., et al. (2016). Proteomics analysis of differential protein expression identifies Heat shock protein 47 as a predictive marker for lymph node metastasis in patients with colorectal cancer. Int. J. Cancer 140, 1425–1435. 10.1002/ijc.30557 [DOI] [PubMed] [Google Scholar]
- Morrow J. D. (2005). Quantification of isoprostanes as indices of oxidant stress and the risk of atherosclerosis in humans. Arterioscler. Thromb. Vascul. Biol. 25, 279–286. 10.1161/01.ATV.0000152605.64964.c0 [DOI] [PubMed] [Google Scholar]
- Mortha N., Uppala D., Kothia N. R., Majumdar S., Kotina S., Sravya K. (2018). A systematic review of saliva on its diagnostic utility. J. NTR Univ. Health Sci. 7, 115–119. 10.4103/JDRNTRUHS.JDRNTRUHS_91_17 [DOI] [Google Scholar]
- Multhoff G. (2007). Heat shock protein 70 (Hsp70): membrane location, export and immunological significance. Methods 43, 229–237. 10.1016/j.ymeth.2007.06.006 [DOI] [PubMed] [Google Scholar]
- Murata A., Kasai T., Matsue Y., Matsumoto H., Yatsu S., Kato T., et al. (2018). Relationship between blood urea nitrogen-to-creatinine ratio at hospital admission and long-term mortality in patients with acute decompensated heart failure. Heart Vessels 33, 877–885. 10.1007/s00380-018-1135-3 [DOI] [PubMed] [Google Scholar]
- Murata H., Shimada N., Yoshioka M. (2004). Current research on acute phase proteins in veterinary diagnosis: an overview. Vet. J. 168, 28–40. 10.1016/S1090-0233(03)00119-9 [DOI] [PubMed] [Google Scholar]
- Musiek E. S., Yin H., Milne G. L., Morrow J. D. (2005). Recent advances in the biochemistry and clinical relevance of the isoprostane pathway. Lipids 40, 987–994. 10.1007/s11745-005-1460-7 [DOI] [PubMed] [Google Scholar]
- Nadkarni G. N., Chauhan K., Rao V., Ix J. H., Shlipak M. G., Parikh C. R., et al. (2019). Effect of intensive blood pressure lowering on kidney tubule injury: findings from the accord trial study participants. Am. J. Kidney Dis. 73, 31–38. 10.1053/j.ajkd.2018.07.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakamura H., Kato M., Nogochi A., Ohira H., Tsujino I., Atsumi T. (2018). Efficient detection of pulmonary arterial hypertension using serum haptoglobin level and cardiac MRI in patients with connective tissue diseases: a pilot study. Clin. Exp. Rheumatol. 36, 345–346. [PubMed] [Google Scholar]
- Nakashima M., Adachi S., Yasuda I., Yamauchi T., Kawaguchi J., Itani M., et al. (2011). Phosphorylation status of heat shock protein 27 plays a key role in gemcitabine-induced apoptosis of pancreatic cancer cells. Cancer Lett. 313, 218–225. 10.1016/j.canlet.2011.09.008 [DOI] [PubMed] [Google Scholar]
- Nallagangula K. S., Shashidhar K. N., Lakshmaiah V., Muninarayana (2018). Evolution of proteomic biomarker for chronic liver disease: promise into reality. J. Circ. Biomark. 7:1849454418777186. 10.1177/1849454418777186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narazaki M., Kishimoto T. (2018). The two-faced cytokine IL-6 in host defense and diseases. Int. J. Mol. Sci. 19:3528. 10.3390/ijms19113528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narberhaus F. (2010). Translational control of bacterial heat shock and virulence genes by temperature-sensing mRNAs. RNA Biol. 7, 84–89. 10.4161/rna.7.1.10501 [DOI] [PubMed] [Google Scholar]
- Nater U. M., La Marca R., Florin L., Moses A., Langhans W., Koller M. M., et al. (2006). Stress-induced changes in human salivary alpha-amylase activity–associations with adrenergic activity. Psychoneuroendocrinology 31, 49–58. 10.1016/j.psyneuen.2005.05.010 [DOI] [PubMed] [Google Scholar]
- Nater U. M., Skoluda N., Strahler J. (2013). Biomarkers of stress in behavioural medicine. Curr. Opin. Psychiatry 26, 440–445. 10.1097/YCO.0b013e328363b4ed [DOI] [PubMed] [Google Scholar]
- Naylor S. (2003). Biomarkers: current perspectives and future prospects. Expert Rev. Mol. Diagn. 3, 525–529. 10.1586/14737159.3.5.525 [DOI] [PubMed] [Google Scholar]
- Nemirovskiy O. V., Radabaugh M. R., Aggarwal P., Funckes-Shippy C. L., Mnich S. J., Meyer D. M., et al. (2009). Plasma 3-nitrotyrosine is a biomarker in animal models of arthritis: pharmacological dissection of iNOS role in disease. Nitric Oxide 20, 150–156. 10.1016/j.niox.2008.12.005 [DOI] [PubMed] [Google Scholar]
- Ng V., Koh D., Mok B., Lim L. P., Yang Y., Chia S. E. (2004). Stressful life events of dental students and salivary immunoglobulin A. Int. J. Immunopathol. Pharmacol. 17, 49–56. 10.1177/03946320040170S209 [DOI] [PubMed] [Google Scholar]
- Ng V., Koh D., Mok B. Y., Chia S. E., Lim L. P. (2003). Salivary biomarkers associated with academic assessment stress among dental undergraduates. J. Dent. Educ. 67, 1091–1094. [PubMed] [Google Scholar]
- Nicholls S. J., Hazen S. L. (2005). Myeloperoxidase and cardiovascular disease. Arterioscler. Thrombosis Vasc. Biol. 25, 1102–1111. 10.1161/01.ATV.0000163262.83456.6d [DOI] [PubMed] [Google Scholar]
- Niedzielska E., Smaga I., Gawlik M., Moniczewski A., Stankowicz P., Pera J., et al. (2016). Oxidative stress in neurodegenerative diseases. Mol. Neurobiol. 53, 4094–4125. 10.5607/en.2015.24.4.325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nielsen B. H., Jacobsen S., Andersen P. H., Niewold T. A., Heegaard P. M. (2004). Acute phase protein concentrations in serum and milk from healthy cows, cows with clinical mastitis and cows with extramammary inflammatory conditions. Vet. Rec. 54, 361–366. 10.1136/vr.154.12.361 [DOI] [PubMed] [Google Scholar]
- Novak M. A., Menard M. T., El-Mallah S. N., Rosenberg K., Lutz C. K., Worlein J., et al. (2017). Assessing significant (>30%) alopecia as a possible biomarker for stress in captive rhesus monkeys (Macaca mulatta). Am. J. Primatol. 79, 1–8. 10.1002/ajp.22547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nuriel T., Deeb R. S., Hajjar D. P., Gross S. S. (2008). Protein 3-nitrotyrosine in complex biological samples: quantification by high-pressure liquid chromatography/electrochemical detection and emergence of proteomic approaches for unbiased identification of modification sites. Methods Enzymol. 441, 1–17. 10.1016/S0076-6879(08)01201-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Brien P. D., Hinder L. M., Callaghan B. C., Feldman E. L. (2017). Neurological consequences of obesity. Lancet Neurol. 16, 465–477. 10.1016/S1474-4422(17)30084-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Odler B., Foris V., Gungl A., Müller V., Hassoun P. M., Kwapiszewska G., et al. (2018). Biomarkers for pulmonary vascular remodeling in systemic sclerosis: a pathophysiological approach. Front. Physiol. 9:587. 10.3389/fphys.2018.00587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Donnell K., Kammerer M., O'Reilly R., Taylor A., Glover V. (2009). Salivary alpha-amylase stability, diurnal profile and lack of response to the cold hand test in young women. Stress 12, 549–554. 10.3109/10253890902822664 [DOI] [PubMed] [Google Scholar]
- Ogawa-Akiyama A., Sugiyama H., Kitagawa M., Tanaka K., Onishi A., Yamanari T., et al. (2018). Serum cystatin C is an independent biomarker associated with the renal resistive index in patients with chronic kidney disease. PLoS ONE 13:e0193695. 10.1371/journal.pone.0193695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohman L., Stridsberg M., Isaksson S., Jerlstad P., Simrén M. (2012). Altered levels of fecal chromogranins and secretogranins in IBS: relevance for pathophysiology and symptoms? Am. J. Gastroenterol. 107, 440–447. 10.1038/ajg.2011.458 [DOI] [PubMed] [Google Scholar]
- Okereke O. I., Prescott J., Wong J. Y., Han J., Rexrode K. M., De Vivo I. (2012). High phobic anxiety is related to lower leukocyte telomere length in women. PLoS ONE 7:e40516. 10.1371/journal.pone.0040516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Onopiuk A., Tokarzewicz A., Gorodkiewicz E. (2015). Cystatin C: a kidney function biomarker. Adv. Clin. Chem. 68, 57–69. 10.1016/bs.acc.2014.11.007 [DOI] [PubMed] [Google Scholar]
- Ottesen A. H., Carlson C. R., Louch W. E., Dahl M. B., Sandbu R. A., Johansen R. F., et al. (2017). Glycosylated chromogranin A in heart failure: implications for processing and cardiomyocyte calcium homeostasis. Circ. Heart Fail. 10:e003675. 10.1161/CIRCHEARTFAILURE.116.003675 [DOI] [PubMed] [Google Scholar]
- Pajcin M., Banks S., Dorrian J., Gupta C. C., Coates A. M., Grant C. L., et al. (2019). Salivary levels of alpha-amylase are associated with neurobehavioral alertness during extended wakefulness, but not simulated night-shift work. Physiol. Behav. 204, 1–9. 10.1016/j.physbeh.2019.02.004 [DOI] [PubMed] [Google Scholar]
