Abstract
Stem cells have the capacity of self-renewal and, through proliferation and differentiation, are responsible for the embryonic development, postnatal development, and the regeneration of tissues in the adult organism. Cancer stem cells, analogous to the physiological stem cells, have the capacity of self-renewal and may account for growth and recurrence of tumors. Development and regeneration of healthy tissues and tumors depend on the balance of different genomic and nongenomic signaling pathways that regulate stem cell quiescence, proliferation, and differentiation. During evolution, this balance became dependent on all-trans retinoic acid (RA), a molecule derived from the environmental factor vitamin A. Here we summarize some recent findings on the prominent role of RA on the proliferation of stem and progenitor cells, in addition to its well-known function as an inductor of cell differentiation. A better understanding of the regulatory mechanisms of stemness and cell differentiation by RA may improve the therapeutic options of this molecule in regenerative medicine and cancer.
Keywords: All-trans retinoic acid (ATRA), stemness, differentiation, regenerative medicine, cancer
1. Introduction
Retinoic acid (RA) regulates a wide range of biological processes during development and in adult organisms [1,2,3,4,5,6,7,8,9]. Retinoic acid signaling is dependent on cells that can metabolize vitamin A (retinol) to RA. Retinol dehydrogenases oxidize retinol to retinal, and aldehyde dehydrogenases (ALDH1A1, ALDH1A2, and ALDH1A3) oxidize retinal to RA [2,10]. Retinoic acid released from these cells generates gradients that regulate neighboring cells. The precise RA level depends on the availability of vitamin A (retinol), the activity of enzymes involved in RA biosynthesis (retinol dehydrogenases and aldehyde dehydrogenases), and the RA catabolism by CYP26 enzymes [11,12,13].
Retinoic acid regulates transcription by interacting with heterodimers of nuclear RA receptors (RARα, RARβ, and RARγ) and retinoid X receptors (RXRα, RXRβ, and RXRγ) bound to RA response elements (RAREs) in the promoters of target genes [4,14,15]. The expression of over 500 genes is upregulated or downregulated by RA [16]. Moreover, RA controls other transcriptional signaling pathways via different nuclear receptors, such as the peroxisome proliferator-activated receptor β/δ [17,18], and can also regulate different protein kinases in a nontranscriptional fashion [19,20,21].
Although RA has been widely described as an inductor of cell differentiation, depending on cell-type, RA can antagonize cell differentiation and promote stemness (Table 1).
Table 1.
Induction of stemness or cell differentiation by retinoic acid (RA) in a cell-type-dependent manner.
| Cell Type | Action | Signaling Pathway | RA Dose-Time | References |
|---|---|---|---|---|
| Pluripotent stem cells | Stemness | Inhibition of Wnt. Activation of Akt-mTOR | 0.5 µM (24 h) | [22] |
| Breast cancer cells T47D403 | Stemness | Lack of expression of RARα tumor suppressor genes and activation of RARα-PI3K-AKT | 1 µM (72 h) | [23] |
| Breast cancer cells MDA-MB-231 | Stemness | Upregulation of 1286 genes, among them MUC4. Activation of the axis Src-YAP-IL6 |
0.1 µM (18 h) 5 µM (48 h) |
[24] [25] |
| Breast cancer cells MDA-MB-468 | Differentiation | Upregulation of 1358 genes, among them HOXA1 Inhibition of the axis Src-YAP-IL6 |
0.1 µM (18 h) 5 µM (48 h) |
[24] [25] |
| Breast cancer cells MCF-7 | Stemness | Activation of ALDH1A1-HIF1α-VEGF | 1 µM (48 h) | [26] |
| Mammary MCF12A cells and T47D breast cancer cells | Differentiation |
RARβ/TET2-miR200c-Suppression of PKCζ |
1 µM (24 h) | [27] |
| Adult hippocampus | Stemness | Activation of HIF1α-VEGF | 1 µM (24 h) | [28] |
| Glioblastoma T1440, T1452 and T1464 | Stemness | Increased SOX2 expression | 1 µM (7d) | [29] |
| Glioblastoma T1338 | Differentiation | Decreased SOX2 expression | 1 µM (7d) | [29] |
| Dormant hematopoietic cells | Stemness | Attenuation of C-MYC expression | 5 µM (24–48 h) | [30] |
| Hematopoietic stem cells | Differentiation or stemness | Differentiation through RARα Stemness through RARγ NOTCH1 expression | 1 µM (14d) | [31] |
| Colorectal cancer cells | Differentiation | RARγ-inhibition of YAP-increased E-cadherin expression | 1 µM (30 min) | [32] |
| Hepatocelular carcinoma cells | Stemness | RARγ-PI3K-AKT-NFκB | 1 µM (48 h) | [33] |
| Pancreatic ductal adenocarcinoma | Differentiation | Decrease ALDH1, SOX2 and NANOG | 10 μM (48 h) | [34] |
| Spermatogonial stem cells | Differentiation |
Upregulation of STRA8, AGPAT3, FAM57A, WDR91 | 0.1 μM (24 h) | [35] |
| Regeneration of keratinocytes | Stemness | TLR3-STAT3 and NFkB-ALDH1-RA-RAR | 0.1µM (48 h) | [36] |
2. Retinoic Acid Induces Stemness or Differentiation in the Mammary Gland and Breast Cancer Cells
Unlike other organs, the mammary gland tissue undergoes development postnatally. An adequate balance between stem self-renewal and stem cell differentiation is essential for this process. Prodifferentiation and antidifferentiation effects of RA have been reported during mammary gland development and breast cancer [23,24,37].
2.1. Growth-Promoting and Growth-Inhibiting Actions of RA in Breast Cancer Depend on the Cell Context-Specific Balance of Activation of Transcriptional and Nontranscriptional Pathways
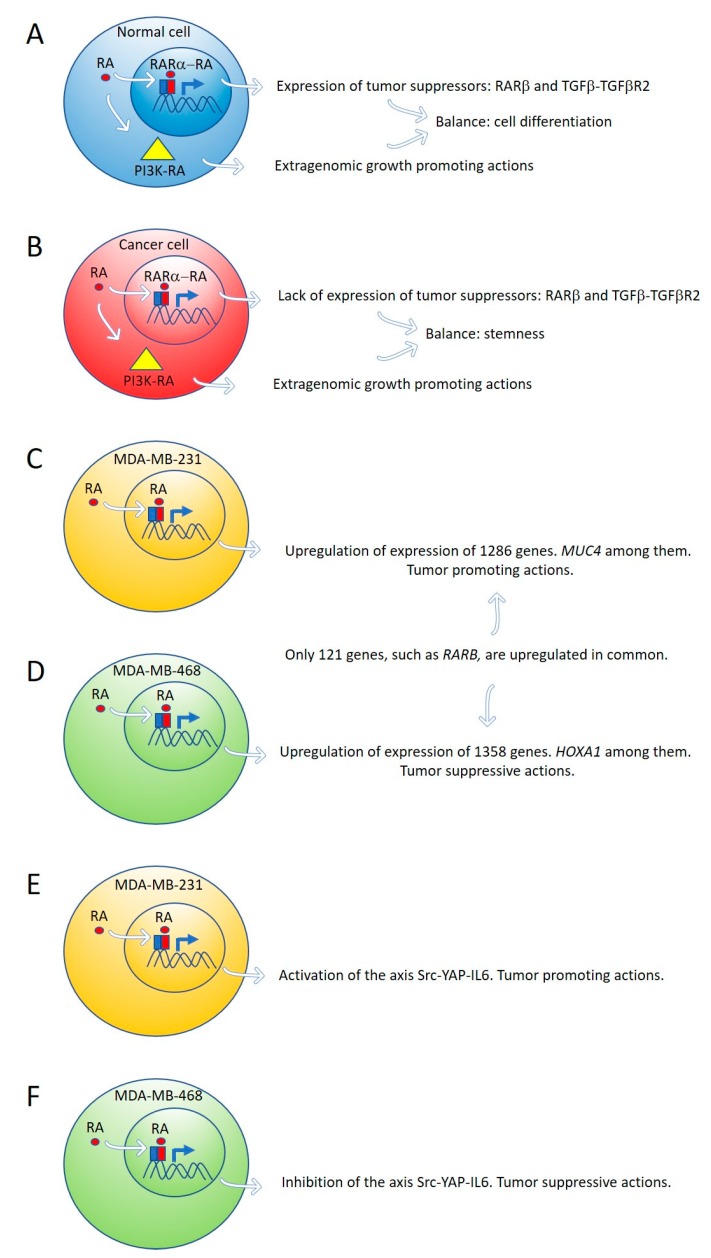
By global gene expression microarray analysis, Rossetti et al. [23] determined that in breast cancer cells (T47DCtrl) grown under “physiological” RA culture conditions, many RARα-target genes, coding for tumor suppressor signaling pathways, as RARβ and the TGFβ-TGFβR2, are in a repressed transcriptional state marked by epigenetic histone modifications. In this situation, lack of expression of tumor suppressor genes cannot counteract the growth-promoting activity of nontranscriptional signaling pathways such as PI3K-AKT, triggered by direct interaction of RARα and the catalytic subunit of PI3K [23]. The degree of inhibition of RARα transcriptional function is variable in different breast cancer cell lines: mild in T47DCtrl, severe in T47DG303E, and extremely severe in T47D403. Both in vitro and in vivo treatment with supraphysiological doses of exogenous RA significantly promoted T47D403 breast cancer cell invasion [23] (Figure 1A,B).
