Supplemental Digital Content is available in the text.
Background:
Currently, there are more than 40 cases of facial allotransplantation performed by 13 different groups in 10 countries. Although it has become a potential option to reconstruct and restore the function and appearance of severely facially disfigured individuals, the ethical concerns of facial allotransplantation remain unsolved. We conducted a systematic review to better understand the ethical concerns on facial allotransplantation and the changing trends of the ethical debate over time.
Methods:
A systematic review of 3 databases was performed to identify articles related to ethical topics on facial allotransplantation. The inclusion criteria were peer-reviewed articles written since 1995 on the topics of ethics and facial allotransplantation in English, French, and Chinese languages. The ethical concerns extracted from the included articles were categorized into 4 core principles of ethics: autonomy, beneficence, nonmaleficence, and justice. The different themes under these 4 principles were extracted and subgrouped. The positions of the included articles were collected. Joinpoint regression was applied to compare the frequency of themes and positions by publication year. We presented the main topics on ethical concerns and the changing trends in ethical themes and principles of facial allotransplantation.
Results:
There were 889 articles identified initially. After excluding 265 duplicated articles, 624 articles were included for title/abstract review process, and 148 articles were included in final data analysis. The publication year was from 2002 to 2018 with 136 articles in English, 11 in French, and 1 in Chinese. The most addressed principle was nonmaleficence (117/148, 79.1%), followed by beneficence (116/148, 78.4%), justice (103/148, 69.6%), and autonomy (86/148, 58.1%). The themes on immunosuppression/rejection, quality of life, and identity were the top 3 addressed ethical concerns. Twelve of 13 most addressed ethical themes demonstrated a decreasing trend after 2004. The themes of identity under beneficence showed a significant decrease after 2004. Ethical concerns on the cost/financial topic were the only one showing consistently increase trends from 2002 to 2018. There was a significant increase of the papers in favor of facial allotransplantation procedure comparing to those were against or neutral before and after 2008.
Conclusions:
More and more articles support facial allotransplantation as a feasible option to reconstruct and restore the function and appearance of severely facially disfigured individuals. The requirement of life-long immunosuppression therapy, quality of life, and identity center the ethical debates. Supported by favorable short-term results, 12 of 13 most addressed ethical concerns have trended down. The theme of cost/financial topic becomes more frequently addressed in recent years.
INTRODUCTION
The human face is a complex 3-dimensional structure that is central to human identity.1,2 Facial appearance identifies our gender, age, and ethnicity; it conveys our emotions and allows us to interact with our surrounding world.3 When the essential features and functions of the human face are damaged, it has not only physical but emotional and psychological consequences. With advancing technological and available immunosuppressive regimens, facial allotransplantation for severely disfigured patient became possible. The ethics on facial allotransplantation has been at the forefront of the ongoing debate even before the world’s first successful case in France in 2005. Within the past 13 years, the field has expanded remarkably. More than 40 cases were reported from 10 different countries, including France, China, United States, Spain, Belgium, Turkey, Poland, Russia, Finland, and Canada.4–6
In 2016, Isabelle Dinoire, the world’s first face transplant patient, died after a long illness, adding one more to a total 7 deaths so far.7 Like her initial introduction into the spotlight, her death perpetuated the ongoing debate. In early 2018, a French team performed the second facial allotransplantation on a patient who lost his graft due to chronic rejection.8 These newly monumental developments in facial allotransplantation add more valuable data to the ethical debate and could shift the trends potentially. In this article, we performed a systematic review of the ethics on facial allotransplantation, collected the data of 4 core principles of bioethics: autonomy, beneficence, nonmaleficence, and justice, the authors’ positions on facial allotransplantation, and presented the changing trends in ethical themes, principles, and positions of facial allotransplantation over time.
MATERIALS AND METHODS
We conducted a literature search in 3 databases (PubMed, Scopus, and Cochrane) from 1995 to October 23, 2018. The literature was searched with specific search strategies designed following the systematic review guidelines and with the assistance of the health sciences librarian (W.H.). The search strings concerned the concepts of the face, allotransplantation, and ethics for the topic of the systematic review. The search strings were constructed by combining controlled vocabulary and keyword terms (see pdf, Supplemental Digital Content 1, which displays the search strategy used, http://links.lww.com/PRSGO/B224). Inclusion criteria were peer-reviewed articles on face allotransplantation and the ethical topics relating to from 1995 to the present, and languages were limited to English, French, or Chinese. Two reviewers (X.L., S.L.) performed the title/abstract screening and review of full-text articles. Any disagreements regarding articles to be excluded and included were resolved by discussion. Ethical themes were extracted qualitatively and categorized under 4 principles of bioethics: autonomy (allows the patient to “self-rule,” free from interference by others), beneficence (the moral obligation to benefit others), nonmaleficence (the obligation to not cause harm to others), justice (provides fair and appropriate treatment to all persons regardless of status or special considerations).9 The positions of the articles were defined as “yes” or “no” by looking for the specific statement regarding facial allotransplantation in the articles; if there was no such statement, it was defined as “neutral.”