- Paltrinieri S. (2008). The feline acute phase reaction. Vet. J. 177, 26–35. 10.1016/j.tvjl.2007.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pandey K. B., Rizvi S. I. (2011). Biomarkers of oxidative stress in red blood cells. Biomed. Pap. Med. Fac. Univ. Palacky. Olomouc. Czech. Repub. 155, 131–136. 10.5507/bp.2011.027 [DOI] [PubMed] [Google Scholar]
- Pandit K., Mukhopadhyay P., Ghosh S., Chowdhury S. (2011). Natriuretic peptides: diagnostic and therapeutic use. Indian J. Endocrinol. Metab. 15, S345–S353. 10.4103/2230-8210.86978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papouin T., Haydon P. G. (2018). D-serine measurements in brain slices or other tissue explants. Bio. Protoc. 8:e2698. 10.21769/BioProtoc.2698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park K. C., Gaze D. C., Collinson P. O., Marber M. S. (2017). Cardiac troponins: from myocardial infarction to chronic disease. Cardiovasc. Res. 113, 1708–1718. 10.1093/cvr/cvx183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel J. B., Shah F. D., Shukla S. N., Shah P. M., Patel P. S. (2009). Role of nitric oxide and antioxidant enzymes in the pathogenesis of oral cancer. J. Cancer Res. Ther. 5, 247–253. 10.4103/0973-1482.59898 [DOI] [PubMed] [Google Scholar]
- Patil S. J., Shah P. P., Patil J. A., Shigli A., Patil A. T., Tamagond S. B. (2015). Assessment of the changes in the stress-related salivary cortisol levels to the various dental procedures in children. J. Indian Soc. Pedod. Prev. Dent. 33, 94–99. 10.4103/0970-4388.155116 [DOI] [PubMed] [Google Scholar]
- Patrono C., Falco A., Davi G. (2005). Isoprostane formation and inhibition in atherothrombosis. Curr. Opin. Pharmacol. 5, 198–203. 10.1016/j.coph.2004.11.003 [DOI] [PubMed] [Google Scholar]
- Pedersen L. H., Aalbaek B., Røntved C. M., Ingvartsen K. L., Sorensen N. S., Heegaard P. M. (2003). Early pathogenesis and inflammatory response in experimental bovine mastitis due to Streptococcus uberis. J. Comp. Pathol. 128, 156–164. 10.1053/jcpa.2002.0620 [DOI] [PubMed] [Google Scholar]
- Peña-Bautista C., Carrascosa-Marco P., Oger C., Vigor C., Galano J. M., Durand T., et al. (2019). Validated analytical method to determine new salivary lipid peroxidation compounds as potential neurodegenerative biomarkers. J. Pham. Biomed. Anal. 164, 742–749. 10.1016/j.jpba.2018.11.043 [DOI] [PubMed] [Google Scholar]
- Peng K. T., Tsai M. H., Lee C. W., Chiang Y. C., Chen P. C., Chen C. C., et al. (2018). Dysregulated expression of antioxidant enzymes in polyethylene particle-induced periprosthetic inflammation and osteolysis. PLoS ONE 13:e0202501. 10.1371/journal.pone.0202501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peng W., Liu Y. N., Zhu S. Q., Li W. Q., Guo F. C. (2018). The correlation of circulating pro-angiogenic mi RNA s' expressions with disease risk, clinicopathological features, and survival profiles in gastric cancer. Cancer Med. 7, 3773–3791. 10.1002/cam4.1618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perera S., Uddin M., Hayes J. A. (1997). Salivary lysozyme: a noninvasive marker for the study of the effects of stress of natural immunity. Int. J. Behav. Med. 4, 170–178. 10.1207/s15327558ijbm0402_5 [DOI] [PubMed] [Google Scholar]
- Pérez-Sánchez C., Arias-de la Rosa I., Aguirre M. Á., Luque-Tévar M., Ruiz-Limón P., Barbarroja N., et al. (2018). Circulating microRNAs as biomarkers of disease and typification of the atherothrombotic status in antiphospholipid syndrome. Haematologica 103, 908–918. 10.3324/haematol.2017.184416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petersen H. H., Nielsen J. P., Heegaard P. M. H. (2004). Application of acute phase protein measurement in veterinary clinical chemistry. Vet. Res. 35, 163–187. 10.1051/vetres:2004002 [DOI] [PubMed] [Google Scholar]
- Pickering R. J., Rosado C. J., Sharma A., Buksh S., Tate M., de Haan J. B. (2018). Recent novel approaches to limit oxidative stress and inflammation in diabetic complications. Clin. Transl. Immunol. 7:e1016. 10.1002/cti2.1016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pineles B. L., Romero R., Montenegro D., Tarca A. L., Han Y. M., Kim Y. M., et al. (2007). Distinct subsets of microRNAs are expressed differentially in the human placentas of patients with preeclampsia. Am J Obstet Gynecol. 196, 261.e1–261.e6. 10.1016/j.ajog.2007.01.008 [DOI] [PubMed] [Google Scholar]
- Pleil J. D., Wallace M. A. G, Stiegel M. A., Funk W. E. (2018). Human biomarker interpretation: the importance of intra-class correlation coefficients (ICC) and their calculations based on mixed models, ANOVA, and variance estimates. J. Toxicol. Environ. Health B Cri.t Rev. 21, 161–180. 10.1080/10937404.2018.1490128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pogribny I. P. (2018). MicroRNAs as biomarkers for clinical studies. Exp. Biol. Med. 243, 283–290. 10.1177/1535370217731291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polineni S., Parker D. M., Alam S. S., Thiessen-Philbrook H., McArthur E., DiScipio A. W., et al. (2018). Predictive ability of novel cardiac biomarkers ST2, Galectin-3, and NT-ProBNP before cardiac surgery. J. Am. Heart Assoc. 7:e008371. 10.1161/JAHA.117.008371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Portilla D., Dent C., Sugaya T., Nagothu K. K., Kundi I., Moore P., et al. (2008). Liver fatty acid-binding protein as a biomarker of acute kidney injury after cardiac surgery. Kidney Int. 73, 465–472. 10.1038/sj.ki.5002721 [DOI] [PubMed] [Google Scholar]
- Prajapati B. M., Gupta J. P., Pandey D. P., Parmar G. A., Chaudhari J. D. (2017). Molecular markers for resistance against infectious diseases of economic importance. Vet. World 10, 112–120. 10.14202/vetworld.2017.112-120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Praticò D., Rokach J., Lawson J., FitzGerald G. A. (2004). F2-isoprostanes as indices of lipid peroxidation in inflammatory diseases. Chem. Phys. Lipids 128, 165–171. 10.1016/j.chemphyslip.2003.09.012 [DOI] [PubMed] [Google Scholar]
- Pullaiah P., Suchitra M. M., Siddhartha Kumar B. (2018). Protein carbonyls and protein thiols in rheumatoid arthritis. Int. J. Res. Med. Sci. 6, 1738–1741. 10.18203/2320-6012.ijrms20181770 [DOI] [Google Scholar]
- Pulvirenti A., Rao D., Mcintyre C. A., Gonen M., Tang L. H., Klimstra D. S., et al. (2019). Limited role of Chromogranin A as clinical biomarker for pancreatic neuroendocrine tumors. HPB (Oxf). 21, 612–618. 10.1016/j.hpb.2018.09.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puppel K., Kapusta A., Kuczynska B. (2015). The etiology of oxidative stress in the various species of animals, a review. J. Sci. Food Agric. 95, 2179–2184. 10.1002/jsfa.7015 [DOI] [PubMed] [Google Scholar]
- Quinn C. M., Duran R. M., Audet G. N., Charkoudian N., Leon L. R. (2014). Cardiovascular and thermoregulatory biomarkers of heat stroke severity in a conscious rat model. J. Appl. Physiol. 117, 971–978. 10.1152/japplphysiol.00365.2014 [DOI] [PubMed] [Google Scholar]
- Qureshi A., Zaigham K., Iqbal M. S., Ali Q. (2016). Detection of endothelin 2 (Et-2) as a novel biomarker of renal dysfunction in patients of liver cirrhosis with ascites. Adv. Life Sci. 3, 112–118. [Google Scholar]
- Radabaugh M. R., Nemirovskiy O. V., Misko T. P., Aggarwal P., Mathews W. R. (2008). Immunoaffinity liquid chromatography-tandem mass spectrometry detection of nitrotyrosine in biological fluids: development of a clinically translatable biomarker. Anal. Biochem. 380, 68–76. 10.1016/j.ab.2008.05.019 [DOI] [PubMed] [Google Scholar]
- Radi R. (2013). Protein tyrosine nitration: Biochemical mechanisms and structural basis of its functional effects. Acc. Chem. Res. 46, 550–559. 10.1021/ar300234c [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raghu C., Ekena J., Cullen J. M., Webb C. B., Trepanier L. A. (2018). Evaluation of potential serum biomarkers of hepatic fibrosis and necroinflammatory activity in dogs with liver disease. J. Vet. Int. Med. 32, 1009–1018. 10.1111/jvim.15064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahal A., Kumar A., Singh V., Yadav B., Tiwari R., Chakraborty S., et al. (2014). Oxidative stress, prooxidants and antioxidants: the interplay. BioMed Res. Int. 2014:761264. 10.1155/2014/761264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rai B., Kaur J. (2011). Salivary stress markers and physiological stress in simulated microgravity. 21 days in 6° head-down tilt. J. Oral. Sci. 53, 103–107. 10.2334/josnusd.53.103 [DOI] [PubMed] [Google Scholar]
- Rajendran L., Honsho M., Zahn T. R., Keller P., Geiger K. D., Verkade P., et al. (2006). Alzheimer's disease β-amyloid peptides are released in association with exosomes. Proc. Natl. Acad. Sci. U.S.A. 103, 11172–11177. 10.1073/pnas.0603838103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramos-Casals M., Retamozo S., Sisó-Almirall A., Pérez-Alvarez R., Pallarés L., Brito-Zerón P. (2019). Clinically-useful serum biomarkers for diagnosis and prognosis of sarcoidosis. Expert Rev. Clin. Immunol. 15, 391–405. 10.1080/1744666X.2019.1568240 [DOI] [PubMed] [Google Scholar]