Figure 1.
Expression of tumor suppressor genes by retinoic acid (RA) in healthy cells counteracts the growth-promoting activity of nontranscriptional RA signaling pathways, such as PI3K-AKT (A). In cancer cells, lack of expression of tumor suppressor genes by RA cannot counteract the extragenomic tumor-promoting actions of RA (B). Differential gene expression induced by ALDH1A3 or RA in MDA-MB-231 and MDA-MB-468 cells (C,D). Retinoic acid upregulates the signaling pathway Src-YAP-IL6 involved in stemness in triple-negative MDA-MB-231 breast cancer cells (E) and downregulates the same pathway in triple-negative MDA-MB-468 breast cancer cells (F).
2.2. Retinoic Acid Induces Tumor-Promoting or Tumor-Suppressive Actions in Triple-Negative Breast Cancer Cells Due to Variable Gene Expression in Cell Lines with Differences in DNA Methylation
Marcato et al. [24] reported that the effects of RA and ALDH1A3 activity were tumor-promoting in MDA-MB-231 and MDA-MB-435 triple-negative breast cancer cells, but tumor-suppressive in triple-negative MDA-MB-468 breast cancer cells. The opposing tumor growth effects of ALDH1A3/RA in breast cancer cells depend upon differential gene expression induced by ALDH1A3 or RA in MDA-MB-231 and MDA-MB-468 cells. Increased ALDH1A3 expression upregulated 1286 and 1358 genes in MDA-MB-231 and MDA-MB-468 cells, respectively. A large divergence in gene expression changes induced by ALDH1A3 in the two cell lines was observed because only 121 genes were upregulated in common in both cell lines. RARβ is one of these genes (Figure 1C,D).
One of the ALDH1A3-induced genes in MDA-MB-468 cells is the homeobox transcription factor A1 (HOXA1). The promotor of HOXA1 possesses a RARE sequence that was previously shown to be inducible by RA [38]. HOXA1 expression is significantly reduced by ALDH1A3 knockdown and induced by RA in MDA-MB-468 cells but is undetectable in MDA-MB-231 cells [24]. HOXA1 is hypermethylated in MDA-MB-231 cells and hypomethylated in MDA-MB-468 cells [24]. HOXA1 is often hypermethylated in cancer, suggesting a tumor-suppressive function [39,40].
Mucin 4 (MUC4), a potential oncogene with a RARE, inducible by RA, and associated with triple-negative breast cancer [41,42], is significantly induced by ALDH1A3 and RA in MDA-MB-231 cells, but not in MDA-MB-468 cells. MUC4 is hypermethylated in MDA-MB-468 and hypomethylated in MDA-MB-231 [24]. MUC4 is typically hypomethylated in cancers, and its expression is associated with more aggressive cancer [41,42,43,44,45]. MUC4 knockdown in MDA-MB-231 cells reduced their tumorigenic and metastatic properties [42], suggesting MUC4 may represent a gene that contributes to ALDH1A3/RA-mediated tumor growth and metastasis of MDA-MB-231 cells [24].
2.3. Retinoic Acid Upregulates the Signaling Pathway Src-YAP-IL6 Involved in Stemness in Triple-Negative MDA-MB-231 Breast Cancer Cells and Downregulates the Same Pathway in Triple-Negative MDA-MB-468 Breast Cancer Cell Line
Retinoic acid induces tumor suppression in tumor xenografts of MDA-MB-468 breast cancer cells while increasing tumor growth and metastasis in xenografts of MDA-MB-231 [24]. We have used these triple-negative breast cancer cell lines as a research model to investigate the role of RA on the regulation of the signaling pathway Src-YAP-Interleukin 6 involved in stemness [25]. We found that RA activates this pro-invasive axis in triple-negative MDA-MB-231 breast cancer cells, yielding to an increased invasion of these cells. On the contrary, RA inhibits the Src-YAP-IL6 axis of triple-negative MDA-MB-468 cells, which results in decreased invasion phenotype (Figure 1E,F). In both types of cells, inhibition of the Src-YAP-IL6 axis by the Src inhibitor PP2 drastically reduces migration and invasion. The Src-YAP-IL6 axis controls invasion, metastasis, resistance to therapy, and stemness of MDA-MB-231 breast cancer cells [46,47]. IL-6 is the first universal transcriptional target of YAP involved in promoting stemness conserved from flies to humans [46,48].
Overexpression of IL-6 induces cancer cell proliferation, angiogenesis, and metastasis through stimulating STAT3, MAPK, and Akt signaling pathways [49]. IL-6 regulates cancer stem cell, mesenchymal stem cell formation, and epithelial to mesenchymal transition in cancer, and is a contributing factor for chemoresistance [49]. Sansone et al. [50] found that IL-6 mRNA was robustly elevated in mammospheres compared with breast epithelium and was required for their self-renewal and aggressive potential. Autocrine IL6-STAT3 signaling increases stem cell properties with efficient tumor colonization and outgrowth in vivo. Conversely, blockage of IL-6 reduces tumor burden and metastasis [51,52,53,54].
Nuclear YAP phosphorylation in MDA-MB-231 breast cancer cells depends on Src activity. Until recently, activation of YAP was believed to solely depend on the inhibition of the Hippo signaling pathway that retains YAP in the cytoplasm [55]. To assess if YAP activation in MDA-MB-231 breast cancer cells depends on Src activity, as observed in other cancer cells [56,57,58], we used Src inhibition by PP2, Src interference by siRNA and transfection of Src into MDA-MB-231 breast cancer cells. Src inhibition by PP2 and Src interference decreased YAP activity and downregulated IL-6 expression, while Src transfection activated YAP and upregulated IL-6 [25].
The mechanism of Src activation induced by RA is not known at present. Mechanisms independent of transcription have been reported in breast cancer cells [23]. However, the activation of the Src-YAP-IL6 axis we have observed should be the consequence of a genomic action of RA, given the 48 h delay following incubation with supraphysiological concentrations of RA (5 μM). Extragenomic effects of RA in breast cancer cells are produced faster and with lower levels of RA [23].
Overexpression of MUC4 in triple-negative breast cancer cells induced by RA [24] is an attractive candidate for Src activation because cell knockdown of MUC4 in pancreatic carcinoma decreased Src tyrosine phosphorylation significantly [59]. IL-6 induces MUC4 expression through the gp130-STAT3 pathway in gastric cancer cell lines [60].
An association of YAP activity and RA signaling with an increase in migration also has been observed in human neural crest cells [61]. YAP, as well as its paralog TAZ, is known to act as a stemness-promoting factor in several tissue types, including hepatic, intestinal, and skin stem cell niches [62,63,64,65].
It has been reported that MDA-MB-231 and MDA-MB-468 are non-sphere-forming cells lines [66]. However, it is not known how the presence of RA could affect mammosphere formation of these cell lines [24] and whether these in vitro assays may reflect the expansion of breast cancer stem and nonstem cells in vivo. Using tumor xenografts, RA increases tumor growth and metastasis of MDA-MB-231 and decreases tumor growth of MDA-MB-468 cells [24].
2.4. Retinoic Acid Conferred Stemness Properties to Breast Cancer MCF-7 Cells
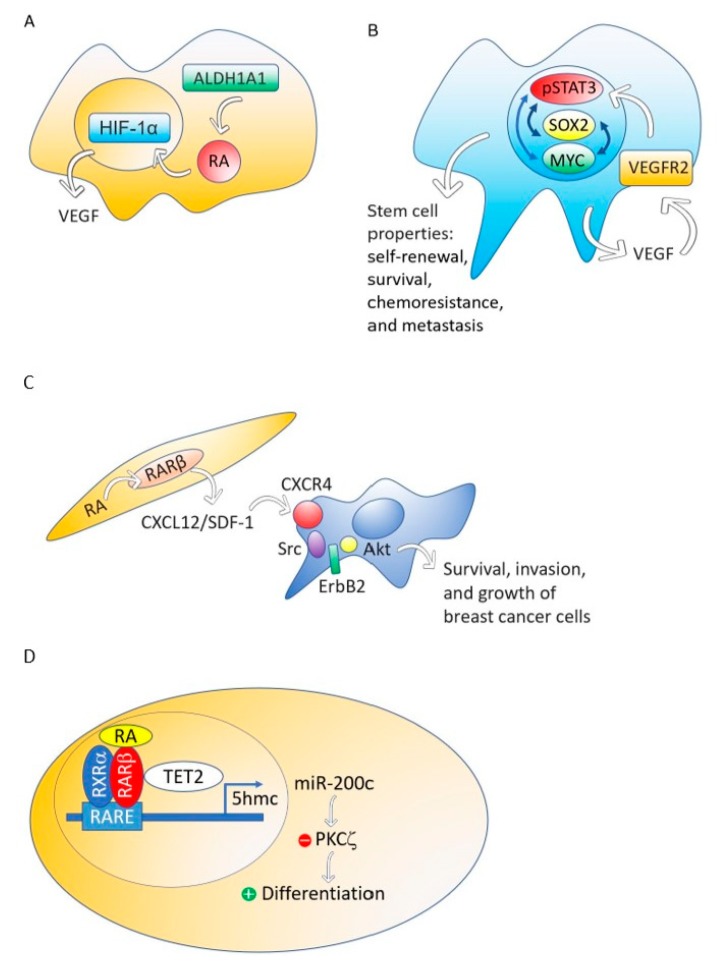
Although different breast cancer cell lines such as 184A1, SUM149, SUM159, and HCC1954 treated with RA presented a decrease in mammosphere formation [67], the breast cancer MCF-7 cell line responds to RA with an increase of stemness through an ALDH1A1-retinoic acid-HIF-1α-VEGF pathway [26] (Figure 2A). It has been reported that VEGF drives breast and lung cancer-initiating stem cells through the VEGFR-2-STATt3 signaling pathway that upregulates MYC and SOX2 [68,69] (Figure 2B). VEGF contributes to the acquisition of stem cell properties, including self-renewal, survival, and chemoresistance through VEGFR2 receptors, VEGF neuropilin receptors [70,71] and intracrine VEGF receptors [72,73].