The frequency of ethical themes/principles and the position of the articles were assessed. The Joinpoint regression program (Version 4.6.0.0, National Cancer Institute, Calverton, Md.) was applied to analyze the trends and its annual percentage change (APC) in most common ethical themes and position of the articles. The χ2 test was used to determine whether there was a statistically significant difference between 3 category groups of the position. P value <0.05 was set as the level of significance.
RESULTS
The initial search discovered 889 citations. After removing 265 duplicates, 624 citations were included in the title/abstract review, 467 articles were excluded during this process, and 157 articles were included for full-text review. There were 5 additional articles included into the full-text review by manual searching of the references. Following the full-text review, 148 articles were included in final data analysis (Fig. 1).
Fig. 1.
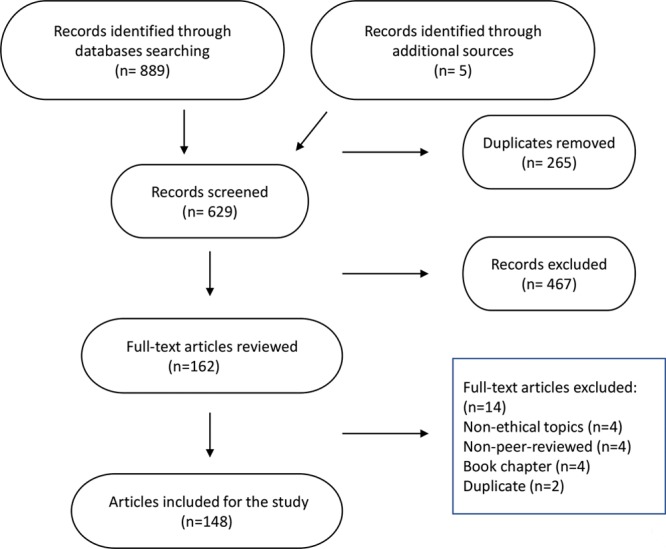
Flow chart shows the results of screening process and final article inclusion.
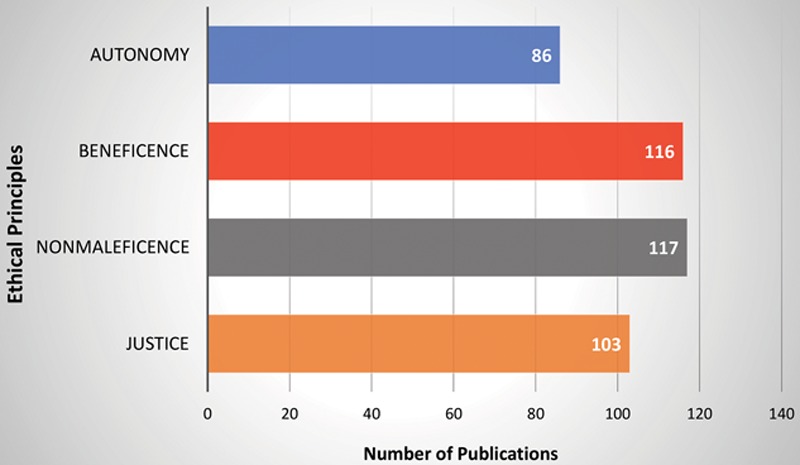
The first publication on the ethics of facial allotransplantation was in 2002.10 The least number of publications per year were in 2002, 2003, and 2015 with only 2 papers, the most number of publications per year was in 2004 with 28 papers, followed by 2006 with 22 papers. The average number of publications per year was 9 (Fig. 2). There were 136 English, 11 French, and 1 Chinese publications (Fig. 3). In all 148 articles included, nonmaleficence was the most frequent ethical principle addressed (117/148, 79.1%),1–3,7,10–121 followed by beneficence (116/148, 78.3%),1–3,5,7,10,13–24,26–29,32–42,44,46,48,49,51–56,58,60,61,63–66,69–84,86,87,89–93,95–137 justice (103/148, 69.6%),2,3,5,7,11,14,17–22,24–28,30–32,34,35,38,39,41–44,46,48,49,51,52,54,55,57,58,60–64,66–73,75–77,79,82–85,87–92,94,95,97–102,104,105,107–112,114,117,119–121,123,125,129–131,135,138–147 and autonomy (86/148, 58.1%).1–3,5,7,12,14–17,19,23–25,27,28,30,32,34,35,37–41,44,46,48,49,53,56,58,61–66,69–74,79,80,82–84,88,91,94,95,97,98,100–105,107,109,111,113,116,117,119–121,124,125,130,131,133,136,138,140–143,145,147–149
Fig. 2.
