Summary:
Preserving a dynamic abdominal wall is the premise behind the evolution of TRAM flaps into deep inferior epigastric perforators (DIEPs). Performing a true DIEP flap requires a highly refined surgical technique and often times involves a tedious intramuscular dissection which may account for the slow, albeit steady adaptation of DIEPs in breast reconstruction. This article intends to address a scenario in which an additional perforator from a different row is needed. Based on our current knowledge of the abdominal wall and its embryology, we propose splitting the rectus abdominis muscle through the intersections while recruiting a second perforator instead of converting the procedure into MS-TRAM or performing a second anastomosis through the perforator exchange technique, APEX. This potentially saves time and simplifies the procedure while maintaining the integrity of the abdominal wall.
INTRODUCTION
Modifications of the deep inferior epigastric perforator (DIEP) flaps continue to evolve ever since its first application in breast reconstruction. When performed with sound surgical principles, the DIEP flap promises to deliver aesthetically pleasing reconstructed breasts with minimal donor site complications. According to the American Society of Plastic Surgeon Statistics in 2016, implant-/expander-based breast reconstruction continues to be the most commonly performed reconstructive procedure with a steady yet slow adaptation of the DIEP flap despite its low morbidity.9 This can be attributed to the steep learning curve and the highly refined technique it requires. This article aims to simplify the technique of recruiting a second perforator from a different row without sacrificing a substantial amount of muscle fibers. We propose splitting and repairing the muscle inscription instead.
SURGICAL TECHNIQUE
Our patient underwent delayed reconstruction of right breast post modified radical mastectomy with a DIEP flap. Computed tomography angiography for perforator mapping was done preoperatively. The marking is similar to the abdominoplasty procedure. The lower incision was made first. The SIEV/SIEA were identified on both sides, and their diameter was judged to be insignificant. We proceeded to the identification and skeletonization of the musculocutaneous perforators. Anterior rectus fasciotomy was performed. Intramuscular dissection showed intervening 4 cm of rectus abdominis muscle between the perforators (Fig. 1). We opted to cut along the tendinous intersection and deliver the perforators. Later repair of the tendinous intersection was performed with 3–0 Vicryl. Sizable bites were taken through the substance, and the continuity of the rectus was reestablished (Fig. 2), and then fascial closure with PDS was followed. The encountered anatomic configuration and the intersection-splitting technique are illustrated in Figure 3. Closure of abdominal donor site without mesh followed by in-setting and anastomosis were straightforward and followed conventional techniques.
Fig. 1.
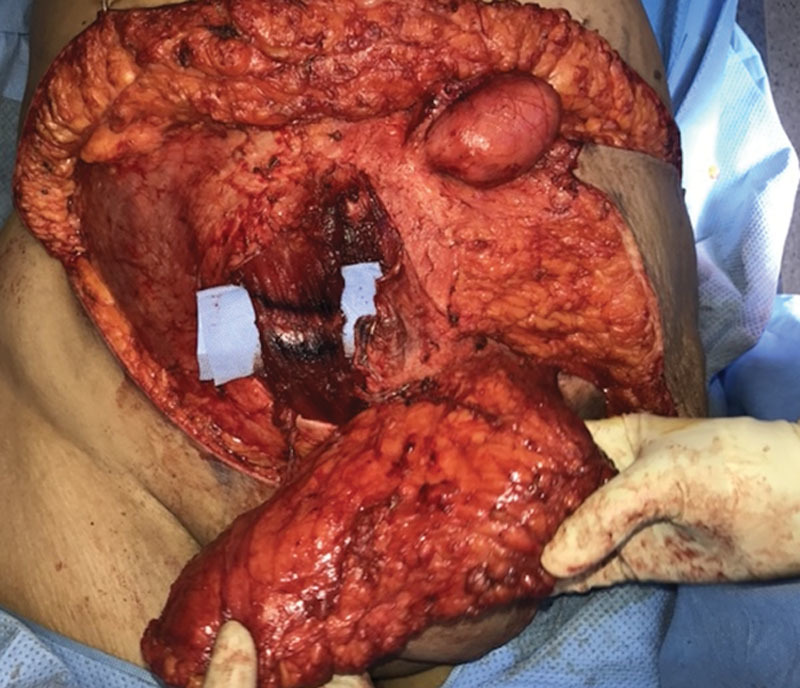
Perforators of the DIEP flap with 4 cm of intervening rectus muscle. Tendinous intersection marked for splitting and later repair. Paraumbilical hernia encountered and repaired.
Fig. 2.