Figure 2.
The ALDH1A1-retinoic acid-HIF-1α-VEGF pathway is activated in breast cancer MCF-7 cells (A). VEGF drives breast and lung cancer-initiating stem cells through the VEGFR-2-STAT3 signaling pathway that upregulates MYC and SOX2 gene expression (B). RA, through RARβ, increases the production of CXCL12/SDF-1 in stroma cells and, consequently, activates the Src-ErbB2-Akt signaling pathway in breast cancer cells, promoting survival, cell growth, and invasion (C). When the nontumorigenic, immortalized mammary epithelial cell line, MCF12A and the non-invasive breast cancer cell line T47D were treated with RA, the RA nuclear receptor RARβ associated with a methylcytosine dioxygenase (TET2) that produces DNA demethylation. The consequence is the induction of genes involved in cell differentiation and the activation of miR-200c expression. MiR-200c downregulates stemness targeting the protein kinase PKCζ. RA does not perform these actions in aggressive breast cancers (D).
2.5. RARβ Expression in the Mammary Gland Stroma Shapes the Tumor Microenvironment Favoring Breast Tumor Growth and Invasion
Although RARβ possesses, in breast cancer cells, many of the functional characteristics of a tumor suppressor, RARβ in the tumor stroma has a dominant role in promoting the growth and progression of mammary epithelial tumors [74]. The mechanism through which stromal RARβ achieves its tumor-promoting effect probably involves the production of CXCL12/SDF-1 in stroma cells and the consequent activation of the Src-ErbB2-Akt signaling pathway in the breast cancer cells (Figure 2C).
2.6. Retinoic Acid Induces Cell Differentiation and Downregulates Stemness in a Nontumorigenic Immortalized Mammary Epithelial Cell Line and a Non-Invasive Breast Cancer Cell line but Does Not Perform These Actions in Aggressive Breast Cancers
Using MCF12A, a nontumorigenic immortalized mammary epithelial cell line, or T47D, a non-invasive breast cancer cell line, RA induces genes involved in cell differentiation such as RUNX1, BMP6, IKZF1 and CAV1, and activates the expression of noncoding RNAs that downregulate stemness, such as miR-200c [27]. This miRNA targets and suppresses the protein kinase PKCζ, a protein that has a pivotal role in directing the asymmetric division of mammalian stem cells to sustain the stem cell pool [75,76,77]. PKCζ overexpression promotes breast cancer invasiveness and metastasis [78]. However, the triple-negative breast cancer cell line MDA-MB-231 does not respond with cell differentiation and downregulation of stemness to RA treatment [27].
Retinoic acid treatment of the nontumorigenic, immortalized mammary epithelial cell line, MCF12A and the non-invasive breast cancer cell line T47D induces the association of the RA nuclear receptor RARβ with a methylcytosine dioxygenase (TET2) [27]. The TET protein family has a crucial role in DNA demethylation by catalyzing the conversion of the modified genomic base 5-methylcytosine into 5-hydroxymethylcytosine (5hmC), thereby activating the target gene expression [79]. Expression of TET2 occurs in the nontumorigenic mammary epithelial cell line MCF12A and also in the non-invasive breast cancer cell line T47D, but repression occurs in aggressive breast cancers [27] (Figure 2D).
Retinoic acid enhanced the nuclear localization of RARβ and TET2, whereas knockdown of RARβ blocked RA mediated TET2 nuclear localization and substantially increased TET2 in the cytoplasm fraction. In contrast to nontumorigenic MCF12A and non-invasive breast cancer cell line T47D, TET2 was predominantly localized in the cytoplasm in aggressive triple-negative breast cancer cell line MDA-MB-231, which is deficient in endogenous RARβ expression. Re-expression of RARβ in MDA-MB-231 cells relocalized TET2 to the nucleus, and the nuclear TET2 level was further enhanced by RA treatment [27].
2.7. Retinoic Acid Blocks the Progesterone Induction of Cytokeratin-5 Expressing Breast Cancer Stem Cells
Half of estrogen receptor-positive breast cancers contain a subpopulation of cytokeratin-5 expressing cells that are therapy-resistant and exhibit increased cancer stem cell properties induced by progesterone. Retinoic acid, through RARα or RARγ, blocks progesterone induction of cytokeratin-5 expression and stemness [80].
3. Janus Faces of RA in Other Tissues
Promotion of either stemness or cell differentiation by the RA signaling pathway also has been observed in pluripotent stem cells, the neural system, the hematopoietic system, colorectal cancer, hepatocellular carcinoma, pancreatic cancer, ovarian cancer, spermatogenesis, and regeneration of tissues, among others.
3.1. Retinoic Acid Sustains Pluripotency and Suppresses Differentiation of Human Induced Pluripotent Stem Cells
Short-time treatment (24 h) with 0.5 μM RA antagonizes cell differentiation sustaining and improving pluripotency. In these conditions, RA inhibits the Wnt canonical pathway and positively modulates the Akt-mTOR signaling pathway.
3.2. Retinoic Acid Induces Stemness or Differentiation in the Neural System
Although RA facilitates differentiation of neurons at the expense of proliferation during neurogenesis [81,82], recent studies have revealed that RA induces proliferation in early neurogenesis in the developing mouse cerebral cortex [83], in the adult hippocampus [28], and also in stem-like glioma cells [29].
3.2.1. Retinoic Acid Induces Proliferation in Cerebral Cortex Early Neurogenesis
Cerebral cortex early neurogenesis is achieved by a proper balance between proliferation and differentiation of progenitor cells. The first progenitors formed in the cortical plate are radial glial cells which generate neurons either directly, or through an indirect mechanism involving the production of intermediate neuronal progenitors, which then give rise to neurons. In the absence of RA, the radial glial cells proliferate less and prematurely produce neurons, leading to their depletion. Furthermore, the lack of RA impairs the generation of intermediate neuronal progenitors, producing a deficit in projection neurons and microcephaly [83].
3.2.2. Retinoic Acid Induces Proliferation in Adult Neurogenesis in the Hippocampus
Neural stem and progenitor cells located in the hippocampus drive adult neurogenesis. The proliferation of these cells is essential to maintain stem cell populations and produce new neurons. A significant departure from the dogma that RA acts mainly to promote neuronal differentiation has been the finding that RA signaling increases proliferation of neural stem and progenitor cells in the adult rodent hippocampus. An increase of expression of the hypoxia-inducible factor-1α (HIF1α) and its transcriptional target vascular endothelial growth factor-A (VEGFA) mediate the proliferative effect of RA [28]. This observation broadens RA’s function beyond its well-described role in neuronal differentiation.
3.2.3. Retinoic Acid Induces Stemness Rather Than Differentiation in Stem-Like Glioma Cells
In cells that display stem-like properties isolated and expanded from different gliomas, RA exerted, in general, a proproliferative and prosurvival effect mediated by RARα and RARγ [29]. Only one glioblastoma multiforme derived cell line (T1338), and a subpopulation of another (T1389), displayed neural differentiation in response to RA [29]. Since SOX2 is a master regulator of stemness in stem-like glioma cells, the effect of RA on SOX2 expression has been determined. Treatment with 1 μM RA almost abrogated SOX2 expression in T1338, where RA displayed neural differentiation, but increased SOX2 levels in T1440, T1452, and T1464, where RA exerted a proproliferative and prosurvival effect [29].
3.3. Retinoic Acid Induces Stemness or Differentiation in the Hematopoietic System
3.3.1. Retinoic Acid Prevents Differentiation of Dormant Primitive Hematopoietic Stem Cells and Induces Differentiation of More Mature Blood Cells
In the hematopoietic system, RA prevents differentiation of primitive stem cells into a more mature population [84], and the opposite occurs in more differentiated blood cells and certain leukemias, in which RA displays prodifferentiation effects [85,86]. Hematopoietic stem cells are unique in their capacity to self-renew and replenish the entire blood system upon transplantation. Hematopoietic stem cells give rise to a pool of multipotent progenitors, which generate lineage-restricted progenitors, and finally, mature effector cells. A subpopulation of hematopoietic stem cells called dormant stem cells is characterized by an extremely low in vivo proliferation history with only approximately five cell divisions per lifetime in a healthy mouse [30]. These cells represent a small fraction of the hematopoietic cells in the murine bone marrow but harbor the highest long-term reconstitution potential and are reversibly activated in response to stress signals. High expression of a RA program is characteristic of dormant hematopoietic stem cells. Treatment with RA significantly attenuates the c-Myc upregulation and antagonizes stress-induced activation of these cells [30].
