Background:
This study aimed to assess the extent of rectus muscle damage in deep inferior epigastric perforator (DIEP) flap harvest and to evaluate its association with functional donor morbidity.
Methods:
A prospective cohort of 76 patients who underwent DIEP flap breast reconstruction was evaluated preoperatively and followed up for 1 year. Abdominal wall strength was assessed using the upper and lower rectus abdominis manual muscle function tests. Functional weakness was defined as a postoperative decrease in function by at least 2 scores. The effects of patient- and operation-related characteristics on adverse outcomes were also assessed.
Results:
The mean width of the transected rectus muscle was 2.2 cm (partial thickness, 1.8 cm; full thickness, 0.4 cm). The mean width ratio of the overall injured muscle to the entire bilateral muscle was 0.18. Muscle injury was more severe in the cases with bipedicled flap elevation and in those with 4 or more perforators harvested. Functional weakness was detected in 13 patients (17.1%). Multivariate analyses demonstrated that the width ratio of the muscle injury was an independent predictor of functional weakness. The width ratio achieved maximal discrimination regarding the rate of functional weakness at a threshold value of 0.12, indicating that functional weakness did not develop in all 19 cases with a width ratio of <0.12.
Conclusions:
The extent of rectus muscle injury during perforator dissection may be associated with functional donor morbidity after DIEP flap harvest. This may be beneficial in achieving proper balance between securing flap perfusion and preserving donor functions.
INTRODUCTION
The abdomen has served as a primary option for recruiting skin and soft tissue for autologous breast reconstruction; however, the developments of abdominal functional weakness and/or bulge or hernia are a main drawback.1,2 As the development of these functional morbidities is closely associated with the sacrifice of the rectus muscle and fascia during flap harvest, continued efforts have been made to preserve these structures, which lead to the emergence of the deep inferior epigastric perforator (DIEP) flap. This flap has gained popularity by virtue of the relatively low associated incidence of abdominal bulge or hernia as compared with that in other flaps.3–6
Nonetheless, DIEP flap harvest still poses the possibility of functional donor morbidity, and a small number of patients experience abdominal functional weakness postoperatively.5,7–9 The disruption of the intercostal nerve innervating the rectus muscle and the division of a portion of the muscle are suggested causes.10,11
In harvesting the DIEP flap, the rectus muscle is inevitably injured during perforator dissection. The extent of damage to the rectus muscle varies widely and could be influenced by the anatomical situation of the perforators. For instance, in some cases, the pedicle can be harvested only by splitting the muscle cleavage. In others, however, where harvesting multiple perforators derived from different muscle cleavage is required, or in situations where the perforator has a long or oblique intramuscular course, part of the rectus muscle needs to be unroofed, either in partial or full thickness, which might hinder the postoperative recovery of the rectus muscle function. Although it has been a long-standing presumption that the extent of rectus muscle injury during perforator dissection affects the development of functional donor morbidity, evidence supporting this is lacking. When transecting some portion of the muscle to capture adjacent perforators or generating another muscle cleavage to harvest a bipedicled flap is considered for securing the flap perfusion, surgeons may face difficulty in making confident decisions, as the extent of muscle injury that can be well tolerated in terms of preservation of donor function is unclear.
Therefore, we conducted a prospective cohort study to assess the extent of injury to the rectus muscle during flap harvest and evaluated its potential impact on the development of functional donor morbidity.
PATIENTS AND METHODS
Study Population
In accordance with the institutional review board oversight, this prospective cohort study included patients who underwent breast reconstruction using DIEP flaps consecutively from October 2015 to February 2017. Before the reconstructive operations, patients were identified for potential enrollment from the outpatient clinic of the senior author. The primary inclusion criteria were patients with breast cancer scheduled for DIEP flap breast reconstruction by a single surgeon and those who consented to study inclusion. Patients were followed up for 1 year postoperatively. Patients were excluded if their reconstructive modality was intraoperatively converted to other methods, including muscle-sparing transverse rectus abdominis myocutaneous (TRAM) flaps, or if they were lost to follow up.
During the study period, 87 patients provided consent and were enrolled initially. All the study participants underwent unilateral breast reconstruction using a DIEP flap without conversion to other methods. Eleven patients were lost to follow up, and 76 patients were finally analyzed.
Data Collection
Elevation of the DIEP flap and closure of the donor site were performed as described previously.5,12,13 A mesh was not used in all the study participants. The entire process of flap elevation was performed by a single attending surgeon, and donor site repair was performed in the same manner according to the stated protocol.5
Data regarding patient- and operation-related characteristics were gathered prospectively. The width of the transected rectus muscle was measured intraoperatively with a ruler just after the flap was harvested by the attending surgeon and recorded. Muscle transection was divided into partial and full thicknesses, and each width was measured. To calibrate the individual anatomical variability of the abdominal wall, we assessed the width ratio of the partially or fully transected rectus muscle to that of the whole muscle. Considering that bilateral rectus muscle complexes have synergistic, not separate, actions on the abdominal wall function, the width of the entire muscle of both sides was used to calculate the width ratio. Although intraoperative direct measurement of the width of the whole rectus muscle and identifying its medial and lateral margins would be more accurate, it requires additional subfascial dissection, which is not mandatory for harvesting perforators. To avoid this potentially additional donor morbidity, it was indirectly measured using preoperative computed tomographic angiography at the umbilical level. The development of postoperative donor complications was also assessed.
