Background:
Appropriate management of soft tissue injury associated with orthopedic trauma is challenging in low- and middle-income countries (LMICs) due to the lack of available reconstructive surgeons. The Surgical Management and Reconstructive Training (SMART) course teaches orthopedic surgeons reconstructive techniques aimed at improving soft tissue management. This study aims to identify additional barriers to implementing these techniques for surgeons in LMICs who have attended SMART courses.
Methods:
This is a mixed-methods study including a Likert-scale-based survey administered to 150 surgeons from LMICs attending the 2018 SMART courses in Tanzania and San Francisco and key informant interviews with 20 surgeons who perform soft tissue coverage procedures.
Results:
In surveys, respondents reported inadequate local plastic surgeon availability for lower extremity fracture requiring muscle flaps (88%). Surgeons agreed that flap surgeries are important for patients with significant soft tissue injury following open fractures (97%). They reported inadequate access to instruments, such as dermatomes (59%) and Humby knives (32%), and senior-level support (31%). Fewer than half of surgeons with flap experience (n = 85) felt confident in training peers (45%). In interviews, delays in returning patients to operating rooms were frequently cited as a barrier (90%).
Conclusions:
Our study demonstrates that soft tissue procedures are perceived as a high priority among orthopedic surgeons, but there are multiple barriers, including a lack of plastic surgeons, and many modifiable barriers including a lack of surgical equipment, peer training, and senior colleague support.
INTRODUCTION
Musculoskeletal injuries are a major global health problem and represent a growing burden of disease in low- and middle-income countries (LMICs).1 Surgeons in LMICs continue to face challenges with the care of complex orthopedic trauma, which is often accompanied by soft tissue defects requiring coverage procedures, such as skin grafts or flaps.2 Without proper management of soft tissue injuries, patients experience increased risk of infections, amputations, and even death.3 Interventions aimed at addressing soft tissue surgical management in LMICs have been shown to improve patient outcomes, and increased access to plastic surgeons capable of performing flap procedures can reduce long-term disability.4–7
However, there remains a lack of local plastic surgeons with the necessary training to perform these complex procedures.1,3,8–12 This is seen in countries such as Zambia, Ghana, and Uganda where there is a severe shortage of surgeons with 1 surgeon for 10 million people in Zambia, 6 for 22 million people in Ghana, and 3 for 27 million people in Uganda.4 There is a massive unmet burden of surgical disease with 66% of the surgical disease DALYs due to conditions typically treated by plastic surgeons.13,14 Thus, there has been a subsequent call for plastic and orthopedic surgeons from high-income countries to engage in soft tissue coverage procedure training for surgeons in LMICs.7,15,16 The advent of ortho-plastic surgery and its subsequent success may represent a possible solution for addressing the surgical disease burden.17,18 Training orthopedic surgeons in locations where plastic surgeons are not readily available may be an effective intervention for scaling patient access to soft tissue coverage procedures in LMICs.11,19,20 The Surgical Management and Reconstructive Training (SMART) course curriculum is 1 such effort to train orthopedic surgeons from low-resource settings in managing soft tissue injuries and complex fractures by introducing the principles of ortho-plastic surgery and the reconstructive ladder to surgeons who must understand plastic surgery principles to address limb trauma. Course educators emphasize lower leg soft tissue coverage using gastrocnemius, soleus, and reverse sural flaps that can easily be performed without loupes, an operating microscope, or microvascular instruments.9
SMART courses have been offered annually in San Francisco, Nepal, and Tanzania and have involved hundreds of participants from 25 countries since 2010.3 A study of the 2012 San Francisco SMART course demonstrated that SMART course participants successfully implemented the curriculum with 34 participants collectively performing 554 successful flap surgeries.3 In addition, investigators have reported SMART course efficacy in Tanzania and Nepal, where SMART course participants increased the number of flaps performed, the success rate of these flaps, and their confidence in completing these procedures.21,22 Despite these successes, there are still a large number of attendees who have not been able to implement the course’s teachings. It is unclear whether this is due to teaching model deficiencies, particularly as it pertains to nonmicrovascular surgical reconstruction. These surgical techniques are generally regarded as having a shorter learning curve than more advanced techniques involving microvascular surgery and the higher rungs of the reconstructive ladder.23 The lack of implementation begs the question if there are other resource limitations and barriers preventing local surgeons from performing flap procedures. Various resource constraints have been cited in LMICs such as lack of perioperative flap monitoring, available and well-equipped operating rooms (ORs), and good laboratory support services.24 This study aims to identify the barriers to performing soft tissue reconstruction among SMART course participants and provide commentary on the obstacles to surgical education delivery more broadly in LMICs.
