Abstract
OBJECTIVES
The aim of this study was to describe the rates and causes of unplanned readmissions at different time periods following percutaneous coronary intervention (PCI).
BACKGROUND
The rates and causes of readmission at different time periods after PCI remain incompletely elucidated.
METHODS
Patients undergoing PCI between 2010 and 2014 in the U.S. Nationwide Readmission Database were evaluated for the rates, causes, predictors, and costs of unplanned readmission between 0 and 7 days, 8 and 30 days, 31 and 90 days, and 91 and 180 days after index discharge.
RESULTS
This analysis included 2,412,000 patients; 2.5% were readmitted between 0 and 7 days, 7.6% between 8 and 30 days, 8.9% between 31 and 90 days, and 8.0% between 91 and 180 days (cumulative rates 2.5%, 9.9%, 18.0%, and 24.8%, respectively). The majority of readmissions during each time period were due to noncardiac causes (53.1% to 59.6%). Nonspecific chest pain was the most common identifiable noncardiac cause for readmission during each time period (14.2% to 22.7% of noncardiac readmissions). Coronary artery disease including angina was the most common cardiac cause for readmission during each time period (37.4% to 39.3% of cardiac readmissions). The second most common cardiac cause for readmission was acute myocardial infarction between 0 and 7 days (27.6% of cardiac readmissions) and heart failure during all subsequent time periods (22.2% to 23.7% of cardiac readmissions).
CONCLUSIONS
Approximately 25% of patients following PCI have unplanned readmissions within 6 months. Causes of readmission depend on the timing at which they are assessed, with noncardiovascular causes becoming more important at longer time points.
Keywords: cost, percutaneous coronary intervention, readmissions
Percutaneous coronary intervention (PCI) is the most common mode of revascularization in the United States in patients with coronary artery disease (1). With advances in stent technology and pharmacotherapy and changes in interventional practices, procedural outcomes post-PCI have improved over time, resulting in low in-hospital mortality and complication rates (2,3). This has led to a growing interest in the study of unplanned readmissions both as a quality metric and to help inform health care resources and use for patients following PCI (4-6).
Unplanned readmissions after PCI are important for several reasons. First, they may result from actions taken or omitted during the initial hospitalization (7), such as incomplete treatment or poor-quality care, often reflective of poor coordination among services at the time of discharge or ongoing care (8). Second, unplanned readmissions can be considered an adverse outcome for patients (9). Complications such as bleeding from dual-antiplatelet therapy (DAPT) have been shown to increase mortality when they occur after PCI (10,11). Third, readmissions may represent an unnecessary cost, which drains both bed capacity and financial resources from other hospital services. Finally, early readmissions are recognized as a quality metric, with financial penalties for hospitals under the Patient Protection and Affordable Care Act if risk-adjusted readmission rates for specific conditions exceed benchmarks (12).
Although multiple studies have evaluated readmissions after PCI at 30 days (3-5), less well known are the causes at longer time points than the 30-day cutoff used as a metric in the Affordable Care Act. “In addition, the recently proposed [Centers for Medicare and Medicaid Services] bundle payment models extend the period of monitoring for readmissions to 90 days after PCI” (13). Understanding these causes is crucial in helping plan the delivery of health care services and adopting measures to reduce readmissions, as the only intervention shown to reduce readmissions is to target specific causes (14). Therefore, in this retrospective cohort study of patients who underwent PCI in the Nationwide Readmission Database (NRD), we examined the rates, causes, predictors, and costs of readmissions following PCI at different time periods after index discharge.
METHODS
The NRD is a nationally representative sample of all-age, all-payer discharges from U.S. nonfederal hospitals produced by the Healthcare Cost and Utilization Project of the Agency for Healthcare Research and Quality (15). This database is composed of discharge-level hospitalization data from 21 geographically dispersed states. The dataset used in the present study was constructed to represent 49.3% of the U.S. population and 49.1% of all U.S. hospitalizations (4-6). Within a calendar year, hospitalizations and rehospitalizations can be determined using a deidentified unique patient linkage number assigned to each patient, which enables tracking of patients across hospitals within a state.
Individual patients in the NRD are assigned up to 15 procedure codes for each hospitalization. We defined PCI with the procedure codes 0066 (PTCA OR CORONARY ATHER), 3606 (INSERT CORON ART STENT), and 3607 (INSERT DRUG ELUTING CRNRY AR).
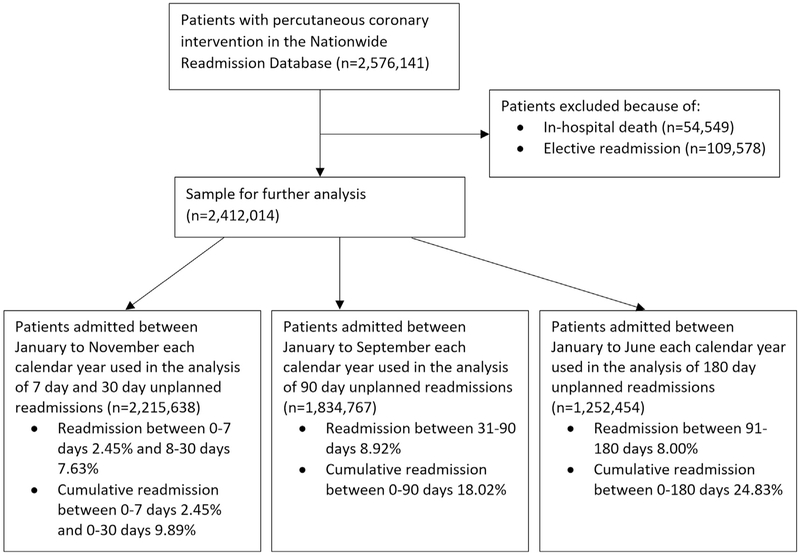
The primary outcome was first readmission after PCI performed between 2010 and 2014, with index discharge dates stratified into the following groups: 0 to 7 days, 8 to 30 days, 31 to 90 days, and 91 to 180 days of index discharge. Patients who died during their initial hospitalizations and planned elective readmissions for PCI were excluded. A problem that has been identified with the NRD dataset is bias related to inadequate follow-up because of the nature of the annualized dataset. For example, for 30 days of follow-up, the cohort patients admitted in the month of December must be excluded, as they may not have 30 days of follow-up, leading to immortal time bias. This is particularly problematic when considering multiple time points of follow-up, as in the case of the present study (7, 30, 90, and 180 days). To reduce the likelihood of biases, we excluded patients in December for the analysis of 7 and 30 days (cohort from January to November). We similarly excluded patients from October to December for the analysis of 90 days (cohort from January to September) and excluded patients from July to December for the analysis of 180 days (cohort from January to June). This is shown in Figure 1. The costs were determined by multiplying the hospital charges with the Agency for Healthcare Research and Quality’s all-payer cost-to-charge ratios for each hospital.
FIGURE 1. Flow Diagram of Patient Inclusion.
Flow diagram of patients included in the analysis according to timing of unplanned readmissions.
International Classification of Diseases-9th Revision (ICD-9) codes were used to define clinical variables, including smoking status, dyslipidemia, coronary artery disease, previous myocardial infarction, previous PCI, previous coronary artery bypass grafting, previous stroke or transient ischemic attack, atrial fibrillation, dementia, and receipt of circulatory support. Other comorbidity variables in the analysis were available via the Elixhauser Comorbidity Index and included alcohol misuse, chronic lung disease, heart failure, diabetes, valvular heart disease, peptic ulcer disease, hypertension, renal failure, obesity, cancer, fluid and electrolyte disorders, depression, peripheral vascular disease, hypothyroidism, liver disease, and anemia. The Charlson Comorbidity Index was calculated as previously described (4-6). Procedural ICD-9 codes were used to define multivessel disease, bifurcation disease, circulatory support, vasopressor use, intra-aortic balloon pump use, fractional flow reserve use, intravascular ultrasound, and drug-eluting stent use. Diagnostic ICD-9 codes were used to define in-hospital outcomes, including complete heart block, transient ischemic attack or stroke, cardiogenic shock, cardiac arrest, major bleeding, blood transfusion, vascular complication, and emergency coronary artery bypass grafting. Additional data were collected on length of stay in hospital, hospital bed size, hospital location and hospital teaching status, and discharge destination. Major bleeding was defined by ICD-9 codes 4590* (unspecified hemorrhage), 56681 (hemoperitoneum), 5789* (gastrointestinal hemorrhage), V582* (blood transfusion), 431* (intracerebral hemorrhage), and 4329* (intracranial hemorrhage). The causes of readmission were determined by the first diagnosis on the basis of Clinical Classification Software codes presented in Online Table 1.