Outcome Measures
The abdominal muscle function was evaluated using the upper rectus abdominis manual muscle function test (URAMMFT) and the lower rectus abdominis manual muscle function test (LRAMMFT), which are frequently used for assessing the donor site function after the harvest of abdomen-based flaps (Table 1).9,14,15 The tests were conducted by ancillary physicians in the outpatient clinic, with examiners blinded to the specific data of the operation-related characteristics. All the participants were evaluated using the tests twice during the study period, before and 8–12 months after the operation.
Table 1.
Grading Scale for the URAMMFT and LRAMMFT
| Grade | Results | |
|---|---|---|
| URAMMFT | ||
| 0 | The patient cannot raise the head off the table, and there are no visible or palpable abdominal muscle contractions. | |
| 1 | The patient cannot raise the head off the table, but a visible or palpable abdominal muscle contraction occurs. | |
| 2 | The patient can raise the head off the table only. | |
| 3 | The patient can raise the inferior angles of the scapulae off the table with arms outstretched in full extension above the plane of the body. | |
| 4 | The patient can raise the inferior angles of the scapulae off the table with arms across the chest. | |
| 5 | The patient can raise the inferior angles of the scapulae off the table with hands clasped behind the head. | |
| LRAMMFT | ||
| 0 | No palpable contraction is present. | |
| 1 | The patient is unable to assume or maintain the position, but a palpable contraction of the rectus abdominis is present. | |
| 2 | The angle between the lower extremities and the table is greater than 75 degrees when the posterior pelvic tilt is lost. | |
| 3 | The angle between the lower extremities and the table is 70 degrees when the posterior pelvic tilt is lost. | |
| 4 | The angle between the lower extremities and the table is 30 degrees when the posterior pelvic tilt is lost. | |
| 5 | The angle between the lower extremities and the table is 0 degrees. The patient is able to lower the legs completely to the table without losing the posterior pelvic tilt. | |
LRAMMFT, lower rectus abdominis manual muscle function test; URAMMFT, upper rectus abdominis manual muscle function test.
The outcome of interest was the development of postoperative functional weakness in the abdomen, defined as a postoperative decrease by at least 2 scores from with the preoperative values in the URAMMFT and/or LRAMMFT.
Statistical Analyses
To investigate factors influencing the extent of rectus muscle injury, univariate and multivariate linear regression analyses were performed. The Wilcoxon signed-rank test was adopted to evaluate whether the scores of the muscle function tests changed significantly after the operation. The Pearson chi-square test was used for analyzing categorical variables, and the Mann-Whitney test was used for analyzing continuous variables. To investigate potential predictors of functional weakness, multivariate logistic regression analysis was conducted, starting with all patient- and operation-related variables. The backward selection model was chosen in the multivariate analyses. A value of P < 0.05 was considered significant.
RESULTS
The patient- and operation-related characteristics of the study population are listed in Table 2. The mean age of the patients was 48.6 years, and the mean body mass index (BMI) was 23.9 kg/m2. Of 76 DIEP flaps, 33 (43.4%) and 43 (56.6%) were harvested on the basis of a unipedicle and bipedicle, respectively. The mean number of harvested perforators was 4.2.
Table 2.
Patient- and Operation-related Characteristics of the Entire Cohort
| Variables | Value |
|---|---|
| Patient No. | 76 |
| Patient demographics | |
| Age, y | 48.6 y (±6.9) |
| BMI, kg/m2 | 23.9 (±2.5) |
| Overweight/obesity | 22 (28.9%) |
| Diabetes | 1 (1.3%) |
| Active smoking | 1 (1.3%) |
| Hypertension | 9 (11.8%) |
| Previous abdominal operation history | 10 (13.2%) |
| Midline vertical scar | 2 (2.6%) |
| Pfannenstiel incision scar | 8 (10.5%) |
| Abdominal circumference, cm | 86.9 (±7.6) |
| Operation related | |
| Timing | |
| Immediate | 44 (57.9%) |
| Delayed | 32 (42.1%) |
| Harvested flap size | |
| Width, cm | 29.2 (±4.9) |
| Height, cm | 12.7 (±1.1) |
| Harvested flap weight, g | 688.2 (±261.0) |
| Pedicle laterality | |
| Unipedicled | 33 (43.4%) |
| Single row based | 25 (32.9%) |
| Medial row based | 24 (31.6%) |
| Lateral row based | 1 (1.3%) |
| Both rows based (medial and lateral) | 8 (10.5%) |
| Bipedicled | 43 (56.6%) |
| No. harvested perforators | 4.2 (±1.7) |
| In unipedicled flap | 3.0 (±1.2) |
| In bipedicled flap | 5.2 (±1.7) |
Table 3 shows the degree of rectus muscle transection developed during the perforator dissection. The mean width of the rectus muscle transected was 1.8 cm in partial thickness and 0.4 cm in full thickness. The mean width of the entire bilateral rectus muscle was 12.5 cm on computed tomographic angiography. The mean width ratio of the muscle injured at least partially to the bilateral muscle was 0.18. In 51 cases (67.1%), only partial thickness muscle transection sufficed for the flap elevation, whereas in the other 25 cases (32.9%), full thickness transection (at any width) was performed. The width and width ratio of the overall injured muscles and those of the partially injured muscles differed significantly according to the pedicle laterality and number of harvested perforators. Multivariate linear regression analysis demonstrated that the number of harvested perforators significantly influenced the width ratio of the overall and partially injured muscles (P < 0.001). The other variables, including previous abdominal operation history and bipedicled flap harvest, did not influence the extent of the rectus muscle injury independently.
Table 3.