- Rani A. J., Mythili S. V. (2014). Study on total antioxidant status in relation to oxidative stress in type 2 diabetes mellitus. J. Clin. Diagn. Res. 8, 108–110. 10.7860/JCDR/2014/7603.4121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rashkova M., Kalchev P., Emilova R., Ribagin L., Doganova Tz., Stoeva I. (2010). Cortisol in saliva – a marker for increased anxiety in children. JIMAB Annu. Proc. 16, 67–69. [Google Scholar]
- Reczynska D., Zalewska M., Czopowicz M., Kaba J., Zwierzchowski L., Bagnicka E. (2018). Acute phase protein levels as an auxiliary tool in diagnosing viral diseases in ruminants–a review. Viruses 10:E502. 10.3390/v10090502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rivara M. B., Yeung C. K., Robinson-Cohen C., Phillips B. R., Ruzinski J., Rock D., et al. (2017). Effect of coenzyme Q10 on biomarkers of oxidative stress and cardiac function in hemodialysis patients: the CoQ10 biomarker trial. Am. J. Kidney Dis. 69, 389–399. 10.1053/j.ajkd.2016.08.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson M. W., Harmon C., O'Farrelly C. (2016). Liver immunology and its role in inflammation and homeostasis. Cell Mol. Immunol. 13, 267–276. 10.1038/cmi.2016.3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogalla T., Ehrnsperger M., Preville X., Kotlyarov A., Lutsch G., Ducasse C., et al. (1999). Regulation of Hsp27 oligomerization, chaperone function, and protective activity against oxidative stress/tumor necrosis factor alpha by phosphorylation. J. Biol. Chem. 274, 18947–18956. 10.1074/jbc.274.27.18947 [DOI] [PubMed] [Google Scholar]
- Roser A. E., Caldi Gomes L., Schünemann J., Maass F., Lingor P. (2018). Circulating miRNAs as diagnostic biomarkers for Parkinson's disease. Front. Neurosci. 12:625. 10.3389/fnins.2018.00625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rother R. P., Bell L., Hillmen P., Gladwin M. T. (2005). The clinical sequelae of intravascular hemolysis and extracellular plasma hemoglobin a novel mechanism of human disease. JAMA 293, 1653–1662. 10.1001/jama.293.13.1653 [DOI] [PubMed] [Google Scholar]
- Roy A., Queirolo E., Peregalli F., Mañay N., Martínez G., Kordas K. (2015). Association of blood levels with urinary F2-8α-isoprostane and 8-hydroxy 2-deoxy-guonosine concentrations in first-grade Uruguayan children. Env Res. 140, 127–135. 10.1016/j.envres.2015.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roy S., Trautwein C., Luedde T., Roderburg C. (2018). A general overview on non-coding rna-based diagnostic and therapeutic approaches for liver diseases. Front. Pharmacol. 9:805. 10.3389/fphar.2018.00805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rücker H., Amslinger S. (2015). Identification of heme oxygenase-1 stimulators by a convenient ELISA-based bilirubin quantification assay. Free Radic. Biol. Med. 78, 135–146. 10.1016/j.freeradbiomed.2014.10.506 [DOI] [PubMed] [Google Scholar]
- Russell E., Koren G., Rieder M., Van Uum S. (2012). Hair cortisol as a biological marker of chronic stress: current status, future directions and unanswered questions. Psychoneuroendocrinology 37, 589–601. 10.1016/j.psyneuen.2011.09.009 [DOI] [PubMed] [Google Scholar]
- Ryu Y., Gracia-Lor E., Bade R., Baz-Lomba J. A., Bramness J. G., Castiglioni S., et al. (2016). Increased levels of the oxidative stress biomarker 8-iso-prostaglandin F2α in wastewater associated with tobacco use. Sci. Rep. 6:39055. 10.1038/srep39055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saban K. L., Mathews H. L., Bryant F. B., Tell D., Joyce C., DeVon H. A., et al. (2018). Perceived discrimination is associated with the inflammatory response to acute laboratory stress in women at risk for cardiovascular disease. Brain Behav. Immun. 73, 625–632. 10.1016/j.bbi.2018.07.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabat R., Ouyang W., Wolk K. (2014). Therapeutic opportunities of the IL-22-IL-22R1 system. Nat. Rev. Drug Discov.13, 21–38. 10.1038/nrd4176 [DOI] [PubMed] [Google Scholar]
- Sahu P., Pinkalwar N., Dubey R. D., Paroha S., Chatterjee S., Chatterjee T. (2011). Biomarkers: an emerging tool for diagnosis of a disease and drug development. Asian J. Res. Pharm. Sci. 1, 9–16. [Google Scholar]
- Saleem U., Khaleghi M., Morgenthaler N. G., Bergmann A., Struck J., Mosley T. H. J., et al. (2009). Plasma carboxy-terminal provasopressin (copeptin): a novel marker of insulin resistance and metabolic syndrome. J. Clin. Endocrinol. Metab. 94, 2558–2564. 10.1210/jc.2008-2278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sales C. F., Lemos F. S., Morais R. D. V. S., Thomé R. G., Santos H. B., Pinheiro A. P. B., et al. (2018). Thermal stress induces heat shock protein 70 and apoptosis during embryo development in a Neotropical freshwater fish. Reprod. Fertil. Dev. 31, 547–556. 10.1071/RD18217 [DOI] [PubMed] [Google Scholar]
- Saman S., Kim W., Raya M., Visnick Y., Miro S., Saman S., et al. (2012). Exosome-associated tau is secreted in tauopathy models and is selectively phosphorylated in cerebrospinal fluid in early Alzheimer disease. J. Biol. Chem. 287, 3842–3849. 10.1074/jbc.M111.277061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santangelo A., Tamanini A., Cabrini G., Dechecchi M. C. (2017). Circulating microRNAs as emerging non-invasive biomarkers for gliomas. Ann. Transl. Med. 5:277. 10.21037/atm.2017.06.15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santoro M. G. (2000). Heat shock factors and the control of the stress response. Biochem. Pharmacol. 59, 55–63. 10.1016/s0006-2952(99)00299-3 [DOI] [PubMed] [Google Scholar]
- Santos V. A., Lollo P. C. B., Cantero M. A., Moura C. S., Amaya-Farfan J., Morato P. N. (2018). Heat shock proteins: protection and potential biomarkers for ischemic injury of cardiomyocytes after surgery. Braz. J. Cardiovasc. Surg. 33, 291–302. 10.21470/1678-9741-2017-0169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santos V. S., Goletti D., Kontogianni K., Adams E. R., Molina-Moya B., Dominguez J., et al. (2019). Acute phase proteins and IP-10 as triage tests for the diagnosis of tuberculosis: systematic review and meta-analysis. Clin. Microbiol. Infect. 25, 169–177. 10.1016/j.cmi.2018.07.017 [DOI] [PubMed] [Google Scholar]
- Schmidt U., Kaltwasser S. F., Wotjak C. T. (2013). Biomarkers in posttraumatic stress disorder: overview and implications for future research. Dis. Markers 35, 43–54. 10.1155/2013/835876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schrag M., Mueller C., Zabel M., Crofton A., Kirsch W. M., Ghribi O., et al. (2013). Oxidative stress in blood in Alzheimer's disease and mild cognitive impairment: a meta-analysis. Neurobiol. Dis. 59, 100–110. 10.1016/j.nbd.2013.07.005 [DOI] [PubMed] [Google Scholar]
- Schrödl W., Büchler R., Wendler S., Reinhold P., Muckova P., Reindl J., et al. (2016). Acute phase proteins as promising biomarkers: perspectives and limitations for human and veterinary medicine. Proteomics Clin. Appl. 10, 1077–1092. 10.1002/prca.201600028 [DOI] [PubMed] [Google Scholar]
- Schueller F., Roy S., Vucur M., Trautwein C., Luedde T., Roderburg C. (2018). The role of miRNAs in the pathophysiology of liver diseases and toxicity. Intern. J. Mol. Sci. 19:261. 10.3390/ijms19010261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz G. J., Kwong T., Erway B., Warady B., Sokoll L., Hellerstein S., et al. (2009). Validation of creatinine assays utilizing HPLC and IDMS traceable standards in sera of children. Pediatr. Nephrol. 24, 113–119. 10.1007/s00467-008-0957-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sciacchitano S., Lavra L., Morgante A., Ulivieri A., Magi F., De Francesco G. P., et al. (2018). Galectin-3: one molecule for an alphabet of diseases, from A to Z. Int. J. Mol. Sci. 19:E379. 10.3390/ijms19020379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selleck M. J., Senthil M., Wall N. R. (2017). Making meaningful clinical use of biomarkers. Biomark. Insights 12:1177271917715236. 10.1177/1177271917715236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sentellas S., Morales-Ibanez O., Zanuy M., Albertí J. J. (2014). GSSG/GSH ratios in cryopreserved rat and human hepatocytes as a biomarker for drug induced oxidative stress. Toxicol. In Vitro. 28, 1006–1015. 10.1016/j.tiv.2014.04.017 [DOI] [PubMed] [Google Scholar]