METHODS
Investigators developed a mixed-methods study protocol that utilized a survey and semistructured interviews. The study was supported by the Tanzanian host institution, approved as exempt by the UCSF Institutional Review Board, and consent was obtained from all participants. Convenience sampling was used to survey 150 practicing orthopedic surgeons from 21 different LMICs in attendance of the 2018 SMART courses in Tanzania (110) and San Francisco (40). Investigators created a survey instrument based on the review of the surgical literature25–27 and expert opinion from SMART course facilitators and local partners at the Tanzanian institution. The survey assessed participants’ experience with skin grafts, muscle and/or fasciocutaneous flap procedures, confidence level in managing these operations, and potential barriers to performing these surgeries in their clinical practice. Confidence levels and barrier perceptions were assessed using a 6-point Likert scale.
Semistructured interviews were conducted with 20 orthopedic surgeons who perform muscle and/or fasciocutaneous flap procedures in their local practice. Participants were interviewed for 15 minutes using open-ended questions to elicit information regarding barriers to performing muscle and/or fasciocutaneous flap surgeries. Interview responses were recorded, transcribed, and inductively coded using thematic analysis by the principal author (JTH). Common themes were identified and categorized by barrier type.
Descriptive statistical analyses were used to summarize survey responses and semistructured interview themes. The paired t test was used to compare averages in barrier attitudes based on participants’ previous experience with soft tissue reconstruction surgeries.
RESULTS
Demographics
The majority of participants were East or West African (87%) and employed at a teaching hospital (83%). The majority of participants reported a training level of attending/specialist (52%) with 1–5 years of work experience or greater (83%) (Table 1). Among all participants, 88% reported inadequate local plastic surgeon availability for lower extremity fractures requiring muscle flap procedures, and 50% reported that the orthopedics department is responsible for performing muscle flap surgeries in their hospital. More than half of all participants reported attending at least 1 SMART course in the past (56%). Among respondents who had performed flap procedures in the past (57%), the majority self-reported performing fewer than 3 muscle and/or fasciocutaneous flap surgeries in the last year.
Table 1.
Self-reported Demographics of Survey Participants
| n (%) | ||
|---|---|---|
| Previously attended a SMART course | 84 (56) | |
| Has performed muscle flap in the past | 86 (57) | |
| Has non-SMART course flap training | 14 (9) | |
| Practice setting | ||
| East or West Africa | 130 (87) | |
| Southeast Asia | 10 (7) | |
| South or Central America and Caribbean | 7 (5) | |
| Employed at a teaching hospital | 125 (83) | |
| Training level | ||
| Attending/specialist | 78 (52) | |
| Years since completing residency | ||
| <1 y | 11 (14) | |
| 1–5 y | 37 (47) | |
| 5–10 y | 12 (15) | |
| >10 y | 16 (21) | |
Survey Results
Surgeons agreed that flap procedures are important for their patients (97%), that their local colleagues understand the importance of these operations (92%), and that orthopedic surgeons should be responsible for performing these surgeries in their practice (89%). However, 31% of participants reported that they did not have support from senior faculty to perform these procedures, and 67% of respondents reported that surgeons are not adequately compensated for performing flap surgeries. Surgeons also noted that cost to patients may be a barrier to performing flap procedures (64%). Notably, many respondents reported a lack of access to surgical equipment, such as dermatomes and Humby knives, which are necessary for completing skin grafts (59% and 32% respectively). Lack of access to Doppler probes, surgical loupes, and negative pressure wound therapy dressings was also reported (81%, 78%, and 55%, respectively) (Fig. 1).