Extent of Rectus Muscle Injury Developed during the Perforator Dissection
| Width of the Transected Rectus Muscle (Width Ratio) | |||
|---|---|---|---|
| Partial Thickness | Full Thickness | Overall | |
| Entire cohort, cm | 1.8 (0.14) | 0.4 (0.03) | 2.2 (0.18) |
| BMI | |||
| Normal, cm | 1.9 (0.15) | 0.3 (0.03) | 2.2 (0.18) |
| Overweight/obesity, cm | 1.5 (0.12) | 0.6 (0.05) | 2.1 (0.17) |
| P | 0.143 | 0.108 | 0.252 |
| Previous abdominal operation history | |||
| Presence, cm | 2.0 (0.15) | 0.3 (0.02) | 2.2 (0.17) |
| Absence, cm | 1.7 (0.14) | 0.4 (0.04) | 2.1 (0.17) |
| P | 0.520 | 0.330 | 0.802 |
| Timing | |||
| Immediate, cm | 1.7 (0.14) | 0.4 (0.03) | 2.1 (0.17) |
| Delayed, cm | 1.8 (0.15) | 0.4 (0.03) | 2.2 (0.18) |
| P | 0.458 | 0.935 | 0.775 |
| Pedicle laterality | |||
| Unipedicled, cm) | 1.3 (0.11) | 0.5 (0.05) | 1.9 (0.16) |
| Bipedicled, cm | 2.1 (0.17) | 0.3 (0.02) | 2.4 (0.19) |
| P | 0.001 | 0.137 | 0.011 |
| No. harvested perforators | |||
| 1–3, cm | 1.2 (0.09) | 0.2 (0.02) | 1.4 (0.11) |
| 4 or more, cm | 2.2 (0.17) | 0.5 (0.04) | 2.6 (0.21) |
| P | <0.001 | 0.369 | <0.001 |
| Pedicle laterality and no. harvested perforators | |||
| Unipedicled on 1–3 perforators, cm | 1.0 (0.08) | 0.3 (0.02) | 1.3 (0.11) |
| Unipedicled on 4 or more perforators, cm | 1.9 (0.16) | 0.7 (0.06) | 2.6 (0.23) |
| Bipedicled on 1–3 perforators, cm | 1.6 (0.13) | 0.2 (0.02) | 1.8 (0.14) |
| Bipedicled on 4 or more perforators, cm | 2.3 (0.18) | 0.3 (0.02) | 2.6 (0.20) |
| P | <0.001 | 0.155 | <0.001 |
Postoperative donor site complications developed in 6 patients (7.9%), with delayed healing being the most common (3.9%). The complications were successfully treated with conservative management in the outpatient clinic. Development of an abdominal bulge was detected in 1 patient at 10 months after operation (Table 4).
Table 4.
Postoperative Complications
| Outcomes | Value, n (%) |
|---|---|
| Postoperative donor site complications | 6 (7.9) |
| Delayed healing | 3 (3.9) |
| Fat necrosis | 2 (2.6) |
| Seroma | 1 (1.3) |
| Bulge | 1 (1.3) |
| Hernia | 0 |
Table 5 shows the postoperative changes in the scores in the URAMMFT/LRAMMFT. The overall postoperative scores were maintained at >4 in both tests. The mean URAMMFT score significantly decreased postoperatively, whereas that of the LRAMMFT remained similar, showing only slightly elevated values. Consistent trends were observed regardless of patient age, BMI, previous abdominal operation history, reconstruction timing, and laterality of the pedicle.
Table 5.
Comparison of Preoperative and Postoperative Grades in the URAMMFT and LRAMMFT
| Variables | URAMMFT Grade (Mean) | LRAMMFT Grade (Mean) | ||||
|---|---|---|---|---|---|---|
| Preop | Postop | P | Preop | Postop | P | |
| Overall | 4.7 | 4.1 | <0.001 | 4.6 | 4.7 | 0.719 |
| Age | ||||||
| >50 y | 4.6 | 3.9 | 0.004 | 4.6 | 4.7 | 0.999 |
| ≤50 y | 4.8 | 4.3 | 0.003 | 4.7 | 4.7 | 0.648 |
| BMI | ||||||
| Normal | 4.70 | 4.27 | 0.002 | 4.73 | 4.75 | 0.658 |
| Overweight/obesity | 4.70 | 3.78 | 0.007 | 4.48 | 4.48 | 0.999 |
| Previous abdominal operation history | ||||||
| Presence | 4.45 | 3.55 | 0.021 | 4.18 | 4.82 | 0.289 |
| Absence | 4.76 | 4.24 | 0.001 | 4.74 | 4.68 | 0.286 |
| Reconstruction timing | ||||||
| Immediate | 4.71 | 4.29 | 0.004 | 4.64 | 4.76 | 0.804 |
| Delayed | 4.68 | 3.91 | 0.002 | 4.68 | 4.56 | 0.302 |
| Pedicle laterality | ||||||
| Unipedicled | 4.56 | 4.03 | 0.019 | 4.56 | 4.56 | 0.804 |
| Bipedicled | 4.80 | 4.20 | <0.001 | 4.73 | 4.76 | 0.999 |
LRAMMFT, lower rectus abdominis manual muscle function test; Postop, postoperative; preop, preoperative; URAMMFT, upper rectus abdominis manual muscle function test.
Postoperative functional weakness was detected in 13 patients (17.1%), most of whom were related to a decreased score in the URAMMFT. Two patients demonstrated decreased scores in both tests. Patients with postoperative functional weakness had a significantly higher BMI than those without it. With regard to the degree of muscle injury, the patients who developed functional weakness showed a significantly greater width ratio of the overall and partially injured muscles. The width and ratio of the full thickness muscle transection were not statistically significant between the groups (Table 6).
Table 6.