- Shaffi S. K., Galas D., Etheridge A., Argyropoulos C. (2018). Role of microRNAs in renal parenchymal diseases-A new dimension. Inter. J. Mol. Sci. 19, 1797. 10.3390/ijms19061797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah B., Ashok L., Sujatha G. P. (2009). Evaluation of salivary cortisol and psychological factors in patients with oral lichen planus. Indian J. Dent. Res. 20, 288–292. 10.4103/0970-9290.57361 [DOI] [PubMed] [Google Scholar]
- Shahanaze J., Jayachandran S., Madhusmita M., Soundravally R. (2018). Clinical utility of pleural fluid YKL-40 as a marker of malignant pleural effusion. Curr. Probl. Cancer 43, 354–362. 10.1016/j.currproblcancer.2018.10.001 [DOI] [PubMed] [Google Scholar]
- Shamay A., Homans R., Fuerman Y., Levin I., Barash H., Silanikove N., et al. (2005). Expression of albumin in nonhepatic tissues and its synthesis by the bovine mammary gland. J. Dairy Sci. 88, 569–576. 10.3168/jds.S0022-0302(05)72719-3 [DOI] [PubMed] [Google Scholar]
- Shan L. P., Chen X. H., Ling F., Zhu B., Wang G. X. (2018). Targeting heat shock protein 70 as an antiviral strategy against grass carp reovirus infection. Virus Res. 247, 1–9. 10.1016/j.virusres.2018.01.005 [DOI] [PubMed] [Google Scholar]
- Sharma A., Tate M., Mathew G., Vince J. E., Ritchie R. H., de Haan J. B. (2018). Oxidative stress and NLRP3-inflammasome activity as significant drivers of diabetic cardiovascular complications: therapeutic implications. Front. Physiol. 9:114. 10.3389/fphys.2018.00114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen S., Lin Y., Yuan X., Shen L., Chen J., Chen L., et al. (2016). Biomarker microRNAs for diagnosis, prognosis and treatment of hepatocellular carcinoma: a functional survey and comparison. Sci. Rep. 6:38311. 10.1038/srep38311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherwani S. I., Khan H. A., Ekhzaimy A., Masood A., Sakharkar M. K. (2016). Significance of HbA1c test in diagnosis and prognosis of diabetic patients. Biomark Insights 11, 95–104. 10.4137/BMI.S38440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi M., Jiang Y., Yang L., Yan S., Wang Y. G., Lu X. J. (2018). Decreased levels of serum exosomal miR-638 predict poor prognosis in hepatocellular carcinoma. J. Cell Biochem. 119, 4711–4716. 10.1002/jcb.26650 [DOI] [PubMed] [Google Scholar]
- Shi Y., Zhang J., He J., Liu D., Meng X., Huang T., et al. (2019). A method of detecting two tumor markers (p-hydroxybenzoic acid and p-cresol) in human urine using a porous magnetic β-cyclodextrine polymer as solid phase extractant, an alternative for early gastric cancer diagnosis. Talanta 191, 133–140. 10.1016/j.talanta.2018.08.036 [DOI] [PubMed] [Google Scholar]
- Shrestha L., Bolaender A., Patel H. J., Taldone T. (2016). Heat shock protein (HSP) drug discovery and development: targeting heat shock proteins in disease. Curr. Top. Med. Chem. 16, 2753–2764. 10.2174/1568026616666160413141911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrotriya S., Walsh D., Nowacki A. S., Lorton C., Aktas A., Hullihen B., et al. (2018). Serum C-reactive protein is an important and powerful prognostic biomarker in most adult solid tumors. PLoS ONE 13:e0202555. 10.1371/journal.pone.0202555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siddiqui I., Ahmed S., Abid S. (2016). Update on diagnostic value of breath test in gastrointestinal and liver diseases. World J. Gastrointest. Pathophysiol. 7, 256–265. 10.4291/wjgp.v7.i3.256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siddiqui I., Majid H., Abid S. (2017). Update on clinical and research application of fecal biomarkers for gastrointestinal diseases. World J. Gastroint. Pharmacol. Ther. 8, 39–46. 10.4292/wjgpt.v8.i1.39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva R. P., Barros C. L., Mendes T. T., Garcia E. S., Valenti V. E., de Abreu L. C., et al. (2019). The influence of a hot environment on physiological stress responses in exercise until exhaustion. PLoS ONE 14:e0209510 10.1371/journal.pone.0209510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva-Costa L. C., Carlson P. T., Guest P. C., de Almeida V., Martins-de-Souza D. (2019). Proteomic markers for depression, in Reviews on Biomarker Studies in Psychiatric and Neurodegenerative Disorders, ed Guest P. C. (Cham: Springer Nature, 191–206. [DOI] [PubMed] [Google Scholar]
- Simioni C., Zauli G., Martelli A. M., Vitale M., Sacchetti G., Gonelli A., et al. (2018). Oxidative stress: role of physical exercise and antioxidant nutraceuticals in adulthood and aging. Oncotarget 9, 17181–17198. 10.18632/oncotarget.24729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh S., Brocker C., Koppaka V., Chen Y., Jackson B. C., Matsumoto A., et al. (2013). Aldehyde dehydrogenases in cellular responses to oxidative/electrophilic stress. Free Radic. Biol. Med. 56, 89–101. 10.1016/j.freeradbiomed.2012.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh S., Gupta S. K., Seth P. K. (2018). Biomarkers for detection, prognosis and therapeutic assessment of neurological disorders. Rev. Neurosci. 29, 771–789. 10.1515/revneuro-2017-0097 [DOI] [PubMed] [Google Scholar]
- Singh V. P., Bali A., Singh N., Jaggi A. S. (2014). Advanced glycation end products and diabetic complications. Korean J. Physiol. Pharmacol. 18, 1–14. 10.4196/kjpp.2014.18.1.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh Z., Karthisegu I. P., Singh P., Kaur R. (2014). Use of malondialdehyde as a biomarker for assessing oxidative stress in different disease pathologies: a review. Iranian J. Public Health 43, 7–16. [PMC free article] [PubMed] [Google Scholar]
- Siti Hajar M. H., Zulkefli S., Juwita S., Norhayati M. N., Siti Suhaila M. Y., Rasool A., et al. (2018). Metabolic, inflammatory, and oxidative stress markers in women exposed to secondhand smoke. Peer J. 6:e5758. 10.7717/peerj.5758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skálová S. (2005). The diagnostic role of urinary N-acetyl-beta-D-glucosaminidase (NAG) activity in the detection of renal tubular impairment. Acta Med. 48, 75–80. [PubMed] [Google Scholar]
- Skórzynska-Dziduszko K. E., Kimber-Trojnar Z., Patro-Małysza J., Stenzel-Bembenek A., Oleszczuk J., Leszczynska-Gorzelak B. (2018). Heat shock proteins as a potential therapeutic target in the treatment of gestational diabetes mellitus: what we know so far. Int. J. Mol. Sci. 19:E3205. 10.3390/ijms19103205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Small H. Y., Migliarino S., Czesnikiewicz-Guzik M., Guzik T. J. (2018). Hypertension: focus on autoimmunity and oxidative stress. Free Radic. Biol. Med. 125, 104–115. 10.1016/j.freeradbiomed.2018.05.085 [DOI] [PubMed] [Google Scholar]
- Smith K. A., Shepherd J., Wakil A., Kilpatrick E. S. (2011). A comparison of methods for the measurement of 8-isoPGF (2 alpha): a marker of oxidative stress. Ann. Clin. Biochem. 48, 147–154. 10.1258/acb.2010.010151 [DOI] [PubMed] [Google Scholar]
- Sordillo L. M., Aitken S. L. (2009). Impact of oxidative stress on the health and immune function of dairy cattle. Vet. Immunol. Immunopathol. 128, 104–109. 10.1016/j.vetimm.2008.10.305 [DOI] [PubMed] [Google Scholar]
- Soto-Mendez M. J., Aguilera C. M., Mesa M. D., Campaña-Martín L., Martín-Laguna V., Solomons N. W., et al. (2016). Strong associations exist among oxidative stress and antioxidant biomarkers in the circulating, cellular and urinary anatomical compartments in Guatemalan children from the western highlands. PLoS ONE 11:e0146921 10.1371/journal.pone.0146921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soudry E., Shavit S. S., Hardy B., Morgenstern S., Hadar T., Feinmesser R. (2017). Heat shock proteins HSP90, HSP70 and GRP78 expression in medullary thyroid carcinoma. Ann. Diagnost. Pathol. 26, 52–56. 10.1016/j.anndiagpath.2016.11.003 [DOI] [PubMed] [Google Scholar]
- Srinivasan M., Meadows M. L., Maxwell L. (2018). Assessment of salivary adipokines resistin, visfatin, and ghrelin as type 2 diabetes mellitus biomarkers. Biochem. Res. Int. 2018:7463796. 10.1155/2018/7463796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stafforini D. M., Sheller J. R., Blackwell T. S., Sapirstein A., Yull F. E., McIntyre T. M., et al. (2006). Release of free F2-isoprostanes from esterified phospholipids is catalyzed by intracellular and plasma platelet-activating factor acetylhydrolases. J. Biol. Chem. 281, 4616–4623. 10.1074/jbc.M507340200 [DOI] [PubMed] [Google Scholar]
- Staley M., Conners M. G., Hall K., Miller L. J. (2018). Linking stress and immunity: Immunoglobulin A as a non-invasive physiological biomarker in animal welfare studies. Horm Behav. 102, 55–68. 10.1016/j.yhbeh.2018.04.011 [DOI] [PubMed] [Google Scholar]
- Stamp L. K., Zhu X., Dalbeth N., Jordan S., Edwards N. L., Taylor W. (2011). Serum urate as a soluble biomarker in chronic gout-evidence that serum urate fulfills the OMERACT validation criteria for soluble biomarkers. Semin. Arthritis Rheum. 40, 483–500. 10.1016/j.semarthrit.2010.09.003 [DOI] [PubMed] [Google Scholar]
