Objective:
In 2017, an academic health center in Chicago launched the multidisciplinary Substance Use Intervention Team (SUIT) to address opioid misuse across 18 inpatient units and in a new outpatient addiction medicine clinic. This report assesses the first 5 months of implementation and associations with patient health and healthcare utilization.
Methods:
Patient demographic and screening data were extracted from the administrative data warehouse of the electronic health record (EHR) infrastructure. Distribution of sample characteristics for positive initial screens for opioid misuse was tested against those of all patients screened using a 2-tailed test of proportions (P < 0.05). A second analysis compared length of stay and 30-day readmissions within a cohort of patients with a secondary diagnosis of substance use disorder.
Results:
Between November, 2017 and March, 2018, 76% of 15,054 unique patients were screened, 578 had positive scores on the Alcohol Use Disorders Identification Test and Drug Abuse Screening Test, 131 had positive scores for opioid misuse, and 52 patients initiated medication treatment. Patients with a secondary diagnosis of substance use disorder who received a SUIT consult (n = 161), compared with those who did not (n = 612), had a shorter average length of stay (5.91 vs 6.73 days) and lower 30-day readmission rate (13.6% vs 15.7%).
Conclusion:
Leveraging the EHR to conduct standardized screenings and treatment has helped identify an at-risk population—disproportionately younger, black, and male—and treat new cases of opioid and substance misuse. The intervention indicates trends toward a shortened length of stay, reduced 30-day readmissions, and has linked patients to outpatient care.
Keywords: addiction medicine, opioids, population health, screening, substance use
In 2016, opioid overdoses killed over 42,000 people across the United States, and 40% of them were due to prescription opioids (Vadivelu et al., 2018). Between 2000 and 2015, prescription opioids were involved in more overdose deaths than any other drug; only in 2016 did fentanyl surpass prescription opioids in its association with overdose deaths (Young et al., 2018). According to a 2015 citywide survey (Chicago Department of Public Health, 2017b), 13% of adults in Chicago reported using a prescription opioid that year, and 3% reported misuse of prescription opioids. Individuals aged 30 to 44 reported the highest rate of opioid pain reliever misuse. In 2000, the Chicago medical examiner reported 310 opioid overdose deaths. By 2015, this number increased to 426 deaths (15.5 per 100,000), which is 50% higher than the national rate (10.4 per 100,000) (Chicago Department of Public Health, 2017a). The majority of Chicago's deaths involved heroin and were accidental (Chicago Department of Public Health, 2017a).
Substance use disorders (SUDs) and opioid use disorders (OUDs), in particular, are associated not only with increased mortality but also with increased morbidity and healthcare costs. Between 2001 and 2012 heroin overdose-related admissions increased 1.9-fold in the United States, and prescription opioid admissions increased 2.5-fold (Hsu et al., 2017). Similarly, opioid-related emergency department (ED) visits increased 183% between 2004 and 2011, with approximately 25% resulting in a hospital admission (Liebschutz et al., 2013). In 2016, overdose costs related to hospital admissions, treatment, comorbidities, and stabilization exceeded $10 billion (Rhyan, 2017).
Hospitalized patients have a high prevalence of SUDs, which may also be associated with rehospitalizations (Walley et al., 2012). The times during which these patients are in the hospital are considered “reachable moments” (Wei et al., 2014), whereby patients dealing with acute illnesses might have increased motivation to change substance use behaviors (Shanahan et al., 2010; Liebschutz et al., 2013). The Substance Use Intervention Team (SUIT) program was designed to identify patients with SUDs who are hospitalized with acute comorbidities and offer treatment. Pharmaceutical approaches, such as buprenorphine—an opioid agonist treatment—have been demonstrated as efficacious in the treatment of opioid dependency for persons who seek treatment, but the treatment's efficacy for patients identified while hospitalized for comorbidities has not been determined (Liebschutz et al., 2013).