3.3.2. Variable Effects of RA on Tumor Immunosuppression
Immature myeloid cells play an essential role in tumor-induced immunosuppression. These cells accumulate in large numbers in tumor-bearing hosts and directly inhibit T-cell functions. In vivo administration of RA dramatically reduced the presence of immature myeloid cells in all tested tumor models, inducing their differentiation into mature dendritic cells, macrophages, and granulocytes [87]. However, aldehyde dehydrogenase expression and the subsequent production of retinoic acid by dendritic cells, macrophages, eosinophils, and epithelial cells, seems essential in regulatory T cell induction. Regulatory T cells promote immune tolerance to tumor cells in multiple types of cancer [88].
3.4. RARγ Inhibits Colorectal Cancer Tumorigenesis and Metastasis, Restricting the YAP Signaling Pathway
We have observed that RA activates the YAP signaling pathway in triple-negative MDA-MB-231 breast cancer cells, but inhibits this pathway in triple-negative MDA-MB-468 breast cancer cells [25]. In vitro and in vivo studies showed that silencing RARγ expression enhanced colorectal cancer cell growth significantly, with increased migration, invasion, and metastasis, whereas ectopic expression of RARγ did the opposite, suggesting that RARγ functions as a tumor suppressor in colorectal cancer [32]. RARγ interacts with YAP in the cytoplasm of colon cancer cells and the interaction between RARγ and YAP could be significantly enhanced after RA treatment. RARγ promotes the binding of the Lats1 kinase to YAP and its phosphorylation. Phosphorylated YAP is retained in the cytoplasm, and the YAP-TEAD transcriptional activity is inhibited. YAP acts as an oncogenic regulator for cancer development. Increased expression and activity of YAP is associated with the growth, metastatic potential, and poor prognosis of several cancer types, including liver cancer and colorectal cancer [89,90,91].
3.5. Cytoplasmic Accumulation of RARγ in Hepatocellular Carcinoma Cells Plays an Oncogenic Role Via Nongenomic Activation of Akt-NFκB Signaling
Levels of RARγ were significantly elevated in tumor tissues from a majority of human hepatocellular carcinoma and in hepatocarcinoma cell lines. Overexpression of RARγ promoted colony formation by hepatocarcinoma cells in vitro and the growth of hepatocarcinoma xenografts in animals [33]. In HepG2 cells, transfection of RARγ enhanced, whereas downregulation of RARγ expression by siRNA impaired, the effect of RA on inducing hepatocarcinogenesis. RARγ interacts with the p85α regulatory subunit of phosphatidylinositol 3-kinase (PI3K). The interaction between RARγ and p85α resulted in activation of Akt and NF-κB, critical regulators of the growth and survival of cancer cells [33].
3.6. Retinoic Acid Induces Cell Differentiation and Reduces Stem Cell Markers in Pancreatic Cancer Cells
Both RA and vitamin A concentrations are reduced in pancreatic ductal adenocarcinoma tissue compared to their normal counterparts, and the expression of RAR α and β, as well as RXR α and β, are down-regulated [92]. This reduced expression of retinoid receptors correlates with a reduction of the expression of some markers of differentiation such as carbonic anhydrase II and downregulation of E-cadherin expression involved in epithelial-to-mesenchymal transition [92].
Herreros-Villanueva et al. [93] using several pancreatic cancer cell lines, reported that RA treatment reduced the sphere-forming capacity as well as the size of spheres formed and the expression of pancreatic stem cell markers CD24, CD44, CD133, and aldehyde dehydrogenase 1. Essential stemness genes, such as SOX2 decreased. Surprisingly, however, the expression of the proto-oncogene c-Met was significantly increased in all the pancreatic cancer cell lines studied.
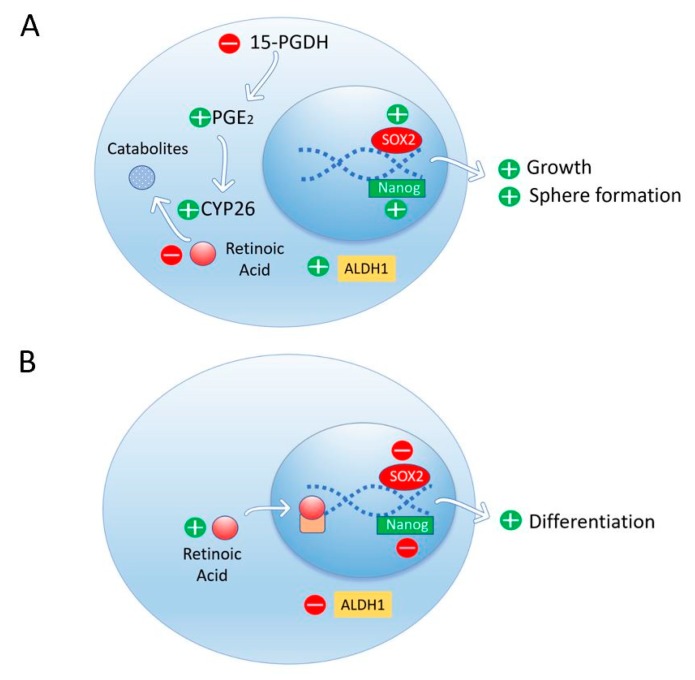
The accumulation of prostaglandin E2 (PGE2) by inhibition of the degradation enzyme 15-hydroxyprostaglandin dehydrogenase (15-PGDH) induces progression of pancreatic ductal adenocarcinoma (PDAC) [34]. Genetic deletion of 15-PGDH showed PGE2 accumulation, enhanced CYP26A1 expression, and in consequence, RA depletion in the pancreas. RA depletion results in PDAC with high levels of Aldh1, Sox2, and Nanog in tumor cells, with growth and sphere formation. RA replacement suppresses Aldh1 signaling in tumor cells and tumor progression in pancreatic adenocarcinoma (Figure 3).
Figure 3.
Depletion of RA by an increase of CYP26 expression due to an accumulation of prostaglandin E2 (PGE2) results in high levels of ALDH1, Sox2, and Nanog in tumor cells with growth and sphere formation (A). Retinoic acid replacement suppresses ALDH1 signaling in pancreatic ductal adenocarcinoma and induces cell differentiation (B).
3.7. Retinoic Acid Downregulates ALDH1-Mediated Stemness and Inhibits Tumor Formation in Ovarian Cancer Cells
ALDH1 activity is positively correlated with stemness in ovarian cancer cells according to measures such as sphere formation and stem cell marker expression, as well as tumorigenesis in a mouse xenograft model. Retinoic acid reduced ALDH1 expression, suppressed tumor formation, and inhibited sphere formation, cell migration, and invasion in ALDH1-abundant ovarian cancer cells [94].
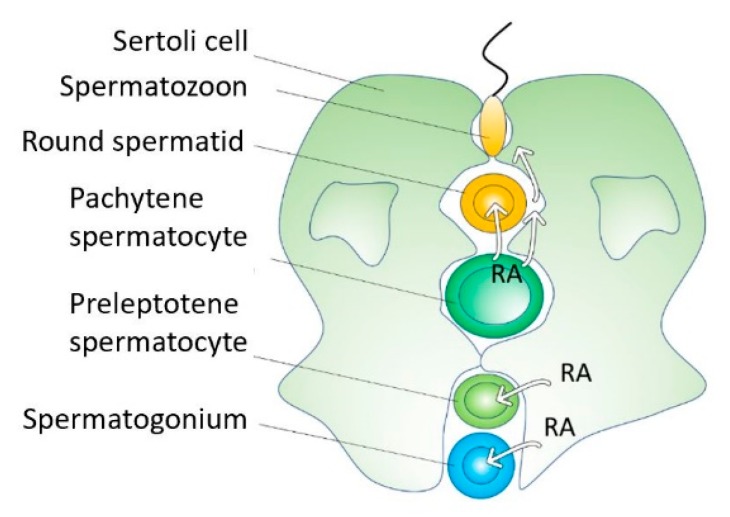
3.8. Retinoic Acid Induces Cell Differentiation and Proliferation During Spermatogenesis
Cell differentiation during spermatogenesis involves four transitions: spermatogonial differentiation, meiotic initiation, spermatid elongation, and sperm release. Retinoic acid induces all four transitions [95] (Figure 4). Retinoic acid from Sertoli cells induces the premeiotic transitions. Once germ cells enter meiosis, pachytene spermatocytes produce RA to coordinate the two postmeiotic transitions [95]. Retinoic acid levels fluctuate in the testis to regulate the different transitions during spermatogenesis [95].
Figure 4.
During spermatogenesis, RA controls spermatogonial proliferation and differentiation, meiotic initiation, spermatid elongation, and sperm release. Spermatogonial stem cells undergo self-renewal or proliferate and differentiate to enter meiosis in response to RA.
Spermatogonial stem cells remain as stem cells (self-renewal) or proliferate and differentiate to entering meiosis in response to RA. A gene induced by RA, Stra8 (stimulated by retinoic acid 8), induces spermatogonial differentiation, meiotic initiation, and proliferation of both spermatogonial stem cells and induced differentiating spermatogonia [35].