- Stanciu A. E., Stanciu M. M., Vatasescu R. G. (2018). NT-proBNP and CA 125 levels are associated with increased pro-inflammatory cytokines in coronary sinus serum of patients with chronic heart failure. Cytokine 1, 13–19. 10.1016/j.cyto.2018.07.037 [DOI] [PubMed] [Google Scholar]
- Stanescu I. I., Calenic B., Dima A., Gugoasa L. A., Balanescu E., Stefan-van Staden R. I., et al. (2018). Salivary biomarkers of inflammation in systemic lupus erythematosus. Ann. Anat. 219, 89–93. 10.1016/j.aanat.2018.02.012 [DOI] [PubMed] [Google Scholar]
- Steudte-Schmiedgen S., Wichmann S., Stalder T., Hilbert K., Muehlhan M., Lueken U., et al. (2017). Hair cortisol concentrations and cortisol stress reactivity in generalized anxiety disorder, major depression and their comorbidity. J. Psychiatric Res. 84, 184–190. 10.1016/j.jpsychires.2016.09.024 [DOI] [PubMed] [Google Scholar]
- Stjärne Aspelund A., Hammarström H., Inghammar M., Larsson H., Hansson L., Christensson B., et al. (2018). Heparin-binding protein, lysozyme, and inflammatory cytokines in bronchoalveolar lavage fluid as diagnostic tools for pulmonary infection in lung transplanted patients. Am. J. Transplant. 18, 444–452. 10.1111/ajt.14458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stocker R., Keaney J. F. (2004). Role of oxidative modifications in atherosclerosis. Physiol. Rev. 84, 1381–1478. 10.1152/physrev.00047.2003 [DOI] [PubMed] [Google Scholar]
- Strahler J., Mueller A., Rosenloecher F., Kirschbaum C., Rohleder N. (2010). Salivary alpha-amylase stress reactivity across different age groups. Psychophysiology 47, 587–595. 10.1111/j.1469-8986.2009.00957.x [DOI] [PubMed] [Google Scholar]
- Su G., Zhang T., Yang H. X., Dai W. L., Wang T., Tian L., et al. (2019). Association of isoprostanes-related oxidative stress with vulnerability of culprit lesions in diabetic patients with acute coronary syndrome. Int. Heart J. 60, 271–279. 10.1536/ihj.18-233 [DOI] [PubMed] [Google Scholar]
- Su H., Gornitsky M., Velly A. M., Yu H., Benarroch M., Schipper H. M. (2009). Salivary DNA, lipid, and protein oxidation in nonsmokers with periodontal disease. Free Radic. Biol. Med. 46, 914–921. 10.1016/j.freeradbiomed.2009.01.008 [DOI] [PubMed] [Google Scholar]
- Sugiyama S., Kugiyama K., Aikawa M., Nakamura S., Ogawa H., Libby P. (2004). Hypochlorous acid, a macrophage product, induces endothelial apoptosis and tissue factor expression: involvement of myeloperoxidase- mediated oxidant in plaque erosion and thrombogenesis. Arterioscler. Thromb. Vasc. Biol. 24:13091314. 10.1161/01.ATV.0000131784.50633.4f [DOI] [PubMed] [Google Scholar]
- Sugiyama S., Okada Y., Sukhova G. K., Virmani R., Heinecke J. W., Libby P. (2001). Macrophage myeloperoxidase regulation by granulocyte macrophage colony-stimulating factor in human atherosclerosis and implications in acute coronary syndromes. Am. J. Pathol. 158, 879–891. 10.1016/S0002-9440(10)64036-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suh M. (2018). Salivary cortisol profile under different stressful situations in female college students moderating role of anxiety and sleep. J. Neurosci. Nursing. 50, 279–285. 10.1097/JNN.0000000000000394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun D., Zhuang X., Zhang S., Deng Z. B., Grizzle W., Miller D., et al. (2013). Exosomes are endogenous nanoparticles that can deliver biological information between cells. Adv. Drug Deliv. Rev. 65, 342–347. 10.1016/j.addr.2012.07.002 [DOI] [PubMed] [Google Scholar]
- Sung C. C., Hsu Y. C., Chen C. C., Lin Y. F., Wu C. C. (2013). Oxidative stress and nucleic acid oxidation in patients with chronic kidney disease. Oxid. Med. Cell Longev. 2013:301982. 10.1155/2013/301982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swarup V., Rajeswari R. M. (2007). Circulating (cell-free) nucleic acids–a promising, non-invasive tool for early detection of several human diseases. FEBS Lett. 581, 795–799. 10.1016/j.febslet.2007.01.051 [DOI] [PubMed] [Google Scholar]
- Tainsky M. A. (2009). Genomic and proteomic biomarkers for cancer: a multitude of opportunities. Biochim. Biophys. Acta 1796, 176–193. 10.1016/j.bbcan.2009.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takahashi A., Flanigan M. E., McEwen B. S., Russo S. J. (2018). Aggression, social stress, and the immune system in humans and animal models. Front. Behavioral Neurosci. 12:56. 10.3389/fnbeh.2018.00056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takahashi S., Nakasatomi M., Takei Y., Ikeuchi H., Sakairi T., Kaneko Y., et al. (2018). Identification of urinary activin A as a novel biomarker reflecting the severity of acute kidney injury. Sci. Rep. 8:5176. 10.1038/s41598-018-23564-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takai N., Yamaguchi M., Aragaki T., Eto K., Uchihashi K., Nishikawa Y. (2004). Effect of physiological stress on salivary cortisol and amylase levels in healthy young adults. Arch. Oral Biol. 49, 963–968. 10.1016/j.archoralbio.2004.06.007 [DOI] [PubMed] [Google Scholar]
- Takamura T. A., Tsuchiya T., Oda M., Watanabe M., Saito R., Sato-Ishida R., et al. (2017). Circulating malondialdehyde-modified low-density lipoprotein (MDA-LDL) as a novel predictor of clinical outcome after endovascular therapy in patients with peripheral artery disease (PAD). Atherosclerosis 263, 192–197. 10.1016/j.atherosclerosis.2017.06.029 [DOI] [PubMed] [Google Scholar]
- Takatsuji K., Sugimoto Y., Ishizaki S., Ozaki Y., Matsuyama E., Yamaguchi Y. (2008). The effects of examination stress on salivary cortisol, immunoglobulin A, and chromogranin A in nursing students. Biomed. Res. 29, 221–224. 10.2220/biomedres.29.221 [DOI] [PubMed] [Google Scholar]
- Tamm N. N., Seferian K. R., Semenov A. G., Mukharyamova K. S., Koshkina E. V., Krasnoselsky M. I., et al. (2008). Novel immunoassay for quantification of brain natriuretic peptide and its precursor in human blood. Clin. Chem. 54, 1511–1518. 10.1373/clinchem.100545 [DOI] [PubMed] [Google Scholar]
- Tampa M., Sarbu M. I., Mitran M. I., Mitran C. I., Matei C., Georgescu S. R. (2018). The pathophysiological mechanisms and the quest for biomarkers in psoriasis, a stress-related skin disease. Dis. Markers 2018:5823684. 10.1155/2018/5823684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan B. L., Norhaizan M. E., Liew W. P., Sulaiman Rahman H. (2018). Antioxidant and oxidative stress: a mutual interplay in age-related diseases. Front. Pharmacol. 9:1162. 10.3389/fphar.2018.01162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan K., Sethi S. K. (2014). Biomarkers in cardiorenal syndromes. Transl. Res. 164, 122–134. 10.1016/j.trsl.2014.04.011 [DOI] [PubMed] [Google Scholar]
- Tanaka Y., Kamohara H., Kinoshita K., Kurashige J., Ishimoto T., Iwatsuki M., et al. (2013). Clinical impact of serum exosomal microRNA-21 as a clinical biomarker in human esophageal squamous cell carcinoma. Cancer 119, 1159–1167. 10.1002/cncr.27895 [DOI] [PubMed] [Google Scholar]
- Tang T., Yang C., Brown H. E., Huang J. (2018). Circulating heat shock protein 70 is a novel biomarker for early diagnosis of lung cancer. Dis. Markers 2018:6184162. 10.1155/2018/6184162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang X. G., Wen J., Zhang X. S., Jiang D. C. (2018). Association between decreased osteopontin and acute mountain sickness upon rapid ascent to 3500 m among young Chinese men. J. Travel. Med. 25:tay075. 10.1093/jtm/tay075 [DOI] [PubMed] [Google Scholar]
- Tasneem M., Mannix C., Wong A., Zhang J., Rangan G. (2018). Is serum copeptin a modifiable biomarker in autosomal dominant polycystic kidney disease? World J. Nephrol. 7, 51–57. 10.5527/wjn.v7.i2.51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor D. D., Gercel-Taylor C. (2008). MicroRNA signatures of tumor-derived exosomes as diagnostic biomarkers of ovarian cancer. Gynecolc. Oncol. 110, 13–21. 10.1016/j.ygyno.2008.04.033 [DOI] [PubMed] [Google Scholar]
- Tesch G. H. (2010). Review: serum and urine biomarkers of kidney disease: a pathophysiological perspective. Nephrology 15, 609–616. 10.1111/j.1440-1797.2010.01361.x [DOI] [PubMed] [Google Scholar]
- Tessier-Vetzel D., Tissier R., Chetboul V., Carlos C., Nicolle A., Benbaron D., et al. (2006). Diagnostic and prognostic value of endothelin-1 plasma concentrations in dogs with heart and respiratory disorders. Vet. Rec. 158, 783–788. 10.1136/vr.158.23.783 [DOI] [PubMed] [Google Scholar]
