Abstract
PURPOSE
To assess the effect of a primary care–based community-links practitioner (CLP) intervention on patients’ quality of life and well-being.
METHODS
Quasi-experimental cluster-randomized controlled trial in socioeconomically deprived areas of Glasgow, Scotland. Adult patients (aged 18 years or older) referred to CLPs in 7 intervention practices were compared with a random sample of adult patients from 8 comparison practices at baseline and 9 months. Primary outcome: health-related quality of life (EQ-5D-5L, a standardized measure of self-reported health-related quality of life that assesses 5 dimensions at 5 levels of severity). Secondary outcomes: well-being (Investigating Choice Experiments for the Preferences of Older People Capability Measure for Adults [ICECAP-A]), depression (Hospital Anxiety and Depression Scale, Depression [HADS-D]), anxiety (Hospital Anxiety and Depression Scale, Anxiety [HADS-A]), and self-reported exercise. Multilevel, multiregression analyses adjusted for baseline differences. Patients were not blinded to the intervention, but outcome analysis was masked.
RESULTS
Data were collected on 288 and 214 (74.3%) patients in the intervention practices at baseline and follow-up, respectively, and on 612 and 561 (92%) patients in the comparison practices. Intention-to-treat analysis found no differences between the 2 groups for any outcome. In subgroup analyses, patients who saw the CLP on 3 or more occasions (45% of those referred) had significant improvements in EQ-5D-5L, HADS-D, HADS-A, and exercise levels. There was a high positive correlation between CLP consultation rates and patient uptake of suggested community resources.
CONCLUSIONS
We were unable to prove the effectiveness of referral to CLPs based in primary care in deprived areas for improving patient outcomes. Future efforts to boost uptake and engagement could improve overall outcomes, although the apparent improvements in those who regularly saw the CLPs may be due to reverse causality. Further research is needed before wide-scale deployment of this approach.
Key words: general practice, primary care, multimorbidity, complex interventions, health inequalities, social prescribing, community link workers
INTRODUCTION
Health inequalities are a global problem, resulting from a fundamental inequity in the distribution of income, power, and wealth. This inequity limits opportunities across the life course, including access to education, housing, jobs, and health care.1,2 In addition, people of low socioeconomic status experience multiple health problems and a concentration of risk factors,3 exacerbated by poor access to resources to manage them.4
A common policy response to health inequalities in recent years has been the introduction of various social prescribing programs. Social prescribing aims to link patients to nonmedical sources of support within a community, thus expanding options and resources beyond those traditionally provided in primary health care.5 In principle, social prescribing interventions should enable a more holistic response to patients’ needs. By providing access to community-based services and support, they can reduce social isolation, promote behavior change (such as joining a walking group), and mitigate some of the effects of poverty through welfare advice or employment opportunities, for example.6 The evidence base for the effectiveness of social prescribing is extremely limited, however.7–9
The Scottish government has recently supported social prescribing in areas of high socioeconomic deprivation. The Glasgow Deep End Links Worker Programme (LWP) aims to help people in areas of deprivation to “live well” in their communities by providing an attached community-links practitioner (CLP) to general practices.10 Here, we report the quantitative findings on patient outcomes of this program. Our aim was to test the hypothesis that the intervention would lead to improvements in patients’ quality of life and other aspects of well-being.
METHODS
Design and Setting
We conducted a quasi-experimental cluster-randomized controlled trial (RCT) of the Glasgow Deep End LWP.11 Practices were eligible for the program if they were located in Glasgow and in the 100 practices in Scotland (which has approximately 1,000 practices) serving the most-deprived patients (based on the percentage of registered patients in practices living in the 15% most-deprived postcodes in Scotland). Fifteen general practices serving patients living in very deprived areas (out of 76 eligible practices in Glasgow) took part. Funding from the Scottish government financed 7 practices to implement the intervention. The remaining 8 practices acted as a comparison group. Patients who participated in the evaluation provided written informed consent. The study was approved by the University of Glasgow College of Medical Veterinary and Life Sciences Ethics Committee (200140077) and registered prospectively with International Standard Randomized Controlled Trials (ISRCTN80842457), and the protocol was published.11
Practice Recruitment and Randomization
Fourteen practices expressed an interest in joining the LWP, in addition to the practice of the program’s clinical lead. Of these, 6 were randomly selected to join the intervention arm of the trial, along with the clinical lead’s practice. The remaining 8 were designated comparator practices.11
Recruitment of Patients to the Study
Intervention Patient Cohort
Adult patients who were registered with an intervention practice and were referred to a CLP during the study recruitment period were eligible. Full details of the recruitment procedure have been published.11 In brief, the health care clinicians—general practitioners (GPs) and practice nurses (PNs)—were briefed to give adult patients (aged 18 years or older) the study information and to seek permission to pass on their contact details to the research team at the time of referral to a CLP. When this permission was received, a member of the research team contacted patients to explain the study and, if patients expressed interest in taking part, mailed them the study consent form and baseline questionnaire to complete and return to the study office. If there was no response within 10 days, patients were telephoned and given additional options for completing the questionnaire, either during a face-to-face meeting or over the telephone with the study researcher. We aimed to collect baseline data before the start of the CLP intervention whenever possible, although the researchers had no control over when the CLP would arrange to see the patient.