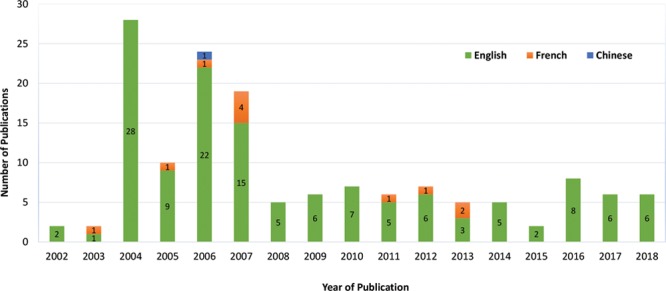
Number of articles (n = 148) addressing the ethical principle on facial allotransplantation.
Fig. 3.
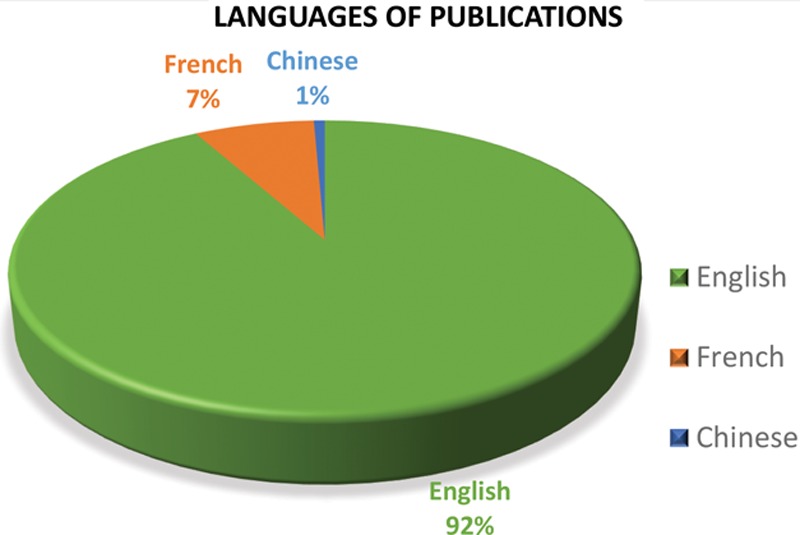
Percentage of the published articles based on language.
The most frequent addressed themes under the principles were risk of immunosuppression or rejection (n = 88, 59.5%),1–3,7,10–12,14,16–19,22,23,25,29–41,43–56,58–64,66,67,69,71,72,75–79,81,83–85,87–92,95,97,100,102–106,108–112,114,115,117–119,121 followed by informed consent or donor family consent (n = 67,45.3%),1–3,5,12,14,15,23,25,27,28,32,34,35,38–41,44,46,48,49,53,56,58,61,63–66,69–74,80,82–84,88,94,97,100–105,107,111,116,117,120,121,130,131,133,136,138,141–143,145,147,149 facial tissue donation and restoration (n = 49, 32.9%),2,11,14,18,21,22,25,28,30,34,39,41–43,46,48,49,51,55,60,64,66–69,71,75,76,83,84,86,89,97,98,100,105,107,108,110,111,119,123,125,131,135,140,143–145 functional recovery or improvement (n = 49,33.1%),2,5,10,17–19,29,32,37,38,42,48,53,55,58,61,63,64,66,69–71,75,76,82,84,86,87,90,92,95,96,98,102,104,106–108,110,111,117,121,129–133,135,137 quality of life (n = 43, 29.1%),3,14,26–29,37,39–41,44,46,49,54,55,66,72,73,77,78,83,86,93,96–99,101,103,104,106,108,111,113,114,117–119,128,133–136 and identity (n = 43, 28.1%)1,7,13,14,19,22,23,33,37,41,42,56,60,61,66,70,72,73,76,78,80,83,84,87,101,105,107,111,112,115,118,122,123,126–128,131,132,135–137 (Fig. 4). The APC trends calculated for the 13 most frequent addressed themes showed 11 themes decreased in frequency overtime (APC < −1), 4 themes increased (APC > 1), and 1 theme remained the same (−1< APC < 1). Three themes including informed consent, identity, and quality of life presented APC trend changes from increase to decrease before and after the year of 2004, and only the theme of identity demonstrated a significant decrease between 2004 and 2018 (APC = −11.1, P < 0.05) (Fig. 5). The theme of cost was the only one that showed a consistent increase from 2002 to 2018 (APC = 6.0) (Table 1).