Fig. 1.
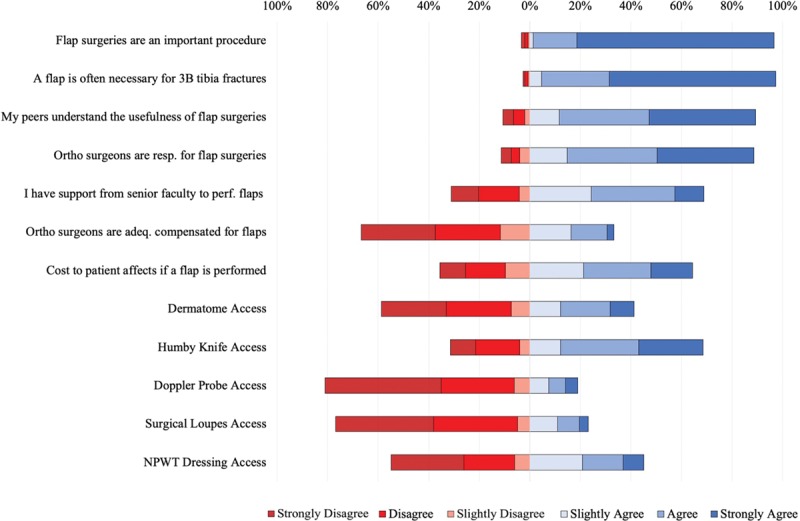
Likert scale results for all participants (n = 150). NPWT, negative pressure wound therapy.
Among survey participants with experience performing flaps (57%), many reported not feeling confident in their ability to perform common soft tissue procedures: gastrocnemius flaps (22%), soleus flaps (31%), reverse sural flaps (60%), and skin grafts (18%). Only 58% of respondents firmly reported (strongly agreed + agreed) to being comfortable managing flap and/or skin graft complications, and only 45% of surgeons firmly reported feeling confident in training their peers. Surgeons also encountered barriers involving the OR. Fifty-two percent of surgeons firmly reported having access to the OR for enough time to perform a flap surgery, and only 46% of surgeons firmly reported that a patient’s flap operation could be done on the same day as fracture fixation. When the operation was delayed, only 62% of surgeons firmly reported that they have access to return to the OR to perform a flap. Only 29% of surgeons firmly reported that their patients could access necessary supplies after a flap surgery (Fig. 2).
Fig. 2.
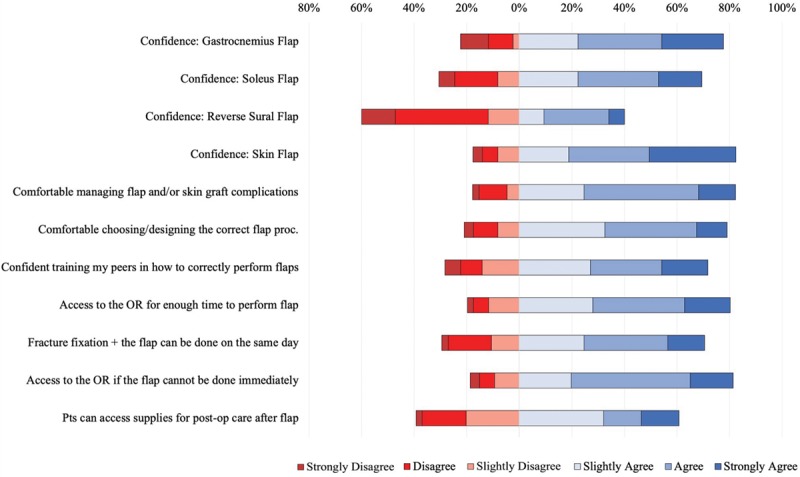
Likert scale results for surgeons with previous flap experience (n = 86).