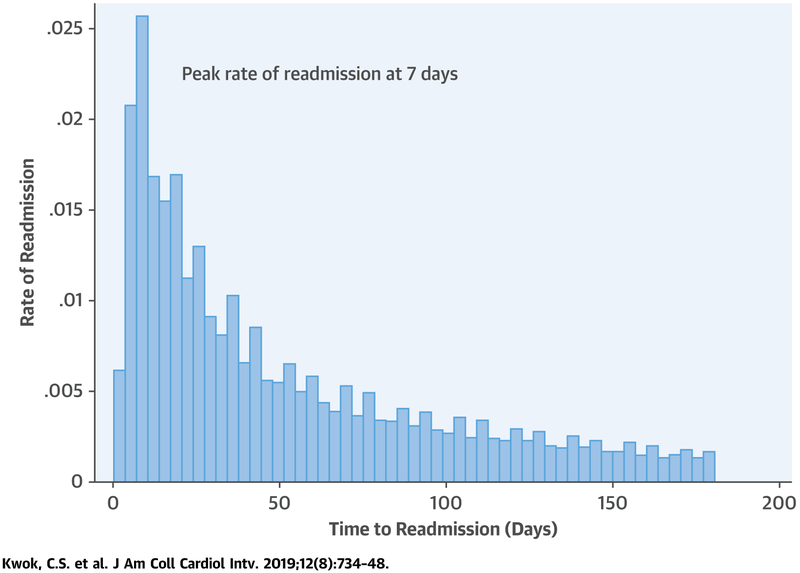
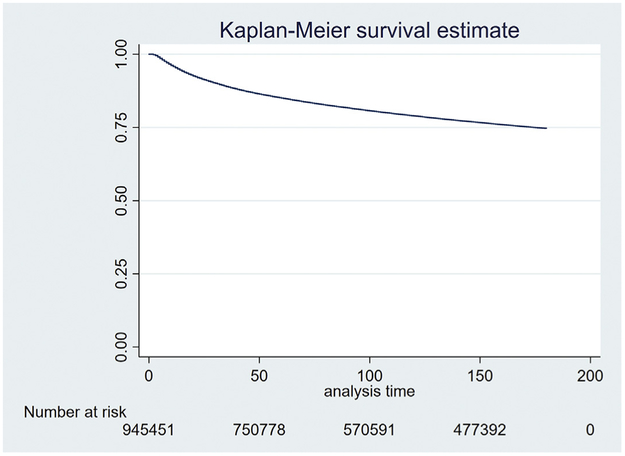
Statistical analysis was performed in Stata 15 (StataCorp, College Station, Texas). The incidence of unplanned readmissions according to time after PCI was graphically examined using a histogram. Bar graphs were used to examine rates of readmissions within the time periods 0 to 7 days, 8 to 30 days, 31 to 90 days, and 91 to 180 days post-PCI. Rates were also determined according to whether patients had acute ischemic syndrome or stable ischemic heart disease. Because there was an unequal number of days within each period, we further considered the rate of readmission per day within each time period by considering the overall rate and dividing by the number of days in the time period examined. A Kaplan-Meier survival curve was plotted to show the cumulative rate of readmission over time using the month of admission to estimate the follow-up for the control group that was not readmitted. Within the time periods, baseline characteristics of participants were examined and tested for statistical differences using the Student’s t-test for continuous variables and the chi-square test for categorical variables with no readmission as the reference group. Multiple logistic regressions were used to determine the predictors of readmission within each time period, with adjustments for all variables except the elective variable. The elective variable was not adjusted for because we adjusted for diagnosis of acute myocardial infarction (AMI), which is not an elective case. The causes of unplanned readmissions were examined with a graph and a table of rates. Total costs were also analyzed graphically.
RESULTS
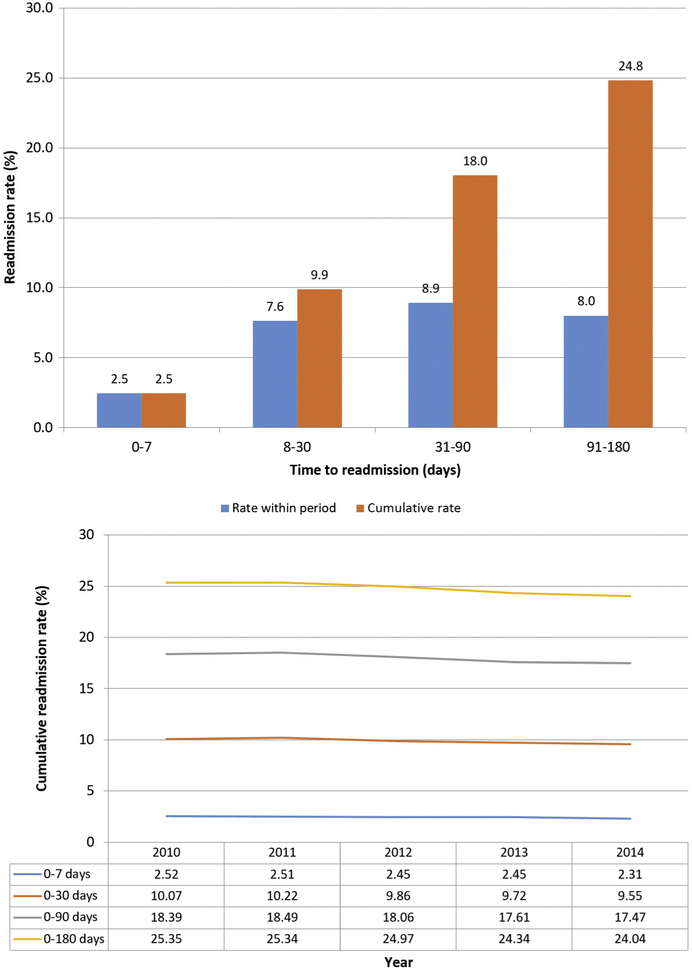
A total of 2,412,000 patients were included in the analysis after excluding patients who died during their index hospitalizations and those with planned readmissions (Figure 1). The percentage of readmissions that occurred between 0 and 7 days was 2.5%, which increased to 24.8% at 91 to 180 days (Figure 2), although there appears to have been a decline in readmissions between 2011 and 2014 for all groups. The median time to readmission was 35 days (interquartile range: 14 to 79 days). The peak readmission rate occurred at 7 days (Central Illustration). The daily readmission rates were 0.35% for 0 to 7 days, 0.33% for 8 to 30 days, 0.15% for 31 to 90 days, and 0.09% for 91 to 180 days. The Kaplan-Meier curve for the proportion of free from readmissions is shown in Figure 3, with a cumulative readmission rate at 6 months of 25%. The rates for unplanned readmissions at each individual time point as well as cumulative rates are shown in Online Tables 2a and 2b, respectively, for the cohorts with and without a diagnosis of AMI. At 0 to 7 days, the rates of readmission for AMI and no diagnosis of AMI were 2.41% and 2.49%, respectively (p = 0.011). At later time points, between 91 and 180 days, unplanned readmissions occurred in 6.83% and 9.24% in the groups with AMI and no diagnosis of AMI, respectively (p < 0.001). The corresponding cumulative rates up to 180 days were 22.86% and 26.84% (p < 0.001), respectively.
FIGURE 2. Rate of Unplanned Readmissions During Different Time Periods.
Rates of unplanned readmission within time groups and cumulative rates of unplanned readmissions over time.
CENTRAL ILLUSTRATION. Histogram and Temporal Trends According to Time to Unplanned Readmission.
Histogram of time to unplanned readmission, with peak rate of readmission at 7 days.
FIGURE 3. Kaplan-Meier Curve for Cumulative Unplanned Readmissions Over Time.
Number of patients without unplanned readmissions over time.