Fig. 4.
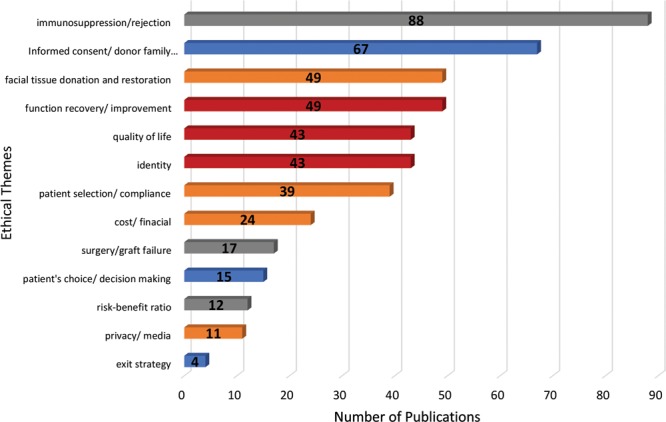
Number of articles addressing the ethical themes.
Fig. 5.
The annual percentage change trends of the position of the included articles from 2002 to 2018.
Table 1.
Joinpoint Analysis of Number of Papers Addressing Ethical Themes from 2002 to 2018
| Principle | Theme | Start of Trend | End of Trend | APC | 95% CI | P |
|---|---|---|---|---|---|---|
| Autonomy | Informed consent/donor family consent | 2002 | 2004 | 296.4 | −49.5 to 3,012.9 | NS |
| 2004 | 2018 | −8.3 | −16.8 to 1.0 | NS | ||
| Patient’s choice/decision making | 2002 | 2018 | −1.8 | −9.5 to 6.5 | NS | |
| Exit strategy | 2002 | 2018 | −2.8 | −6.6 to 1.1 | NS | |
| Beneficence | Identity | 2002 | 2004 | 228.9 | −63.2 to 2,838.0 | NS |
| 2004 | 2018 | −11.1 | −19.8 to −1.5 | <0.05* | ||
| Quality of life | 2002 | 2004 | 235.1 | −39.4 to 1,753.7 | NS | |
| 2004 | 2018 | −6.1 | −13.3 to 1.8 | NS | ||
| Functional recovery/improvement | 2002 | 2018 | −1.6 | −9.8 to 7.4 | NS | |
| Nonmaleficence | Immunosuppression/rejection | 2002 | 2018 | −3.4 | −11.5 to 5.4 | NS |
| Risk-benefit ratio | 2002 | 2018 | −5.3 | −11.1 to 0.9 | NS | |
| Surgery/graft failure | 2002 | 2018 | −2.3 | −9.8 to 5.7 | NS | |
| Justice | Cost/financial | 2002 | 2018 | 6.0 | −1.1 to 13.6 | NS |
| Patient selection/compliance | 2002 | 2018 | 0.3 | −8.4 to 9.8 | NS | |
| Facial tissue donation and restoration | 2002 | 2018 | −5.5 | −14.4 to 4.3 | NS | |
| Privacy/media | 2002 | 2018 | −2.8 | −8.2 to 2.9 | NS |
CI, confidence interval; NS, not significant.
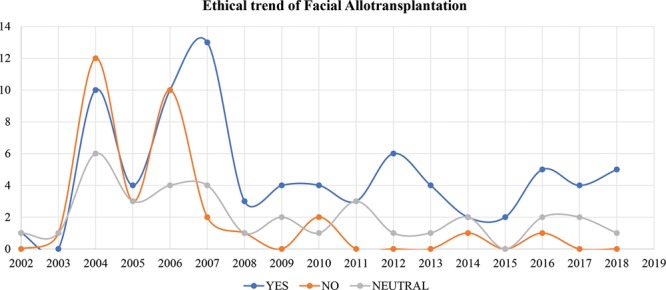
A total of 54.1% of the publications tended to support facial allotransplantation (n = 80), 22.3% of publications tended to oppose it (n = 33), and 23.6% showed neutral position (n = 35). As shown in Figure 5, there was a turning point at the year of 2008. Chi-squared test results demonstrated that there was statistically significant difference when comparing “yes” group to both “no” group and “ neutral” group before and after the year of 2008 (P < 0.05), whereas there was no significant difference between “no” group and “neutral” group before and after year of 2008.