Interview Results
All surgeons who participated in semistructured interviews reported that flap surgeries were not being done for the number of patients who require these procedures at their institution. When asked about potential barriers to soft tissue reconstruction procedures, surgeons reported significant delays in returning patients to the OR for flap surgeries following initial bony fixation (90%), and a lack of local orthopedic colleagues with adequate flap training (85%). When surgeons wanted to return patients to the OR for flap procedures, many interviewees reported a lack of OR availability (85%), and that these barriers are related to the excessive burden of other surgical cases at their institution (70%). In concordance with survey findings, surgeons’ commonly reported a lack of access to skin-grafting equipment; 85% of surgeons reported an insufficient number of Humby knives and/or dermatomes. Many surgeons also reported that flap surgeries at their institution were viewed as elective and/or nonemergency cases (65%) and that there was a lack of local peer-to-peer training in flap procedures (65%) (Table 2).
Table 2.
Semistructured Interview Coded Themes and Selected Quotes
| Coded Barrier Themes | Selected Quotes | Reported (%) |
|---|---|---|
| Delay in returning patients to the OR following bony fixation | “We have so many new patients coming, that whenever surgical debridement is done, the patient is pushed into the wards. To bring that patient back to theater for washout is challenging.” | 90 |
| Lack of orthopedic colleagues with adequate flap surgery training | “Most of the rest of the team is younger now. So they haven’t done flap courses before. So they wouldn’t be comfortable doing a flap procedure.” | 85 |
| Lack of appropriate skin-grafting equipment | “There’s only one of it [Humby knife] in the hospital. So if someone else is doing a skin graft, I can’t do it for the next 2 hours because it is going to be used, and then I have to go back to the autoclave. Or if I have two skin grafts, then I have to space them and have something else in-between. That becomes sometimes logistically challenging. There is no dermatome and no mesher.” | 85 |
| Lack of OR availability | “Yes the other thing [barrier] is theater time; to get proper theater time. Usually we have a lot of patients, so to get the patient twice or three times to theater is really difficult. Yeah, so they are just staying in the ward for a long time. So when we are finally doing the procedure, the complications will be more.” | 85 |
| Low confidence in performing complex flap procedures | “First, it is a lack of expertise. Because some of these flaps are not as easy as they look, so you need someone who is well-trained and more experienced to do it.” | 80 |
| Burden of other surgical cases is too high | “Because of the burden of patients that we have on our units, most of the time we are fixing major limb fractures. So we don’t always put these flaps on the list.” | 70 |
| Flap procedures being viewed as nonemergency or elective cases | “They are not seen as emergencies according to the policy of the hospital. They don’t consider them as emergency. They can wait.” | 65 |
| Lack of peer-to-peer training | “The training, as I see it, is just on-the-job training. So, it is very little training that has been going on in my hospital in terms of flaps and plastic surgery.” | 65 |
DISCUSSION
Soft tissue reconstruction following open fractures continues to be a critical component of musculoskeletal trauma management; yet, many surgeons in LMICs lack the necessary resources and training to adequately manage complex injures. This study identifies that the vast majority of respondents felt there was inadequate plastic surgeon availability at their hospital. Our study also demonstrates that there are numerous modifiable barriers to performing soft tissue coverage procedures. These barriers included a lack of surgical equipment, OR availability, adequate peer training, adequate access to postoperative wound care, compensation, and senior-level support from colleagues.
The current study adds to the evidence that many LMICs lack adequate access to plastic surgery.13,14 Given the excessive burden of surgical disease and noted lack of plastic surgeons, particularly in sub-Saharan Africa, our results are consistent with prior literature indicating that the absence of surgeons is a major barrier to performing soft tissue coverage procedures.4,24 This barrier, unfortunately, is not readily modifiable, but nevertheless, must be a critical focus as policy makers seek to address the plastic surgery burden of disease.