Tables 1 and 2 show the characteristics of patients according to time of readmission. Overall, patients who were readmitted were older and more likely to be women. Of the patients readmitted after index discharge, the average age and proportion of women were numerically similar across each readmission time period. There was also a greater prevalence of hypertension, diabetes mellitus, chronic lung disease, renal failure, and anemia among patients who were readmitted compared with those who were not across all time periods. The burden of comorbidity as measured by the Charlson Comorbidity Index was on average 1.4, 1.9, 2.0, and 1.8 for patients with readmissions between 0 and 7 days, 8 and 30 days, 31 and 90 days, and 91 and 180 days, respectively. This was significantly higher than patients who had no readmission during each of these time periods. The average length of stay during the index admission was shorter among patients who were readmitted between 0 and 7 days (2.4 days) compared with all other time points (5.2, 6.2, and 4.8 days for 8 to 30 days, 31 to 90 days, and 91 to 180 days, respectively). The index admission cost was $18,631, $25,018, $27,292, and $23,797 among patients who were readmitted between 0 and 7 days, 8 and 30 days, 31 and 90 days, and 91 and 180, respectively. Considering the cost of readmissions, the total cost increased from $29,767 in readmitted within 0 to 7 days group to $40,186 in the 31 to 90 days group (Online Figure 1).
TABLE 1.
Characteristics of Participants Readmitted Between 0 and 7 Days and Between 8 and 30 Days of Index Discharge After Percutaneous Coronary Intervention
| Available 30-Day Follow-Up With No Readmission Between 0 and 7 Days |
Readmission Between 0 and 7 Days |
Available 30-Day Follow-Up With No Readmission Between 8 and 30 Days |
Readmission Between 8 and 30 Days |
|||
|---|---|---|---|---|---|---|
| Mean ± SD or % | p Value* | Mean ± SD or % | 3 Value* | |||
| Age (yrs) | 65 ± 12 | 66 ± 13 | <0.001 | 64 ± 12 | 67 ± 13 | <0.001 |
| Female | 32.4 | 38.3 | <0.001 | 31.8 | 40.4 | <0.001 |
| Elective | 16.0 | 13.4 | <0.001 | 16.4 | 10.7 | <0.001 |
| Diagnosis of acute myocardial infarction | 51.8 | 51.0 | 0.011 | 51.9 | 50.5 | <0.001 |
| Primary expected payer | <0.001 | <0.001 | ||||
| Medicare | 52.3 | 59.6 | 51.3 | 64.9 | ||
| Medicaid | 7.5 | 8.5 | 7.3 | 9.3 | ||
| Private | 30.1 | 23.0 | 31.0 | 18.3 | ||
| Self-pay | 5.7 | 4.8 | 5.8 | 3.9 | ||
| No charge | 0.8 | 0.8 | 0.8 | 0.6 | ||
| Other | 3.7 | 3.4 | 3.7 | 3.0 | ||
| Quartile of median household income | 0.23 | <0.001 | ||||
| 0-25th | 28.8 | 29.3 | 28.6 | 31.2 | ||
| 26th-50th | 25.3 | 25.2 | 25.3 | 25.5 | ||
| 51st-75th | 24.0 | 24.0 | 24.1 | 23.2 | ||
| 76th-100th | 22.0 | 21.5 | 22.1 | 20.1 | ||
| Smoker | 41.5 | 39.8 | <0.001 | 41.7 | 39.1 | <0.001 |
| Alcohol misuse | 2.7 | 2.4 | 0.016 | 2.6 | 2.9 | <0.001 |
| Dyslipidemia | 71.4 | 71.2 | 0.56 | 71.7 | 67.3 | <0.001 |
| Hypertension | 74.6 | 77.6 | <0.001 | 74.3 | 78.1 | <0.001 |
| Diabetes | 36.7 | 40.3 | <0.001 | 35.9 | 45.7 | <0.001 |
| Obesity | 16.0 | 15.2 | 0.001 | 15.9 | 16.3 | 0.007 |
| Heart failure | 1.6 | 0.5 | <0.001 | 1.4 | 3.1 | <0.001 |
| Coronary artery disease | 94.1 | 94.8 | <0.001 | 94.1 | 93.9 | 0.013 |
| Previous myocardial infarction | 14.2 | 15.1 | <0.001 | 14.1 | 15.8 | <0.001 |
| Previous PCI | 20.9 | 22.1 | <0.001 | 20.8 | 21.3 | 0.004 |
| Previous CABG | 7.8 | 9.0 | <0.001 | 7.6 | 9.3 | <0.001 |
| Valvular heart disease | 0.5 | 0.2 | <0.001 | 0.4 | 1.0 | <0.001 |
| Atrial fibrillation | 11.6 | 12.8 | <0.001 | 10.9 | 19.5 | <0.001 |
| Previous stroke or TIA | 6.9 | 8.6 | <0.001 | 6.6 | 10.3 | <0.001 |
| Peripheral vascular disease | 11.0 | 12.7 | <0.001 | 10.5 | 16.7 | <0.001 |
| Pulmonary circulatory disorders | 0.3 | 0.1 | <0.001 | 0.3 | 0.6 | <0.001 |
| Peptic ulcer disease | 0.02 | 0.02 | 0.50 | 0.02 | 0.03 | 0.22 |
| Chronic lung disease | 16.7 | 19.5 | <0.001 | 16.0 | 25.8 | <0.001 |
| Renal failure | 13.4 | 16.2 | <0.001 | 12.4 | 25.4 | <0.001 |
| Liver disease | 1.3 | 1.6 | <0.001 | 1.2 | 2.0 | <0.001 |
| Hypothyroidism | 9.2 | 10.5 | <0.001 | 9.0 | 11.9 | <0.001 |
| Fluid and electrolyte disorder | 12.6 | 11.1 | <0.001 | 11.9 | 21.2 | <0.001 |
| Anemia | 10.8 | 11.8 | <0.001 | 9.9 | 21.1 | <0.001 |
| Cancer | 1.7 | 2.0 | 0.006 | 1.6 | 3.1 | <0.001 |
| Depression | 6.6 | 8.2 | <0.001 | 6.4 | 9.3 | <0.001 |
| Dementia | 1.9 | 2.6 | <0.001 | 1.8 | 3.5 | <0.001 |
| Charlson score | 1.3 ± 1.4 | 1.4 ± 1.5 | <0.001 | 1.2 ± 1.4 | 1.9 ± 1.7 | <0.001 |
| Hospital bed size | 0.10 | <0.001 | ||||
| Small | 5.6 | 5.6 | 5.7 | 4.8 | ||
| Medium | 20.7 | 21.3 | 20.8 | 20.4 | ||
| Large | 73.7 | 73.1 | 73.6 | 74.8 | ||
| Urban hospital | 95.8 | 95.7 | 0.56 | 95.8 | 95.9 | 0.029 |
| Teaching hospital | 54.6 | 52.4 | <0.001 | 54.7 | 54.2 | 0.022 |
| Multivessel | 16.1 | 16.8 | 0.004 | 16.1 | 16.1 | 0.59 |
| Bifurcation lesion | 2.9 | 2.8 | 0.45 | 2.9 | 2.7 | 0.045 |
| Circulatory support | 3.0 | 1.9 | <0.001 | 2.9 | 4.9 | <0.001 |
| Vasopressor use | 0.5 | 0.3 | 0.002 | 0.4 | 0.7 | <0.001 |
| Intra-aortic balloon pump | 2.7 | 1.7 | <0.001 | 2.6 | 4.4 | <0.001 |
| Fractional flow reserve | 1.9 | 2.1 | 0.14 | 1.9 | 2.0 | 0.066 |
| Intravascular ultrasound | 7.0 | 6.8 | 0.20 | 7.0 | 7.0 | 0.87 |
| Drug-eluting stent | 74.2 | 71.7 | <0.001 | 74.8 | 67.0 | <0.001 |
| In-hospital complete heart block | 1.0 | 0.7 | <0.001 | 1.0 | 1.3 | <0.001 |
| In-hospital stroke/TIA | 2.9 | 2.7 | 0.036 | 2.9 | 4.1 | <0.001 |
| Cardiogenic shock | 2.8 | 1.5 | <0.001 | 2.6 | 4.6 | <0.001 |
| Cardiac arrest | 1.8 | 1.0 | <0.001 | 1.8 | 2.3 | <0.001 |
| In-hospital bleeding | 0.7 | 0.4 | <0.001 | 0.6 | 1.3 | <0.001 |
| In-hospital vascular complications | 0.8 | 0.6 | 0.003 | 0.8 | 1.2 | <0.001 |
| In-hospital emergency CABG | 1.4 | 0.1 | <0.001 | 1.4 | 1.9 | <0.001 |
| Index admission length of stay (days) | 3.8 ± 5.2 | 2.4 ± 1.3 | <0.001 | 3.7 ± 5.3 | 5.2 ± 4.3 | <0.001 |
| Index admission cost (U.S. $) | $21,958 ± 17,906 | $18,631 ± 8,616 | <0.001 | $21,704 ± 18,026 | $25,018 ± 16,072 | <0.001 |
| Discharge destination | <0.001 | <0.001 | ||||
| Home/self-care | 87.7 | 88.2 | 88.8 | 74.6 | ||
| Transfer to other hospital | 4.9 | 3.9 | 4.4 | 10.2 | ||
| Care home | 7.0 | 6.8 | 6.4 | 14.6 | ||
| Discharge against medical advice | 0.4 | 1.1 | 0.4 | 0.7 | ||
| Readmission length of stay (days) | – | 3.6 ± 4.7 | – | – | 4.5 ± 5.6 | – |
| Readmission cost (U.S. $) | – | $11,258 ± 16,472 | – | – | $12,191 ± 16,939 | – |
| Readmission death | – | 2.3 | – | – | 2.9 | – |
| Total cost (index and readmission) | $21,958 ± 17,906 | $29,767 ± 19,548 | <0.001 | $21,704 ± 18,026 | $37,155 ± 25,312 | <0.001 |
Values are mean ± SD or %, unless otherwise indicated.