Comparator Practice Patient Cohort
Because the characteristics of patients seen by a CLP were unknown in advance (any patient deemed suitable for referral to the CLP by the practice was eligible), it was not possible to select matched control patients from the comparator practices at the time of recruitment and baseline data collection. Therefore, 1,000 adult patients (aged 18 years or older) registered with a comparator practice were randomly selected for invitation to participate in the evaluation. A senior GP in each practice reviewed the list to remove patients they considered inappropriate for health or social reasons (such as terminal illness or family or other social crisis).11 The practice then mailed the study invitation pack to the patients included.
Intervention
The practice-level intervention had 2 key components: a funded full-time CLP in each practice and a practice development fund. Table 1 describes the key features of the program. Its core functions were as follows:
CLPs established links between the practice and local community organizations, helped by the practice development fund used to “buy out” practice staff time to spend improving systems and building relationships.
General practices developed referral systems through which GPs and PNs referred patients they believed likely to benefit from seeing a CLP.
Table 1.
Description of the Glasgow Deep End Links Worker Program Using the TIDieR Framework12
| Name | The Glasgow Deep End Links Worker Program |
|---|---|
| Purpose | The development of the Glasgow Deep End LWP drew on the theory of community-oriented primary care13 and was based on a report by GPs working in the Deep End.14 Patients attending general practices in deprived areas commonly have multiple problems, many of which are not amenable to medical intervention. Community organizations offer a wide range of resources, but people in deprived areas with multiple health and social problems can find it hard to access them. Closer links between general practices and community organizations, and support to access to available community resources, could mitigate the effects of deprivation. Links between general practices and community organizations could be enhanced by adding a nonmedical CLP to the practice team. CLPs would operate from the general practice, forge relationships between general practices and community organizations, and support patients to access the nonmedical services and support on offer. CLPs would act as a catalyst to hope and self-determination, using the strong relationships with patients that exist in general practice. If patients with complex needs feel supported, they would be more likely to respond to information on ways to improve their health. |
| Resources | A practice-attached CLP with a previous working background in community development. The CLPs all had previous experience of working with individuals and community organizations and had skills in identifying assets, needs, opportunities, rights, and responsibilities. Management support for the program was provided by the CLPs’ employing organization, the Scottish Alliance for Health and Social Care (Scotland). Support included (1) an experienced program director, overseeing all aspects of the program including the production of detailed records of learninga; (2) a community links manager, with experience in community development and staff management, responsible for establishing protocols and polices for CLP work and line managing the CLPs; (3) a learning and evaluation officer, responsible for establishing local protocols for program monitoring (independent of the evaluation conducted by the research team); (4) administrative staff; and (5) a clinical lead. A practice development fund (GBP £35,000) to spend on activities to help each practice develop the new LWP approach. The fund was used mainly to “buy time” away from clinical care to focus on the LWP. The A Local Information System for Scotland (ALISS) website,b which allows individuals and community organizations to make real-time lists of sources of support searchable by locality. |
| Procedures | CLPs made links between practices and community organizations in the local area (eg, walking groups, debt management support, welfare rights, drug and alcohol management support, lunch clubs, befriending schemes, crafting clubs, bereavement support). Practice staff used time away from clinical care to set up systems and learn more about services and support available in community organizations. Each practice devised its own system for GPs and PNs to identify and refer patients who would benefit from help from a CLP who would link them to community-based resources. The system was devised jointly by clinical staff and CLPs and was customized for each practice. The choice of which patients to refer to the CLP was left open by practices but was based mainly on the presence of social problems that exacerbated long-term health problems. CLPs met patients. CLPs elicited patients’ main needs and worked flexibly, making links with community organizations for patients and, if necessary, supporting patients to attend the organizations’ services. Services depended on patients’ needs, their enthusiasm to engage, and the availability of local services accessible to patients. CLPs met together weekly with a manager to share and discuss experiences and problem solve collectively. |
| Providers | GPs and PNs referred patients who might benefit to CLPs. CLPs saw patients and provided support to link patients to existing community organizations. |
| How | All contacts were one-to-one and usually face-to-face, although some telephone contacts could occur. |
| Where | CLP contacts with patients were usually in the practice, although some home visits could occur, and the CLPs could accompany patients to support their contact with a community organization. |
| When and how much | CLPs and patients could meet as many times, and when, they thought necessary. |
| Tailoring | The intervention was very flexible and dependent on patient needs, patient wants, and professionals’ judgments as to what help was needed. |
| Modifications | The intervention was not modified during the research. |
| How well | Given the flexibility of the intervention, we did not assess fidelity. |
CLP = community-links practitioner; GBP = Great Britain pound sterling; GP = general practitioner; LWP = Links Worker Programme; PN = practice nurse; TIDieR = Template for Intervention, Description, and Replication.