- Testa U., Pelosi E., Castelli G., Labbaye C. (2017). miR-146 and miR-155: two key modulators of immune response and tumor development. Noncoding RNA 3:E22. 10.3390/ncrna3030022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Théry C., Zitvogel L., Amigorena S. (2002). Exosomes: composition, biogenesis and function. Nat. Rev. Immunol. 2, 569–579. 10.1038/nri855 [DOI] [PubMed] [Google Scholar]
- Tiku M. L., Narla H., Jain M., Yalamanchili P. (2007). Glucosamine prevents in vitro collagen degradation in chondrocytes by inhibiting advanced lipoxidation reactions and protein oxidation. Arthritis Res. Ther. 9:R76. 10.1186/ar2274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Topal A., Alak G., Altun S., Erol H. S., Atamanalp M. (2017). Evaluation of 8-hydroxy-2-deoxyguanosine and NF-kB activation, oxidative stress response, acetylcholinesterase activity, and histopathological changes in rainbow trout brain exposed to linuron. Environ. Toxicol. Pharmacol. 49, 14–20. 10.1016/j.etap.2016.11.009 [DOI] [PubMed] [Google Scholar]
- Tothova C., Nagy O., Seize H., Kovac G. (2010). The effect of chronic respiratory diseases on acute phase proteins and selected blood parameters of protein metabolism in calves. Berl. Munch. Tierarztl. Wochenschr. 123, 307–313. 10.2376/0005-9366-123-307 [DOI] [PubMed] [Google Scholar]
- Tran V., Tindula G., Huen K., Bradman A., Harley K., Kogut K., et al. (2017). Prenatal phthalate exposure and 8-isoprostane among Mexican-American children with high prevalence of obesity. J. Dev. Ori. Health Dis. 8, 196–205. 10.1017/S2040174416000763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trigona W. L., Mullarky I. K., Cao Y., Sordillo L. M. (2006). Thioredoxin reductase regulates the induction of haem oxygenase-1 expression in aortic endothelial cells. Biochem. J. 394, 207–216. 10.1042/BJ20050712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trpkovic A., Resanovic I., Stanimirovic J., Radak D., Mousa S. A., Cenic-Milosevic D., et al. (2015). Oxidized low-density lipoprotein as a biomarker of cardiovascular diseases. Crit. Rev. Clin. Lab Sci. 52, 70–85. 10.3109/10408363.2014.992063 [DOI] [PubMed] [Google Scholar]
- Trzybulska D., Vergadi E., Tsatsanis C. (2018). miRNA and other non-coding rnas as promising diagnostic markers. EJIFCC 29, 221–226. [PMC free article] [PubMed] [Google Scholar]
- Tsikas D., Rothmann S., Schneider J. Y., Suchy M. T., Trettin A., Modun D., et al. (2016). Development, validation and biomedical applications of stable-isotope dilution GC–MS and GC–MS/MS techniques for circulating malondialdehyde (MDA) after pentafluorobenzyl bromide derivatization: MDA as a biomarker of oxidative stress and its relation to 15 (S)-8-iso-prostaglandin F 2α and nitric oxide (NO). J. Chromatogr. B 1019, 95–111. 10.1016/j.jchromb.2015.10.009 [DOI] [PubMed] [Google Scholar]
- Tsimikas S. (2006). Oxidative biomarkers in the diagnosis and prognosis of cardiovascular disease. Am. J. Cardiol. 98, S9–S17. 10.1016/j.amjcard.2006.09.015 [DOI] [PubMed] [Google Scholar]
- Tsuji M., Kawamoto T., Koriyama C., Matsumural F. (2012). IL-22 mRNA Expression in blood samples as a useful biomarker for assessing the adverse health effects of PCBs on allergic children. Int. J. Environ. Res. Public Health 9, 4321–4332. 10.3390/ijerph9124321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker P. S., Dalbo V. J., Han T., Kingsley M. I. (2013). Clinical and research markers of oxidative stress in chronic kidney disease. Biomarkers 18, 103–115. 10.3109/1354750X.2012.749302 [DOI] [PubMed] [Google Scholar]
- Turk R., Juretic D., Geres D., Turk N., Rekic B., Simeon-Rudolf V., et al. (2004). Serum paraoxonase activity and lipid parameters in the early postpartum period of dairy cows. Res. Vet. Sci. 76, 57–61. 10.1016/j.rvsc.2003.08.001 [DOI] [PubMed] [Google Scholar]
- Turner M. D., Ship J. A. (2008). Salivary secretion in health and disease, in Salivary Diagnostics, ed. Wong D. T. (IA: Wiley-Blackwell, 60–68. [Google Scholar]
- Umeno A., Biju V., Yoshida Y. (2017). In vivo ROS production and use of oxidative stress-derived biomarkers to detect the onset of diseases such as Alzheimer's disease, Parkinson's disease, and diabetes. Free Radic. Res. 51, 413–427. 10.1080/10715762.2017.1315114 [DOI] [PubMed] [Google Scholar]
- Umeoka E. H., Robinson E. J., Turimella S. L., van Campen J. S, Motta-Teixeira R. L. C., Sarabdjitsingh A., et al. (2019). Hyperthermia-induced seizures followed by repetitive stress are associated with age-dependent changes in specific aspects of the mouse stress system. J. Neuroendocrinol. 31:e12697. 10.1111/jne.12697 [DOI] [PubMed] [Google Scholar]
- Vaidya V. S., Ford G. M., Waikar S. S., Wang Y., Clement M. B., Ramirez V., et al. (2009). A rapid urine test for early detection of kidney injury. Kidney Int. 76, 108–114. 10.1038/ki.2009.96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vainer N., Dehlendorff C., Johansen J. S. (2018). Systematic literature review of IL-6 as a biomarker or treatment target in patients with gastric, bile duct, pancreatic and colorectal cancer. Oncotarget 9, 29820–29841. 10.18632/oncotarget.25661 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaishnav D., Holkar S., Hivre M. (2015). Serum bilirubin as a marker of oxidative stress in patients with hypertension. Hypertension 5:6. [Google Scholar]
- Vaishya S., Sarwade R. D., Seshadri V. (2018). MicroRNA, proteins, and metabolites as novel biomarkers for prediabetes, diabetes, and related complications. Front. Endocrinol. 9:180. 10.3389/fendo.2018.00180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaisvaser S., Modai S., Farberov L., Lin T., Sharon H., Gilam A., et al. (2016). Neuro-epigenetic indications of acute stress response in humans: the case of MicroRNA-29c. PLoS ONE 11:e0146236. 10.1371/journal.pone.0146236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Campen J. S., Hessel E. V. S., Bohmbach K., Rizzi G., Lucassen P. J., Lakshmi Turimella S., et al. (2018). Stress and corticosteroids aggravate morphological changes in the dentate gyrus after early-life experimental febrile seizures in mice. Front. Endocrinol. 9:3. 10.3389/fendo.2018.00003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Kolk J. H., Pacholewska A., Gerber V. (2015). The role of microRNAs in equine medicine: a review. Vet. Q. 35, 88–96. 10.1080/01652176.2015.1021186 [DOI] [PubMed] [Google Scholar]
- van der Reest J., Lilla S., Zheng L., Zanivan S., Gottlieb E. (2018). Proteome-wide analysis of cysteine oxidation reveals metabolic sensitivity to redox stress. Nat. Commun. 9:1581. 10.1038/s41467-018-04003-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Eden W., Wick G., Albani S., Cohen I. (2010). Stress, heat shock proteins, and autoimmunity. How immune responses to heat shock proteins are to be used for the control of chronic inflammatory diseases. Ann. N. Y. Acad. Sci. 1113, 217–237. 10.1196/annals.1391.020 [DOI] [PubMed] [Google Scholar]
- Van Timmeren M. M., van den Heuvel M. C., Bailly V., Bakker S. J., van Goor H., Stegeman C. A. (2007). Tubular kidney injury molecule-1 (KIM-1) in human renal disease. J. Pathol. 212, 209–217. 10.1002/path.2175 [DOI] [PubMed] [Google Scholar]
- Vance T. M., Azabdaftari G., Pop E. A., Lee S. G., Su L. J., Fontham E. T., et al. (2016). Intake of dietary antioxidants is inversely associated with biomarkers of oxidative stress among men with prostate cancer. Br. J. Nutr. 115, 68–74. 10.1017/S0007114515004249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van't Erve T. J. (2018). Strategies to decrease oxidative stress biomarker levels in human medical conditions: a meta-analysis on 8-iso-prostaglandin F2α. Redox Biol. 17, 284–296. 10.1016/j.redox.2018.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van't Erve T. J., Lih F. B., Jelsema C., Deterding L. J., Eling T. E., Mason R. P., et al. (2016). Reinterpreting the best biomarker of oxidative stress: the 8-iso-prostaglandin F 2α/prostaglandin F 2α ratio shows complex origins of lipid peroxidation biomarkers in animal models. Free Radic. Biol. Med. 95, 65–73. 10.1016/j.freeradbiomed.2016.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verber N. S., Shepheard S. R., Sassani M., McDonough H. E., Moore S. A., Alix J. J. P., et al. (2019). Biomarkers in motor neuron disease: a state of the art review. Front. Neurol. 10:291. 10.3389/fneur.2019.00291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verbrugghe A., Janssens G. P., Van de Velde H., Cox E., De Smet S., Vlaeminck B., et al. (2014). Failure of a dietary model to affect markers of inflammation in domestic cats. BMC Vet. Res. 10:104. 10.1186/1746-6148-10-104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vernunft A., Viergutz T., Plinski C., Weitzel J. M. (2014). Postpartum levels of 8-iso-prostaglandin F2α in plasma and milk phospholipid fractions as biomarker of oxidative stress in first-lactating dairy cows. Prostaglandins Other Lipid Mediat. 112, 34–38. 10.1016/j.prostaglandins.2014.07.004 [DOI] [PubMed] [Google Scholar]