Comparison of Variables between Cases Developing Postoperative Functional Weakness and Those Not
| Variables | Postop Functional Weakness | P | |
|---|---|---|---|
| Absence (n = 63, 82.9%) | Presence (n = 13, 17.1%) | ||
| Patient demographics | |||
| Age, y | 47.7 (±6.7) | 51.1 (±8.2) | 0.176 |
| BMI, kg/m2 | 23.5 (±2.4) | 24.9 (±1.9) | 0.023 |
| Overweight/obesity | 15 (23.8%) | 7 (53.8%) | 0.030 |
| Diabetes | 1 (1.3%) | 0 | 0.647 |
| Active smoking | 1 (1.3%) | 0 | 0.647 |
| Hypertension | 6 (9.5%) | 3 (23.1%) | 0.169 |
| Previous abdominal operation history | 7 (11.1%) | 3 (23.1%) | 0.245 |
| Midline vertical scar | 1 (1.6%) | 1 (7.7%) | 0.211 |
| Pfannenstiel incision scar | 6 (9.5%) | 2 (15.4%) | 0.531 |
| Abdominal circumference | 86.2 (±7.2) | 87.2 (±7.7) | 0.817 |
| Operation related | |||
| Timing | 0.119 | ||
| Immediate | 39 (88.6%) | 5 (11.4%) | |
| Delayed | 24 (75.0%) | 8 (25.0%) | |
| Harvested flap size | |||
| Width | 28.7 (±4.7) | 32.5 (±5.2) | 0.025 |
| Height | 12.7 (±1.1) | 13.0 (±0.9) | 0.715 |
| Harvested flap weight | 674.3 (±247.4) | 816.7 (±314.7) | 0.166 |
| Rows of harvested perforators | 0.651 | ||
| Unilateral | 29 (87.9%) | 4 (12.1%) | 0.600 |
| Single row based | 22 (88.0%) | 3 (12.0%) | |
| Both rows based (medial and lateral) | 7 (87.5%) | 1 (12.5%) | |
| Bilateral | 34 (79.1%) | 9 (20.9%) | |
| No. harvested perforators | 4.2 (±1.8) | 4.6 (±1.1) | 0.310 |
| 1–3 (n, %) | 24 (85.7%) | 4 (14.3%) | 0.618 |
| 4 or more (n, %) | 39 (81.3%) | 9 (18.7%) | |
| Width of transected muscle, cm | 2.0 (±0.9) | 2.8 (±1.4) | 0.051 |
| Partial thickness | 1.7 (±1.1) | 2.3 (±0.8) | 0.019 |
| Full thickness | 0.3 (±0.7) | 0.4 (±1.1) | 0.546 |
| Width ratio of transected muscle to entire muscle | 0.17 (±0.08) | 0.22 (±0.10) | 0.087 |
| Partial thickness | 0.14 (±0.09) | 0.19 (±0.06) | 0.046 |
| Full thickness | 0.03 (±0.06) | 0.03 (±0.08) | 0.558 |
| Receiving chemotherapy after reconstruction | 14 (22.2%) | 2 (15.4%) | 0.582 |
Postop, postoperative.
Of the variables related to the extent of the rectus muscle injury, the width ratio of the overall injured muscle showed the greatest odds ratio with the lowest P value in the univariate analysis and was used in the subsequent multivariate analyses. The width ratio of the overall injured muscle had a significant influence on the development of functional weakness, after adjusting for other factors (Table 7). BMI and hypertension also significantly affected the development of functional weakness. Other variables, including the number of harvested perforators, laterality of pedicles, and previous abdominal operation history were not significantly associated with postoperative functional weakness.
Table 7.
Univariate and Multivariate Analyses for Predictors of Postoperative Functional Weakness
| Variables | Univariate Analysis | Multivariate Analysis | ||
|---|---|---|---|---|
| Unadjusted P | OR (95% CI) | Adjusted P | OR (95% CI) | |
| Age, y | 0.153 | 1.066 (0.977–1.163) | ||
| BMI, kg/m2 | 0.085 | 1.222 (0.973–1.537) | 0.031 | 1.374 (1.029–1.834) |
| Diabetes | 0.999 | 0 (0–0) | ||
| Active smoking | 0.999 | 0 (0–0) | ||
| Hypertension | 0.030 | 5.083 (1.176–21.980) | 0.017 | 10.135 (1.502–68.370) |
| Previous abdominal operation history | 0.047 | 4.286 (1.023–17.962) | ||
| Abdominal circumference | 0.671 | 1.017 (0.939–1.102) | ||
| Reconstruction timing | ||||
| Immediate | ref | ref | ||
| Delayed | 0.041 | 3.780 (1.053–13.563) | ||
| Harvested flap size | ||||
| Width | 0.086 | 1.108 (0.986–1.246) | ||
| Height | 0.328 | 1.351 (0.739–2.471) | ||
| Harvested flap weight | 0.175 | 1.002 (0.999–1.004) | ||
| Laterality of harvested perforators | ||||
| Unipedicled | ref | ref | ||
| Bipedicled | 0.748 | 1.221 (0.361–4.125) | ||
| No. harvested perforators | 0.878 | 1.027 (0.733–1.438) | ||
| 1–3 | ref | ref | ||
| 4 or more | 0.585 | 1.427 (0.398–5.112) | ||
| Width of transected muscle | 0.038 | 1.802 (1.033–3.145) | ||
| Partial thickness | 0.094 | 1.635 (0.919–2.908) | ||
| Full thickness | 0.438 | 1.325 (0.651–2.698) | ||
| Width ratio of transected muscle | 0.019 | 6802.992 (4.169–11109986.229) | 0.003 | 253680.851 (42.782–150424409.694) |
| Partial thickness | 0.063 | 863.385 (0.689–1081175.403) | ||
| Full thickness | 0.468 | 26.275 (0.004–180662.424) | ||
| Chemotherapy after reconstruction | 0.219 | 0.266 (0.032–2.204) | ||
CI, confidence interval; OR, odds ratio; ref, reference.