Each CLP met the referred patient as many times as both thought appropriate, identified the patient’s most pressing problems, and supported referral to and ongoing contact with local community resources. The “theory of change” that underpinned the evaluation is shown in Supplemental Table 1, available at http://www.AnnFamMed.org/content/17/6/518/suppl/DC1/. Comparison practices were not allocated a CLP or a practice development fund.
Primary Patient Outcome
The primary patient outcome was health-related quality of life, measured at baseline and at 9 months’ follow-up by the EQ-5D-5L, a standardized measure of self-reported health-related quality of life that assesses 5 dimensions at 5 levels of severity.15
Secondary Patient Outcomes
Secondary patient outcome measures at baseline and follow-up at 9 months included the Investigating Choice Experiments for the Preferences of Older People Capability Measure for Adults (ICECAP-A,16 a capability-based measure of well-being in adults), the Hospital Anxiety and Depression Scale (HADS),17 the Work and Social Adjustment Scale,18 burden of multimorbidity,19 and self-reported lifestyle activities (smoking, alcohol, exercise). At baseline, data were collected on sociodemographic measures (age, sex, education, ethnicity, and work status) and deprivation status based on postcode by using the Scottish Index of Multiple Deprivation (the Scottish government’s small-area index, which integrates 7 domains of deprivation to give an overall score).20
Blinding
It was not possible to mask participants or health care professionals to the group allocation of their practice. It was also not feasible to blind members of the core study team collecting the data (B.F., L.G.), but the statisticians carrying out the primary analyses (A.M., A.B., G.J.-R.) and all other coauthors were blinded to the allocation. The statistical analysis plan was written before unblinded data analysis.
Sample Size
The minimum target sample sizes of 286 patients for intervention and 484 patients for comparator practices was calculated to have 80% power to detect a minimally important effect size of 0.274 standard deviations (SDs) in the EQ-5D-5L with a 95% degree of confidence, assuming an intraclass correlation of 0.01 and a 50% follow-up rate. This sample size would provide 90% power to detect an effect size of 0.316 SDs under the same assumptions.
Analysis
Primary analysis was on an intention-to-treat basis (all patients referred to a CLP) using all available data. Subgroup analysis was conducted on patients who actually attended a CLP face-to-face consultation. Differences between groups were tested with appropriate mixed-effects linear or generalized linear regression models, allowing clustering by practice. Because the comparator patients were respondents from a randomly selected sample, it was expected that there would be differences in patient characteristics and outcome measures at baseline compared with the intervention patients. The statistical model used retained the standard adjustments (baseline outcome value, age, sex, deprivation, and multimorbidity) plus any other variables that differed at baseline and were significant predictors of outcome in the regression model.
RESULTS
Study Sample Achieved
Of 980 adult patients referred to a CLP during the study period (March-December 2015), 559 (57%) were referred to the research team for potential recruitment to the study. Of these, 288 (52%) were recruited (Supplemental Figure 1a, available at http://www.AnnFamMed.org/content/17/6/518/suppl/DC1/). Patients recruited into the study were representative of all CLP patient referrals in terms of sex, number and type of referral problems, and deprivation level but were slightly older (mean 46.4 years vs 48.3 years for all CLP referrals vs CLP study recruits, respectively, P = 0.018). (Supplemental Table 1, available at http://www.AnnFamMed.org/content/17/6/518/suppl/DC1/.) In comparison practices, a random sample of 7,942 yielded 612 (8%) returned completed baseline questionnaires (Supplemental Figure 1b, available at http://www.AnnFamMed.org/content/17/6/518/suppl/DC1/).
Of the 288 patients recruited to the study in the intervention group, 214 (74.3%) completed the follow-up questionnaire 9 months later. Of the 612 patients recruited into the study in the comparison group, 561 (92%) completed the follow-up questionnaire.
Baseline Characteristics of Study Sample
In both the intervention and comparison groups, English was the predominant first language (98%), and 60% of participants were female (Table 2). Patients in the intervention group were younger, of lower socioeconomic status, and more likely to be living alone than patients in the comparison group. They also had more medical and social problems, poorer quality of life, and poorer mental health (Table 2). The prevalence of individual medical conditions and social problems is shown in the supplementary file (Supplemental Tables 2 and 3, available at http://www.AnnFamMed.org/content/17/6/518/suppl/DC1/). Almost one-half (45%) of the intervention group smoked, and 58% reported that they did not exercise regularly.
Table 2.