- Vidyasagar A., Wilson N. A., Djamali A. (2012). Heat shock protein 27 (HSP27): biomarker of disease and therapeutic target. Fibrinogenesis Tissue Repair 5:7. 10.1186/1755-1536-5-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vijayan M., Reddy P. H. (2016). Peripheral biomarkers of stroke: Focus on circulatory microRNAs. Biochim. Biophys. Acta 1862, 1984–1993. 10.1016/j.bbadis.2016.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vineetha R., Pai K. M., Vengal M., Gopalakrishna K., Narayanakurup D. (2014). Usefulness of salivary alpha amylase as a biomarker of chronic stress and stress related oral mucosal changes–a pilot study. J. Clin. Exp. Dent. 6, e132–e137. 10.4317/jced.51355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Virzì G. M., Breglia A., Brocca A., de Cal M., Bolin C., Vescovo G., et al. (2018). Levels of proinflammatory cytokines, oxidative stress, and tissue damage markers in patients with acute heart failure with and without cardiorenal syndrome type 1. Cardiorenal. Med. 8, 321–331. 10.1159/000492602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vodovar N., Mebazaa A., Januzzi J. L., Jr., Murtagh G., Stough W. G., Adams K. F., Jr., et al. (2018). Evolution of natriuretic peptide biomarkers in heart failure: implications for clinical care and clinical trials. Int. J. Cardiol. 254, 215–221. 10.1016/j.ijcard.2017.11.001 [DOI] [PubMed] [Google Scholar]
- Wagner J., Cik M., Marth E., Santner B. I., Gallasch E., Lackner A., et al. (2010). Feasibility of testing three salivary stress biomarkers in relation to naturalistic traffic noise exposure. Int. J. Hyg. Environ. Health 213, 153–155. 10.1016/j.ijheh.2009.08.004 [DOI] [PubMed] [Google Scholar]
- Waikar S. S., Bonventre J. V. (2006). Can we rely on blood urea nitrogen as a biomarker to determine when to initiate dialysis? Clin. J. Am. Soc. Nephrol. 1, 903–904. 10.2215/CJN.02560706 [DOI] [PubMed] [Google Scholar]
- Walker J. J. (2000). Pre-eclampsia. Lancet 356, 1260–1265. 10.1016/S0140-6736(15)00070-7 [DOI] [PubMed] [Google Scholar]
- Wallace R. G., Twomey L. C., Custaud M. A., Moyna N., Cummins P. M., Mangone M., et al. (2016). Potential diagnostic and prognostic biomarkers of epigenetic drift within the cardiovascular compartment. BioMed Res. Int. 2016, 1–11. 10.1155/2016/2465763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh N. P., Alba B. M., Bose B., Gross C. A., Sauer R. T. (2003). OMP peptide signals initiate the envelope-stress response by activating DegS protease via relief of inhibition mediated by its PDZ domain. Cell 113, 61–71. 10.1016/s0092-8674(03)00203-4 [DOI] [PubMed] [Google Scholar]
- Wan G., Xiang L., Sun X., Wang X., Li H., Ge W., et al. (2017). Elevated YKL-40 expression is associated with a poor prognosis in breast cancer patients. Oncotarget 8:5382. 10.18632/oncotarget.14280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang H., Peng R., Wang J., Qin Z., Xue L. (2018). Circulating microRNAs as potential cancer biomarkers: the advantage and disadvantage. Clin. Epigenet. 10:59. 10.1186/s13148-018-0492-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang S., Wang J., Zhang R., Wang T., Yan D., He Z., et al. (2018). Mendelian randomization analysis to assess a causal effect of haptoglobin on macroangiopathy in Chinese type 2 diabetes patients. Cardiovasc. Diabetol. 17:14. 10.1186/s12933-018-0662-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watkins R. A., Evans-Molina C., Terrell J. K., Day K. H., Guindon L., Restrepo I. A., et al. (2016). Proinsulin and heat shock protein 90 as biomarkers of beta-cell stress in the early period after onset of type 1 diabetes. Transl. Res. 168, 96–106. 10.1016/j.trsl.2015.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weigelt K., Bergink V., Burgerhout K. M., Pescatori M., Wijkhuijs A., Drexhage H. A. (2013). Down-regulation of inflammation-protective microRNAs 146a and 212 in monocytes of patients with postpartum psychosis. Brain Behav. Immun. 29, 147–155. 10.1016/j.bbi.2012.12.018 [DOI] [PubMed] [Google Scholar]
- Whongsiri P., Pimratana C., Wijitsettakul U., Jindatip D., Sanpavat A., Schulz W. A., et al. (2018). LINE-1 ORF1 protein is up-regulated by reactive oxygen species and associated with bladder urothelial carcinoma progression. Cancer Genomics Proteomics 15, 143–151. 10.21873/cgp.20072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wichmann S., Kirschbaum C., Lorenz T., Petrowski K. (2017). Effects of the cortisol stress response on the psychotherapy outcome of panic disorder patients. Psychoneuroendocrinology 77, 9–17. 10.1016/j.psyneuen.2016.11.030 [DOI] [PubMed] [Google Scholar]
- Winter P., Fuchs K., Walshe K., Colditz I. G. (2003). Serum amyloid A in the serum and milk of ewes with mastitis induced experimentally with Staphylococcus epidermidis. Vet. Rec. 152, 558–562. 10.1136/vr.152.18.558 [DOI] [PubMed] [Google Scholar]
- Wispriyono B., Kurniawan R., Novirsa R., Hartono B., Sari M. (2016). Pulmonary function and malondialdehyde (MDA) content in blood due to chromium exposure among tannery workers in Sukaregang, Garut. Res. J. Env. Toxicol. 10, 183–188. 10.3923/rjet.2016.183.188 [DOI] [Google Scholar]
- Wolk K., Kunz S., Witte E. (2004). IL-22 increases the innate immunity of tissues. Immunity 21, 241–254. 10.1016/j.immuni.2004.07.007 [DOI] [PubMed] [Google Scholar]
- Wong D. T. (2006). Salivary diagnostics powered by nanotechnologies, proteomics and genomics. J. Am. Dent. Assoc. 137, 313–321. 10.14219/jada.archive.2006.0180 [DOI] [PubMed] [Google Scholar]
- Wopereis S., Stroeve J. H. M., Stafleu A., Bakker G. C. M., Burggraaf J., van Erk M. J., et al. (2017). Multi-parameter comparison of a standardized mixed meal tolerance test in healthy and type 2 diabetic subjects: the PhenFlex challenge. Genes Nutr. 12:21. 10.1186/s12263-017-0570-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu L. L., Chiou C. C., Chang P. Y., Wu J. T. (2004). Urinary 8-OHdG: a marker of oxidative stress to DNA and a risk factor for cancer, atherosclerosis and diabetics. Clin. Chim. Acta 339, 1–9. 10.1016/j.cccn.2003.09.010 [DOI] [PubMed] [Google Scholar]
- Xie Y., Bowe B., Li T., Xian H., Yan Y., Al-Aly Z. (2018). Higher blood urea nitrogen is associated with increased risk of incident diabetes mellitus. Kidney Int. 93, 741–752. 10.1016/j.kint.2017.08.033 [DOI] [PubMed] [Google Scholar]
- Xu L., Liu X., Wu S., Gai L. (2018). The clinical application value of the plasma copeptin level in the assessment of heart failure with reduced left ventricular ejection fraction: a cross-sectional study. Medicine 97:e12610. 10.1097/MD.0000000000012610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu Y. Y., Ge J. F., Liang J., Cao Y., Shan F., Liu Y., et al. (2018). Nesfatin-1 and cortisol: potential novel diagnostic biomarkers in moderate and severe depressive disorder. Psycho. Res. Behav. Manag. 11, 495–502. 10.2147/PRBM.S183126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xue J., Nguyen D. T., Habtezion A. (2012). Aryl hydrocarbon receptor regulates pancreatic IL-22 production and protects mice from acute pancreatitis. Gastroenterology 143, 1670–1680. 10.1053/j.gastro.2012.08.051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xue X., Zhao Y., Wang X., Qin L., Hu R. (2019). Development and validation of serum exosomal microRNAs as diagnostic and prognostic biomarkers for hepatocellular carcinoma. J. Cell Biochem. 120, 135–142. 10.1002/jcb.27165 [DOI] [PubMed] [Google Scholar]
- Yamakoshi T., Park S. B., Jang W. C., Kim K., Yamakoshi Y., Hirose H. (2009). Relationship between salivary chromogranin-A and stress induced by simulated monotonous driving. Med. Biol. Engin. Comput. 47, 449–456. 10.1007/s11517-009-0447-y [DOI] [PubMed] [Google Scholar]
- Yan W., Qian L., Chen J., Chen W., Shen B. (2016). Comparison of prognostic microRNA biomarkers in blood and tissues for gastric cancer. J. Cancer 7, 95–106. 10.7150/jca.13340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang W., Han W., Gao H., Zhang L., Wang S., Xing L., et al. (2018). Self-powered implantable electronic-skin for in situ analysis of urea/uric-acid in body fluids and the potential applications in real-time kidney-disease diagnosis. Nanoscale 10, 2099–2107. 10.1039/c7nr08516h [DOI] [PubMed] [Google Scholar]