As the width ratio of the overall injured muscle showed the highest odds with statistical significance, a receiver operating characteristic curve analysis was performed to calculate an optimal cutoff width ratio that has the greatest discrimination between cases with and without functional weakness. Maximal statistical significance was achieved at a width ratio of the muscle injury threshold of 0.12. Nineteen patients had a rectus muscle injury width ratio of <0.12, and the other 57 had ≥0.12. The rate of development of functional weakness was remarkably different; none of the patients with a width ratio of <0.12 had a functional weakness postoperatively, whereas 22.8% of those with a width ratio of ≥0.12 had a postoperative functional weakness (P = 0.022). Two representative cases are shown in Figures 1 and 2.
Fig. 1.
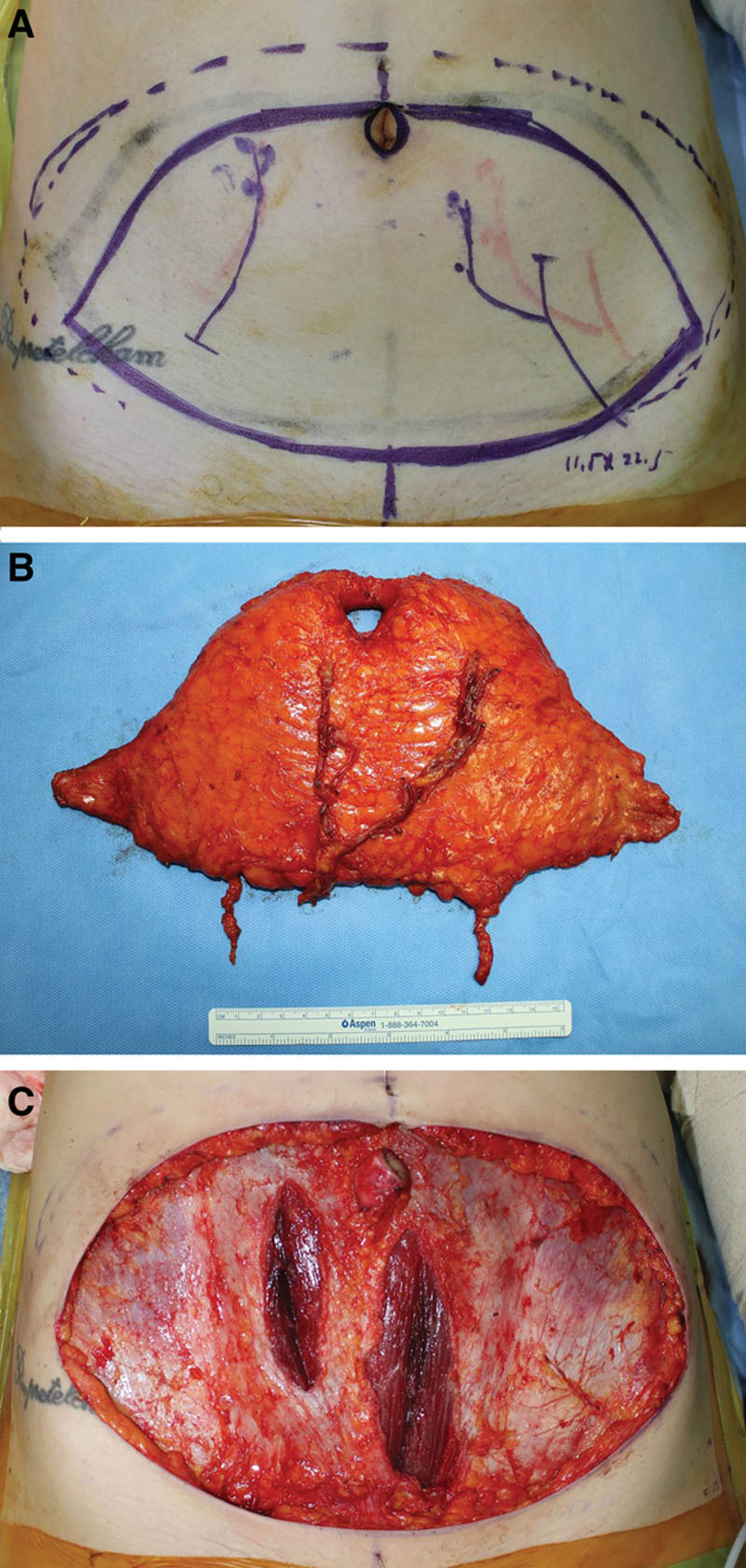
A 37-year-old woman underwent immediate breast reconstruction using a DIEP flap. As transfer of almost the entire flap was needed, harvest of a bipedicled flap was planned (A) and executed. On her right abdomen, making 1 muscle cleavage sufficed for harvesting 2 medial row-based perforators without severing any muscle. On the left side, partial thickness muscle transection 0.5 cm in width was performed during dissecting 3 medial row-based perforators (B). The width ratio of the overall injured muscle was 0.04 (C). Her both preoperative URAMMFT and the LRAMMFT scores were 5, which remained the same after the operation.
Fig. 2.