This urban, academic health center developed a population-level strategy to address this crisis across its inpatient units based on an intervention deployed at Boston University (Trowbridge et al., 2017), and prior experience from Duke University. The SUIT is a multidisciplinary consultation team of addiction medicine specialists from emergency medicine, psychiatry, toxicology, social work, and pharmacology. This report summarizes and assesses the results from the first five months of SUIT's implementation; preliminary findings indicate SUIT is associated with screening successes, identification and treatment of opioid misuse, and reduced length of stay and 30-day readmissions.
METHODS
To implement SUIT's screening, brief intervention, referral, and treatment (SBIRT), SUD screening and intervention flow sheets, and also consult order sets were added to the electronic health record (EHR)-driven workflows of both inpatient nurses and social workers on 18 medical and surgical units. Leveraging the EHR infrastructure, SUIT begins with standardized, universal screening of all patients who have not been screened in the past 12 months (see Fig. 1). Specifically, if patients report a positive on a 2-question screening for excessive alcohol use (ie, 5 or more drinks for a male or 4 or more drinks for a female) and/or illicit drug use in the past year, the algorithm triggers the workflow for the social worker to conduct a full screening with the Alcohol Use Disorders Identification Test (AUDIT) or the Drug Abuse Screening Test (DAST) (Skinner, 1982; Babor et al., 1992). Guided by the risk-stratified score, the social worker may provide a brief intervention using motivational interviewing and may request the SUIT consult team to round on identified high-risk patients. The consult team determines with the patient whether to initiate medication and linkage to outpatient services upon discharge. If ready, patients can begin medication (eg, buprenorphine), and, upon discharge, receive individual and group psychotherapy, case management, continued medication treatment at the new, outpatient addiction medicine clinic.
FIGURE 1.
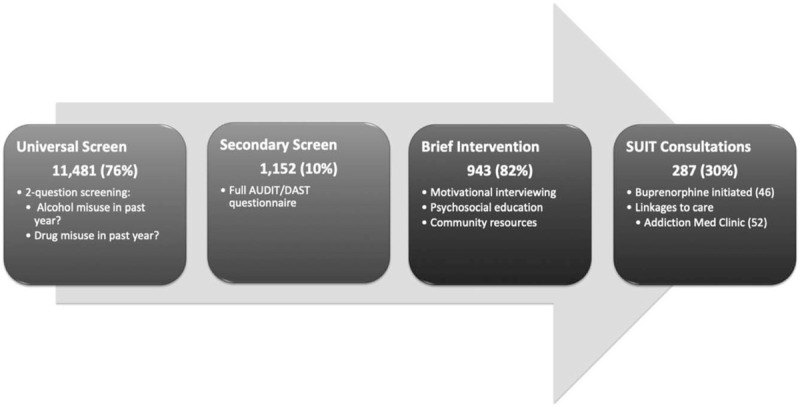
The Substance Use Intervention Team schema implemented across 18 inpatient units at a Chicago academic health center between November, 2017 and March, 2018 (n = 15,054).
To assess effectiveness, we conducted 2 different analyses: one to assess results of universal screening and one to assess SUIT's potential impact on 2 utilization metrics, length of stay, and 30-day readmissions. To conduct the first analysis, we extracted demographic and SBIRT flow sheet data by inpatient unit from the EHR administrative data warehouse. As SUIT centers opioid misuse among a range of substance misuse, we hypothesized that demographic distribution of patients positive for opioid misuse (ie, patients who specified opioid misuse following the positive RN screen) would differ significantly from the distribution of the patient population universally screened across the 18 units. We calculated z-scores with a 2-tailed test of 2 proportions (P < 0.05). Stata was used to conduct all statistical analyses (StataCorp., 2015).
