INTRODUCTION
The word calcium is derived from a Latin word “calx or calcis” which means “lime.” Calcium was known as early as the 1stcentury when ancient Romans prepared lime as calcium oxide; however, it was isolated in 1808 by Englishman Sir Humphrey Davy. In 1883, Sydney Ringer demonstrated the biological significance of calcium, when he showed that frog hearts needed the presence of calcium in the bathing solution in order to continue beating.
Calcium as a nutrient is most commonly associated with the formation and metabolism of bone. Over 99% of the total body calcium is found as calcium hydroxyapatite (Ca10[PO4]6[OH]2) in bones and teeth. The rest 1% is intracellular and about 0.1% is in extracellular fluid. Calcium is an important intracellular and extracellular cation, which is required physiologically for muscle contraction, nerve conduction, vascular reactivity, and hormonal secretion. Calcium in plasma or serum exists in the following three forms or fractions: ionized or free calcium (50%), protein-bound calcium (40%), and complexed or chelated calcium which is bound to phosphate, bicarbonate, sulfate, citrate, and lactate (10%).[1]
According to the Institute of Medicine,[1] daily allowance for calcium ranges from 600 to 1300 mg in relation to age and gender. The Indian Council of Medical Research[2] recommends 600 mg for both genders. In the USA and Northern Europe, the average daily intake of calcium is about 900–1000 mg, and in South Asia and India, it is 400–500 mg.[3,4] This means that at both geographical areas, intake of calcium is suboptimal in >50% of population. This also gives impression that these all people require calcium supplementation. If this holds true, then it has huge financial and commercial implications. If more than half of the world's population is calcium deficient, then why we do not observe its consequences often? To address this question, we first discuss the physiological aspects of calcium homeostasis, then discuss about when, which, and how calcium supplementation should be given.
PHYSIOLOGY OF CALCIUM HOMEOSTASIS
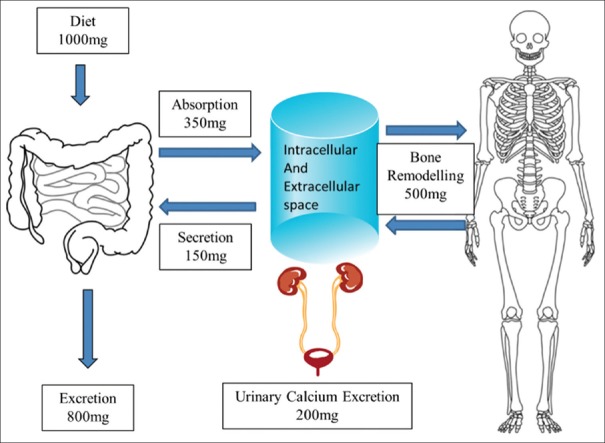
Calcium is absorbed actively in the duodenum through transcellular (active transport – 80%) process which is Vitamin D dependent, whereas passive absorption is a paracellular (passive diffusion – 20%) process which occurs throughout intestine independent of Vitamin D and is dependent on the concentration of calcium in the intestinal tract. The total fraction of calcium absorbed from the total intake can vary from 20% to 80%. In the event of decreased calcium availability from intake, calcium is released from the bone under the effect of Vitamin D–parathyroid hormone (PTH) system to maintain its homeostasis. Calcium excretion is also dependent on calcium balance. Normally, about 98% of filtered calcium is absorbed from the kidney and about 150–250 mg is excreted in urine daily, which is compensated by intestinal calcium absorption or bone resorption. Serum calcium is maintained in narrow range with contribution from calcium absorption, bone remodeling, and calcium excretion [Figure 1].[1]
Figure 1.
Physiology of calcium homeostasis
WHY – CALCIUM SUPPLEMENTATION?
“…. Something that is added to something else in order to improve it or complete it.”