A fraction of spermatogonia undergoes neither spermatogonial differentiation nor meiotic initiation in response to RA, ensuring that a reservoir of undifferentiated spermatogonia is maintained throughout the animal’s reproductive lifetime [96]. Spermatogonia and their precursors prospermatogonia exhibit a different capacity to respond to RA with at least two underlying causes. First, progenitor spermatogonia are prevented from responding to RA by the catabolic activity of CYP26 enzymes. Second, a smaller subset of undifferentiated spermatogonia enriched for spermatogonial stem cells exhibits catabolism-independent RA insensitivity [97]. Retinoic acid receptor α balances proliferation and differentiation of spermatogonia, and controls genome integrity during meiosis, coordinating proper spatial and temporal development of germ cells throughout spermatogenesis [98].
3.9. Retinoic Acid Controls the Regeneration of Tissues in the Adult Organism
Retinoic acid coordinates salamander limb regrowth after amputation [99]. Recently, Kim et al. reported a mechanism of tissue regeneration in adult organisms consisting of activation of the damage sensor TLR3 receptor and the consequent induction of intrinsic synthesis of RA [36]. Using an adult model of regeneration, where stem cells regenerate de novo hair follicles after a skin injury, they propose the following hypothesis: damage of tissue might induce the release of double-stranded RNA (dsRNA) that activates the TLR3 receptor and its downstream pathways STAT3 and NF-kB. Both pathways induced the expression of aldehyde dehydrogenase1A3 (ALDH1A3), which converts retinaldehyde to RA [100]. Either RA or dsRNA, but particularly both of them together, robustly increased ALDH1A3 protein expression [36]. Under these conditions, maximal upregulation of stem cell markers and downregulation of differentiation markers occur. Retinoic acid receptors (RAR) are essential in responding to RA and enhancing regeneration. In both, humans and mice, the dsRNA-RA axis is a conserved pathway for promoting regeneration [36]. An interesting question is whether a similar mechanism can activate tumor regeneration since TLR3 stimulation facilitates stem cell-like phenotypes in breast cancer [101,102,103,104].
4. Conclusions
The balance between self-renewal and differentiation of stem cells is crucial for development, regeneration in the adult organism, and cancer progression. Cancer progression involves a gradual loss of the differentiated phenotype and the acquisition of progenitor and stem cell-like features [105]. Retinoic acid is a well-known inductor of cell differentiation in many experimental models and has been effectively used in the treatment of acute promyelocytic leukemia. However, our present knowledge broadens the function of RA to include induction of cell stemness and progenitor cell proliferation. In consequence, RA can produce protumorigenic and anti-tumorigenic effects in different cancer cell types. The antagonistic effects of RA are not surprising since RA can activate more than one thousand different genes in two lines of triple-negative breast cancer cells [24]. RA also can promote extragenomic actions [23]. Moreover, the effect of RA on tumor stromal cells can shape the tumor microenvironment favoring tumor growth and invasion [74]. Finally, RA controls tumor immunosuppression in opposing ways, reducing immature myeloid cells and inducing regulatory T cells [87,88].
We need to know the critical signaling pathways controlled by RA that determine the final balance to stemness or differentiation. The main goal is to find cancer therapies able to block stemness and promote cell differentiation. Among the pathways promoting stemness controlled by RA that could be particularly significant are the VEGF signaling pathway [26,28,68,69], the Src-YAP-IL6 axis [25], and the activation of sensors of cell damage, such as TLR3 [36].
Retinoic acid controls the beginnings, transitions, and endings. With his two faces, RA looks to the past (stemness) and the future (differentiation), deciding the cell fate.
Acknowledgments
We thank Teresa Mas for her help in English writing.
Author Contributions
Conceptualization and writing, B.M. and C.M.; all authors proofread the manuscript.
Funding
This work was supported by MINECO (BIO2016-78006-R) and Fundació Marató de TV3 (2013–2830).
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Ghyselinck N.B., Duester G. Retinoic acid signaling pathways. Development. 2019;146:dev167502. doi: 10.1242/dev.167502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vassalli G. Aldehyde Dehydrogenases: Not Just Markers, but Functional Regulators of Stem Cells. Stem Cells Int. 2019;2019:1–15. doi: 10.1155/2019/3904645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nakajima Y. Retinoic acid signaling in heart development. Genes. 2019;57:e23300. doi: 10.1002/dvg.23300. [DOI] [PubMed] [Google Scholar]
- 4.Cunningham T.J., Duester G. Mechanisms of retinoic acid signalling and its roles in organ and limb development. Nat. Rev. Mol. Cell Boil. 2015;16:110–123. doi: 10.1038/nrm3932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Samarut E., Fraher D., Laudet V., Gibert Y. ZebRA: An overview of retinoic acid signaling during zebrafish development. Biochim. et Biophys. Acta (BBA) Bioenerg. 2015;1849:73–83. doi: 10.1016/j.bbagrm.2014.05.030. [DOI] [PubMed] [Google Scholar]
- 6.Gutierrez-Mazariegos J., Schubert M., Laudet V. Evolution of Retinoic Acid Receptors and Retinoic Acid Signaling. Subcell. Biochem. 2014;70:55–73. doi: 10.1007/978-94-017-9050-5_4. [DOI] [PubMed] [Google Scholar]
- 7.Das B.C., Thapa P., Karki R., Das S., Mahapatra S., Liu T.C., Torregroza I., Wallace D.P., Kambhampati S., Van Veldhuizen P., et al. Retinoic acid signaling pathways in development and diseases. Bioorg. Med. Chem. 2014;22:673–683. doi: 10.1016/j.bmc.2013.11.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tang X.-H., Gudas L.J. Retinoids, Retinoic Acid Receptors, and Cancer. Annu. Rev. Pathol. Mech. Dis. 2011;6:345–364. doi: 10.1146/annurev-pathol-011110-130303. [DOI] [PubMed] [Google Scholar]
- 9.Theodosiou M., Laudet V., Schubert M. From carrot to clinic: an overview of the retinoic acid signaling pathway. Cell. Mol. Life Sci. 2010;67:1423–1445. doi: 10.1007/s00018-010-0268-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Black W.J., Stagos D., Marchitti S.A., Nebert D.W., Tipton K.F., Bairoch A., Vasiliou V. Human aldehyde dehydrogenase genes: alternatively spliced transcriptional variants and their suggested nomenclature. Pharm. Genom. 2009;19:893–902. doi: 10.1097/FPC.0b013e3283329023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thatcher J.E., Isoherranen N. The role of CYP26 enzymes in retinoic acid clearance. Expert Opin. Drug Metab. Toxicol. 2009;5:875–886. doi: 10.1517/17425250903032681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stevison F., Jing J., Tripathy S., Isoherranen N. Role of Retinoic Acid-Metabolizing Cytochrome P450s, CYP26, in Inflammation and Cancer. HIV-1: Mol. Boil. Pathog. 2015;74:373–412. doi: 10.1016/bs.apha.2015.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Alonso S., Jones R.J., Ghiaur G. Retinoic acid, CYP26, and drug resistance in the stem cell niche. Exp. Hematol. 2017;54:17–25. doi: 10.1016/j.exphem.2017.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McGrane M.M. Vitamin A regulation of gene expression: molecular mechanism of a prototype gene. J. Nutr. Biochem. 2007;18:497–508. doi: 10.1016/j.jnutbio.2006.10.006. [DOI] [PubMed] [Google Scholar]
- 15.Gilardi F., Desvergne B. RXRs: Collegial Partners. Subcell. Biochem. 2014;70:75–102. doi: 10.1007/978-94-017-9050-5_5. [DOI] [PubMed] [Google Scholar]
- 16.Balmer J.E., Blomhoff R. Gene expression regulation by retinoic acid. J. Lipid Res. 2002;43:1773–1808. doi: 10.1194/jlr.R100015-JLR200. [DOI] [PubMed] [Google Scholar]
- 17.Schug T.T., Berry D.C., Shaw N.S., Travis S.N., Noy N. Opposing effects of retinoic acid on cell growth result from alternate activation of two different nuclear receptors. Cell. 2007;129:723–733. doi: 10.1016/j.cell.2007.02.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shaw N., Elholm M., Noy N. Retinoic Acid Is a High Affinity Selective Ligand for the Peroxisome Proliferator-activated Receptor β/δ. J. Boil. Chem. 2003;278:41589–41592. doi: 10.1074/jbc.C300368200. [DOI] [PubMed] [Google Scholar]