DISCUSSION
The ethics debate on facial allotransplantation started in the early 2000s when the first article on ethics of facial allotransplantation was published.10 Initially, both the Royal College of Surgeons of England and the National Consultative Ethics Committee for Health and Life Science from France stated that the timing for facial allotransplantation was not suitable at that moment due to the unsolved concerns about how to obtain fully valid informed consent, the risk of life-long immunosuppressive therapy, and the potential psychologic impact on the recipient.14,27 In 2004, the Louisville team published the ethical guidelines for facial allotransplantation and claimed they are ready for the procedure.18 At the same year, the Cleveland Clinic team received the world first institutional review board approval to perform human facial allotransplantation. These sparked fierce debates on the ethics topic of facial allotransplantation in medical community.2,15–17,19–22,24,25,27–29,31–35,122,123,138,148,150 As shown in our search results, there were 28 articles published in 2004 representing the highest output year from 2002 to 2018. With limited data and research on the procedure, most of the parties were either against or neutral to facial allotransplantation. Only 34.3% (11/32) of the parties were in favor to the procedure before 2005. The ethical debates did not trend down after the first successful human facial allotransplantation performed in France in 2005,151 instead the transplant brought up another round of debate not only within the medical community this time but also the general populations and the media.44,48–50 As shown in the study, 24 papers were published in 2006 representing the second highest number on a yearly basis.46,56,59,128 Although this time the debate involved some discussion of surgical techniques, the ethical topics still centered the stage. The England team reiterated that “until there is further research and the prospect of better control of the complications, it would be unwise to proceed with human facial transplantation.”49 The French team stated that “a full facial CTA does not make sense at present.”48 The United States team encouraged “further research work in improving transplant immunology and analyzing the long-term results.”152
Despite the unfavorable opinions from both profession societies and the public, 3 different research groups from China, United States, and France successfully carried out another 3 cases of facial allotransplantation from 2006 to 2008.153–155 The APC change results showed there was a turning point in year 2008 regarding the positions of the included articles (Fig. 5). Only 45.6% (41/90) of the articles were in favor of the procedure before 2008, whereas >67.2% (39/58) supported it after 2008. There was a statistically significant increase of the articles in favor of facial allotransplantation before and after 2008 comparing to other 2 groups (P < 0.05). In the next 4 years, from 2009 to 2012, nearly 2 dozen cases were performed worldwide and supported by the favorable short-term result. Facial allotransplantation has become a potential treatment option for carefully selected patients.152 This shift was shown clearly in our study that there were only 2 articles against facial allotransplantation procedures after 2010 (Fig. 5). In the first article, Flynn et al.101 stated that technological readiness was insufficient for the implementation of facial transplantation within pediatrics. The second article addressed social anonymity which was almost impossible for facial allotransplantation cases.146
Encouraged by the favorable functional and aesthetic outcome, more and more groups joined the research and the number of facial allotransplantation climbed to 38 cases worldwide from 2010 to 2016. Although huge advancements were achieved in the research of facial allotransplantation, the ethical debate continued. On April 22, 2016, Isabelle Dinoire, the world’s first facial allotransplantation recipient, died after a long illness, adding one more to a total 7 deaths so far.7 On January 2018, a French team performed the second facial allotransplantation on a patient who lost his graft due to chronic rejection.8 During our preparation of the article, the Italian team encountered acute rejection and total graft loss in the country’s first facial allotransplantation case.156 All these recent incidences reminded us this type of procedure is still in its infancy and associated with significant morbidity and mortality. Patients are at risks of graft rejection, immunosuppressive therapy–associated complications even years after the initial operation.