Patient Characteristics at Baseline
| Characteristic | Intervention | Comparison | P Value |
|---|---|---|---|
| Age, y | 49 (16) | 56 (15) | <.001 |
| Female, % | 59.2 | 61.1 | .61 |
| Deprived,a % | 79.3 | 58.1 | <.001 |
| Employed, % | 24.1 | 48.7 | <.001 |
| Lives alone, % | 67.5 | 45.9 | <.001 |
| Current smoker, % | 45.2 | 20.4 | <.001 |
| Never exercises, % | 58.0 | 31.0 | <.001 |
| Multimorbidity,b % | 3.1 (2.1) | 2.3 (1.8) | <.001 |
| Social problems,c % | 3.9 (2.5) | 1.8 (2.1) | <.001 |
| EQ-5D-5L | 0.382 (0.337) | 0.683 (0.300) | <.001 |
| ICECAP-A | 0.563 (0.228) | 0.812 (0.212) | <.001 |
| WASAS | 22.3 (12.2) | 9.4 (11.4) | <.001 |
| HADS-A >10,d % | 71.7 | 29.0 | <.001 |
| HADS-D >10,e % | 57.5 | 19.0 | <.001 |
EQ-5D-5L = a standardized measure of self-reported health-related quality of life that assesses 5 dimensions at 5 levels of severity; HADS = Hospital Anxiety and Depression Scale; HADS-A = Hospital Anxiety and Depression Scale, Anxiety; HADS-D = Hospital Anxiety and Depression Scale, Depression; ICECAP-A = Investigating Choice Experiments for the Preferences of Older People Capability Measure for Adults; WASAS = Work and Social Adjustment Scale.
Note: Characteristics are either shown as mean (standard deviation) or percentages.
Those in the top quintile of deprivation for Scotland as measured by the Scottish Index of Multiple Deprivation.
The count of self-reported chronic conditions.
The count of self-reported social problems.
The HADS percentage scoring above 10 (likely case-ness) for anxiety.
The HADS percentage scoring above 10 (likely case-ness) for depression symptoms.
Although we endeavored to collect baseline patient questionnaires before the patient first consulted with the CLP, this was possible in only 159/288 (55%) of patients. However, the baseline outcome and demographic measures of patients who completed the questionnaire before or after the first CLP appointment did not differ significantly (Supplemental Tables 4 and 5, available at http://www.AnnFamMed.org/content/17/6/518/suppl/DC1/). This finding suggests that seeing the CLP once before completing the baseline questionnaire did not affect the baseline outcome scores (further supported by our findings below).
Patient Engagement
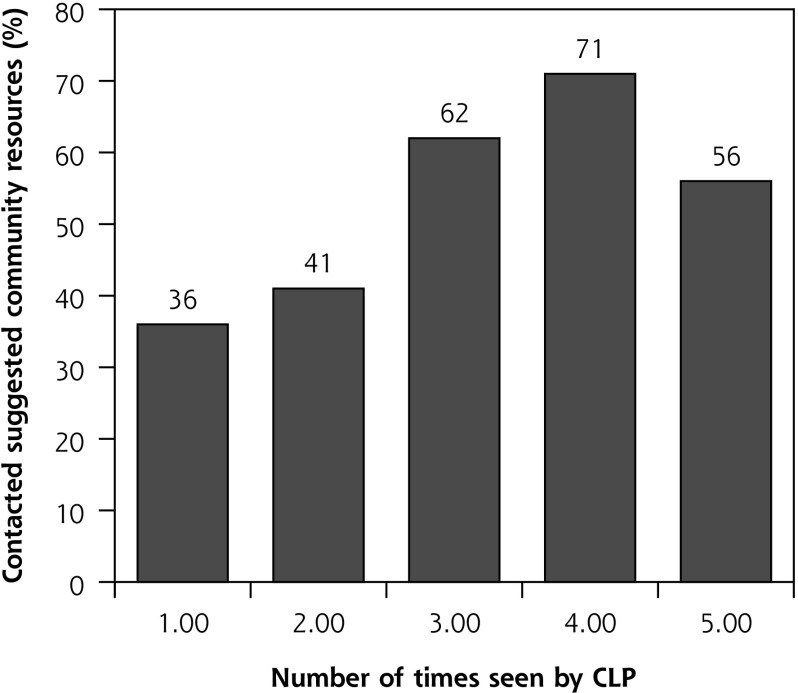
Of the 288 patients in the study who were referred to the CLP, 26 (9.0%) did not engage at all. Of the 262 who engaged, 41.4% had 1 face-to face consultation with the CLP, 13.4% had 2, 12.1% had 3, and 33.5% had 4 or more, with the mean number being 3.1 (SD 4.59). Uptake of community resources by patients increased with increasing number of CLP contacts (Spearman’s ρ = 0.684, P <.001), although it declined somewhat above 4 consultations (Figure 1).
Figure 1.
Relationship between number of times seen by CLP and patient contact with suggested community resource.
CLP = community-links practitioner.