– Cambridge Dictionary
According to the above-stated recommendations, more than half of the world's population will require calcium supplementation. Calcium supplementation is decided by recommended daily allowances. Logically, to maintain calcium homeostasis, first, the body will try to absorb maximum available calcium, rather than affecting bone remodeling. Hence, calcium absorption is the first most important adaptive mechanism. It is well known that fractional calcium absorption (FCA) is inversely proportional to the calcium intake. High FCA (54%–63%) has been reported from the region of China with low calcium intake (<500 mg)[5] compared to 25%–34% among US children with high intake of calcium (>900 mg).[6] There are no such studies reported from India, because this requires double calcium isotopes, which are not available in India. Calcium absorption is mainly facilitated by Vitamin D. The conventional explanation of homeostasis is by systemic adaptation in which decreased calcium intake results in decreased calcium absorption, which leads to increase in PTH levels. The PTH upregulates the 1-α hydroxylase enzyme, leading to increase in the generation of 1,25-dihydroxyvitamin D (1,25(OH)2D) levels and increased calcium absorption. However, calcium absorption can be kept static over a wide range of calcium intake and serum 25OHD levels.[7] Calcium absorption varies between 20% and 70% at the serum 25OHD levels >10 ng/ml[8] and does not increase with higher levels of 25OHD.[9] This suggests that it is the calcium absorptive mechanism, rather than dietary calcium intake, will decide the adequacy of calcium homeostasis. An alternative hypothesis has been proposed, wherein the adaptation of calcium absorption occurs at the level of intestine called “intestinal calcistat.”[10,11] This “calcistat” senses the calcium intake or available calcium in the gastrointestinal (GI) tract and regulates the generation of active Vitamin D in intestinal cells to adjust FCA. With daily calcium intake of <500 mg, the FCA is about 60%–80%, which can easily supply the daily needs of calcium, i.e., 200 mg. In contrast, with daily calcium intake of >900 mg, FCA is about 25%–35% to maintain calcium homeostasis.
According to the above discussion, about 400–500 mg of elemental calcium daily should be able to meet daily requirement. The average daily intake of calcium in India ranges from 200 to 600 mg among various studies. This suggests that those with low calcium intake should either increase calcium intake by modifying their diet or take calcium supplements.
WHICH – DIET VERSUS CALCIUM SUPPLEMENTATION?
The American Association of Clinical Endocrinologists (2016) guideline recommends that calcium intake among adults aged 50 years and older (including diet, plus calcium supplements, if necessary, if dietary intake is insufficient) should be 1200 mg/day.[12] The United States Preventive Task Force (USPTF) concludes that the current evidence is insufficient to assess the balance of the benefits and harms of combined Vitamin D and calcium supplementation. It recommends against daily supplementation of more than 1000 mg of calcium.[13]
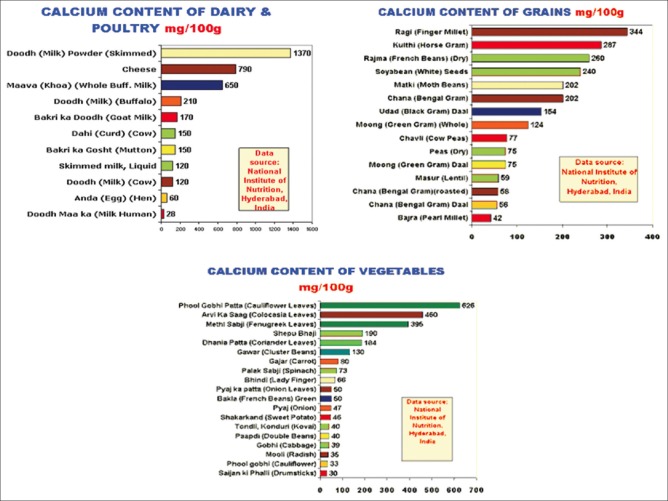
The main sources of calcium are dairy products such as milk, curd, and cheese. Other foods such as grains, legumes, fruits, and vegetables also contribute to calcium intake (Figure 2, National Institute of Nutrition, Hyderabad, at fitjog.com). It will be desirable to increase calcium intake through modification of diet. Daily intake of two glasses of milk or curd with enough pulses can meet the calcium requirement of body without the need for any dietary supplementation.
