Sir,
We report the case of a 65-year-old male patient, who presented with pleuritic and chest pain, cough, and fever for 2 weeks. On physical examination, vital signs were normal. Pulse oximetry was 98% on room air at rest. On auscultation, decreased breath sounds were noted at the left lung base. Chest radiographs showed a moderate left pleural effusion with clear lung parenchyma. Left-sided thoracocentesis yielded 85 ml of thick, cloudy, white fluid. Laboratory data included a positive rheumatoid factor: 128 IU/ml (normal 0–20); antinuclear antibody, antimyeloperoxidase, and antiproteinase 3 were all negative. The C-reactive protein was 18.57 mg/l. The white blood cells in the peripheral blood were 8.27 × 103μl with 1.7% of the cells being eosinophils. Pleural fluid contained 3490 white blood cells/mm3 with 18% segmented cells and 82% lymphocytes and monocytes. The pleural fluid analysis revealed a pleural fluid lactate dehydrogenase of 11181.00 U/l, glucose 5 mg/dl, and a pH of 7.4. Pleural fluid and blood cultures for bacteria, fungus, and mycobacteria were negative. Real-time polymerase chain reaction (PCR) for mycobacteria tuberculosis was also negative.
Microscopic examination
Microscopic examination of the pleural fluid revealed a characteristic picture of degenerating polymorphs with amorphous extracellular material, numerous macrophages, and epithelioid cells, many of which were multinucleate.[1] Effusions associated with rheumatoid arthritis (RA) have pathognomonic cytologic features that allow the cytopathologist to make a specific diagnostic with such an accuracy that the diagnosis of rheumatic disease in an effusion, at times, may even antedate the onset of the arthritis.[1,2] Cytologic picture [Figure 1] of rheumatoid pleuritis comprises three main patterns: large slender or elongated macrophages, round or spindle giant multinucleated cells, and a background of amorphous granular material.[3]
Figure 1.
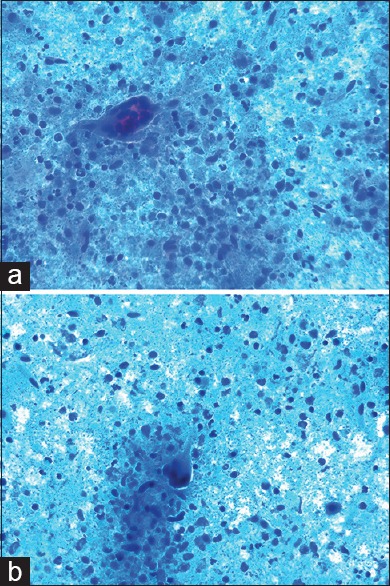
(a) Giemsa smear of pleural fluid with a giant multinucleated macrophage and amorphous granular background material (×400). (b) Cytologic findings from the patient's pleural fluid, including spindle and multinucleated giant cells (Giemsa, ×400)
The necrotic exudate is formed by cells debris, derived from the necrobiotic core of the rheumatoid nodule-like granulomas, and may contain numerous visible necrotic cells that can impart appearance of a purulent effusion.[1,2,3]
Differential diagnosis
The characteristics of the pleural effusion of RA may mimic those of the infected para-pneumonic effusion, a condition that is treated optimally with thoracic drainage and antibiotics. (In fact, patients with RA have an increased risk of developing major infections.)[4] Tuberculosis was also included in the differential diagnosis in this case; however, the radiological picture of our patient is not typical of tuberculosis, and was not identified in the PCR, Ziehl–Neelsen, and culture. The biochemical characteristics of the pleura fluid thus suggested rheumatoid pleural effusion, and cytology confirmed the diagnosis. The emergence of a new therapy for RA makes it imperative also to rule out tuberculosis in patients with RA and a pleural effusion with lymphocytic predominance.
Short discussion
RA affects the pleura in up to 5% of cases and, in keeping with other extraarticular manifestations of the disease, is more common in men. Rheumatoid effusions characteristically have a low glucose and pH. If the pleural fluid glucose is >28.8 mg/dl, rheumatoid is an unlikely cause. Nonsteroidal antiinflammatory drugs can be used, and one case report supports the use of intrapleural corticosteroids in resistant cases. The cytologic examination of such effusions can be diagnostic of the underlying disease; this is of great clinical significance when the rheumatoid condition has not been diagnosed prior to the pleural involvement.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Geisinger KR, Stanley MW, Raab SS, Silverman JF, Abati A. Effusions. In: Churchill Livingstone., editor. Modern cytopathology. Philadelphia: 2003. pp. 270–1. [Google Scholar]
- 2.Komarla A, Yu GH, Shahane A. Pleural effusion, pneumothorax, and lung entrapment in rheumatoid arthritis. J Clin Rheumatol. 2015;21:211–5. doi: 10.1097/RHU.0000000000000244. [DOI] [PubMed] [Google Scholar]
- 3.Chou CW, Chang SC. Pleuritis as a presenting manifestation of rheumatoid arthritis: Diagnostic clues in pleural fluid cytology. Am J Med Sci. 2002;323:158–61. doi: 10.1097/00000441-200203000-00008. [DOI] [PubMed] [Google Scholar]
- 4.Avnon LS, Abu-Shakra M, Flusser D, Heimer D, Sion-Vardy N. Pleural effusion associated with rheumatoid arthritis: What cell predominance to anticipate? Rheumatol Int. 2007;27:919–25. doi: 10.1007/s00296-007-0322-9. [DOI] [PubMed] [Google Scholar]