Next, we extracted from Vizient by unit, the length of stay, and 30-day readmission data for patients with a secondary diagnosis of substance use to compare utilization metrics of those receiving a SUIT consult order and those who did not. The rationale for this cohort of patients was that 85% of those patients who received a SUIT consult had a secondary diagnosis of SUD. Further, we know that SUD is associated with hospitalizations and rehospitalizations (Walley et al., 2012; Wei et al., 2014). Drawing on Wei et al.'s analysis, we performed t tests (P < 0.05) hypothesizing that the length of stay and 30-day readmissions would trend lower for SUIT patients with a secondary diagnosis of substance misuse than non-SUIT patients with the same diagnosis. Similarly, we hypothesized that this cohort of patients would have a shorter length of stay and lower 30-day readmissions for this period compared with the same period in the previous year before the SUIT implementation. This research was certified by the Rush University Medical Center institutional review board as a quality improvement study.
RESULTS
Screening rates for the first 5 months across the 18 designated inpatient medical and surgical units averaged 76% of the total number of patients admitted (n = 15,054). Sample characteristics indicate that SUIT patients were significantly younger (37.4% vs 19.3%; P < 0.05), black (55.0% vs 35.7%), and male (60.3% vs 45.4%) compared with the general inpatient population that received the initial screen (see Table 1). Of patients screened, 5% (n = 578) were positive for substance misuse and 1% (n = 131) for opioid misuse.
TABLE 1.
Sample Characteristics Across 18 Inpatient Units at a Chicago Academic Health Center: Positive Opioid Misuse Screenings, Positive Substance Misuse Screenings, and Total Screened; Test of Proportions Positive Opioid vs Total Screened Between November, 2017 to March, 2018
| Positive Screenings | Positive Screenings | Total Screenings | |||||
| Opioid Misuse | Substance Misuse | ||||||
| n | % | n | % | n | % | P < 0.05 | |
| Sex | |||||||
| Female | 52 | 39.7% | 222 | 38.4% | 6262 | 54.6% | 0.001 |
| Male | 79 | 60.3% | 356 | 61.6% | 5216 | 45.4% | 0.001 |
| Race | |||||||
| Black | 72 | 55.0% | 251 | 43.4% | 4097 | 35.7% | 0.000 |
| White | 49 | 37.4% | 246 | 42.6% | 5441 | 47.4% | 0.023 |
| Other | 8 | 6.1% | 72 | 12.5% | 1668 | 14.5% | 0.006 |
| American Indian | 2 | 1.5% | 5 | 0.9% | 38 | 0.3% | 0.020 |
| Asian | 0 | 0.0% | 4 | 0.7% | 218 | 1.9% | 0.112 |
| Native Hawaiian/Pacific Islander | 0 | 0.0% | 0 | 0.0% | 16 | 0.1% | 0.667 |
| Ethnicity | |||||||
| Hispanic/Latin | 12 | 8.6% | 94 | 16.3% | 1906 | 16.6% | 0.023 |
| Non-Hispanic/non-Latin | 119 | 91.4% | 484 | 83.7% | 9572 | 83.4% | 0.023 |
| Age, yrs | |||||||
| 0–17 | 0 | 0.0% | 0 | 0.0% | 33 | 0.3% | 0.542 |
| 18–24 | 2 | 1.5% | 33 | 5.7% | 381 | 3.3% | 0.254 |
| 25–44 | 49 | 37.4% | 213 | 36.9% | 2214 | 19.3% | 0.000 |
| 45–64 | 62 | 47.3% | 277 | 47.9% | 4410 | 38.4% | 0.038 |
| 65+ | 18 | 13.7% | 55 | 9.5% | 4440 | 38.7% | 0.000 |
| 131 | 578 | 11478 | |||||
Excluding psychiatry, obstetrics, and rehabilitation units where screening was not occurring, we compared utilization statistics of all patients who had a pre-existing secondary diagnosis of SUD and did (n = 161) or did not (n = 612) receive a SUIT consult to Addiction Medicine. Of 773 patients with a secondary diagnosis of SUD, 21% received a SUIT consult order to Addiction Medicine and 79% did not. Statistical tests revealed no significant differences between the 2 groups along levels of acuity (ie, severity of illness) or axes of age, sex, or race, although black patients represented 52% of consulted patients and only 47% of non-consulted patients. In terms of utilization, patients who received a SUIT consult had a 0.83-day shorter average length of stay over the first 5 months compared with those patients who did not receive a SUIT consult (5.91 vs 6.73 days). Similarly, patients who received a SUIT consult had lower 30-day readmissions than those patients with a secondary diagnosis of SUD who did not receive a consult (13.6% vs 15.7%). Although they indicate cost-saving utilization trends, none of these differences reached statistical significance (P < 0.05).