p value compared with no readmission.
CABG = coronary artery bypass graft; PCI = percutaneous coronary intervention; TIA = transient ischemic attack.
TABLE 2.
Characteristics of Participants Readmitted Between 31 and 90 Days and Between 91 and 180 Days of Index Discharge After Percutaneous Coronary Intervention
| Available 90-Day Follow-Up With No Readmission Between 31 and 90 Days |
Readmission Between 31 and 90 Days |
Available 180-Day Follow-Up With No Readmission Between 90 and 180 Days |
Readmission Between 91 and 180 Days |
|||
|---|---|---|---|---|---|---|
| Mean ± SD or % | p Value* | Mean ± SD or % | p Value* | |||
| Age (yrs) | 64 ± 12 | 67 ± 13 | <0.001 | 64 ± 12 | 66 ± 13 | <0.001 |
| Female | 30.8 | 40.4 | <0.001 | 30.1 | 38.8 | <0.001 |
| Elective | 17.0 | 12.5 | <0.001 | 17.4 | 14.6 | <0.001 |
| Diagnosis of acute myocardial infarction | 51.9 | 45.1 | <0.001 | 51.9 | 43.8 | <0.001 |
| Primary expected payer | <0.001 | <0.001 | ||||
| Medicare | 50.0 | 64.6 | 49.0 | 62.3 | ||
| Medicaid | 7.0 | 9.9 | 6.8 | 9.4 | ||
| Private | 32.4 | 17.8 | 33.5 | 19.6 | ||
| Self-pay | 6.0 | 4.0 | 6.0 | 4.7 | ||
| No charge | 0.8 | 0.7 | 0.8 | 0.8 | ||
| Other | 3.8 | 2.9 | 3.8 | 3.2 | ||
| Quartile of median household income | <0.001 | <0.001 | ||||
| 0-25th | 28.3 | 31.9 | 27.9 | 32.0 | ||
| 26th-50th | 25.2 | 25.4 | 25.2 | 25.0 | ||
| 51st-75th | 24.2 | 22.9 | 24.3 | 22.7 | ||
| 76th-100th | 22.4 | 19.9 | 22.6 | 20.3 | ||
| Smoker | 41.9 | 38.7 | <0.001 | 41.8 | 39.5 | <0.001 |
| Alcohol misuse | 2.6 | 3.1 | <0.001 | 2.5 | 2.8 | 0.005 |
| Dyslipidemia | 72.2 | 67.2 | <0.001 | 72.5 | 70.3 | <0.001 |
| Hypertension | 73.8 | 78.5 | <0.001 | 73.4 | 79.1 | <0.001 |
| Diabetes | 34.9 | 46.9 | <0.001 | 33.9 | 46.1 | <0.001 |
| Obesity | 15.8 | 16.7 | <0.001 | 15.7 | 17.0 | <0.001 |
| Heart failure | 1.2 | 4.1 | <0.001 | 1.0 | 2.7 | <0.001 |
| Coronary artery disease | 94.2 | 93.9 | 0.001 | 94.2 | 94.9 | <0.001 |
| Previous myocardial infarction | 14.0 | 16.6 | <0.001 | 13.8 | 17.8 | <0.001 |
| Previous PCI | 20.8 | 23.5 | <0.001 | 20.7 | 26.1 | <0.001 |
| Previous CABG | 7.5 | 10.1 | <0.001 | 7.3 | 11.0 | <0.001 |
| Valvular heart disease | 0.4 | 1.2 | <0.001 | 0.3 | 0.8 | <0.001 |
| Atrial fibrillation | 10.1 | 18.6 | <0.001 | 9.7 | 15.3 | <0.001 |
| Previous stroke or TIA | 6.1 | 10.6 | <0.001 | 5.7 | 10.1 | <0.001 |
| Peripheral vascular disease | 9.8 | 17.0 | <0.001 | 9.3 | 15.5 | <0.001 |
| Pulmonary circulatory disorders | 0.2 | 0.8 | <0.001 | 0.2 | 0.5 | <0.001 |
| Peptic ulcer disease | 0.02 | 0.03 | 0.20 | 0.02 | 0.03 | 0.16 |
| Chronic lung disease | 15.0 | 25.4 | <0.001 | 14.5 | 22.8 | <0.001 |
| Renal failure | 11.0 | 25.8 | <0.001 | 10.1 | 21.9 | <0.001 |
| Liver disease | 1.1 | 2.0 | <0.001 | 1.0 | 1.7 | <0.001 |
| Hypothyroidism | 8.7 | 11.5 | <0.001 | 8.4 | 10.9 | <0.001 |
| Fluid and electrolyte disorder | 10.9 | 20.8 | <0.001 | 10.3 | 16.1 | <0.001 |
| Anemia | 8.8 | 21.0 | <0.001 | 8.1 | 16.9 | <0.001 |
| Cancer | 1.5 | 3.1 | <0.001 | 1.4 | 2.4 | <0.001 |
| Depression | 6.1 | 9.1 | <0.001 | 5.8 | 8.8 | <0.001 |
| Dementia | 1.6 | 3.5 | <0.001 | 1.5 | 2.8 | <0.001 |
| Charlson score | 1.1 ± 1.3 | 2.0 ± 1.7 | <0.001 | 1.1 ± 1.3 | 1.8 ± 1.6 | <0.001 |
| Hospital bed size | <0.001 | <0.001 | ||||
| Small | 5.8 | 4.8 | 5.9 | 5.1 | ||
| Medium | 20.8 | 19.7 | 20.8 | 20.2 | ||
| Large | 73.4 | 75.4 | 73.3 | 74.7 | ||
| Urban hospital | 95.8 | 95.9 | 0.25 | 95.8 | 96.0 | 0.039 |
| Teaching hospital | 54.7 | 54.8 | 0.54 | 54.8 | 55.0 | 0.42 |
| Multivessel | 16.0 | 16.4 | 0.003 | 16.0 | 17.0 | <0.001 |
| Bifurcation lesion | 2.9 | 2.8 | 0.33 | 2.9 | 2.8 | 0.23 |
| Circulatory support | 2.7 | 4.7 | <0.001 | 2.6 | 3.3 | <0.001 |
| Vasopressor use | 0.4 | 0.6 | <0.001 | 0.4 | 0.4 | 0.57 |
| Intra-aortic balloon pump | 2.4 | 4.1 | <0.001 | 2.3 | 2.8 | <0.001 |
| Fractional flow reserve | 1.8 | 1.9 | 0.96 | 1.8 | 1.9 | 0.12 |
| Intravascular ultrasound | 7.0 | 7.1 | 0.58 | 7.1 | 7.5 | 0.006 |
| Drug-eluting stent | 75.7 | 65.8 | <0.001 | 76.2 | 69.3 | <0.001 |
| In-hospital complete heart block | 1.0 | 1.2 | <0.001 | 0.9 | 1.0 | 0.32 |
| In-hospital stroke/TIA | 2.7 | 4.4 | <0.001 | 2.6 | 3.6 | <0.001 |
| Cardiogenic shock | 2.4 | 4.6 | <0.001 | 2.3 | 2.9 | <0.001 |
| Cardiac arrest | 1.7 | 2.3 | <0.001 | 1.6 | 1.6 | 0.38 |
| In-hospital bleeding | 0.5 | 1.3 | <0.001 | 0.5 | 0.9 | <0.001 |
| In-hospital vascular complications | 0.7 | 1.2 | <0.001 | 0.7 | 0.9 | <0.001 |
| In-hospital emergency CABG | 1.3 | 1.6 | <0.001 | 1.4 | 1.2 | 0.001 |
| Index admission length of stay (days) | 3.4 ± 4.8 | 6.2 ± 7.8 | <0.001 | 3.3 ± 4.5 | 4.8 ± 7.3 | <0.001 |
| Index admission cost (U.S. $) | $20,978 ± 16,664 | $27,292 ± 26,175 | <0.001 | $20,645 ± 15,983 | $23,797 ± 23,480 | <0.001 |
| Discharge destination | <0.001 | <0.001 | ||||
| Home/self-care | 90.3 | 74.9 | 91.0 | 82.0 | ||
| Transfer to other hospital | 3.6 | 11.8 | 3.3 | 7.1 | ||
| Care home | 5.7 | 12.8 | 5.3 | 10.3 | ||
| Discharge against medical advice | 0.4 | 0.5 | 0.4 | 0.5 | ||
| Readmission length of stay (days) | – | 4.7 ± 6.2 | – | – | 4.3 ± 5.5 | – |
| Readmission cost (U.S. $) | – | $12,960 ± 17,858 | – | – | $13,175 ± 17,810 | – |
| Readmission death | – | 2.6 | – | – | 2.1 | – |
| Total cost (index and readmission) | $20,978 ± 16,664 | $40,186 ± 34,142 | <0.001 | $20,645 ± 15,983 | $36,905 ± 31,858 | <0.001 |
Values are mean ± SD or %, unless otherwise indicated.