Outcome Analysis
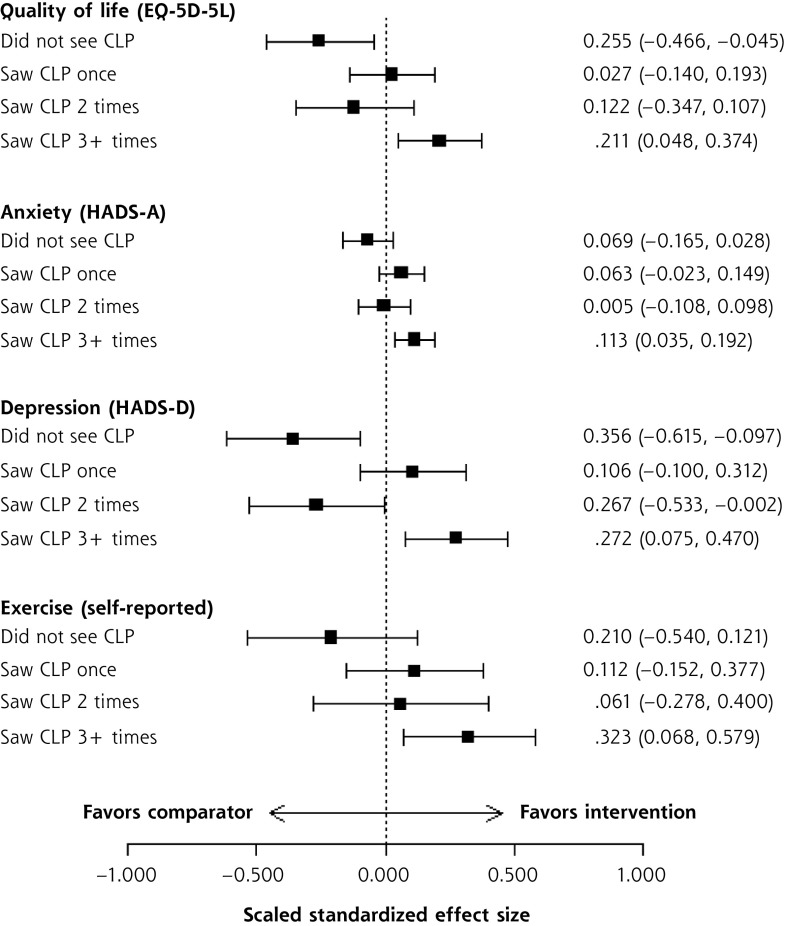
In the intention-to-treat analysis, referral to a CLP had no significant effect on the primary outcome (health-related quality of life) at 9 months compared with the comparison group in the adjusted analyses (Table 3). This was also the case for all secondary outcomes (Table 3). Subgroup analyses of the patients who consulted face to face with a CLP showed significant improvements in health-related quality of life among those who consulted 3 or more times (Table 4). Similar significant improvements were also observed for anxiety, depression, and self-reported exercise levels (Table 4). No effects were seen on work and social adjustment (Table 4), nor on smoking rates or self-reported alcohol intake (results not shown). The standardized effect sizes of these significant changes in quality of life, anxiety, depression, and exercise levels were generally small (Figure 2).
Table 3.
Effect of Referral to a Community-Links Practitioner on Patient Outcomes
| Outcome Measure | Intervention Group vs Comparison Group
|
|
|---|---|---|
| Adjusted Effect Estimate (95% CI) | P Value | |
| EQ-5D-5L | 0.008 (−0.028 to 0.045) | .648 |
| ICECAP-A | −0.011 (−0.039 to 0.016) | .411 |
| WASAS | 0.05 (−1.37 to 1.48) | .940 |
| HADS-A | −0.41 (−0.99 to 0.18) | .172 |
| HADS-D | 0.09 (−0.49 to 0.68) | .753 |
| Exercise | 0.12 (−0.06 to 0.3) | .183 |
EQ-5D-5L = a standardized measure of self-reported health-related quality of life that assesses 5 dimensions at 5 levels of severity; HADS-A = Hospital Anxiety and Depression Scale, Anxiety; HADS-D = Hospital Anxiety and Depression Scale, Depression; ICECAP-A = Investigating Choice Experiments for the Preferences of Older People Capability Measure for Adults; SIMD = Scottish Index of Multiple Deprivation; WASAS = Work and Social Adjustment Scale.
Note: Intention-to-treat analysis. Mixed effects regression models at follow-up in relation to intervention group. Effect estimates represent mean differences. Each model adjusts for age, sex, SIMD, comorbidity, and significant baseline outcome measures as covariates and includes practice identifier as a random effects term.
Table 4.