Finally, we compared pre-SUIT (November, 2016–March, 2017) and post-SUIT (November, 2017–March, 2018) utilization metrics for the cohort of patients with a secondary diagnosis of SUD. While there were no significant differences or noteworthy trends along axes of race, sex, or age, the average length of stay was slightly higher for the post-SUIT period: 6.38 days in the pre-SUIT time period (n = 754) compared with 6.50 days during the first 5 months of SUIT (n = 773); the severity of illness (pre: 2.58 vs post: 2.68) and expected length of stay (pre: 7.11 vs post: 8.11 days) were both higher for the 5-month SUIT period compared with the previous year. None of the differences were statistically significant (P < 0.05).
DISCUSSION
This preliminary assessment of a population-level intervention shows promising feasibility and effectiveness toward the identification and treatment of substance misuse and opioid dependence at a large academic health center. Standardized workflows have enabled screening thousands of patients (76%), and the timely identification (10%), intervention (6.3%), and medication treatment (0.3%) of patients who self-report misuse among 15,054 total unique patients. A systems-level SBIRT strategy reduces bias in this process and in health disparities. The 24% of patients who were not screened may indicate a threshold at which some patients are not ready to disclose their substance use in this setting and other patients who are not accessible for screening due to level of acuity. Put another way, self-disclosure of substance misuse requires a readiness on the part of the patient; though their hospitalization may represent a “reachable moment,” the unscreened 24% may indicate that not all patients are ready to disclose their misuse and receive treatment. However, of those screened, the prevalence of substance misuse aligns with other studies of hospitalized patients (Walley et al., 2012; Liebschutz et al., 2013; Trowbridge et al., 2017).
Utilization metrics also indicate positive trends. First, given the shorter length of stay and lower 30-day readmissions of SUIT-consulted patients compared with non-SUIT-consulted patients with a secondary diagnosis of SUD, these trends are associated with cost savings and improving health outcomes. SUIT may contribute both to the reduction of time that patients spend in the hospital and to more effective treatments, like medication, and also warm handoffs to additional therapies and support. The launch of an integrated, multidisciplinary addiction medicine team and outpatient clinic has provided a more direct and seamless linkage in which hospitalized patients may receive medication treatment and enroll upon discharge; the outpatient clinic may offer additional support for the reduction of length of stay and readmissions. The slightly increasing severity of illness and length of stay for post-SUIT compared with pre-SUIT may reflect the trend of increasing substance misuse and severity of illness among this cohort of patients. Increased attention to follow-up care, medication treatment, and retention and adherence to them, respectively, will likely improve health outcomes and help lower these utilization measurements.
This preliminary analysis has limitations. It is not a randomized controlled trial, and, although we did not identify significant differences in demographic characteristics, there may be other sources of unmeasured confounding. The comparison groups are imperfect; in particular, the pre and post-SUIT comparisons of patients with SUD have a relatively small number of patients who actually received a SUIT consult. Moreover, the different time periods may be impacted by increasing substance use prevalence. In addition, work flows may have prevented social workers from consistently entering patient AUDIT and DAST scores; missing scores may be skewed toward negative ones but likely include some positive scores as some SUIT-consult cases had no AUDIT or DAST score entered in the EHR but indications of positive scores in the progress notes. Longitudinal and learning health systems research is recommended to investigate longer-term health outcomes related to opioid and substance misuse treatments and follow-up care.