The best methods to address this burden has been discussed at length in the literature with both short- and long-term mission trips, vertical and diagonal partnerships, and twinning models being suggested as methods to scale up the surgical workforce.28,29 The long-term, sustainable solution must emphasize training of plastic surgeons in LMICs. However, it is possible to start to meet the surgical disease burden by training orthopedic surgeons in principles of plastic surgery and reconstruction.
In high-income countries, ortho-plastic surgery has resulted in good outcomes that ultimately may help meet the growing burden of open fractures.17,18,30 As evidenced by the results of past SMART courses, it is possible to effectively teach the principles and lower rungs of the reconstructive ladder to nonplastic surgeons in LMICs.3,21,22 The SMART course includes entire lectures on these principles, but putting these principles into practice likely requires more training than that gained in a 2-day course. Performing adequate complex limb trauma management on a patient-by-patient basis requires a thorough knowledge of plastic surgery principles and the reconstructive ladder. Nonetheless, the SMART course has proven to be an effective method to quickly train surgeons in procedures that may drastically improve patient quality of life. These courses may additionally have a ripple effect for peer-to-peer training that is needed in LMICs. However, to climb up the reconstructive ladder and perform more advanced microvascular surgical techniques, policy makers must seek to address some of the more easily modifiable resource-related barriers that we identify in this study.
There are numerous examples in the literature identifying various barriers to surgical care in resource-limited settings.10,25–27,31,32 The current study is novel in its identification of barriers to surgical care specific to soft tissue coverage procedures. Notably, participants reported that lack of access to surgical equipment is a significant barrier. The literature presents few examples of the cost-effectiveness of interventions specific to soft tissue management, but there is evidence from multiple studies that addressing surgical burden through both prevention and capacity building is cost-effective.31,33–35 It may be useful to provide a toolkit of basic soft tissue coverage procedure tools to meet the burden of soft tissue injury.
In addition, the lack of OR availability cited by participants in the current study is consistent with prior studies having identified similar barriers.10,27 Flap procedures are time intensive and may not be considered urgent or emergent in an austere setting. For this reason, they may not receive priority in scheduling limited OR space or in returning a patient to the OR for a flap procedure the same day as fracture fixation. Development of an LMIC-specific soft tissue injury protocol may help to standardize treatment and emphasize the importance of flap operations for institutions capable of performing them. A unique finding from our study was that participants reported they are not adequately compensated for flap procedures and that the cost may be exorbitant for many patients. Lack of adequate compensation for flap procedures may be incentivizing surgeons to forego these procedures with their limited time and OR availability. Further study is needed to better understand the economic impact of these injuries and the potential return on investment in building capacity to perform soft tissue coverage procedures.
There were limitations in completing this study. The study survey is a nonvalidated instrument created by the authors for the purpose of the study. To our knowledge, there is no standardized, validated instrument designed to capture surgeons’ perception of surgical barriers in LMICs. The survey does not capture all barriers to care, but the mixed-methods sampling survey strategy helped to collect comprehensive data from participants. The survey was also provided solely in English, but questions could be misinterpreted by individuals nonfluent in English. Of note, although English is not the first language for most participants, residency training and orthopedic conferences in sub-Saharan Africa are commonly in English. The survey response data also rely on surgeon recall and subjective interpretation of care barriers which will be inherently subject to bias. In future studies, it will be useful to empirically quantify the extent of the barriers identified in the survey. In addition, the study populations may differ slightly between Tanzanian and San Francisco SMART course attendees. However, the pooling of participants does lend statistical power to the study analysis.
CONCLUSIONS
This study presents a novel evaluation of the barriers to performing soft tissue coverage procedures in a cohort of primarily Central and East African surgeons who participated in a SMART course. It is essential that plastic surgeons and orthopedic surgeons in high-income countries emphasize scaling up the surgeon workforce to perform reconstructive limb procedures, particularly through ortho-plastic training. This training may have the potential to ameliorate the lack of plastic surgeons in the short term whereas training plastic surgeons in the long term. Course participants also express a need for greater resource allocation to provide surgical equipment and opportunities for peer-to-peer training. Future studies will seek to assess the economic impact of addressing the barriers identified in this study and assess the effectiveness of targeted interventions aimed at addressing identified barriers.