p value compared with no readmission.
Abbreviations as in Table 1.
Table 3 describes the significant predictors of readmissions within the 4 time periods, after multivariate adjustment for baseline characteristics. The strongest predictors of readmission were diabetes mellitus, chronic lung disease, renal failure, liver disease, anemia, cancer, and discharge to another hospital or care home or discharge against medical advice.
TABLE 3.
Significant Predictors of Readmissions at Different Time Periods After Index Discharge for Percutaneous Coronary Intervention
| Readmission Between 0 and 7 Days |
Readmission Between 8 and 30 Days |
Readmission Between 31 and 90 Days |
Readmission Between 90 and 180 Days |
|
|---|---|---|---|---|
| Age (per yr increase) | – | 1.00 (1.00-1.00) | 1.00 (1.00-1.00) | 1.00 (1.00-1.00) |
| Female | 1.28 (1.23-1.32) | 1.20 (1.18-1.23) | 1.23 (1.20-1.26) | 1.26 (1.22-1.30) |
| Diagnosis of acute myocardial infarction | 1.18 (1.14-1.23) | – | 0.81 (0.79-0.83) | 0.80 (0.77-0.82) |
| Primary expected payer vs. Medicare | ||||
| Medicaid | 1.11 (1.04-1.19) | 1.18 (1.13-1.22) | 1.19 (1.14-1.25) | 1.18 (1.11-1.25) |
| Private | 0.73 (0.69-0.76) | 0.69 (0.67-0.71) | 0.63 (0.61-0.65) | 0.64 (0.61-0.67) |
| Self-pay | 0.82 (0.75-0.89) | 0.74 (0.70-0.78) | 0.75 (0.70-0.79) | 0.81 (0.76-0.87) |
| No charge | – | 0.85 (0.75-0.97) | 0.84 (0.75-0.93) | – |
| Other | 0.90 (0.82-0.99) | 0.79 (0.75-0.84) | 0.76 (0.72-0.81) | 0.78 (0.72-0.85) |
| Quartile of median household income vs. 0-25th | ||||
| 26th-50th | – | 0.96 (0.93-0.99) | 0.94 (0.91-0.97) | 0.89 (0.85-0.93) |
| 51st-75th | – | 0.94 (0.91-0.97) | 0.92 (0.89-0.95) | 0.90 (0.86-0.94) |
| 76th-100th | – | 0.94 (0.91-0.98) | 0.93 (0.90-0.96) | 0.90 (0.86-0.95) |
| Smoker | 0.92 (0.89-0.96) | 0.97 (0.95-1.00) | – | 0.97 (0.94-1.00) |
| Alcohol misuse | – | 1.14 (1.07-1.21) | 1.17 (1.10-1.24) | 1.16 (1.06-1.27) |
| Dyslipidemia | 0.91 (0.88-0.95) | 0.87 (0.85-0.89) | 0.85 (0.83-0.87) | 0.87 (0.85-0.90) |
| Hypertension | 1.07 (1.02-1.11) | 1.06 (1.03-1.08) | 1.07 (1.04-1.10) | 1.09 (1.05-1.12) |
| Diabetes | 1.15 (1.11-1.19) | 1.24 (1.21-1.26) | 1.31 (1.28-1.35) | 1.34 (1.30-1.37) |
| Obesity | 0.95 (0.91-0.99) | 0.94 (0.91-0.96) | 0.95 (0.93-0.98) | – |
| Heart failure | – | – | – | – |
| Coronary artery disease | – | – | – | – |
| Previous myocardial infarction | – | 1.06 (1.03-1.09) | 1.08 (1.04-1.11) | 1.14 (1.10-1.19) |
| Previous PCI | – | – | 1.11 (1.08-1.14) | 1.21 (1.17-1.25) |
| Previous CABG | – | 1.11 (1.07-1.14) | 1.16 (1.12-1.20) | 1.31 (1.25-1.37) |
| Valvular heart disease | – | – | 1.18 (1.03-1.35) | – |
| Atrial fibrillation | 1.30 (1.23-1.37) | 1.45 (1.41-1.49) | 1.37 (1.33-1.42) | 1.25 (1.20-1.30) |
| Previous stroke or TIA | 1.17 (1.10-1.24) | 1.17 (1.13-1.21) | 1.23 (1.18-1.27) | 1.33 (1.27-1.40) |
| Peripheral vascular disease | 1.18 (1.12-1.25) | 1.19 (1.16-1.22) | 1.25 (1.21-1.29) | 1.24 (1.19-1.30) |
| Pulmonary circulatory disorders | – | – | – | – |
| Peptic ulcer disease | – | – | – | – |
| Chronic lung disease | 1.27 (1.22-1.33) | 1.42 (1.38-1.45) | 1.43 (1.39-1.47) | 1.35 (1.30-1.40) |
| Renal failure | 1.36 (1.30-1.43) | 1.51 (1.47-1.55) | 1.57 (1.52-1.61) | 1.59 (1.53-1.66) |
| Liver disease | 1.36 (1.30-1.65) | 1.34 (1.25-1.44) | 1.37 (1.33-1.42) | 1.25 (1.12-1.40) |
| Hypothyroidism | – | – | – | – |
| Fluid and electrolyte disorder | 1.16 (1.10-1.23) | 1.24 (1.21-1.28) | 1.17 (1.14-1.21) | 1.11 (1.06-1.16) |
| Anemia | 1.26 (1.19-1.34) | 1.37 (1.33-1.41) | 1.39 (1.35-1.43) | 1.32 (1.26-1.38) |
| Cancer | 1.19 (1.05-1.35) | 1.45 (1.37-1.54) | 1.59 (1.48-1.69) | 1.45 (1.31-1.61) |
| Depression | 1.23 (1.16-1.31) | 1.23 (1.19-1.27) | 1.20 (1.15-1.25) | 1.28 (1.21-1.35) |
| Dementia | 1.23 (1.10-1.38) | 1.12 (1.06-1.19) | 1.16 (1.09-1.25) | 1.11 (1.00-1.23) |
| Hospital bed size vs. small | ||||
| Medium | – | – | – | – |
| Large | – | – | 1.10 (1.01-1.19) | – |
| Urban hospital | 1.12 (1.03-1.22) | 1.09 (1.03-1.15) | 1.09 (1.04-1.15) | 1.14 (1.07-1.21) |
| Teaching hospital | 0.91 (0.88-0.95) | – | – | 0.96 (0.93-1.00) |
| Multivessel | 1.05 (1.01-1.10) | – | – | 1.07 (1.03-1.11) |
| Bifurcation lesion | – | – | – | 0.90 (0.83-0.98) |
| Circulatory support | – | – | – | – |
| Vasopressor use | – | – | – | – |
| Intra-aortic balloon pump | – | 1.28 (1.09-1.51) | – | – |
| Fractional flow reserve | – | 1.10 (1.03-1.19) | – | – |
| Intravascular ultrasound | – | – | – | – |
| Drug-eluting stent | 0.82 (0.79-0.85) | 0.81 (0.80-0.83) | 0.73 (0.71-0.74) | 0.76 (0.74-0.79) |
| In-hospital complete heart block | – | – | – | – |
| In-hospital stroke/TIA | – | – | – | – |
| Cardiogenic shock | – | – | – | – |
| Cardiac arrest | – | – | 0.83 (0.76-0.90) | 0.73 (0.65-0.82) |
| In-hospital bleeding | – | 1.15 (1.04-1.28) | 1.21 (1.08-1.35) | – |
| In-hospital vascular complications | – | 1.14 (1.04-1.24) | – | – |
| In-hospital emergency CABG | 0.30 (0.19-0.46) | 0.84 (0.78-0.92) | 0.62 (0.57-0.68) | 0.52 (0.46-0.59) |
| Index admission length of stay (days) | 0.76 (0.75-0.77) | 1.00 (1.00-1.00) | 1.03 (1.02-1.03) | 1.02 (1.01-1.02) |
| Discharge destination vs. home/self-care | ||||
| Transfer to other hospital | 1.47 (1.32-1.64) | 1.52 (1.45-1.59) | 1.74 (1.66-1.83) | 1.30 (1.21-1.40) |
| Care home | 1.38 (1.29-1.48) | 1.69 (1.63-1.74) | 1.47 (1.42-1.53) | 1.32 (1.26-1.39) |
| Discharge against medical advice | 2.16 (1.86-2.52) | 1.70 (1.51-1.92) | 1.38 (1.20-1.60) | 1.42 (1.18-1.71) |
Values are odds ratio (95% confidence interval).