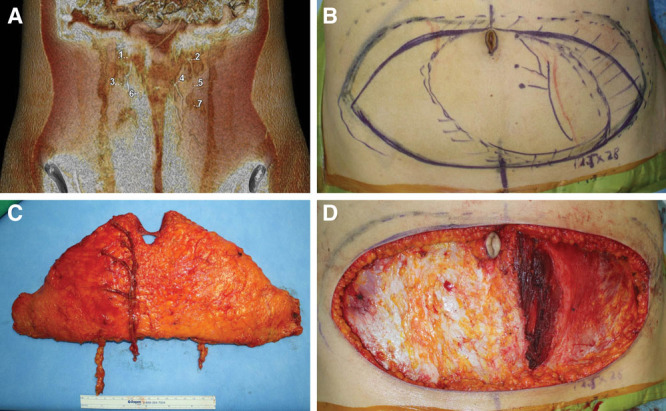
A 50-year-old woman visited our clinic for right breast reconstruction after completing oncological treatments. As no dominant perforators were identified on preoperative computed tomographic angiography (A), elevation of a unipedicled flap incorporating 4 small perforators (Nos. 2, 4, 5, and 7) was planned (B). A DIEP flap based on 4 medial row perforators was elevated as planned (C). The weight of the harvested flap was 653 g, 73% (479 g) of which was inset finally. A 1.5-cm-wide partial myotomy and total myotomy of the same width were found in the donor site, showing the width ratio of the overall injured rectus muscle (3 cm) to the entire bilateral muscle (10 cm) of 0.3 (D). She showed a score of 5 in both the URAMMFT and LRAMMFT preoperatively, which decreased by 2 scores in the URAMMFT and by 1 in the LRAMMFT postoperatively.
Subgroup analyses were conducted in accordance with the pedicle laterality. In the unipedicled flap harvest group, 12.5% of the patients had a postoperative functional weakness and showed a significantly larger width and ratio of transected muscle than the patients without morbidity. In the group of bipedicled flap harvest, 20.5% of cases showed functional morbidity; however, the extent of muscle injury was not significantly different (Table 8). The multivariable analyses for identifying the independent predictors in each group were not performed owing to the small number of cases.
Table 8.
Comparison of the Extent of Muscle Injury in the Groups of Unipedicled and Bipedicled Flap Harvest
| Group | Postop Functional Weakness | P | |
|---|---|---|---|
| Absence | Presence | ||
| Unipedicled flap harvest | |||
| No. cases | 28 (87.5%) | 4 (12.5%) | |
| Width of transected muscle (ratio) | |||
| In partial thickness, cm | 1.3 (0.10) | 2.1 (0.19) | 0.054 |
| In full thickness, cm | 0.4 (0.03) | 0.5 (0.05) | 0.721 |
| Overall, cm | 1.7 (0.14) | 2.6 (0.24) | 0.047 |
| Bipedicled flap harvest | |||
| No. cases | 35 (79.5%) | 9 (20.5%) | |
| Width of transected muscle (ratio) | |||
| In partial thickness, cm | 2.0 (0.16) | 2.4 (0.18) | 0.261 |
| In full thickness, cm | 0.3 (0.02) | 0.4 (0.03) | 0.456 |
| Overall, cm | 2.3 (0.19) | 2.8 (0.21) | 0.606 |
Postop, postoperative.
DISCUSSION
The present study prospectively assessed functional changes of the anterior abdominal wall after DIEP flap harvest and investigated several variables associated with postoperative functional impairments. The degree of rectus muscle injury that occurred during perforator dissection was objectively measured, and its impact on the adverse outcomes was evaluated. To our knowledge, this is the first prospective study to investigate whether the extent of rectus muscle injury could influence the development of functional donor morbidity in DIEP flap harvest. The enrolled patients were relatively homogenous in nature in terms of proficiency of surgical procedures.
In this study, the URAMMFT and LRAMMFT were used to evaluate the functional donor morbidity of the DIEP flap. The strengths of the manual muscle function test can lie in its being simple, practical, and easily reproducible and are closely associated with actual daily activities, which is further supported by the popularity of this measurement in previous studies.9,16
We found that >80% of the study population did not have functional weakness in the donor sites. The mean score in both the URAMMFT and LRAMMFT was maintained at >4 after operation. This favorable finding validates the results of previous studies and could reconfirm that the DIEP flap harvest generally leads to a low functional morbidity at the donor site.
Nevertheless, the finding was also not negligible in that approximately 17% of patients showed downgrading by at least 2 levels in either the URAMMFT or LRAMMFT. This suggests that some functional impairment could develop postoperatively in a few patients who have undergone DIEP flap harvest. Consistent findings have been reported in previous studies,7,9,17,18 demonstrating a decrease in the strength or contractility of the rectus muscle by varying degrees after DIEP flap harvest, although its extent may not be as much as that after TRAM flap harvest.4,6,9 We can assume that the donor site of the DIEP flap, although potentially safer than that of other abdominal flaps, might not be completely free from postoperative functional impairment. Especially, the present study demonstrated that patients with high BMI and hypertension showed significantly increased odds for developing postoperative functional weakness regardless of impacts of other factors, including the degree of rectus muscle damage.
Obesity can reduce the wound-healing potential,19 which can hinder the functional recovery of the donor site. Hypertension could be associated with delayed wound healing,20 and potentially detrimental effects of antihypertensive medications on wound healing also may affect the outcomes.21 Thus, patients with these characteristics might need to be informed of a potential risk of functional donor morbidity before surgery.