- 19.Ochoa W.F., Torrecillas A., Fita I., Verdaguer N., Corbalán-García S., Gómez-Fernández J.C., Torrecillas-Sanchez A. Retinoic Acid Binds to the C2-Domain of Protein Kinase Cα†. Biochemistry. 2003;42:8774–8779. doi: 10.1021/bi034713g. [DOI] [PubMed] [Google Scholar]
- 20.Radominska-Pandya A., Chen G., Czernik P.J., Little J.M., Samokyszyn V.M., Carter C.A., Nowak G. Direct Interaction of All-trans-retinoic Acid with Protein Kinase C (PKC) J. Boil. Chem. 2000;275:22324–22330. doi: 10.1074/jbc.M907722199. [DOI] [PubMed] [Google Scholar]
- 21.Masiá S., Alvarez S., De Lera A.R., Barettino D. Rapid, Nongenomic Actions of Retinoic Acid on Phosphatidylinositol-3-Kinase Signaling Pathway Mediated by the Retinoic Acid Receptor. Mol. Endocrinol. 2007;21:2391–2402. doi: 10.1210/me.2007-0062. [DOI] [PubMed] [Google Scholar]
- 22.De Angelis M.T., Parrotta E.I., Santamaria G., Cuda G. Short-term retinoic acid treatment sustains pluripotency and suppresses differentiation of human induced pluripotent stem cells. Cell Death Dis. 2018;9:6. doi: 10.1038/s41419-017-0028-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rossetti S., Ren M., Visconti N., Corlazzoli F., Gagliostro V., Somenzi G., Yao J., Sun Y., Sacchi N. Tracing anti-cancer and cancer-promoting actions of all-trans retinoic acid in breast cancer to a RARa epigenetic mechanism of mammary epithelial cell fate. Oncotarget. 2016;7:87064–87080. doi: 10.18632/oncotarget.13500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Marcato P., Dean C.A., Liu R.Z., Coyle K.M., Bydoun M., Wallace M., Clements D., Turner C., Mathenge E.G., Gujar S.A., et al. Aldehyde dehydrogenase 1A3 influences breast cancer progression via differential retinoic acid signaling. Mol. Oncol. 2015;9:17–31. doi: 10.1016/j.molonc.2014.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mezquita B., Mezquita P., Pau M., Gasa L., Navarro L., Samitier M., Pons M., Mezquita C. All-trans-retinoic acid activates the pro-invasive Src-YAP-Interleukin 6 axis in triple-negative MDA-MB-231 breast cancer cells while cerivastatin reverses this action. Sci. Rep. 2018;8:7047. doi: 10.1038/s41598-018-25526-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ciccone V., Terzuoli E., Donnini S., Giachetti A., Morbidelli L., Ziche M. Stemness marker ALDH1A1 promotes tumor angiogenesis via retinoic acid/HIF-1α/VEGF signalling in MCF-7 breast cancer cells. J. Exp. Clin. Cancer Res. 2018;37:311. doi: 10.1186/s13046-018-0975-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wu M.-J., Kim M.R., Chen Y.-S., Yang J.-Y., Chang C.-J. Retinoic acid directs breast cancer cell state changes through regulation of TET2-PKCζ pathway. Oncogene. 2017;36:3193–3206. doi: 10.1038/onc.2016.467. [DOI] [PMC free article] [PubMed] [Google Scholar] [Research Misconduct Found]
- 28.Mishra S., Kelly K.K., Rumian N.L., Siegenthaler J.A. Retinoic Acid Is Required for Neural Stem and Progenitor Cell Proliferation in the Adult Hippocampus. Stem Cell Rep. 2018;10:1705–1720. doi: 10.1016/j.stemcr.2018.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Choschzick I., Hirseland E., Cramer H., Schultz S., Leppert J., Tronnier V., Zechel C. Responsiveness of stem-like human glioma cells to all-trans retinoic acid and requirement of retinoic acid receptor isotypes α, β and γ. Neuroscience. 2014;279:44–64. doi: 10.1016/j.neuroscience.2014.07.078. [DOI] [PubMed] [Google Scholar]
- 30.Cabezas-Wallscheid N., Buettner F., Sommerkamp P., Klimmeck D., Ladel L., Thalheimer F.B., Pastor-Flores D., Roma L.P., Renders S., Zeisberger P., et al. Vitamin A-Retinoic Acid Signaling Regulates Hematopoietic Stem Cell Dormancy. Cell. 2017;169:807–823.e19. doi: 10.1016/j.cell.2017.04.018. [DOI] [PubMed] [Google Scholar]
- 31.Purton L.E., Dworkin S., Olsen G.H., Walkley C.R., Fabb S.A., Collins S.J., Chambon P. RARγ is critical for maintaining a balance between hematopoietic stem cell self-renewal and differentiation. J. Exp. Med. 2006;203:1283–1293. doi: 10.1084/jem.20052105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Guo P.-D., Lu X.-X., Gan W.-J., Li X.-M., He X.-S., Zhang S., Ji Q.-H., Zhou F., Cao Y., Wang J.-R., et al. RARγ Downregulation Contributes to Colorectal Tumorigenesis and Metastasis by Derepressing the Hippo–Yap Pathway. Cancer Res. 2016;76:3813–3825. doi: 10.1158/0008-5472.CAN-15-2882. [DOI] [PubMed] [Google Scholar]
- 33.Yan T.-D., Wu H., Zhang H.-P., Lu N., Ye P., Yu F.-H., Zhou H., Li W.-G., Cao X., Lin Y.-Y., et al. Oncogenic Potential of Retinoic Acid Receptor- in Hepatocellular Carcinoma. Cancer Res. 2010;70:2285–2295. doi: 10.1158/0008-5472.CAN-09-2968. [DOI] [PubMed] [Google Scholar]
- 34.Ishimoto T., Arima K., Uchihara T., Miyake K., Yonemura A., Yasuda T., Itoyama R., Iwatsuki M., Baba Y., Yoshida N., et al. Abstract 4677: Inhibition of 15-PGDH causes Kras-driven tumor expansion through prostaglandin E2-ALDH1 signaling in the pancreas. Tumor Biol. 2019;79:4677. doi: 10.1038/s41388-018-0510-y. [DOI] [PubMed] [Google Scholar]
- 35.Wang S., Wang X., Ma L., Lin X., Zhang D., Li Z., Wu Y., Zheng C., Feng X., Liao S., et al. Retinoic Acid Is Sufficient for the In Vitro Induction of Mouse Spermatocytes. Stem Cell Rep. 2016;7:80–94. doi: 10.1016/j.stemcr.2016.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kim D., Chen R., Sheu M., Kim N., Kim S., Islam N., Wier E.M., Wang G., Li A., Park A., et al. Noncoding dsRNA induces retinoic acid synthesis to stimulate hair follicle regeneration via TLR3. Nat. Commun. 2019;10:2811. doi: 10.1038/s41467-019-10811-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cho K.-W., Kwon H.-J., Shin J.-O., Lee J.-M., Cho S.-W., Tickle C., Jung H.-S. Retinoic acid signaling and the initiation of mammary gland development. Dev. Boil. 2012;365:259–266. doi: 10.1016/j.ydbio.2012.02.020. [DOI] [PubMed] [Google Scholar]
- 38.Gudas L.J., Wagner J.A. Retinoids regulate stem cell differentiation. J. Cell. Physiol. 2011;226:322–330. doi: 10.1002/jcp.22417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chung J.-H., Lee H.J., Kim B.-H., Cho N.-Y., Kang G.H. DNA methylation profile during multistage progression of pulmonary adenocarcinomas. Virchows Archiv. 2011;459:201–211. doi: 10.1007/s00428-011-1079-9. [DOI] [PubMed] [Google Scholar]
- 40.Pilato B., Pinto R., De Summa S., Lambo R., Paradiso A., Tommasi S. HOX gene methylation status analysis in patients with hereditary breast cancer. J. Hum. Genet. 2013;58:51–53. doi: 10.1038/jhg.2012.118. [DOI] [PubMed] [Google Scholar]
- 41.Chaturvedi P., Singh A.P., Batra S.K. Structure, evolution, and biology of the MUC4 mucin. FASEB J. 2008;22:966–981. doi: 10.1096/fj.07-9673rev. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mukhopadhyay P., Lakshmanan I., Ponnusamy M.P., Chakraborty S., Jain M., Pai P., Smith L.M., Lele S.M., Batra S.K. MUC4 Overexpression Augments Cell Migration and Metastasis through EGFR Family Proteins in Triple Negative Breast Cancer Cells. PLOS ONE. 2013;8:e54455. doi: 10.1371/journal.pone.0054455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yonezawa S., Goto M., Yamada N., Higashi M., Nomoto M. Expression profiles of MUC1, MUC2, and MUC4 mucins in human neoplasms and their relationship with biological behavior. Proteomics. 2008;8:3329–3341. doi: 10.1002/pmic.200800040. [DOI] [PubMed] [Google Scholar]
- 44.Yonezawa S., Higashi M., Yamada N., Yokoyama S., Kitamoto S., Kitajima S., Goto M. Mucins in human neoplasms: Clinical pathology, gene expression and diagnostic application. Pathol. Int. 2011;61:697–716. doi: 10.1111/j.1440-1827.2011.02734.x. [DOI] [PubMed] [Google Scholar]
- 45.Zhu Y., Zhang J.J., Zhu R., Liang W.B., Gao W.T., Yu J.B., Xu Z.K., Miao Y. The increase in the expression and hypomethylation of MUC4 gene with the progression of pancreatic ductal adenocarcinoma. Med. Oncol. 2011;28:S175–S184. doi: 10.1007/s12032-010-9683-0. [DOI] [PubMed] [Google Scholar]