Abbreviations as in Table 1.
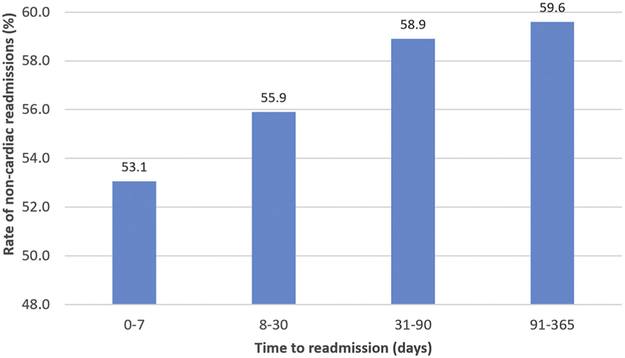
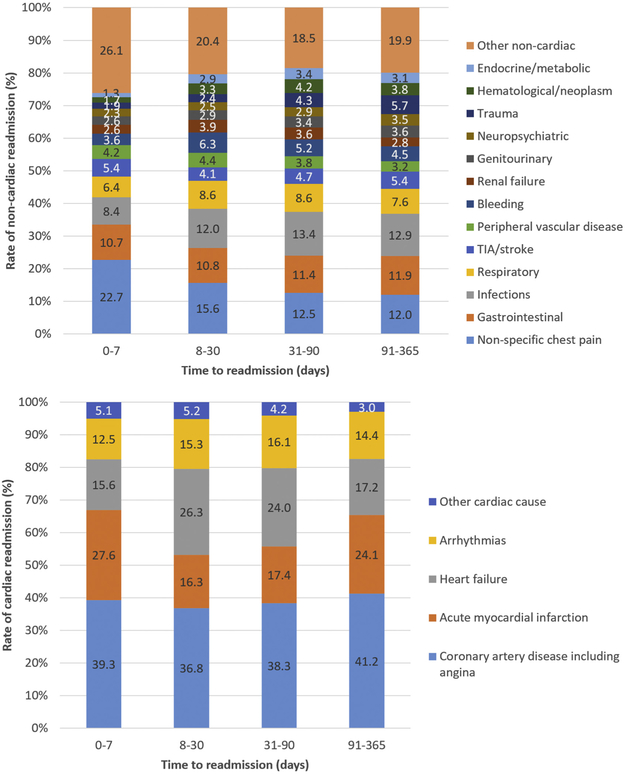
Noncardiac causes were the most common causes of readmission at all time points studied, increasing from 53.1% at 0 to 7 days to 59.6% between 91 and 180 days (Figure 4). The causes of readmissions at different readmission time periods are shown in Table 4 and Figure 5. Nonspecific chest pain was the most common cause of noncardiac readmission early post-discharge at 22.7% in the period from 0 to 7 days but declined to 12.0% in the period from 90 to 180 days. Readmissions for gastrointestinal (excluding gastrointestinal bleeding) and infectious causes for readmissions increased from 10.7% to 11.9% and from 8.4% to 12.9%, respectively, at 90 to 180 days. Major bleeding (6.3%) and renal failure (3.9%) readmission rates peaked at 8 to 30 days post-index discharge. For cardiac causes, at the early time point of 0 to 7 days, the rate of AMI was 27.9%, whereas for heart failure it was 15.6%. These rates for AMI decreased to 18.7% but increased for heart failure to 26.3% between 8 to 30 days.
FIGURE 4. Rate of Noncardiac Unplanned Readmissions at Different Time Points.
Increase in noncardiac unplanned readmissions with increasing time after discharge.
TABLE 4.
Noncardiac and Cardiac Causes of Readmissions at Different Time Periods After Index Discharge for Percutaneous Coronary Intervention
| Readmission Between 0 and 7 Days |
Readmission Between 8 and 30 Days |
Readmission Between 31 and 90 Days |
Readmission Between 90 and 180 Days |
|
|---|---|---|---|---|
| Noncardiac causes for readmission | ||||
| Nonspecific chest pain | 22.7 | 15.6 | 12.5 | 12.0 |
| Gastrointestinal | 10.7 | 10.8 | 11.4 | 11.9 |
| Infections | 8.4 | 12.0 | 13.4 | 12.9 |
| Respiratory | 6.4 | 8.6 | 8.6 | 7.6 |
| TIA/stroke | 5.4 | 4.1 | 4.7 | 5.4 |
| Peripheral vascular disease | 4.2 | 4.4 | 3.8 | 3.2 |
| Bleeding | 3.6 | 6.3 | 5.2 | 4.5 |
| Renal failure | 2.6 | 3.9 | 3.6 | 2.8 |
| Genitourinary | 2.6 | 2.9 | 3.4 | 3.6 |
| Neuropsychiatric | 2.3 | 2.5 | 2.9 | 3.5 |
| Trauma | 1.9 | 2.4 | 4.3 | 5.7 |
| Hematological/neoplasm | 1.7 | 3.3 | 4.2 | 3.8 |
| Endocrine/metabolic | 1.3 | 2.9 | 3.4 | 3.1 |
| Other noncardiac causes | 26.1 | 20.4 | 18.5 | 19.9 |
| Cardiac causes for readmission | ||||
| Coronary artery disease including angina | 39.3 | 36.8 | 38.3 | 41.2 |
| Acute myocardial infarction | 27.6 | 16.3 | 17.4 | 24.1 |
| Heart failure | 15.6 | 26.3 | 24.0 | 17.2 |
| Arrhythmias | 12.5 | 15.3 | 16.1 | 14.4 |
| Other cardiac causes | 5.1 | 5.2 | 4.2 | 3.0 |
Values are %.
TIA = transient ischemic attack.
FIGURE 5. Causes of Unplanned Readmissions at Different Time Points.
Causes of unplanned readmissions at different time points. TIA = transient ischemic attack.
