ABSTRACT
A 45-year-old white male noticed on awakening the painless loss of inferior vision in the left eye 2 days ago. He was otherwise well and his medical history was unremarkable. Visual acuity was 20/20 in OD and 20/32 in OS with a left inferior altitudinal defect and right blind spot enlargement demonstrable on visual field test. On fundus examination, both disc margins were blurred and the left disc was diffusely oedematous, with linear haemorrhages in the adjacent nerve fibre layer. Radiologic imaging and laboratory tests were unremarkable. Bilateral optic nerve head drusen (ONHD) was demonstrated by optical coherence tomography and fundus autofluorescence imaging. Unilateral acute non-arteritic anterior ischemic optic neuropathy (NAION) and concomitant bilateral ONHD were diagnosed. NAION may develop secondary to ONHD. Therefore, clinicians should be aware of this rare association and inform the patients about this risk. Patients with ONHD should be followed-up periodically in terms of possible ischemic complications.
KEYWORDS: Fundus autofluorescence, ischemic optic neuropathy, optical coherence tomography, optic nerve head drusen
Introduction
Non-arteritic anterior ischemic optic neuropathy (NAION) is the most common acquired primary optic neuropathy in individuals over the age of 50.1 Factors which predispose certain eyes to develop NAION have been recognized. The primary risk factor for NAION appears to be a small-crowded optic disc. Suggested additional identified factors associated with NAION include atherosclerotic vascular disease, diabetes mellitus, hypertension, hyperlipidemia, obesity and use of specific medications such as phosphodiesterase 5 inhibitors.1–4 It has been suggested that NAION arise as a consequence of the obstruction of the axoplasmic flow due to the ischemia. NAION has been reported in cases, some relatively young, with optic nerve head drusen (ONHD). Herein, we report on a young white-male who had bilateral ONHD and developed unilateral NAION.
Case report
A 45-year-old man was admitted to our neuro-ophthalmology clinic with complaint of left blurred vision. His complaint commenced suddenly two days ago. He was receiving no medications and he did not have any habits such as smoking or drinking alcohol and had no history of recent infectious or toxic exposure. His family history was unremarkable and medical history revealed no preexisting systemic diseases. On admission, he was conscious and oriented. The patient’s body temperature was normal. His blood pressure was 125/75 mm Hg, with a regular pulse of 72 beats/min. A neurological examination gave normal results. On neuro-ophthalmological examination, external, motility gave normal results. His pupils were sluggish, with a marked left relative afferent defect. Colour vision was assessed by Ishihara pseudoisochromatic test. Right and left eyes were 15/15 and 8/15, respectively. Best corrected visual acuities (BCVA) were 20/20 in OD and 20/32 in OS. Cycloplegic refraction were + 0.25 diopters OU. Slit-lamp examination was unremarkable OU. Intraocular pressure by applanation was 13 mmHg in each eye. We observed bilateral blurred optic disc margins with left disc oedema with splinter hemorrhages in adjacent nerve fibre layer (Figure 1A). Fundus autofluorescence (FAF) image detected “hyperautofluorescence” appearance associated with superficial drusen in the nasal side of right disc and inferior side of left disc (Figure 1B). Optical coherence tomography (OCT) revealed a “lumpy-bumpy” internal contour appearance at the optic disc (Figure 1C). Visual field analysis using by computerized automatic perimetry showed an inferior altitudinal defect in left eye and blind spot enlargement in the right eye (Figure 2). Laboratory parameters including blood cell counts, erythrocyte sedimentation rate, C-reactive protein level, assays for antiphospholipid antibodies (lupus anticoagulant (LA)), antinuclear antibody (ANA), antineutrophil cytoplasmic antibody (ANCA) and antidouble-stranded DNA (anti-dsDNA), coagulation parameters [bleeding time, prothrombin time (PT), activated partial thromboplastin time (aPTT), anti-thrombin III, protein C and S] were within normal ranges. Methylene-tetrahydrofolate reductase (MTHFR), factor V Leiden mutation and plasminogen activator inhibitor 1(PAI-1) analyses were negative. Brain MRI and CT scans of head and orbits were considered normal. However, orbital CT scan showed calcification in both optic nerve heads (Figure 3). A diagnosis of NAION was made. He was treated with 100 mg of acetylsalicylic acid and 80 mg of prednisone a day by mouth, which was tapered over 2 weeks period. Four weeks later his visual function was partially improved although disc margin was blurred. His visual function improved 20/25 in OS at the last visit.