ACKNOWLEDGMENT
The authors would also like to thank the staff at Muhimbili Orthopaedic Institute and the Institute for Global Orthopaedics and Traumatology for their support and assistance with this project.
Footnotes
Published online 25 October 2019.
This project was funded with a research grant from the Heiman Orthopaedic Fellowship.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
REFERENCES
- 1.Murray CJL, Vos T, Lozano R, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: a systematic analysis of the Global Burden of Disease Study 2010. Lancet. 2012;380:2197–2223. [DOI] [PubMed] [Google Scholar]
- 2.Gosselin RA, Spiegel DA, Coughlin R, et al. Injuries: the neglected burden in developing countries. Bull World Health Organ. 2009;87:246–246a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Carey JN, Caldwell AM, Coughlin RR, et al. Building orthopaedic trauma capacity: IGOT international SMART course. J Orthop Trauma. 2015;29(Suppl 10):S17–S19. [DOI] [PubMed] [Google Scholar]
- 4.Semer NB, Sullivan SR, Meara JG. Plastic surgery and global health: how plastic surgery impacts the global burden of surgical disease. J Plast Reconstr Aesthet Surg. 2010;63:1244–1248. [DOI] [PubMed] [Google Scholar]
- 5.Goodacre TE. Plastic surgery in a rural African hospital: spectrum and implications. Ann R Coll Surg Engl. 1986;68:42–44. [PMC free article] [PubMed] [Google Scholar]
- 6.Jovic G, Corlew DS, Bowman KG. Plastic and reconstructive surgery in Zambia: epidemiology of 16 years of practice. World J Surg. 2012;36:241–246. [DOI] [PubMed] [Google Scholar]
- 7.Pollak AN, McCarthy ML, Burgess AR. Short-term wound complications after application of flaps for coverage of traumatic soft-tissue defects about the tibia. The Lower Extremity Assessment Project (LEAP) study group. J Bone Joint Surg Am. 2000;82:1681–1691. [PubMed] [Google Scholar]
- 8.Ikem IC, Oginni LM, Bamgboye EA. Open fractures of the lower limb in Nigeria. Int Orthop. 2001;25:386–388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Conway DJ, Coughlin R, Caldwell A, et al. The institute for global orthopedics and traumatology: a model for academic collaboration in orthopedic surgery. Front Public Health. 2017;5:146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grimes CE, Bowman KG, Dodgion CM, et al. Systematic review of barriers to surgical care in low-income and middle-income countries. World J Surg. 2011;35:941–950. [DOI] [PubMed] [Google Scholar]
- 11.Ngcelwane M. Expanding the orthopaedic training programme to improve the management of lower extremity trauma. SA Orthop J. 2015; 14:14–15. [Google Scholar]
- 12.Corlew DS. Perspectives on plastic surgery and global health. Ann Plast Surg. 2009;62:473–477. [DOI] [PubMed] [Google Scholar]
- 13.Ozgediz D, Jamison D, Cherian M, et al. The burden of surgical conditions and access to surgical care in low- and middle-income countries. Bull World Health Organ. 2008;86:646–647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Borelli MR. What is the role of plastic surgery in global health? A review. World J Plast Surg. 2018;7:275–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mishra B, Koirala R, Tripathi N, et al. Plastic surgery-myths and realities in developing countries: experience from eastern Nepal. Plast Surg Int. 2011;2011:870902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nguyen TA. Soft tissue coverage at the resource-challenged facility. Clin Orthop Relat Res. 2008;466:2451–2456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Levin LS. The reconstructive ladder. An orthoplastic approach. Orthop Clin North Am. 1993;24:393–409. [PubMed] [Google Scholar]