DISCUSSION
This large retrospective analysis demonstrates that approximately 25% of patients who undergo PCI had unplanned readmissions within 6 months. The time point at which patients are at greatest risk is at 7 days post-discharge, with the majority of unplanned readmissions occurring within 30 days. Thereafter, the daily rate of unplanned readmissions declines over time. In addition, the causes of readmission vary depending on the time periods of readmission, with noncardiac chest pain as an important cause at early time points and gastrointestinal bleeding and infections more important at longer time points (91 to 180 days). For cardiac causes of readmission, readmissions for AMI are highest 0 to 7 days post-discharge, whereas for heart failure the peak is at 8 to 30 days post-discharge.
These results have differences and similarities to a recent 2-center study reporting the incidence and causes of rehospitalization within 1 year after PCI in 17,111 patients in Denmark (16). First, although the investigators reported a higher 1-year readmission rate of 50.4%, this included planned staged procedures. The investigators also reported that the majority of readmissions occurred within the first month, whereas the present study suggests that it actually peaks in the first 7 days. Second, at 1 year the most common cause of readmission in Denmark was either AMI or angina or chest pain (49.7%), and the second most common cause of readmission was heart failure (5.5%). In contrast, in the present study, the most common cause of readmission varied according to the time period evaluated, although noncardiac causes were consistently more prevalent at all time periods studied. The Danish study may reflect that noncardiac diagnoses are more likely to be managed by primary care, whereas in the United States they are more likely to present in the emergency department, likely because of less developed primary care services. Third, the present study had a far larger sample size that is reflective of the whole country rather than 2 centers, with more demographic, comorbidity, hospital, and procedural variables, so it is not surprising that we identified additional strong predictors, including chronic lung disease, renal failure, liver disease, anemia, cancer, and discharge to another hospital or nursing facility or discharge against medical advice. Finally, we evaluated rates of readmissions following diagnosis of acute ischemic syndrome and stable ischemic heart diseases within time periods, whereas the Danish study reported cumulative rates with survival curves.
We observed differences in readmission rates comparing patients who had diagnoses of AMI and patients without diagnoses of AMI, and interestingly, after adjustments, there was an increased odds ratio for readmission for patients with AMI in the early follow-up period (0 to 7 days). Patients presenting with acute coronary syndromes tend to be older, to be more comorbid, and to have more complex disease, which are independent predictors of unplanned readmissions (17). Patients presenting with acute coronary syndrome have a higher incidence of complications, which may also contribute to the higher rate of unplanned readmissions. Data from the NOBORI-2 study suggest that patients with acute coronary syndromes have double the major adverse cardiovascular events at 180 days compared with stable angina (17). Similarly, data derived from the CathPCI Registry suggest that major bleeding complications were significantly greater in patients undergoing PCI for acute coronary syndromes compared with elective patients (18), with similar findings reported for acute kidney injury and requirement for dialysis (19). We have previously shown that both ischemic and hemorrhagic stroke complications occur between 2 and 5 times more commonly in patients with acute coronary syndromes compared with elective patients (20). Finally, presentation with acute coronary syndromes is associated with an increased risk for heart failure readmission post-discharge, and recent data from the nationwide readmission dataset suggest that this may be as high as 13.9% in patients with ST-segment elevation myocardial infarction (21). We observed that gastrointestinal causes for readmissions are common and increase in rate over time. Dyspepsia may mimic symptoms of heart disease. Studies have suggested that gastroesophageal reflux disease is twice as common in patients with coronary heart disease compared with the general population (22). At the same time, the DAPT administered to patients may cause or exacerbate dyspepsia (23). Use of proton pump inhibitors may reduce some of these gastrointestinal-related readmissions.
A common complication following PCI is bleeding related to DAPT, with gastrointestinal bleeding among the most common. The ADAPT-DES (Assessment of Dual Antiplatelet Therapy With Drug Eluting Stents) study suggests that gastrointestinal bleeding was the most common source of post-discharge bleeding after PCI (24). Our study reveals that bleeding causing hospitalization peaks at 8 to 30 days and declines with time despite DAPT that may last for up to 1 year. This may relate to the fact that many bleeds occurring at later time points may be nuisance bleeds that do not require hospital readmission or are fatal bleeds that do not survive to hospital readmission. It is not clear the extent to which these types of bleeding episodes could have been prevented, although there may be a potential role for gastrointestinal prophylaxis in PCI, as observational studies have suggested that fewer than one-half of patients with acute coronary syndromes at high risk for bleeding on DAPT are provided with gastrointestinal prophylaxis (25).
Readmission risk could be assessed using risk scores (26) and high-risk subjects scheduled for early follow-up. As noncardiac readmissions remain prevalent beyond 90 days, clinicians should consider appropriate referral to hospital specialists or community care for continuing care of comorbid conditions, with close liaison with primary care. Many patients who undergo PCI are comorbid, and these comorbidities drive readmissions.
The only intervention to date that has been shown to reduce readmissions after PCI has used short video-based patient education materials that specifically target heart failure and chest discomfort (14). The videos described in the study by Tanguturi et al. (14) provided education regarding the different types of chest discomfort, how to contact cardiologists by phone to evaluate low-risk symptoms, how to use nitroglycerin to treat angina, the role of anxiety after PCI, and information about heart failure symptoms after PCI. According to the investigators, these videos are provided as web-based links in discharge instructions, which allows patients to view the videos as often as needed. Our present study supports such interventions, as nonspecific chest pain is a common noncardiac cause of unplanned readmission between 0 and 7 days, and heart failure is a major cause of readmissions between 8 and 90 days. There are also admission avoidance strategies such as notification systems in the emergency department, which flag patients who return to the hospital who have been recently admitted to the hospital. The use of an automated notification system has been shown to reduce readmission rates from 14% to 12% (27) through rapid assessment by the cardiac team, leading to fewer rehospitalizations after PCI for low-risk patients (14). In addition, there are also other measures that may be implemented to reduce readmissions such as the use of a discharge toolkit (28), multifaceted interventions to improve medication adherence (29), programs to reduce medication errors (30), and the increased role of pharmacists and social workers (31).
STUDY LIMITATIONS.
First, the NRD is constructed in a format that precludes linkage of between years, so it is possible that the same patient appears in more than 1 year, and it is not possible to follow patients across years.
Secondly, because of the nature of the annualized data, each patient could have a maximum follow-up duration of only 1 year, with the numbers at risk decreasing with time.
Third, the NRD is not designed to allow determination of regional variations within the dataset, and our results may be generalizable only to the U.S. health care system.
Fourth, we excluded patients admitted during the month of December, and there were further exclusions for the last 6 months of the year, so seasonal effects may not be captured. One of the limitations of using administrative data is uncertainty in classification of nonspecific chest pain as a reason for readmission. This code is derived from codes for chest pain, unspecified, precordial pain, and other chest pain, and in the present analysis it was classified as noncardiac. Although there is the potential that the pain coded using these terms may potentially have been cardiac in origin, we are unable to explore this further. In addition, the present dataset is further limited because it lacks outpatient PCI procedures and represents only hospital admissions.
Finally, as with any observational data, it would be incorrect to make causal inferences with the data, and there are the limitations related to unmeasured confounders.
CONCLUSIONS
We show that readmissions after PCI are common, occurring in 1 in 4 of patients, with the highest risk for readmissions at 7 days post-procedure. The time period when there are the most readmissions is up to 30 days. Although there is a decline in readmissions beyond 30 days, readmissions related to noncardiac causes increase. The most common cause for readmission in the early period is noncardiac chest pain. Other important causes for readmissions include heart failure, gastrointestinal disease, and infections. Any interventions developed to reduce unplanned readmissions should consider the important differences in causes of readmission at different time points after PCI.
Supplementary Material
PERSPECTIVES.
WHAT IS KNOWN? The rates and causes of readmission at different time periods after PCI remain incompletely elucidated.
WHAT IS NEW? Our analysis of 2,412,000 patients reveals that approximately 25% of patients who underwent PCI had unplanned readmissions within 6 months, and the time point at which patients are at greatest risk is at 7 days post-discharge, with the majority of unplanned readmissions occurring within 30 days. For cardiac causes of readmission, readmissions for AMI are highest 0 to 7 days post-discharge, whereas for heart failure the peak is at 8 to 30 days post-discharge.
WHAT IS NEXT? Any interventions developed to reduce unplanned readmissions should consider the important differences in causes of readmission at different time points after PCI.
ACKNOWLEDGMENTS
The authors are grateful to the Healthcare Cost and Utilization Project and the Healthcare Cost and Utilization Project Data Partners for providing the data used in the analysis.