CONCLUSIONS
Electronic health record infrastructure offers the capacity to intervene on the opioid crisis at the population level, identifying a range of substance misuse and opioid dependency across inpatient units of a large academic health center in Chicago. Screening rates are high, and the universal mode helps mitigate biases in the identification of a substance misusing population. Moreover, the timely medication treatments and subsequent warm handoffs linking patients to additional supportive therapies help ensure continuity of care and improved health outcomes. Longitudinal and outcomes data will inform future directions for opioid prevention practice and policy. Replication of SUIT may be warranted at comparable hospitals in the face of this epidemic.
Footnotes
Funding: Dr Thompson received research support from the BMO Harris Bank Health Disparities Fellowship and the Illinois Department of Human Services (Opioid STR Grant 43.788, agreement no. 43CXZ03198). Dr Karnik received research support from the Substance Abuse and Mental Health Services Administration (no. 1233-505-94/940155-0618).
Conflicts of interest: With the exception of Dr Pollack, none of the authors have any existing or potential conflicts of interest to disclose.
REFERENCES
- Geneva, Switzerland, Babor T, de la Fuente J, Saunders J, et al. AUDIT: The Alcohol Use Disorders Identification Test. Guidelines for use in primary health care. 1992. [Google Scholar]
- Chicago, IL, Chicago Department of Public Health. Epidemiology Brief: Characterizing Opioid Use, Misuse, and Overdose in Chicago. 2017. [Google Scholar]
- Chicago and Suburban Cook County, IL, Chicago Department of Public Health. Epidemiology Brief: Opioid-Related Overdose Deaths in Cook County, IL, 2015. 2017. [Google Scholar]
- Hsu D, McCarthy E, Stevens J, et al. Hospitalizations, costs and outcomes associated with heroin and prescription opioid overdoses in the United States 2001–12. Addiction 2017; 112:1558–1564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liebschutz JM, Crooks D, Herman D, et al. Buprenorphine treatment for hospitalized, opioid-dependent patients: a randomized clinical trial. JAMA 2013; 174:1369–1376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhyan C. The Potential Societal Benefit of Eliminating Opioid Overdoses, Deaths, and Substance Use Disorders Exceeds $95 Billion Per Year [Altarum web site]. November 16, 2017. Available at: https://altarum.org/sites/default/files/uploaded-publication-files/Research-Brief_Opioid-Epidemic-Economic-Burden.pdf. Accessed June 11, 2018. [Google Scholar]
- Shanahan C, Beers D, Alford DP, et al. A transitional opioid program to engage hospitalized drug users. J Gen Intern Med 2010; 25:803–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skinner H. The Drug Abuse Screening Test. Addict Behav 1982; 7:363–371. [DOI] [PubMed] [Google Scholar]
- Stata Statistical Software [computer, program]. Release, 14. College Station, TX: StataCorp LP; 2015. [Google Scholar]
- Trowbridge P, Weinstein ZM, Kerensky T, et al. Addiction consultation services: linking hospitalized patients to outpatient addiction treatment. J Subst Abuse Treat 2017; 79:1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vadivelu N, Kai AM, Kodumudi V, et al. The opioid crisis: a comprehensive overview. Curr Pain and Headache Rep 2018; 22:16. [DOI] [PubMed] [Google Scholar]
- Walley AY, Paasche-Orlow M, Lee EC, et al. Acute care hospital utilization among medical inpatients discharged with a substance use disorder diagnosis HHS public access. J Addict Med 2012; 6:50–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wei J, Defries T, Lozada M, et al. An inpatient treatment and discharge planning protocol for alcohol dependence: efficacy in reducing 30-day readmissions and emergency department visits. J Gen Intern Med 2015; 30:365–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young L, Crausman R, Fulton J. Suboptimal opioid prescribing: a practice change project. R I Med J 2018; 101:41–44. [PubMed] [Google Scholar]