- Yang Y., Koh D., Ng V., Lee C. Y., Chan G., Dong F., et al. (2002). Self-perceived work related stress and the relation with salivary IgA and lysozyme among emergency department nurses. Occup. Environ. Med. 59, 836–841. 10.1136/oem.59.12.836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yatoo M. I., Deepa P. M., Mandal R. S. K., Sharma B., Mendiratta S. K., Patel B. H. M., et al. (2015). Prevalence of subclinical diabetes in a commercial flock of dairy goats in India and its interaction with milk quality. Small Rumin. Res. 132, 1–11. 10.1016/j.smallrumres.2015.09.012 [DOI] [Google Scholar]
- Yatoo M. I., Dimri U., Gopalakrishan A., Saminathan M., Dhama K., Mathesh K., et al. (2016). Antidiabetic and oxidative stress ameliorative potential of ethanolic extract of Pedicularis longiflora Rudolph. Inter. J. Pharmacol. 12, 1–11. 10.3923/ijp.2016.177.187 [DOI] [Google Scholar]
- Yatoo M. I., Dimri U., Gopalakrishnan A., Saxena A., Wani S. A., Dhama K. (2018). In vitro and in vivo immunomodulatory potential of Pedicularis longiflora and Allium carolinianum in alloxan-induced diabetes in rats. Biomed. Pharmacother. 97, 375–384. 10.1016/j.biopha.2017.10.133 [DOI] [PubMed] [Google Scholar]
- Yatoo M. I., Dimri U., Mashooq M., Saxena A., Gopalakrishnan A., Bashir S. T. (2019a). Redox disequilibrium vis-a-vis inflammatory cascade mediation of lymphocyte dysfunction, apoptosis, cytokine expression and activation of NF-kB in subclinical diabetic goats. Indian J. Anim. Sci. 89, 40–45. [Google Scholar]
- Yatoo M. I., Parray O. R., Mir M., Bhat R. A., Malik H. U., Fazili M. R., et al. (2019b). Comparative evaluation of different therapeutic protocols for contagious caprine pleuropneumonia in Himalayan Pashmina goats. Trop. Ani. Health Prod. 10.1007/s11250-019-01913-2. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- Ye X., Liu Y., Li F. (2017). Biomarkers of oxidative stress in the assessment of enantioselective toxicity of chiral pesticides. Curr. Protein Pept. Sci. 18, 33–40. 10.2174/1389203717666160413124654 [DOI] [PubMed] [Google Scholar]
- Yimcharoen M., Kittikunnathum S., Suknikorn C., Nak-On W., Yeethong P., Anthony T. G., et al. (2019). Effects of ascorbic acid supplementation on oxidative stress markers in healthy women following a single bout of exercise. J. Int. Soc. Sports Nutr. 16:2. 10.1186/s12970-019-0269-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yimer E. M., Zewdie K. A., Hishe H. Z. (2018). Netrin as a novel biomarker and its therapeutic implications in diabetes mellitus and diabetes-associated complications. J. Diabetes Res. 2018:8250521. 10.1155/2018/8250521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yonny M. E., García E. M., Lopez A., Arroquy J. I., Nazareno M. A. (2016). Measurement of malondialdehyde as oxidative stress biomarker in goat plasma by HPLC-DAD. Microchem. J. 129, 281–285. 10.1016/j.microc.2016.07.010 [DOI] [Google Scholar]
- Yoshida Y., Umeno A., Akazawa Y., Shichiri M., Murotomi K., Horie M. (2015). Chemistry of lipid peroxidation products and their use as biomarkers in early detection of diseases. J. Oleo. Sci. 64, 347–356. 10.5650/jos.ess14281 [DOI] [PubMed] [Google Scholar]
- Yoshikawa T., Naito Y. (2002). What is oxidative stress? JMAJ 45:271276. [Google Scholar]
- Yu D., Cai Y., Zhou W., Sheng J., Xu Z. (2018). The potential of angiogenin as a serum biomarker for diseases: systematic review and meta-analysis. Dis. Markers 2018:1984718. 10.1155/2018/1984718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan Y., Meeker J. D., Ferguson K. K. (2017). Serum polybrominated diphenyl ether (PBDE) concentrations in relation to biomarkers of oxidative stress and inflammation: the National Health and Nutrition Examination Survey 2003–2004. Sci. Total Environ. 575, 400–405. 10.1016/j.scitotenv.2016.10.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeng R., Bequette B. J., Vinyard B. T., Bannerman D. D. (2009). Determination of milk and blood concentrations of lipopolysaccharide-binding protein in cows with naturally acquired subclinical and clinical mastitis. J. Dairy Sci. 92, 980–989. 10.3168/jds.2008-1636 [DOI] [PubMed] [Google Scholar]
- Zhang C., Huang Y., Long J., Yao X., Wang J., Zang S., et al. (2019). Serum chromogranin A for the diagnosis of gastroenteropancreatic neuroendocrine neoplasms and its association with tumour expression. Oncol. Lett. 17, 1497–1504. 10.3892/ol.2018.9795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang G., Liu J., Wu L., Fan Y., Sun L., Qian F., et al. (2018). Elevated expression of serum amyloid a 3 protects colon epithelium against acute injury through TLR2-dependent induction of neutrophil IL-22 expression in a mouse model of colitis. Front. Immunol. 9:1503. 10.3389/fimmu.2018.01503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang K., Zhao Z., Lan L., Wei X., Wang L., Liu X., et al. (2017). Sigma-1 receptor plays a negative modulation on N-type calcium channel. Front. Pharmacol. 8:302. 10.3389/fphar.2017.00302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang L., Masetti G., Colucci G., Salvi M., Covelli D., Eckstein A., et al. (2018). Combining micro-RNA and protein sequencing to detect robust biomarkers for Graves'disease and orbitopathy. Sci. Rep. 8:8386 10.1038/s41598-018-26700-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang R., Brennan M. L., Fu X., Aviles R. J., Pearce G. L., Penn M. S., et al. (2001). Association between myeloperoxidase levels and risk of coronary artery disease. JAMA 286:21362142. 10.1001/jama.286.17.2136 [DOI] [PubMed] [Google Scholar]
- Zhang X. G., Zhang Y. Q., Cheng Q. P., Cao Y., Sun J. M., et al. (2018). The impact of insulin pump therapy to oxidative stress in patients with diabetic nephropathy. Eur. J. Med. Res. 23:7. 10.1186/s40001-018-0304-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y., Catts V. S., Shannon Weickert C. (2017). Lower antioxidant capacity in the prefrontal cortex of individuals with schizophrenia. Aust. N. Z. J. Psychiatry 52, 690–698. 10.1177/0004867417728805 [DOI] [PubMed] [Google Scholar]
- Zhang Y. X., Li J. F., Yang Y. H., Huang K., Miao R., Zhai Z. G., et al. (2018). Identification of haptoglobin as a potential diagnostic biomarker of acute pulmonary embolism. Blood Coagul. Fibrinol. 29, 275–281. 10.1097/MBC.0000000000000715 [DOI] [PubMed] [Google Scholar]
- Zhang Z., Li S., Fang H. (2017). Enzymatic antioxidants status in patients with recurrent aphthous stomatitis. J. Oral Pathol. Med. 46, 817–820. 10.1111/jop.12547 [DOI] [PubMed] [Google Scholar]
- Zhao P., Guo Y., Zhang W., Chai H., Xing H., Xing M. (2017). Neurotoxicity induced by arsenic in Gallus gallus: regulation of oxidative stress and heat shock protein response. Chemosphere 166, 238–245. 10.1016/j.chemosphere.2016.09.060 [DOI] [PubMed] [Google Scholar]
- Zhou H., Cheruvanky A., Hu X., Matsumoto T., Hiramatsu N., Cho M. E., et al. (2008). Urinary exosomal transcription factors, a new class of biomarkers for renal disease. Kidney Int. 74, 613–621. 10.1038/ki.2008.206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou H., Kajiyama H., Tsuji T., Hu X., Leelahavanichkul A., Vento S., et al. (2013). Urinary exosomal Wilms' tumor-1 as a potential biomarker for podocyte injury. Am. J. Physiol. Renal Physiol. 305, F553–F559. 10.1152/ajprenal.00056.2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou Q., Liu J., Quan J., Liu W., Tan H., Li W. (2018). MicroRNAs as potential biomarkers for the diagnosis of glioma: A systematic review and meta-analysis. Cancer Sci. 109, 2651–2659. 10.1111/cas.13714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou S. S., Jin J. P., Wang J. Q., Zhang Z. G., Freedman J. H., Zheng Y., et al. (2018). miRNAs in cardiovascular diseases: potential biomarkers, therapeutic targets and challenges. Acta Pharmacol. Sin. 39, 1073–1084. 10.1038/aps.2018.30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Z. W., Friess H., Wang L., Zimmermann A., Büchler M. W. (2001). Brain-derived neurotrophic factor (BDNF) is upregulated and associated with pain in chronic pancreatitis. Dig. Dis. Sci. 46, 1633–1639. 10.1023/A:101068491 [DOI] [PubMed] [Google Scholar]
- Ziech D., Franco R., Georgakilas A. G., Georgakila S., Malamou-Mitsi V., Schoneveld O., et al. (2010). The role of reactive oxygen species and oxidative stress in environmental carcinogenesis and biomarker development. Chem. Biol. Interact. 188, 334–339. 10.1016/j.cbi.2010.07.010 [DOI] [PubMed] [Google Scholar]
- Zininga T., Ramatsui L., Shonhai A. (2018). Heat shock proteins as immunomodulants. Molecules 23:2846. 10.3390/molecules23112846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zitka O., Skalickova S., Gumulec J., Masarik M., Adam V., Hubalek J., et al. (2012). Redox status expressed as GSH:GSSG ratio as a marker for oxidative stress in paediatric tumour patients. Oncol. Lett. 4, 1247–1253. 10.3892/ol.2012.931 [DOI] [PMC free article] [PubMed] [Google Scholar]