Figure 2.
Dietary contents of calcium
Many calcium supplements are available in Indian markets [Table 1]. Calcium is available as carbonate, citrate, acetate, phosphate, lactate, and gluconate, with varying concentrations of ionic calcium contents as summarized in Table 1.
Table 1.
Calcium Supplements
| Preparation | Calcium (%) | Calcium (mg/g) |
|---|---|---|
| Calcium carbonate (Shelcal) | 40 | 400 |
| Calcium phosphate (Ostocalcium) | 38 | 383 |
| Calcium citrate (Ucal) | 21 | 210 |
| Calcium acetate (Eliphos®) | 25 | 253 |
| Calcium lactate (Decal) | 13 | 130 |
| Calcium gluconate (Calcium Sandoz) | 9 | 93 |
HOW – CALCIUM SUPPLEMENTATION?
Calcium carbonate is the least expensive and requires the fewest tablets. However, it may cause constipation and bloating and must be taken with meals for adequate absorption. Calcium citrate is often more expensive than calcium carbonate and requires more tablets to get the desired dose. Its absorption is not dependent on gastric acid, and it is less likely to cause GI side effects. For optimal absorption, the dose of calcium should not exceed 500 mg per dose, irrespective of calcium preparation. For patients requiring >500 mg/day, the dose should be divided.
All nutrients have side effects when taken in excess quantity like obesity with excess calories. There are contradictory evidences about increased calcium intake and cardiovascular deaths both from observational studies and meta-analyses.[14,15,16] Previous studies and meta-analyses found no correlation between calcium intake and cardiovascular mortality. A recently published large prospective observational study among Swedish females found a positive relation between calcium intake and cardiovascular death.[16] Increased serum calcium will suppress PTH and also increase serum levels of fibroblast growth factor 23 which is known to be associated with an increased risk of cardiovascular events and all-cause mortality.[17] Increased serum calcium level induces hypercoagulable state and can increase the risk of cardiovascular mortality.[18]
Hence, to conclude, we should not be overenthusiastic to prescribe calcium supplementation to all but be cautious. It should be prescribed after due consideration and diligence to those whose dietary calcium intake is insufficient and can be increased by dietary means due to food intolerance or avoidance.
REFERENCES
- 1.Ross AC, Manson JE, Abrams SA, Aloia JF, Brannon PM, Clinton SK, et al. The 2011 report on dietary reference intakes for calcium and Vitamin D from the institute of medicine: What clinicians need to know. J Clin Endocrinol Metab. 2011;96:53–8. doi: 10.1210/jc.2010-2704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sesikeran B. Jamai-Osmania PO, Hyderabad: National Institute of Nutrition, Indian Council of Medical Research; 2009. Nutritional Requirements and Recommended Daily Allowances for Indians: A Report of the Expert Group of the Indian Council of Medical Research. [Google Scholar]
- 3.Wang Y, Li S. Worldwide trends in dairy production and consumption and calcium intake: Is promoting consumption of dairy products a sustainable solution for inadequate calcium intake? Food Nutr Bull. 2008;29:172–85. doi: 10.1177/156482650802900303. [DOI] [PubMed] [Google Scholar]
- 4.Balk EM, Adam GP, Langberg VN, Earley A, Clark P, Ebeling PR, et al. Global dietary calcium intake among adults: A systematic review. Osteoporos Int. 2017;28:3315–24. doi: 10.1007/s00198-017-4230-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee WT, Jiang J, Hu P, Hu X, Roberts DC, Cheng JC. Use of stable calcium isotopes (42Ca & 44Ca) in evaluation of calcium absorption in Beijing adolescents with low Vitamin D status. Food Nutr Bull. 2002;23:42–7. [PubMed] [Google Scholar]