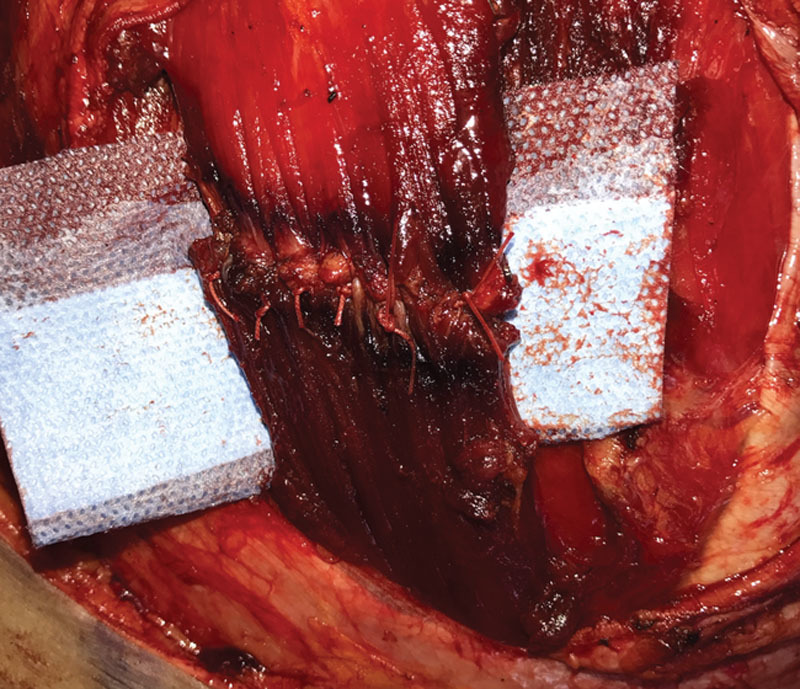
Tendinous intersection repaired after the perforator delivery.
Fig. 3.
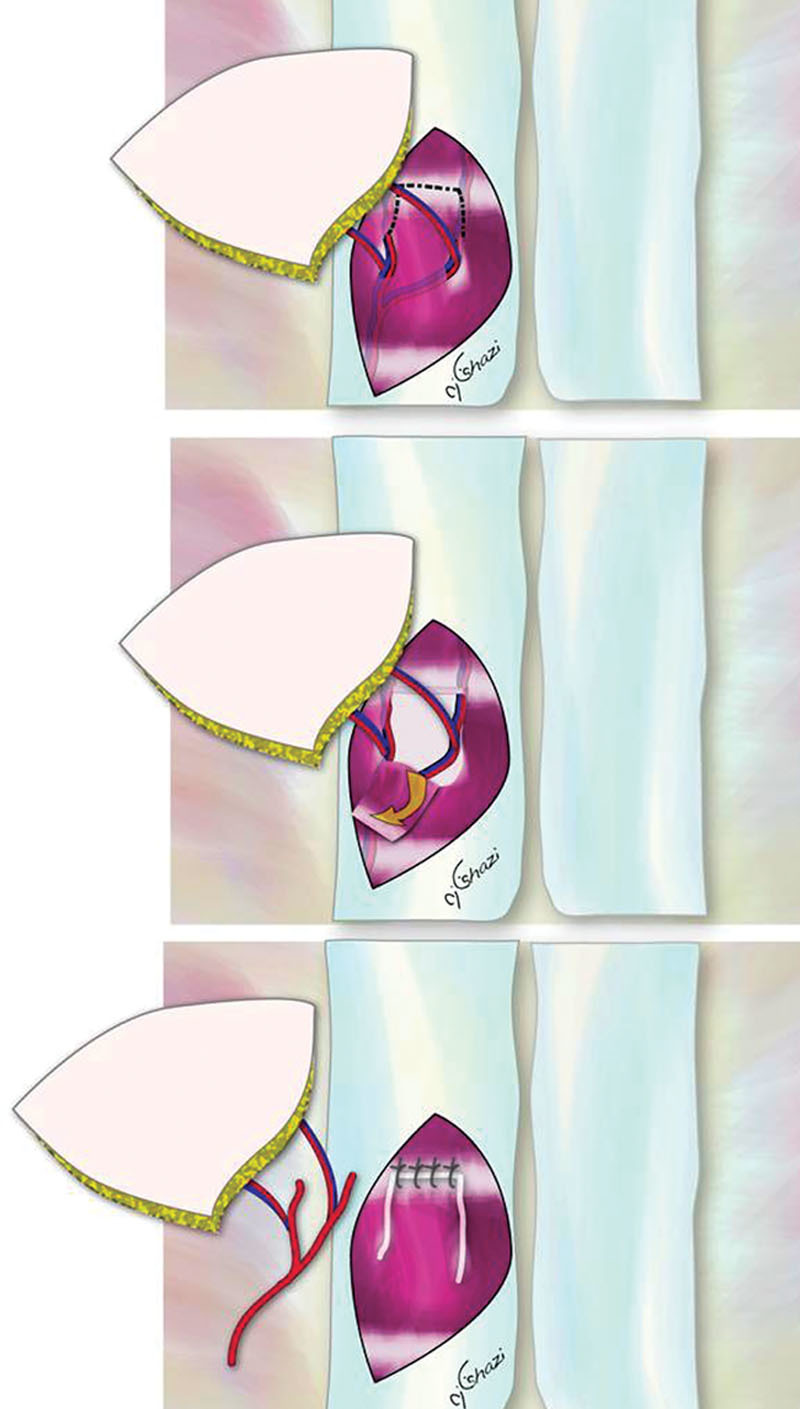
Illustration of intersection-splitting DIEP flap technique.