Effect of Seeing a Community-Links Practitioner on Patient Outcomes
| Outcome Measure | Intervention Group vs Comparison Group | ||
|---|---|---|---|
| CLP Variable | Adjusted Effect Estimate (95% CI) | P Value | |
| EQ-5D-5L | Saw CLP once | 0.009 (−0.047 to 0.065) | .755 |
| Saw CLP twice | −0.041 (−0.117 to 0.036) | .298 | |
| Saw CLP 3+ | 0.071 (0.016 to 0.126) | .011 | |
| ICECAP-A | Saw CLP once | 0.004 (−0.038 to 0.046) | .841 |
| Saw CLP twice | −0.002 (−0.056 to 0.052) | .938 | |
| Saw CLP 3+ | 0.002 (−0.038 to 0.042) | .909 | |
| WASAS | Saw CLP once | −1.097 (−3.361 to 1.168) | .342 |
| Saw CLP twice | 1.146 (−1.766 to 4.058) | .441 | |
| Saw CLP 3+ | −0.795 (−3.042 to 1.452) | .488 | |
| HADS-A | Saw CLP once | −0.768 (−1.815 to 0.278) | .150 |
| Saw CLP twice | 0.064 (−1.194 to 1.322) | .920 | |
| Saw CLP 3+ | −1.380 (−2.339 to -0.421) | .005 | |
| HADS-D | Saw CLP once | −0.497 (−1.465 to 0.471) | .314 |
| Saw CLP twice | 1.256 (0.009 to 2.504) | .048 | |
| Saw CLP 3+ | −1.280 (−2.209 to –0.352) | .007 | |
| Exercise | Saw CLP once | 0.118 (−0.159 to 0.396) | .403 |
| Saw CLP twice | 0.064 (−0.292 to 0.420) | .726 | |
| Saw CLP 3+ | 0.339 (0.071 to 0.607) | .013 | |
CLP = community-links practitioner; EQ-5D-5L = a standardized measure of self-reported health-related quality of life that assesses 5 dimensions at 5 levels of severity; HADS-A = Hospital Anxiety and Depression Scale, Anxiety; HADS-D = Hospital Anxiety and Depression Scale, Depression; ICECAP-A = Investigating Choice Experiments for the Preferences of Older People Capability Measure for Adults; SIMD = Scottish Index of Multiple Deprivation; WASAS = Work and Social Adjustment Scale.
Note: Intention-to-treat analysis. Mixed effects regression models at follow-up in relation to intervention group. Effect estimates represent mean differences.
Each model adjusts for age, sex, SIMD, comorbidity, and baseline outcome level as covariates and includes practice identifier as a random effects term.
Figure 2.
Effect sizes of frequency of seeing a community-links practitioner on patient outcomes.
CLP = community-links practitioner; EQ-5D-5L = a standardized measure of self-reported health-related quality of life that assesses 5 dimensions at 5 levels of severity; HADS-A = Hospital Anxiety and Depression Scale, Anxiety; HADS-D = Hospital Anxiety and Depression Scale, Depression.
Because of the high correlation between the number of times patients consulted a CLP and the uptake of suggested community resources (Figure 1), it was not possible in the regression analysis to isolate the effects of consulting a CLP from the effects of attending a community resource.
DISCUSSION
This quasi-experimental cluster RCT evaluated the effects of a social prescribing initiative, the Glasgow Deep End LWP, in 15 general practices located in areas of high socioeconomic deprivation in Scotland. We were unable to prove that intervention was effective overall (intention-to-treat analysis). Subgroup analysis found significant improvements in the primary outcome and some secondary outcomes in patients who saw the CLP several times. However, this amounted to less than one-half of the patients referred. Caution is warranted in the interpretation of such subgroup analysis because of the possibility of reverse causality.21
Relationship With Published Literature
Despite the increasing popularity of social prescribing approaches, there is a limited evidence base on its effectiveness.5,7–9 Recent reviews have found few studies that have included a control group or used a randomized design. The RCT by Grant et al22 was the most similar to the current study in that it targeted patients with psychosocial problems (as identified by GPs), but the sample size was small, patients were generally not of low socioeconomic status (only 10% were in lowest 2 social classes), and follow-up was shorter (4 months) than in our study (9 months). They reported significant improvements in anxiety, depression, and overall general health. A more recent study of a link-worker intervention (with a matched control group), also conducted in a high-deprivation inner-city setting, found no effects of the intervention on anxiety, depression, or general health at 8 months’ follow-up.23 Similarly, another RCT in an older group, with a 3-year follow-up, found no effects of a link-worker approach.24 Our results, based on the intention-to-treat analysis, are thus in line with these other studies and add to the growing caution about the widely assumed benefits of such approaches.9
Qualitative studies have found that patients who engage with social prescribing initiatives generally find it a positive experience,23,25 but these studies also report that services are often not used to their full extent.23 Other barriers can include lack of buy-in from some GPs or funding for the third sector in a context of social care cuts.26 Our group recently published a qualitative evaluation of the views of the community organizations and the CLPs in the present study, which also concluded that such approaches may not achieve their potential because of ongoing economic austerity and lack of funding for the third sector.27
Strengths and Weaknesses
This is the largest study to date on the effects of social prescribing in deprived areas and one of only a few with a comparison group and cluster randomization. The study had adequate statistical power, with the achieved sample size being larger than the power calculation. The choice of quality of life as the primary outcome was appropriate, given that the intervention was generic rather than aimed at a particular problem or condition. We also included a wide range of validated secondary outcome measures relating to well-being.