- 46.Kim T., Lim D.-S. The SRF-YAP-IL6 axis promotes breast cancer stemness. Cell Cycle. 2016;15:1311–1312. doi: 10.1080/15384101.2016.1161994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lehmann W., Mossmann D., Kleemann J., Mock K., Meisinger C., Brummer T., Herr R., Brabletz S., Stemmler M.P., Brabletz T. ZEB1 turns into a transcriptional activator by interacting with YAP1 in aggressive cancer types. Nat. Commun. 2016;7:10498. doi: 10.1038/ncomms10498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kim T., Yang S.-J., Hwang D., Song J., Kim M., Kim S.K., Kang K., Ahn J., Lee D., Kim M.-Y., et al. A basal-like breast cancer-specific role for SRF–IL6 in YAP-induced cancer stemness. Nat. Commun. 2015;6:10186. doi: 10.1038/ncomms10186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bharti R., Dey G., Mandal M. Cancer development, chemoresistance, epithelial to mesenchymal transition and stem cells: A snapshot of IL-6 mediated involvement. Cancer Lett. 2016;375:51–61. doi: 10.1016/j.canlet.2016.02.048. [DOI] [PubMed] [Google Scholar]
- 50.Sansone P., Storci G., Tavolari S., Guarnieri T., Giovannini C., Taffurelli M., Ceccarelli C., Santini D., Paterini P., Marcu K.B., et al. IL-6 triggers malignant features in mammospheres from human ductal breast carcinoma and normal mammary gland. J. Clin. Investig. 2007;117:3988–4002. doi: 10.1172/JCI32533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Johnson D.E., O’Keefe R.A., Grandis J.R. Targeting the IL-6/JAK/STAT3 signalling axis in cancer. Nat. Rev. Clin. Oncol. 2018;15:234–248. doi: 10.1038/nrclinonc.2018.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Soleymani Abyaneh H., Gupta N., Alshareef A., Gopal K., Lavasanifar A., Lai R. Hypoxia Induces the Acquisition of Cancer Stem-like Phenotype Via Upregulation and Activation of Signal Transducer and Activator of Transcription-3 (STAT3) in MDA-MB-231, a Triple Negative Breast Cancer Cell Line. Cancer Microenviron. 2018;11:141–152. doi: 10.1007/s12307-018-0218-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lin C., Liao W., Jian Y., Peng Y., Zhang X., Ye L., Cui Y., Wang B., Wu X., Xiong Z., et al. CGI-99 promotes breast cancer metastasis via autocrine interleukin-6 signaling. Oncogene. 2017;36:3695–3705. doi: 10.1038/onc.2016.525. [DOI] [PubMed] [Google Scholar]
- 54.Banerjee K., Resat H. Constitutive activation of STAT3 in breast cancer cells: A review. Int. J. Cancer. 2016;138:2570–2578. doi: 10.1002/ijc.29923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yu F.-X., Guan K.-L. The Hippo pathway: regulators and regulations. Genes Dev. 2013;27:355–371. doi: 10.1101/gad.210773.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Taniguchi K., Wu L.-W., Grivennikov S.I., De Jong P.R., Lian I., Yu F.-X., Wang K., Ho S.B., Boland B.S., Chang J.T., et al. A gp130–Src–YAP module links inflammation to epithelial regeneration. Nature. 2015;519:57–62. doi: 10.1038/nature14228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Taniguchi K., Moroishi T., De Jong P.R., Krawczyk M., Grebbin B.M., Luo H., Xu R.-H., Golob-Schwarzl N., Schweiger C., Wang K., et al. YAP–IL-6ST autoregulatory loop activated on APC loss controls colonic tumorigenesis. Proc. Natl. Acad. Sci. USA. 2017;114:1643–1648. doi: 10.1073/pnas.1620290114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Rosenbluh J., Nijhawan D., Cox A.G., Li X., Neal J.T., Schafer E.J., Zack T.I., Wang X., Tsherniak A., Schinzel A.C., et al. β-Catenin-driven cancers require a YAP1 transcriptional complex for survival and tumorigenesis. Cell. 2012;151:1457–1473. doi: 10.1016/j.cell.2012.11.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zhi X., Tao J., Xie K., Zhu Y., Li Z., Tang J., Wang W., Xu H., Zhang J., Xu Z. MUC4-induced nuclear translocation of β-catenin: A novel mechanism for growth, metastasis and angiogenesis in pancreatic cancer. Cancer Lett. 2014;346:104–113. doi: 10.1016/j.canlet.2013.12.021. [DOI] [PubMed] [Google Scholar]
- 60.Mejías-Luque R., Peiró S., Vincent A., Van Seuningen I., De Bolós C. IL-6 induces MUC4 expression through gp130/STAT3 pathway in gastric cancer cell lines. Biochim. et Biophys. Acta (BBA) Bioenerg. 2008;1783:1728–1736. doi: 10.1016/j.bbamcr.2008.05.020. [DOI] [PubMed] [Google Scholar]
- 61.Hindley C.J., Condurat A.L., Menon V., Thomas R., Azmitia L.M., Davis J.A., Pruszak J. The Hippo pathway member YAP enhances human neural crest cell fate and migration. Sci. Rep. 2016;6:23208. doi: 10.1038/srep23208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Camargo F.D., Gokhale S., Johnnidis J.B., Fu D., Bell G.W., Jaenisch R., Brummelkamp T.R. YAP1 Increases Organ Size and Expands Undifferentiated Progenitor Cells. Curr. Boil. 2007;17:2054–2060. doi: 10.1016/j.cub.2007.10.039. [DOI] [PubMed] [Google Scholar]
- 63.Schlegelmilch K., Mohseni M., Kirak O., Pruszak J., Rodriguez J.R., Zhou D., Kreger B.T., Vasioukhin V., Avruch J., Brummelkamp T.R., et al. Yap1 acts downstream of α-catenin to control epidermal proliferation. Cell. 2011;144:782–795. doi: 10.1016/j.cell.2011.02.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zhou D., Zhang Y., Wu H., Barry E., Yin Y., Lawrence E., Dawson D., Willis J.E., Markowitz S.D., Camargo F.D., et al. Mst1 and Mst2 protein kinases restrain intestinal stem cell proliferation and colonic tumorigenesis by inhibition of Yes-associated protein (Yap) overabundance. Proc. Natl. Acad. Sci. USA. 2011;108:E1312–E1320. doi: 10.1073/pnas.1110428108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Zanconato F., Cordenonsi M., Piccolo S. YAP and TAZ: a signalling hub of the tumour microenvironment. Nat. Rev. Cancer. 2019;19:454–464. doi: 10.1038/s41568-019-0168-y. [DOI] [PubMed] [Google Scholar]
- 66.Iglesias J.M., Beloqui I., Garcia-Garcia F., Leis O., Vázquez-Martín A., Eguiara A., Cufí S., Pavon A., Menendez J.A., Dopazo J., et al. Mammosphere Formation in Breast Carcinoma Cell Lines Depends upon Expression of E-cadherin. PLOS ONE. 2013;8:e77281. doi: 10.1371/journal.pone.0077281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ginestier C., Wicinski J., Cervera N., Monville F., Finetti P., Bertucci F., Wicha M.S., Birnbaum D., Charafe-Jauffret E. Retinoid signaling regulates breast cancer stem cell differentiation. Cell Cycle. 2009;8:3297–3302. doi: 10.4161/cc.8.20.9761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Zhao D., Pan C., Sun J., Gilbert C., Drews-Elger K., Azzam D.J., Picon-Ruiz M., Kim M., Ullmer W., El-Ashry D., et al. VEGF drives cancer-initiating stem cells through VEGFR-2/Stat3 signaling to upregulate Myc and Sox2. Oncogene. 2015;34:3107–3119. doi: 10.1038/onc.2014.257. [DOI] [PubMed] [Google Scholar]
- 69.Kim M., Jang K., Miller P., Picon-Ruiz M., Yeasky T.M., El-Ashry D., Slingerland J.M. VEGFA links self-renewal and metastasis by inducing Sox2 to repress miR-452, driving Slug. Oncogene. 2017;36:5199–5211. doi: 10.1038/onc.2017.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Elaimy A.L., Guru S., Chang C., Ou J., Amante J.J., Zhu L.J., Goel H.L., Mercurio A.M. VEGF–Neuropilin-2 signaling promotes stem-like traits in breast cancer cells by TAZ-mediated repression of the Rac GAP β2-chimaerin. Sci. Signal. 2018;11:eaao6897. doi: 10.1126/scisignal.aao6897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Mercurio A.M. VEGF/Neuropilin Signaling in Cancer Stem Cells. Int. J. Mol. Sci. 2019;20:490. doi: 10.3390/ijms20030490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Lee T., Seng S., Sekine M., Hinton C., Fu Y., Avraham H., Avraham S. Vascular endothelial growth factor mediates intracrine survival in human breast carcinoma cells through internally expressed VEGFR1/FLT1. PLoS Med. 2007;4:e186. doi: 10.1371/journal.pmed.0040186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Bhattacharya R., Fan F., Wang R., Ye X., Xia L., Boulbes D., Ellis L.M. Intracrine VEGF signalling mediates colorectal cancer cell migration and invasion. Br. J. Cancer. 2017;117:848–855. doi: 10.1038/bjc.2017.238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Liu X., Nugoli M., Laferrière J., Saleh S.M., Rodrigue-Gervais I.G., Saleh M., Park M., Hallett M.T., Muller W.J., Giguère V. Stromal retinoic acid receptor beta promotes mammary gland tumorigenesis. Proc. Natl. Acad. Sci. USA. 2011;108:774–779. doi: 10.1073/pnas.1011845108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Martin-Belmonte F., Perez-Moreno M. Epithelial cell polarity, stem cells and cancer. Nat. Rev. Cancer. 2011;12:23–38. doi: 10.1038/nrc3169. [DOI] [PubMed] [Google Scholar]