Whether the extent of rectus muscle injury could influence the development of functional donor weakness was of primary interest in this study. We found that with an increase in injury, either in partial or full thickness, of the rectus abdominis during perforator dissection, the risk of developing postoperative functional weakness elevated significantly. When the harvest of multiple perforators not aligned along the main cleavage line is required owing to a lack of a dominant perforator or the harvest of a single perforator with a long and oblique intramuscular course is necessary, transecting or unroofing the rectus muscle with variable width and depth may be unavoidable. This transversely severed muscle would not be rigidly repaired straightforward and may be healed with fibrosis or scarring even in the long term. Although the muscle volume may appear to be maintained without a significant reduction on postoperative radiological examinations,22 this incomplete healing of the transected muscle may lead to suboptimal functional recovery and functional weakness ultimately. In cases with considerable rectus muscle injury, although no rectus muscle is harvested within the flap itself, the sequelae in the donor site may likely appear to be functionally similar with that of muscle-sparing TRAM flap harvest.23 That is, all DIEP flaps may not be the same in terms of functional donor morbidity.10
The width ratio of the injured muscle achieved maximal discrimination for the rate of functional weakness at a threshold value of 0.12. Moreover, the functional weakness did not develop in all 19 patients with a width ratio of <0.12. Of course, this threshold value may change with further investigations, as our value of 0.12 was calculated on the basis of a few cases. Nonetheless, we could assume that conducting myotomy, mostly in partial thickness, to a certain extent might be permissible in terms of donor site functional preservation, whereas the muscle injury above it may contain high risks of functional impairments. It is likely that perforators placed close to a main targeted perforator, up to approximately 1.5 cm in unilateral cases and 0.75 cm on each side in bilateral cases [crudely calculated on the basis of the mean width of the bilateral rectus muscle (12.5 cm in our data)], may be hooked up via a partial myotomy without a significant burden in terms of functional donor morbidity
Although we expected that the width of the rectus muscle transected in full thickness could influence the development of functional weakness more than that in partial thickness, no significant association was observed. This result is likely because a total myotomy was conducted in only a few patients, and even if performed, its extent was very small (0.4 cm on average). Future studies need to evaluate the influence of the depth of the rectus muscle injury on functional donor morbidity more specifically.
This study demonstrated that the odds for developing functional weakness were not significantly different between cases of unipedicled and bipedicled flap harvest. As expected, the harvest of the bipedicled flap left a significantly greater extent of overall muscle injury than the unipedicled flap; however, this difference did not significantly elevate the risk of functional weakness. Generally, only a slight muscle injury occurs during the secondary pedicle harvest, as a shorter pedicle with a smaller number of perforators is usually harvested as compared with that for the primary pedicle.24 We can assume that making another muscle cleavage for a bipedicled flap harvest to augment flap perfusion might not affect donor site function seriously as long as the added muscle injury is not severe.
The present study has several limitations. First, quantification of the degree of intercostal nerve injury, which could affect the postoperative function of the rectus muscle, was lacking. However, every effort was made to preserve the intercostal nerves, especially those running near the arcuate line, which innervates the rectus muscle dominantly (type 2 nerves),11,25 for reducing the risk of functional donor morbidity. This was further supported by the very low incidence of postoperative abdominal bulge and hernia during the study period. In our series, when a unipedicled flap was harvested, medial row perforators were favored to the lateral ones to capture more tissue from the contralateral side to the pedicle. Usually, in the medial row perforator-based DIEP flap, rectus muscle injury may play a greater role than neural disruption in developing functional weakness, given that the innervation from the intercostal nerve to the large portion of the muscle lateral to the cleavage can be mostly preserved. This situation is likely to be even more advantageous to evaluate the genuine effects of rectus muscle injury on the functional donor morbidity; however, whether similar findings may be observed in lateral row perforator-based DIEP flaps requires further verifications. The decreases in the scores in the manual muscle function tests could be multifactorial and may not be solely attributable to the functional sequelae of the rectus muscle. Postoperative rehabilitations or patients’ own habitus also could affect the functional recovery of the abdominal wall. The heterogenous characteristics of the study population were also an inherent limitation of the present study. Especially unipedicled and bipedicled flap harvests are different in terms of the degree of disruption of the rectus muscle and fascia, as shown in Table 8, which can act as a confounder; however, multivariable analyses could not be conducted because of the small number of cases in each group. Moreover, analyzing many variables with a small sample size could reduce the statistical power. In the present study, the time of postoperative evaluation of abdominal muscle function was variable across the cohorts, ranging from 8 to 12 months after operation, which could affect the outcomes. Further large-scale well-controlled studies would be required to make more definite conclusions. Lastly, the relatively lower BMI of the study population than those of other Western populations might make generalization of our results difficult.
CONCLUSIONS
Our results suggest that the extent of rectus muscle injury during perforator dissection might affect the patient’s postoperative recovery and risk of functional sequelae. As the injury to the rectus muscle worsens, the risk of developing functional weakness may also increase. Although further large-scale studies are required to verify these results, this information may be helpful not only in patient counseling and preoperative planning but also in intraoperative decision-making to balance between achieving a more robust flap perfusion and preserving more donor site function.