Weaknesses of the study included its quasi-experimental design and the fact that it was not possible to have a matched comparison group at baseline. The fact that the research team was not involved in the design of the intervention (which was a service development) was unfortunate, because we could have contributed in terms of underpinning theory and evidence-based development. A longer duration of follow-up (beyond 9 months) would have been desirable, but this was not possible because of the funding limit. It was also not possible to include a cost-effectiveness analysis or access routine data on prescribing and health care utilization because the estimated costs for these data were not accepted by the funder. In addition, we did not have the information to link individual patients with the number and type of community resources used, and thus we cannot say whether some resources were more useful than others. With regard to self-reported exercise level, we used a short, simple measure rather than a better-validated questionnaire (such as the International Physical Activity Questionnaire28) in order to limit questionnaire length in the deprived population under study.
Implications for Policy, Practice, and Future Research
The management of patients with multiple complex health and social problems is a major global challenge with a limited evidence base.29 This type of complex multimorbidity is much more common in deprived than in affluent areas.30 Primary care clinicians and patients in deprived areas struggle to cope with such complexity.31,32 Given the ongoing existence of the inverse care law in deprived areas4,33,34 and the current shortage of GPs in the United Kingdom,35 social prescribing is an attractive option for policy makers as a potential way to reduce health inequalities. The findings of the present study question the effectiveness of this approach, however, with no benefits found in any measured outcome overall and possible benefit found only in those who repeatedly saw the CLP (which was less than one-half of those referred and which may be a spurious finding). Finding ways to improve the uptake and engagement rates of the intervention may lead to better overall outcomes, but further research is needed. Wide-scale deployment of social prescribing initiatives to reduce or mitigate health inequalities seems inappropriate until such research is conducted.
Acknowledgments
We are grateful to the practice staff and patients who took part in the study. Members of the evaluation advisory group, Andrea Williamson, Anne Ludbrook, Peter Craig, Jill Mutrie, Jane Ford, and Diane Stockton, gave helpful comments on the conduct of the evaluation. Peter Cawston, Mark Kelvin, and Chris Gourley facilitated data collection.
Footnotes
Conflicts of interest: authors report none.
To read or post commentaries in response to this article, see it online at http://www.AnnFamMed.org/content/17/6/518.
Author contributions: S.W.M. and S.W. were the principal investigators, and together with B.F. and C.O. they conceptualized and planned the study. All authors contributed to protocol development, and B.F. and S.W.M. liaised with practices and coordinated recruitment of patients. B.F. coordinated the trial. A.M. led the statistical analyses, which were undertaken by A.B. and G.J.-R. S.W.M. and S.W. wrote the first draft of the manuscript; all authors reviewed the manuscript for intellectual input, and all authors were involved in revisions, including the final revision.
Funding support: This study was funded by the NHS Health Scotland (contract 66450/1, 13/08/2014). The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the funder.
Supplementary materials: Available at http://www.AnnFamMed.org/content/17/6/518/suppl/DC1/.
References
- 1.Commission on Social Determinants of Health Closing the Gap in a Generation: Health Equity Through Action on the Social Determinants of Health. Geneva, Switzerland: World Health Organization; 2008. [DOI] [PubMed] [Google Scholar]
- 2.Dickman SL, Himmelstein DU, Woolhandler S. Inequality and the health-care system in the USA. Lancet. 2017; 389(10077): 1431–1441. [DOI] [PubMed] [Google Scholar]
- 3.Katikireddi SV, Skivington K, Leyland AH, Hunt K, Mercer SW. The contribution of risk factors to socioeconomic inequalities in multimorbidity across the lifecourse: a longitudinal analysis of the Twenty-07 cohort. BMC Med. 2017; 15(1): 152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mercer SW, Watt GCM. The inverse care law: clinical primary care encounters in deprived and affluent areas of Scotland. Ann Fam Med. 2007;5(6):503–510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wilson P, Booth A. Evidence to Inform the Commissioning of Social Prescribing. York, England: University of York, Centre for Reviews and Dissemination; 2015. [Google Scholar]
- 6.Rempel ES, Wilson EN, Durrant H, Barnett J. Preparing the prescription: a review of the aim and measurement of social referral programmes. BMJ Open. 2017; 7(10): e017734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mossabir R, Morris R, Kennedy A, Blickem C, Rogers A. A scoping review to understand the effectiveness of linking schemes from healthcare providers to community resources to improve the health and well-being of people with long-term conditions. Health Soc Care Community. 2015; 23(5): 467–484. [DOI] [PubMed] [Google Scholar]
- 8.Husk K, Blockley K, Lovell R, et al. What approaches to social prescribing work, for whom, and in what circumstances? A protocol for a realist review. Syst Rev. 2016; 5: 93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bickerdike L, Booth A, Wilson PM, Farley K, Wright K. Social prescribing: less rhetoric and more reality. A systematic review of the evidence. BMJ Open. 2017; 7(4): e013384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.The Health and Social Care Alliance Scotland Links Worker Programme, making links between people and their communities through their GP practice. https://www.alliance-scotland.org.uk/in-the-community/national-link-programme/ Accessed Aug 10, 2019.