DISCUSSION
Original description of DIEP flap goes back to 1989 but it was not until 1991 that Allen and Treece applied its use in reconstructive breast surgery.1,5 Over the past 20 years, several refinements made this flap the most highly esteemed method of breast reconstruction. The premise of the DIEP flap is to have minimal donor site complications in terms of bulge and hernia, which is accomplished via the preservation of the rectus abdominis muscle/fascia complex yet providing a soft breast which in turn entails a good number of suitable perforators to be harvested.2,7 Perhaps, the most challenging part of this procedure is choosing the perforator on which to carry the abdominal flap on. The situation where a good number of perforators are aligned making their incorporation to enhance the blood supply, whereas preserving the muscle in between has proven to be the exception. More commonly, the reconstructive surgeon is faced with the decision to either limit the number of perforators, convert to muscle-sparing TRAMs or perform a pedicle disassembly.10 When faced with such a challenge, we chose to cut the muscle along the tendinous intersection and we found that its substance can withstand repair, limiting the need to sacrifice muscle and avoiding a second micro-anastomosis.
Rectus abdominis muscle has 3 transverse tendinous intersections or tendinous inscriptions: 1 just below the costal margin, 1 at the level of the umbilicus, and 1 half-way in between. One or 2 incomplete intersections can be found below the level of the umbilicus.3 These intersections represent myosepta that delineate the distinct myotomes of the rectus abdominis.6,8 They represent areas of adherence to the anterior rectus sheath. They can be full thickness, but they more often tend to span half of the muscle substance.3 Some may believe that these intersections are evolutions to bones in the ventral wall called gastria, which do not articulate with the vertebral column and are usually referred to as inscription ribs.4 No matter the embryonal origin, we found that the intersection had sufficient substance to withstand repair.
This technique was deemed suitable for use on multiple other patients. Follow-up assessment of these patients showed integrity of the abdominal wall without the evidence of hernias nor bulges. Patients were assessed by clinical examinations and magnetic resonance imaging of the abdomen.
CONCLUSIONS
We present the technique of intersection-splitting DIEP flap. This technique is tailored to the well-known anatomy of the rectus abdominis muscle. It serves to simplify the intramuscular dissection of the perforators while preserving this functionally important muscle. The technique was used on multiple patients, all of whom maintained their abdominal wall configuration, with no bulges or hernias upon follow-up assessment.
ACKNOWLEDGMENT
The patient provided written consent for the use of her image.
Footnotes
Published online 18 October 2019.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
REFERENCES
- 1.Allen RJ, Treece P. Deep inferior epigastric perforator flap for breast reconstruction. Ann Plast Surg. 1994;32:32–38. [DOI] [PubMed] [Google Scholar]
- 2.Baumann DP, Lin HY, Chevray PM. Perforator number predicts fat necrosis in a prospective analysis of breast reconstruction with free TRAM, DIEP, and SIEA flaps. Plast Reconstr Surg. 2010;125:1335–1341. [DOI] [PubMed] [Google Scholar]
- 3.Broyles JM, Schuenke MD, Patel SR, et al. Defining the anatomy of the tendinous intersections of the rectus abdominis muscle and their clinical implications in functional muscle neurotization. Ann Plast Surg. 2018;80:50–53. [DOI] [PubMed] [Google Scholar]
- 4.Claessens LP. Dinosaur gastralia; origin, morphology, and function. J Vertebr Paleontol. 2010;89–106. [Google Scholar]
- 5.Koshima I, Soeda S. Inferior epigastric artery skin flaps without rectus abdominis muscle. Br J Plast Surg. 1989;42:645–658. [DOI] [PubMed] [Google Scholar]
- 6.McMinn RMH, Gaddum-Rosse P, Hutchings RT, et al. Chapter –19: Abdomen and pelvis. In: McMinn’s Functional and Clinical Anatomy. 199519th ed Chicago, IL: Mosby Comp. [Google Scholar]
- 7.Nahabedian MY, Dooley W, Singh N. Contour abnormalities of the abdomen after breast reconstruction with abdominal flaps: the role of muscle preservation. Plast Reconstr Surg. 2002;109:91–101. [DOI] [PubMed] [Google Scholar]
- 8.Standring S. Chapter – 61: Anterior abdominal wall. In: Gray’s Anatomy the Anatomical Basis of Clinical Practice. 200840th ed Elsevier. [Google Scholar]
- 9.American Society of Plastic Surgeons. Plastic surgery statistics report. Available at: https://www.plasticsurgery.org/documents/News/Statistics/2016/plastic-surgery-statistics-full-report-2016.pdf.
- 10.DellaCroce FJ, DellaCroce HC, Blum CA, et al. Mythbusting the DIEP flap and an introduction to the Abdominal Perforator Exchange (APEX) breast reconstruction technique: a single-surgeon retrospective review. Plast Reconstr Surg. 2019;143:992–1008. [DOI] [PMC free article] [PubMed] [Google Scholar]