Figure 1.
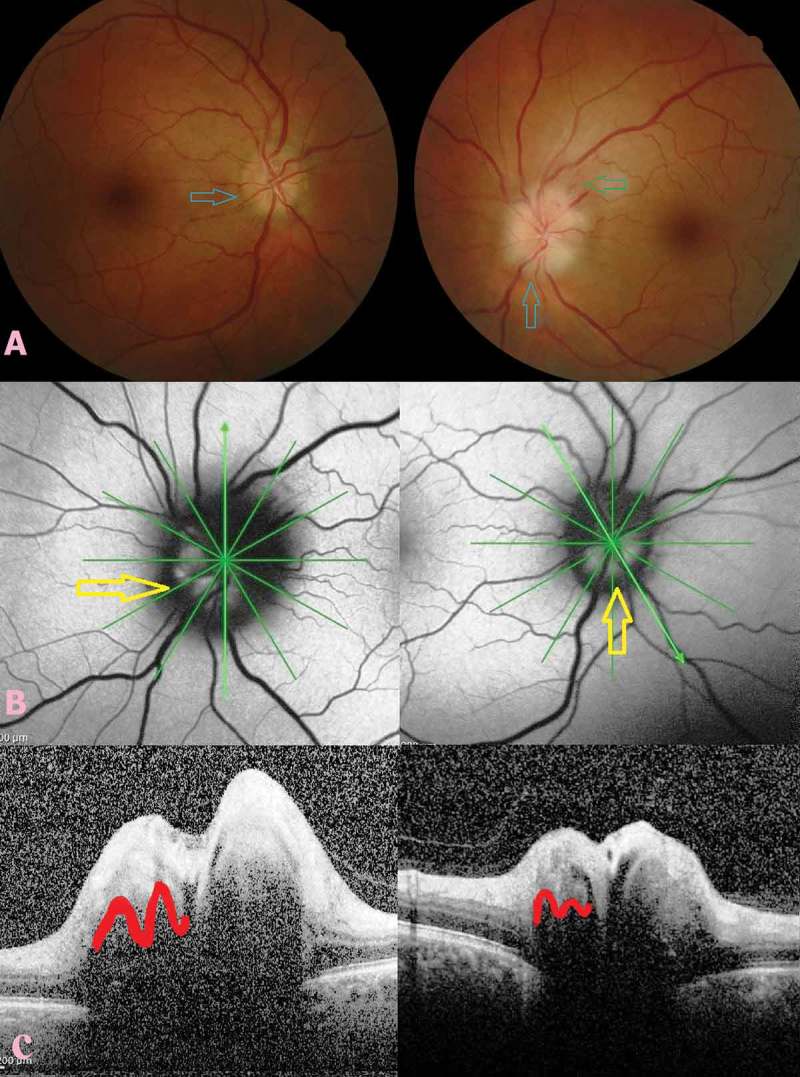
Fundus picture, fundus autofluorescence (FAF) image and spectral-domain optical coherence tomography (SD-OCT) findings of optic nerve head drusen (ONHD). Fundus picture showing bilateral blurred optic disc margins with left disc oedema with splinter hemorrhages in adjacent nerve fibre layer (green arrow) and ONHD appearance in the nasal side of the right disc and inferior side of the left disc (blue arrows) (A). FAF image showing “hyperautofluorescence” appearance in the nasal side of the right disc and inferior side of the left disc (yellow arrows) (B). SD-OCT image showing a “lumpy-bumpy” internal contour appearance at the optic disc in both eyes (red contours) (C).
Figure 2.
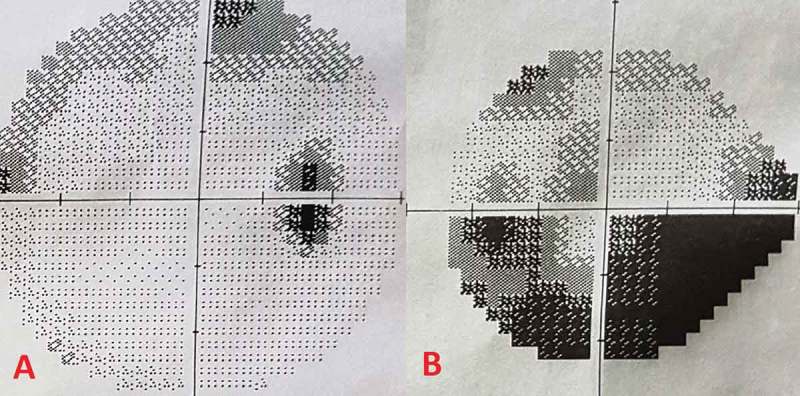
Visual field showing blind spot enlargement in the right eye (A) and inferior altitudinal defect in the left eye (B).