Footnotes
Published online 29 October 2019.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
REFERENCES
- 1.Arnez ZM, Khan U, Pogorelec D, et al. Rational selection of flaps from the abdomen in breast reconstruction to reduce donor site morbidity. Br J Plast Surg. 1999;52:351–354. [DOI] [PubMed] [Google Scholar]
- 2.Chang EI, Chang EI, Soto-Miranda MA, et al. Comprehensive analysis of donor-site morbidity in abdominally based free flap breast reconstruction. Plast Reconstr Surg. 2013;132:1383–1391. [DOI] [PubMed] [Google Scholar]
- 3.Knox AD, Ho AL, Leung L, et al. Comparison of outcomes following autologous breast reconstruction using the DIEP and pedicled TRAM flaps: a 12-year clinical retrospective study and literature review. Plast Reconstr Surg. 2016;138:16–28. [DOI] [PubMed] [Google Scholar]
- 4.Man LX, Selber JC, Serletti JM. Abdominal wall following free TRAM or DIEP flap reconstruction: a meta-analysis and critical review. Plast Reconstr Surg. 2009;124:752–764. [DOI] [PubMed] [Google Scholar]
- 5.Paik JM, Lee KT, Jeon BJ, et al. Donor site morbidity following DIEP flap for breast reconstruction in Asian patients: is it different? Microsurgery. 2015;35:596–602. [DOI] [PubMed] [Google Scholar]
- 6.Zhong T, Novak CB, Bagher S, et al. Using propensity score analysis to compare major complications between DIEP and free muscle-sparing TRAM flap breast reconstructions. Plast Reconstr Surg. 2014;133:774–782. [DOI] [PubMed] [Google Scholar]
- 7.Bajaj AK, Chevray PM, Chang DW. Comparison of donor-site complications and functional outcomes in free muscle-sparing TRAM flap and free DIEP flap breast reconstruction. Plast Reconstr Surg. 2006;117:737–746; discussion 747. [DOI] [PubMed] [Google Scholar]
- 8.Chun YS, Sinha I, Turko A, et al. Comparison of morbidity, functional outcome, and satisfaction following bilateral TRAM versus bilateral DIEP flap breast reconstruction. Plast Reconstr Surg. 2010;126:1133–1141. [DOI] [PubMed] [Google Scholar]
- 9.Selber JC, Nelson J, Fosnot J, et al. A prospective study comparing the functional impact of SIEA, DIEP, and muscle-sparing free TRAM flaps on the abdominal wall: part I. Unilateral reconstruction. Plast Reconstr Surg. 2010;126:1142–1153. [DOI] [PubMed] [Google Scholar]
- 10.Weissler JM, Albino FP, Carney MJ, et al. Revisiting the abdominal donor site: introducing a novel nomenclature for autologous breast reconstruction. Plast Reconstr Surg. 2017;140:1110–1118. [DOI] [PubMed] [Google Scholar]
- 11.Lee BT, Chen C, Nguyen MD, et al. A new classification system for muscle and nerve preservation in DIEP flap breast reconstruction. Microsurgery. 2010;30:85–90. [DOI] [PubMed] [Google Scholar]
- 12.Lee KT, Eom Y, Jeon BJ, et al. Vertical spacing of perforators in deep inferior epigastric perforator flap breast reconstruction can affect the outcomes. Plast Reconstr Surg. 2018;142:319–329. [DOI] [PubMed] [Google Scholar]
- 13.Lee KT, Mun GH. Volumetric planning using computed tomographic angiography improves clinical outcomes in DIEP flap breast reconstruction. Plast Reconstr Surg. 2016;137:771e–780e. [DOI] [PubMed] [Google Scholar]
- 14.Sarti MA, Monfort M, Fuster MA, et al. Muscle activity in upper and lower rectus abdominus during abdominal exercises. Arch Phys Med Rehabil. 1996;77:1293–1297. [DOI] [PubMed] [Google Scholar]
- 15.Krause DA, Youdas JW, Hollman JH, et al. Abdominal muscle performance as measured by the double leg-lowering test. Arch Phys Med Rehabil. 2005;86:1345–1348. [DOI] [PubMed] [Google Scholar]
- 16.Nelson JA, Tecci MG, Lanni MA, et al. Function and strength after free abdominally based breast reconstruction: a 10-year follow-up. Plast Reconstr Surg. 2019;143:22e–31e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Futter CM, Webster MH, Hagen S, et al. A retrospective comparison of abdominal muscle strength following breast reconstruction with a free TRAM or DIEP flap. Br J Plast Surg. 2000;53:578–583. [DOI] [PubMed] [Google Scholar]
- 18.Blondeel N, Vanderstraeten GG, Monstrey SJ, et al. The donor site morbidity of free DIEP flaps and free TRAM flaps for breast reconstruction. Br J Plast Surg. 1997;50:322–330. [DOI] [PubMed] [Google Scholar]
- 19.Pierpont YN, Dinh TP, Salas RE, et al. Obesity and surgical wound healing: a current review. ISRN Obes. 2014;2014:638936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ahmed AA, Mooar PA, Kleiner M, et al. Hypertensive patients show delayed wound healing following total hip arthroplasty. PLoS One. 2011;6:e23224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Park JW, Mun GH. Comparative analysis of the effect of antihypertensive drugs on the survival of perforator flaps in a rat model. Microsurgery. 2018;38:310–317. [DOI] [PubMed] [Google Scholar]
- 22.Seal SKF, Hewitt MK, Martin ML, et al. Preoperative and postoperative assessment of rectus abdominis muscle size and function following DIEP flap surgery. Plast Reconstr Surg. 2018;141:1261–1270. [DOI] [PubMed] [Google Scholar]
- 23.Tokumoto H, Akita S, Arai M, et al. A comparison study of deep muscle sparing transverse rectus abdominis musculocutaneous flap for breast reconstruction. Microsurgery. 2019. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 24.Kim SY, Lee KT, Mun GH. Computed tomographic angiography-based planning of bipedicled DIEP flaps with intraflap crossover anastomosis: an anatomical and clinical study. Plast Reconstr Surg. 2016;138:409e–418e. [DOI] [PubMed] [Google Scholar]
- 25.Rozen WM, Ashton MW, Kiil BJ, et al. Avoiding denervation of rectus abdominis in DIEP flap harvest II: an intraoperative assessment of the nerves to rectus. Plast Reconstr Surg. 2008;122:1321–1325. [DOI] [PubMed] [Google Scholar]