- 11.Mercer SW, Fitzpatrick B, Grant L, et al. The Glasgow “Deep End” Links Worker Study Protocol: a quasi-experimental evaluation of a social prescribing intervention for patients with complex needs in areas of high socioeconomic deprivation. J Comorb. 2017; 7(1): 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hoffmann TC, Glasziou PP, Boutron I, et al. Better reporting of interventions: Template for Intervention Description and Replication (TIDieR) checklist and guide. BMJ. 2014; 348: g1687. [DOI] [PubMed] [Google Scholar]
- 13.Lenihan P, Iliffe S. Community-oriented primary care: a multidisciplinary community-oriented approach to primary care? J Community Appl Soc Psychol. 2001; 11(1): 11–18. [Google Scholar]
- 14.Watt G. What can the NHS do to prevent and reduce health inequalities? Br J Gen Pract. 2013; 63(614): 494–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.The EuroQol Group EQ-5D home page. https://www.euroqol.org Accessed Aug 10, 2019.
- 16.Al-Janabi H, Flynn TN, Coast J. Development of a self-report measure of capability wellbeing for adults: the ICECAP-A. Qual Life Res. 2012; 21(1): 167–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand. 1983; 67(6): 361–370. [DOI] [PubMed] [Google Scholar]
- 18.Mundt JC, Marks IM, Shear MK, Greist JH. The Work and Social Adjustment Scale: a simple measure of impairment in functioning. Br J Psychiatry. 2002; 180: 461–464. [DOI] [PubMed] [Google Scholar]
- 19.Bayliss EA, Ellis JL, Steiner JF. Seniors’ self-reported multimorbidity captured biopsychosocial factors not incorporated into two other data-based morbidity measures. J Clin Epidemiol. 2009; 62(5): 550–7.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.The Scottish Government The Scottish Index of Multiple Deprivation. http://www.gov.scot/Topics/Statistics/SIMD Accessed Aug 20, 2019.
- 21.Katz M. Study Design and Statistical Analysis: A Practical Guide for Clinicians. Cambridge, UK: Cambridge University Press; 2006. [Google Scholar]
- 22.Grant C, Goodenough T, Harvey I, Hine C. A randomised controlled trial and economic evaluation of a referrals facilitator between primary care and the voluntary sector. BMJ. 2000; 320(7232): 419–423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Carnes D, Sohanpal R, Frostick C, et al. The impact of a social prescribing service on patients in primary care: a mixed methods evaluation. BMC Health Serv Res. 2017; 17(1): 835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Andersson L. Intervention against loneliness in a group of elderly women: an impact evaluation. Soc Sci Med. 1985; 20(4): 355–364. [DOI] [PubMed] [Google Scholar]
- 25.Moffatt S, Steer M, Lawson S, Penn L, O’Brien N. Link worker social prescribing to improve health and well-being for people with long-term conditions: qualitative study of service user perceptions. BMJ Open. 2017; 7(7): e015203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bertotti M, Frostick C, Hutt P, Sohanpal R, Carnes D. A realist evaluation of social prescribing: an exploration into the context and mechanisms underpinning a pathway linking primary care with the voluntary sector. Prim Health Care Res Dev. 2018; 19(3): 232–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Skivington K, Smith M, Chng NR, Mackenzie M, Wyke S, Mercer SW. Delivering a primary care–based social prescribing initiative: a qualitative study of the benefits and challenges. Br J Gen Pract. 2018; 68(672): e487–e494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.International Physical Activity Questionnaire. https://sites.google.com/site/theipaq/.
- 29.Smith SM, Wallace E, O’Dowd T, Fortin M. Interventions for improving outcomes in patients with multimorbidity in primary care and community settings. Cochrane Database Syst Rev. 2016; 3: CD006560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012; 380(9836): 37–43. [DOI] [PubMed] [Google Scholar]
- 31.O’Brien R, Wyke S, Watt GGCM, Guthrie B, Mercer SW. The “everyday work” of living with multimorbidity in socioeconomically deprived areas of Scotland. J Comorb. 2014; 4(1): 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.O’Brien R, Wyke S, Guthrie B, Watt G, Mercer SW. An “endless struggle”: a qualitative study of general practitioners’ and practice nurses’ experiences of managing multimorbidity in socioeconomically deprived areas of Scotland. Chronic Illn. 2011; 7(1): 45–59. [DOI] [PubMed] [Google Scholar]
- 33.Hart JT. The inverse care law. Lancet. 1971; 1(7696): 405–412. [DOI] [PubMed] [Google Scholar]
- 34.McLean G, Guthrie B, Mercer SW, Watt GC. General practice funding underpins the persistence of the inverse care law: cross-sectional study in Scotland. Br J Gen Pract. 2015; 65(641): e799–e805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hobbs FDR, Bankhead C, Mukhtar T, et al. National Institute for Health Research School for Primary Care Research Clinical workload in UK primary care: a retrospective analysis of 100 million consultations in England, 2007-14. Lancet. 2016; 387(10035): 2323–2330. [DOI] [PMC free article] [PubMed] [Google Scholar]