Figure 3.

Computed tomography scan of optic nerve head showing calcification of the optic disc in both eyes (red arrows).
Discussion
ONHD consists of calcified aggregates of extracellular materials that accumulate as a consequence of alterations in axoplasmic transport at the disc. The incidence in the general population varies from 0.4–2.4%.4–8 Involvement is bilateral in 75–86% of cases, but is usually asymmetric.7 It is known that ONHD may occur alone without any other ocular disease. ONHD has also been reported in certain syndromes including retinitis pigmentosa, Usher, Joubert and Alagille.8,9 ONHD is commonly seen together with anomalous vascular patterns including an increased number of arterial and venous branches, presence of shunt vessels between choroid and retinal circulation, and increased capillarity on the disc.10 Most cases are usually asymptomatic and the diagnosis is often established during routine eye examination as an incidental fundus finding. However, transient visual obscuration may happen in cases with ONHD due to transient ischemia of the optic nerve head. It is suggested that increased optic disc tissue pressure may cause temporary impairment of circulation of the disc.11,12 Patients with ONHD may also experience visual field loss such as enlarged blind spot, arcuate defects and peripheral depression, which is usually not noticed by the patient. Visual field loss is usually slowly progressive in nature and is thought to be the direct result of axonal compression. Though quite rare, NAION, central retinal artery and vein occlusion have been reported to occur in cases with ONHD.13–21 The exact mechanism by which ONHD causes NAION is uncertain. By tightening the disc space drusen can increase the susceptibility to optic nerve head ischemia. To best of our knowledge, there are approximately 10 reports published to examine this association. However, most of these reports are not recent.13–20 The recent published cases have additional risk factors such as diabetes mellitus that could cause NAION apart from ONHD.21 It is therefore very difficult to directly associate ONHD with NAION. Our report has two contributions to the literature. First, ONHD is documented in detail by using recent techniques. Second, our case had no known systemic risk factors that could cause NAION except for the ONHD. Therefore, it can be directly associated with NAION unlike other presented cases. Our medical treatment consisted of systemic steroid and acetylsalicylic acid for this case. Firm evidence is lacking about the corticosteroid efficacy on visual function. Mild improvement noted in our patient can be due to the natural course of the disease other than the treatment effect.
In conclusion, ONHD can mimic disc oedema and can very rarely cause NAION. Clinicians should be aware of this association. In addition, such patients can sometimes have multiple risk factors. Therefore, detailed investigations should be performed in a patient with NAION and concomitant ONHD for possible systemic disorders, even if there are no known risk factors. Finally, patients with ONHD should be followed-up periodically because of possible ischemic disc complications.
Funding Statement
None.
Author contributions
All authors contributed significantly to the creation of this manuscript; each fulfilled criteria as established by the ICMJE.
Declaration of interest
The authors declare that they have no conflict of interest.
Consent from
Authors obtained consent from the patients for publishing the photo.