- 76.Knoblich J.A. Asymmetric cell division: recent developments and their implications for tumour biology. Nat. Rev. Mol. Cell Boil. 2010;11:849–860. doi: 10.1038/nrm3010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Smith C.A., Lau K.M., Rahmani Z., Dho S.E., Brothers G., She Y.M., Berry D.M., Bonneil E., Thibault P., Schweisguth F., et al. aPKC-mediated phosphorylation regulates asymmetric membrane localization of the cell fate determinant Numb. EMBO J. 2007;26:468–480. doi: 10.1038/sj.emboj.7601495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Urtreger A.J., Kazanietz M.G., Bal de Kier Joffé E.D. Contribution of individual PKC isoforms to breast cancer progression. IUBMB Life. 2012;64:18–26. doi: 10.1002/iub.574. [DOI] [PubMed] [Google Scholar]
- 79.Song S.J., Poliseno L., Song M.S., Ala U., Webster K., Ng C., Beringer G., Brikbak N.J., Yuan X., Cantley L.C., et al. MicroRNA-antagonism regulates breast cancer stemness and metastasis via TET-family-dependent chromatin remodeling. Cell. 2013;154:311–324. doi: 10.1016/j.cell.2013.06.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Fettig L.M., McGinn O., Finlay-Schultz J., LaBarbera D.V., Nordeen S.K., A Sartorius C. Cross talk between progesterone receptors and retinoic acid receptors in regulation of cytokeratin 5-positive breast cancer cells. Oncogene. 2017;36:6074–6084. doi: 10.1038/onc.2017.204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Maden M. Retinoic acid in the development, regeneration and maintenance of the nervous system. Nat. Rev. Neurosci. 2007;8:755–765. doi: 10.1038/nrn2212. [DOI] [PubMed] [Google Scholar]
- 82.Janesick A., Wu S.C., Blumberg B. Retinoic acid signaling and neuronal differentiation. Cell. Mol. Life Sci. 2015;72:1559–1576. doi: 10.1007/s00018-014-1815-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Haushalter C., Asselin L., Fraulob V., Dollé P., Rhinn M. Retinoic acid controls early neurogenesis in the developing mouse cerebral cortex. Dev. Boil. 2017;430:129–141. doi: 10.1016/j.ydbio.2017.08.006. [DOI] [PubMed] [Google Scholar]
- 84.E Purton L., Bernstein I.D., Collins S.J. All-trans retinoic acid enhances the long-term repopulating activity of cultured hematopoietic stem cells. Blood. 2000;95:470–477. doi: 10.1182/blood.V95.2.470. [DOI] [PubMed] [Google Scholar]
- 85.Collins S.J. Retinoic acid receptors, hematopoiesis and leukemogenesis. Curr. Opin. Hematol. 2008;15:346–351. doi: 10.1097/MOH.0b013e3283007edf. [DOI] [PubMed] [Google Scholar]
- 86.Masetti R., Vendemini F., Zama D., Biagi C., Gasperini P., Pession A. All-transretinoic acid in the treatment of pediatric acute promyelocytic leukemia. Expert Rev. Anticancer. Ther. 2012;12:1191–1204. doi: 10.1586/era.12.101. [DOI] [PubMed] [Google Scholar]
- 87.Kusmartsev S., Cheng F., Yu B., Nefedova Y., Sotomayor E., Lush R., Gabrilovich D. All-trans-retinoic acid eliminates immature myeloid cells from tumor-bearing mice and improves the effect of vaccination. Cancer Res. 2003;63:4441–4449. [PubMed] [Google Scholar]
- 88.Bazewicz C.G., Dinavahi S.S., Schell T.D., Robertson G.P. Aldehyde dehydrogenase in regulatory T-cell development, immunity and cancer. Immunology. 2019;156:47–55. doi: 10.1111/imm.13016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Zhou D., Conrad C., Xia F., Park J.-S., Payer B., Yin Y., Lauwers G.Y., Thasler W., Lee J.T., Avruch J., et al. Mst1 and Mst2 maintain hepatocyte quiescence and suppress hepatocellular carcinoma development through inactivation of the Yap1 oncogene. Cancer Cell. 2009;16:425–438. doi: 10.1016/j.ccr.2009.09.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Xu M.Z., Yao T.-J., Lee N.P.Y., Ng I.O.L., Chan Y.-T., Zender L., Lowe S.W., Poon R.T.P., Luk J.M. Yes-associated protein is an independent prognostic marker in hepatocellular carcinoma. Cancer. 2009;115:4576–4585. doi: 10.1002/cncr.24495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Avruch J., Zhou D., Bardeesy N. YAP oncogene overexpression supercharges colon cancer proliferation. Cell Cycle. 2012;11:1090–1096. doi: 10.4161/cc.11.6.19453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Bleul T., Rühl R., Bulashevska S., Karakhanova S., Werner J., Bazhin A.V. Reduced retinoids and retinoid receptors’ expression in pancreatic cancer: A link to patient survival. Mol. Carcinog. 2015;54:870–879. doi: 10.1002/mc.22158. [DOI] [PubMed] [Google Scholar]
- 93.Herreros-Villanueva M., Er T.K., Bujanda L. Retinoic Acid Reduces Stem Cell–Like Features in Pancreatic Cancer Cells. Pancreas. 2015;44:918–924. doi: 10.1097/MPA.0000000000000373. [DOI] [PubMed] [Google Scholar]
- 94.Young M.-J., Wu Y.-H., Chiu W.-T., Weng T.-Y., Huang Y.-F., Chou C.-Y. All-trans retinoic acid downregulates ALDH1-mediated stemness and inhibits tumour formation in ovarian cancer cells. Carcinog. 2015;36:498–507. doi: 10.1093/carcin/bgv018. [DOI] [PubMed] [Google Scholar]
- 95.Endo T., Freinkman E., De Rooij D.G., Page D.C. Periodic production of retinoic acid by meiotic and somatic cells coordinates four transitions in mouse spermatogenesis. Proc. Natl. Acad. Sci. USA. 2017;114:E10132–E10141. doi: 10.1073/pnas.1710837114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Endo T., Romer K.A., Anderson E.L., Baltus A.E., De Rooij D.G., Page D.C. Periodic retinoic acid–STRA8 signaling intersects with periodic germ-cell competencies to regulate spermatogenesis. Proc. Natl. Acad. Sci. USA. 2015;112:E2347–E2356. doi: 10.1073/pnas.1505683112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Velte E.K., Niedenberger B.A., Serra N.D., Singh A., Roa-DeLaCruz L., Hermann B.P., Geyer C.B. Differential RA responsiveness directs formation of functionally distinct spermatogonial populations at the initiation of spermatogenesis in the mouse. Development. 2019;146:dev173088. doi: 10.1242/dev.173088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Peer N.R., Law S.M., Murdoch B., Goulding E.H., Eddy E.M., Kim K. Germ Cell–Specific Retinoic Acid Receptor α Functions in Germ Cell Organization, Meiotic Integrity, and Spermatogonia. Endocrinol. 2018;159:3403–3420. doi: 10.1210/en.2018-00533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Stocum D.L. Mechanisms of urodele limb regeneration. Regeneration. 2017;4:159–200. doi: 10.1002/reg2.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Canino C., Luo Y., Marcato P., Blandino G., Pass H.I., Cioce M. A STAT3-NFkB/DDIT3/CEBPβ axis modulates ALDH1A3 expression in chemoresistant cell subpopulations. Oncotarget. 2015;6:12637–12653. doi: 10.18632/oncotarget.3703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Jia D., Yang W., Li L., Liu H., Tan Y., Ooi S., Chi L., Filion L.G., Figeys D., Wang L. β-Catenin and NF-κB co-activation triggered by TLR3 stimulation facilitates stem cell-like phenotypes in breast cancer. Cell Death Differ. 2015;22:298–310. doi: 10.1038/cdd.2014.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Jia D., Wang L. The other face of TLR3: A driving force of breast cancer stem cells. Mol. Cell. Oncol. 2015;2 doi: 10.4161/23723556.2014.981443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Bondhopadhyay B., Moirangthem A., Basu A. Innate adjuvant receptor Toll-like receptor 3 can promote breast cancer through cell surface. Tumour Biol. 2015;36:1261–1271. doi: 10.1007/s13277-014-2737-8. [DOI] [PubMed] [Google Scholar]
- 104.Venkatesh A., Nandigam H., Muccioli M., Singh M., Loftus T., Lewis D., Pate M., Benencia F. Regulation of inflammatory factors by double-stranded RNA receptors in breast cancer cells. Immunobiology. 2018;223:466–476. doi: 10.1016/j.imbio.2017.11.005. [DOI] [PubMed] [Google Scholar]
- 105.Malta T.M., Sokolov A., Gentles A.J., Burzykowski T., Poisson L., Kamińska B., Huelsken J., Gevaert O., Colaprico A., Czerwińska P., et al. Machine Learning Identifies Stemness Features Associated with Oncogenic Dedifferentiation. Cell. 2018;173:338–354.e15. doi: 10.1016/j.cell.2018.03.034. [DOI] [PMC free article] [PubMed] [Google Scholar]