This study was supported by a grant from the Research and Development Department at the Royal Stoke Hospital. This work is conducted as a part of a PhD for Dr. Kwok, which is supported by Biosensors International. All other authors have reported that they have no relationships relevant to the contents of this paper to disclose.
ABBREVIATIONS AND ACRONYMS
- AMI
acute myocardial infarction
- DAPT
dual-antiplatelet therapy
- ICD-9
International Classification of Disease-9th Revision
- NRD
Nationwide Readmission Database
- PCI
percutaneous coronary intervention
Footnotes
APPENDIX For supplemental tables and a figure, please see the online version of this paper.
REFERENCES
- 1.Stuntz M, PaLak A. Recent trends in percutaneous coronary intervention volume in the United States. Value Health 2016;19:A347. [Google Scholar]
- 2.Stathopoulos I, Jimenez M, Panagopoulos G, et al. The decline in PCI complication rate: 2003–2006 versus 1999–2002. Hellenic J Cardiol 2009;50:379–87. [PubMed] [Google Scholar]
- 3.Valle JA, Smith DE, Booher AM, Menees DS, Gurm HS. Cause and circumstance of in-hospital mortality among patients undergoing contemporary percutaneous coronary intervention. Circ Cardiovasc Qual Outcomes 2012;5:229–35. [DOI] [PubMed] [Google Scholar]
- 4.Kwok CS, Rao SV, Potts JE, et al. Burden of 30-day readmissions after percutaneous coronary intervention in 833,344 patients in the United States: predictors, causes, and cost: insights from the Nationwide Readmissions Database. J Am Coll Cardiol Intv 2018;11:665–74. [DOI] [PubMed] [Google Scholar]
- 5.Kwok CS, Rao SV, Gilchrist I, et al. Relation between age and unplanned readmissions after percutaneous coronary intervention (findings from the Nationwide Readmission Database). Am J Cardiol 2018;122:220–8. [DOI] [PubMed] [Google Scholar]
- 6.Kwok CS, Potts J, Gulati M, et al. Effect of gender on unplanned readmissions after percutaneous coronary intervention (from the Nationwide Readmission Database). Am J Cardiol 2018;121:810–7. [DOI] [PubMed] [Google Scholar]
- 7.HoLdfieLd NI, McCullough E, Hughes JS, et al. Identifying potentially preventable readmissions. Health Care Financ Rev 2008;30:75–91. [PMC free article] [PubMed] [Google Scholar]
- 8.Halfon P, Eggli Y, Pretre-Rohrbach I, Meylan D, Marazzi A, Burnand B. Validation of the potentially avoidable hospital readmission rate as a routine indicator of the quality of hospital care. Med Care 2006;44:972–81. [DOI] [PubMed] [Google Scholar]
- 9.Kwok CS, Hulme W, OLier I, Holroyd E, Mamas MA. Review of early hospitalisations after percutaneous coronary intervention. Int J Cardiol 2017;227:370–7. [DOI] [PubMed] [Google Scholar]
- 10.Kwok CS, Rao SV, Myint PK, et al. Major bleeding after percutaneous coronary intervention and risk of subsequent mortality: a systematic review and meta-analysis. Open Heart 2014;1:e000021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kwok CS, Khan MA, Rao SV, et al. Access and non-access site bleeding after percutaneous coronary intervention and risk of subsequent mortality and major adverse cardiovascular events: systematic review and meta-analysis. Circ Cardiovasc Interv 2015;8:e001645. [DOI] [PubMed] [Google Scholar]
- 12.Patient Protection and Affordable Care Act, Public Law No. 111–148 (2010).
- 13.Centers for Medicare and Medicaid Services. Bundled Payments for Care Improvement Advanced (BPCI Advanced) voluntary bundled payment model. Available at: https://www.cms.gov/newsroom/fact-sheets/bundled-payments-care-improvement-advanced-bpci-advanced-voluntary-bundled-payment-model. Accessed February 16, 2019.
- 14.Tanguturi VK, Temin E, Yeh RW, et al. Clinical interventions to reduce preventable hospital readmission after percutaneous coronary intervention. Circ Cardiovasc Qual Outcomes 2016;9:600–4. [DOI] [PubMed] [Google Scholar]
- 15.Agency for Healthcare Research and Quality. Healthcare Cost and Utilization Project. Available at: https://www.ahrq.gov/research/data/hcup/index.html. Accessed February 16, 2019. [PubMed]
- 16.Hansen KN, Bendix K, Antonsen L, et al. One-year rehospitalization after percutaneous coronary intervention: a retrospective analysis. Euro-Intervention 2018;14:926–34. [DOI] [PubMed] [Google Scholar]
- 17.Fath-Ordoubadi F, Spaepen E, El-Omar M, et al. Outcomes in patients with acute and stable coronary syndromes; insights from the prospective NOBORI-2 study. PLoS ONE 2014;9:e88577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rao SV, Dai D, Subherwal S, et al. Association between periprocedural bleeding and long-term outcomes following percutaneous coronary intervention in older patients. J Am Coll Cardiol Intv 2012;5:958–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tsai TT, Patel UD, Chang TI, et al. Contemporary incidence, predictors, and outcomes of acute kidney injury in patients undergoing percutaneous coronary interventions: insights from the NCDR Cath-PCI registry. J Am Coll Cardiol Intv 2014;7:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kwok CS, Kontopantelis E, Myint PK, et al. Stroke following percutaneous coronary intervention: type-specific incidence, outcomes and determinants seen by the British Cardiovascular Intervention Society 2007–12. Eur Heart J 2015;36:1618–28. [DOI] [PubMed] [Google Scholar]
- 21.Kim LK, Yeo I, Cheung JW, et al. Thirty-day readmission rates, timing, causes and costs after ST-elevation myocardial infarction in the United States: a national readmission database analysis 2010–2014. J Am Heart Assoc 2018;7:e009863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pulkowski G, Majer M, Budzynski J, Swiatkowski M. Gastroesophageal reflux disease and coronary heart disease—coexistence or inter-relationship? Pol Merkur Lekarski 2006;20:104–8. [PubMed] [Google Scholar]
- 23.Serebruany VL, Dinicolantonio JJ, Can MM, Pershukov IV, Kuliczkowski W. Gastrointestinal adverse events after dual antiplatelet therapy: clopidogrel is safer than ticagrelor, but prasugrel data are lacking or inconclusive. Cardiology 2013; 126:35–40. [DOI] [PubMed] [Google Scholar]
- 24.Généreux P, Giustino G, Witzenbichler B, et al. Incidence, predictors, and impact of post-discharge bleeding after percutaneous coronary intervention. J Am Coll Cardiol 2015;66:1036–45. [DOI] [PubMed] [Google Scholar]
- 25.Badar A, Scaife J, Yan AT, et al. Provision of gastroprotective medications and bleeding risk following acute coronary syndrome. J Invasive Cardiol 2013;25:397–401. [PubMed] [Google Scholar]
- 26.Kansagara D, Englander H, Salanitro A, et al. Risk prediction models for hospital readmission: a systematic review. JAMA 2011;306:1688–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bell H, Povilus J, Yarbrough PM. The use of automated notification system to identify and address early readmission by university hospital service. Hosp Pract 2015;43:70–3. [DOI] [PubMed] [Google Scholar]
- 28.Adams CJ, Stephens K, Whiteman K, Kersteen H, Katruska J. Implementation of the Re-Engineered Discharge (RED) toolkit to decrease all-cause readmission rates at a rural community hospital. Qual Manag Health Care 2014;23:169–77. [DOI] [PubMed] [Google Scholar]
- 29.Ho PM, Lambert-Kerzner A, Carey EP, et al. Multifaceted intervention to improve medication adherence and secondary prevention measures after acute coronary syndrome hospital discharge: a randomized clinical trial. JAMA Intern Med 2014;174:186–93. [DOI] [PubMed] [Google Scholar]
- 30.Kripalani S, Roumie CL, Dalal AK, et al. for the PILL-CVD (Pharmacist Intervention for Low Literacy in Cardiovascular Disease) Study Group. Effect of a pharmacist intervention on clinically important medication errors after hospital discharge: a randomized trial. Ann Intern Med 2012;157:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gil M, Mikaitis DK, Shier G, Johnson TJ, Sims S. Impact of a combined pharmacist and social worker program to reduce hospital readmissions. J Manag Care Pharm 2013;19:558–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.