- 6.Aloia JF, Chen DG, Yeh JK, Chen H. Serum Vitamin D metabolites and intestinal calcium absorption efficiency in women. Am J Clin Nutr. 2010;92:835–40. doi: 10.3945/ajcn.2010.29553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gallagher JC, Jindal PS, Smith LM. Vitamin D does not increase calcium absorption in young women: A randomized clinical trial. J Bone Miner Res. 2014;29:1081–7. doi: 10.1002/jbmr.2121. [DOI] [PubMed] [Google Scholar]
- 8.Abrams SA, Griffin IJ, Hawthorne KM, Gunn SK, Gundberg CM, Carpenter TO. Relationships among vitamin D levels, parathyroid hormone, and calcium absorption in young adolescents. J Clin Endocrinol Metab. 2005;90:5576–81. doi: 10.1210/jc.2005-1021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Christakos S, Lieben L, Masuyama R, Carmeliet G. Vitamin D endocrine system and the intestine. Bonekey Rep. 2014;3:496. doi: 10.1038/bonekey.2013.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Garg MK, Mahalle N. Calcium homeostasis, and clinical or subclinical Vitamin D deficiency – Can a hypothesis of “intestinal calcistat” explain it all? Med Hypotheses. 2013;81:253–8. doi: 10.1016/j.mehy.2013.04.035. [DOI] [PubMed] [Google Scholar]
- 11.Garg MK, Kalra S, Mahalle N. The intestinal calcistat: Determinant of clinical Vitamin D deficiency. Indian J Endocrinol Metab. 2013;17:780–3. doi: 10.4103/2230-8210.117187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Camacho PM, Petak SM, Binkley N, Clarke BL, Harris ST, Hurley DL, et al. American association of clinical endocrinologists and American college of endocrinology clinical practice guidelines for the diagnosis and treatment of postmenopausal osteoporosis – 2016. Endocr Pract. 2016;22:1–42. doi: 10.4158/EP161435.GL. [DOI] [PubMed] [Google Scholar]
- 13.Moyer VA. U.S. Preventive Services Task Force*. Vitamin D and calcium supplementation to prevent fractures in adults: U.S. Preventive services task force recommendation statement. Ann Intern Med. 2013;158:691–6. doi: 10.7326/0003-4819-158-9-201305070-00603. [DOI] [PubMed] [Google Scholar]
- 14.Li K, Kaaks R, Linseisen J, Rohrmann S. Associations of dietary calcium intake and calcium supplementation with myocardial infarction and stroke risk and overall cardiovascular mortality in the Heidelberg Cohort of the European Prospective Investigation into Cancer and Nutrition Study (EPIC-heidelberg) Heart. 2012;98:920–5. doi: 10.1136/heartjnl-2011-301345. [DOI] [PubMed] [Google Scholar]
- 15.Bolland MJ, Grey A, Avenell A, Gamble GD, Reid IR. Calcium supplements with or without Vitamin D and risk of cardiovascular events: Reanalysis of the women's health initiative limited access dataset and meta-analysis. BMJ. 2011;342:d2040. doi: 10.1136/bmj.d2040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Michaëlsson K, Melhus H, Warensjö Lemming E, Wolk A, Byberg L. Long term calcium intake and rates of all cause and cardiovascular mortality: Community based prospective longitudinal cohort study. BMJ. 2013;346:f228. doi: 10.1136/bmj.f228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Faul C, Amaral AP, Oskouei B, Hu MC, Sloan A, Isakova T, et al. FGF23 induces left ventricular hypertrophy. J Clin Invest. 2011;121:4393–408. doi: 10.1172/JCI46122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Reid IR, Bolland MJ, Avenell A, Grey A. Cardiovascular effects of calcium supplementation. Osteoporos Int. 2011;22:1649–58. doi: 10.1007/s00198-011-1599-9. [DOI] [PubMed] [Google Scholar]