- 18.Fernandez MA, Wallis K, Venus M, et al. The impact of a dedicated orthoplastic operating list on time to soft tissue coverage of open lower limb fractures. Ann R Coll Surg Engl. 2015;97:456–459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Barbier O, Ollat D, Pasquier P, et al. Could the orthopaedic surgeon deployed in austere setting perform flaps on the leg? Acta Orthop Belg. 2017;83:35–39. [PubMed] [Google Scholar]
- 20.Boopalan PR, Nithyananth M, Titus VT, et al. Experience of using local flaps to cover open lower limb injuries at an Indian trauma center. J Emerg Trauma Shock. 2011;4:325–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Challa S, Conway D, Wu HH, et al. Can a 2-day course teach orthopaedic surgeons rotational flap procedures? An evaluation of data from the Nepal SMART course over 2 years. J Orthop Trauma. 2018;32 (Suppl 7):S38–S42. [DOI] [PubMed] [Google Scholar]
- 22.Wu HH, Patel KR, Caldwell AM, et al. Surgical management and reconstruction training (SMART) course for international orthopedic surgeons. Ann Glob Health. 2016;82:652–658. [DOI] [PubMed] [Google Scholar]
- 23.Selber JC, Chang EI, Liu J, et al. Tracking the learning curve in microsurgical skill acquisition. Plast Reconstr Surg. 2012;130:550e–557e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nangole WF, Khainga S, Aswani J, et al. Free flaps in a resource constrained environment: a five-year experience-outcomes and lessons learned. Plast Surg Int. 2015;2015:194174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stewart BT, Gyedu A, Abantanga F, et al. Barriers to essential surgical care in low- and middle-income countries: a pilot study of a comprehensive assessment tool in Ghana. World J Surg. 2015;39:2613–2621. [DOI] [PubMed] [Google Scholar]
- 26.Yao CA, Swanson J, Chanson D, et al. Barriers to reconstructive surgery in low- and middle-income countries: a cross-sectional study of 453 cleft lip and cleft palate patients in Vietnam. Plast Reconstr Surg. 2016;138:887e–895e. [DOI] [PubMed] [Google Scholar]
- 27.Ologunde R, Maruthappu M, Shanmugarajah K, et al. Surgical care in low and middle-income countries: burden and barriers. Int J Surg. 2014;12:858–863. [DOI] [PubMed] [Google Scholar]
- 28.Broer PN, Jenny HE, Ng-Kamstra JS, et al. The role of plastic surgeons in advancing development global. World J Plast Surg. 2016;5:109–113. [PMC free article] [PubMed] [Google Scholar]
- 29.Ng-Kamstra J, Greenberg SL, Abdullah F, et al. Global surgery 2030: A roadmap for high income country actors. BMJ Global Health. 2016;6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jordan DJ, Malahias M, Khan W, et al. The ortho-plastic approach to soft tissue management in trauma. Open Orthop J. 2014;8:399–408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Meara JG, Leather AJ, Hagander L, et al. Global surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet. 2015;386:569–624. [DOI] [PubMed] [Google Scholar]
- 32.Spiegel DA, Gosselin RA. Surgical services in low-income and middle-income countries. Lancet. 2007;370:1013–1015. [DOI] [PubMed] [Google Scholar]
- 33.Opondo E, Wanzala P, Makokha A. Cost effectiveness of using surgery versus skeletal traction in management of femoral shaft fractures at Thika level 5 hospital, Kenya. Pan Afr Med J. 2013;15:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wesson HK, Boikhutso N, Bachani AM, et al. The cost of injury and trauma care in low- and middle-income countries: a review of economic evidence. Health Policy Plan. 2014;29:795–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Grimes CE, Henry JA, Maraka J, et al. Cost-effectiveness of surgery in low- and middle-income countries: a systematic review. World J Surg. 2014;38:252–263. [DOI] [PubMed] [Google Scholar]