References
- 1.Karti O, Karti DT, Kilic IH, Gokcay F, Celebisoy N.. Baseline demographics, clinical features, and treatment protocols of 240 patients with optic neuropathy: experiences from a neuro-ophthalmological clinic in the Aegean region of Turkey. Int Ophthalmol. 2017. December 19. doi: 10.1007/s10792-017-0799-5. [DOI] [PubMed] [Google Scholar]
- 2.Pomeranz HD. Erectile dysfunction agents and nonarteritic anterior ischemic optic neuropathy. Neurol Clin. 2017;35(1):17–27. doi: 10.1016/j.ncl.2016.08.007. [DOI] [PubMed] [Google Scholar]
- 3.Hayreh SS, Zimmerman MB. Nonarteritic anterior ischemic optic neuropathy: natural history of visual outcome. Ophthalmology. 2008;115(2):298–305. doi: 10.1016/j.ophtha.2007.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gili P, Flores-Rodriguez P, Yanguela J, Orduna-Azcona J, Martin-Rios MD. Sensitivity and specificity of monochromatic photography of the ocular fundus in differentiating optic nerve head drusen and optic disc oedema: optic disc drusen and oedema. Graefes Arch Clin Exp Ophthalmol. 2013;251(3):923–928. doi: 10.1007/s00417-012-2223-1. [DOI] [PubMed] [Google Scholar]
- 5.Hu K, Davis A, O’Sullivan E. Distinguishing optic disc drusen from papilloedema. BMJ. 2008;337:a2360. doi: 10.1136/bmj.a2360. [DOI] [PubMed] [Google Scholar]
- 6.Perez-Alvarez F, Luque A, Penas A. Bilateral disc drusen as an important differential diagnosis of pseudotumor cerebri. Brain Devel. 2007;29(6):387–388. doi: 10.1016/j.braindev.2006.10.006. [DOI] [PubMed] [Google Scholar]
- 7.Arbabi EM, Fearnley TE, Carrim ZI. Drusen and the misleading optic disc. Pract Neurol. 2010;10(1):27–30. doi: 10.1136/jnnp.2009.200089. [DOI] [PubMed] [Google Scholar]
- 8.Nentwich MM, Maertz J, Rudolph G. Optic disk drusen: historical and up-to-date aspects. Klin Monbl Augenheilkd. 2016;232(3):257–265. doi: 10.1055/s-0042-101554. [DOI] [PubMed] [Google Scholar]
- 9.Megur B, Megur D, Megur U, Reddy S. Anterior ischemic optic neuropathy in association with optic nerve head drusen. Indian J Ophthalmol. 2014;62(7):829–831. doi: 10.4103/0301-4738.138636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Borruat FX, Sanders MD. Vascular anomalies and complications of optic nerve drusen [in French]. Klin Monbl Augenheilkd. 1996;208(5):294–296. doi: 10.1055/s-2008-1035219. [DOI] [PubMed] [Google Scholar]
- 11.Sadun AA, Currie JN, Lessell S. Transient visual obscurations with elevated optic discs. Ann Neurol. 1984;16(4):489–494. doi: 10.1002/ana.410160410. [DOI] [PubMed] [Google Scholar]
- 12.Tan DK, Tow SL. Acute visual loss in a patient with optic disc drusen. Clin Ophthalmol. 2013;7:795–799. doi: 10.2147/OPTH.S42233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Farah SG, Mansour AM. Central retinal artery occlusion and optic disc drusen. Eye. 1998;12(3):480–482. doi: 10.1038/eye.1998.102. [DOI] [PubMed] [Google Scholar]
- 14.Chern S, Magargal LE, Annesley WH. Central retinal vein occlusion associated with drusen of the optic disc. Ann Ophthalmol. 1991;23:66–69. [PubMed] [Google Scholar]
- 15.Gittinger JW, Lessell S, Bondar RL. Ischemic optic neuropathy associated with optic disc drusen. J Clin Neuroophthalmol. 1984;4:79–84. [PubMed] [Google Scholar]
- 16.Michaelson C, Behrens M, Odel J. Bilateral anterior ischaemic optic neuropathy associated with optic disc drusen and systemic hypotension. Br J Ophthalmol. 1989;73(9):762–764. doi: 10.1136/bjo.73.9.762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Newman WD, Dorrell ED. Anterior ischemic optic neuropathy associated with disc drusen. J Neuro-Ophthalmol. 1996;16(1):7–8. doi: 10.1097/00041327-199603000-00002. [DOI] [PubMed] [Google Scholar]
- 18.Liew SCK, Mitchell P. Anterior ischaemic optic neuropathy in a patient with optic disc drusen. Aust N Z J Ophthalmol. 1999;27(2):157–160. doi: 10.1046/j.1440-1606.1999.00176.x. [DOI] [PubMed] [Google Scholar]
- 19.Kamath GG, Prasad S, Phillips RP. Bilateral anterior ischaemic optic neuropathy due to optic disc drusen. Eur J Ophthalmol. 2000;10(4):341–343. doi: 10.1177/112067210001000414. [DOI] [PubMed] [Google Scholar]
- 20.Purvin V, King R, Kawasaki A, Yee R. Anterior ischemic optic neuropathy in eyes with optic disc drusen. Arch Ophthalmol. 2004;122(1):48–53. doi: 10.1001/archopht.122.1.48. [DOI] [PubMed] [Google Scholar]
- 21.Ayhan Z, Yaman A, Soylev Bajin M, Saatci AO. Unilateral acute anterior ischemic optic neuropathy in a patient with an already established diagnosis of bilateral optic disc drusen. Case Rep Ophthalmol Med. 2015;2015:730606. [DOI] [PMC free article] [PubMed] [Google Scholar]