Based on our study, the nonmaleficence (the obligation to not cause harm to others) was the most addressed ethical principle, appearing in 79.1% (117/148) of the articles, followed by 78.4% (116/148) in beneficence (the moral obligation to benefit others), 69.6% (103/148) in justice (provides fair and appropriate treatment to all persons regardless of status or special considerations), and 58.1% in autonomy (allows the patient to “self-rule,” free from interference by others) (Fig. 6). These results reflected the natural characteristic of the life-enhancing procedure compared with other life-saving solid organ transplantation procedures. Similar results were found in the research of hand allotransplantation.157 Among the 13 most addressed themes, immunosuppression/rejection (n = 88), informed consent/donor family consent (n = 67), facial tissue donation and restoration (n = 49), functional recovery/improvement (n = 49), quality of life (n = 43), and identity (n = 43) were among the leading concerns (see details in Fig. 4). From 2002 to 2004, the APC trends of the informed consent/donor family consent (APC = 296.4), identity (APC = 228.9), and quality of life (APC = 235.1) were far beyond +1 which indicated these 3 themes were the most increasingly discussed ethical concerns at that time. After 2004, all the themes except the cost/financial under justice showed a decreased trend. These findings could be interpreted that the ethical concerns on facial allotransplantation procedure were partially relieved as more and more cases were done and with a favorable functional and aesthetic outcome. Among them, the theme of identity under beneficence showed significant decrease in APC trend (P < 0.05), indicated the identity had become a less and less concerned ethical topic (Table 1). This finding was further supported by the fact that all facial allotransplantation recipients reported adapted to their new identity without difficulty. The theme of cost/financial under justice was the only one had consistently increase in trend (APC = 6.0) from 2002 to 2018. This indicated that the theme of cost/financial had become a more and more discussed ethical topic. Toure et al.60 estimated the total cost of facial allotransplantation procedure to be between $250,000 and $1,500,500 in the French system. Siemionow et al.158 demonstrated that the cost of conventional reconstructive procedures and the cost of facial allotransplantation procedure in the first US case was similar between $250,000 and $350,000. This amount did not include the cost of life-long immunosuppression which was estimated at $20,000 per year.110 Currently, facial allotransplantation cases were supported by either research funding or an institutional budget and each case was funded on an individual basis. Fortunately, as discussed at the 6th Biennial American Society for Reconstructive Transplantation meeting in Chicago on November 2018, the researchers were planning for the application of new Current Procedural Terminology code for facial allotransplantation procedure and other vascularized composite tissue allotransplantation procedures which were the first step to get possible insurance coverage. The researchers agreed that it may be unrealistic to have commercial insurance coverage before facial allotransplantation procedures could become a standard option for the reconstruction of severely disfigured patients. Considering the high cost and the patient’s mental and physical suffering from numerous conventional reconstructive procedures, it would be possible to have Medicare/Medicaid coverage on a case by case basis in the near future.
Fig. 6.
Number of articles addressing the principles of ethics.
Often, information is only available through the public media with no official data from the surgical teams.159 For example, some of the facial allotransplantation cases done by the teams from Turkey and the case done by the Russian team were not reported in the medical literature. One of the limitations of our study is, although we included English, French, and Chinese, we were still missing Spanish, Turkish, Polish, Russian, and Finnish language, in which its case population consisted of at least one-third of the total case volume. This issue may become more apparent when there is significant under-reporting of a large number of cases in the medical literature, especially in recent years. Another limitation is the difference number of library search during the long process of preparation of the article. To reduce this bias, we performed a follow-up search 6 months after our initial search on April 2018. Not surprising, we yielded 5 more articles into the final data analysis.
CONCLUSIONS
Although facial allotransplantation has been proved to be a potential option to reconstruct and restore the function and appearance of patients with devastating facial injuries, the unsolved ethical debates on this life-enhancing procedure continue. Supported by favorable short-term outcomes, the ethical concerns on immunosuppression/rejection, quality of life, and identity tended to decrease sharply, especially on the theme of identity after 2004. To better address the increasing concerns on the cost and financial-related topic, the researchers should work together to strive for the coverage from governmental insurances.
ACKNOWLEDGMENT
The authors appreciate Dr. Ren Dongren for his valuable help during the statistical analysis of the data.
Supplementary Material
Footnotes
Published online 18 October 2019.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Alexander AJ, Alam DS, Gullane PJ, et al. Arguing the ethics of facial transplantation. Arch Facial Plast Surg. 2010;12:60–63. [DOI] [PubMed] [Google Scholar]
- 2.Wiggins OP, Barker JH, Martinez S, et al. On the ethics of facial transplantation research. Am J Bioeth. 2004;4:1–12. [DOI] [PubMed] [Google Scholar]
- 3.Soni CV, Barker JH, Pushpakumar SB, et al. Psychosocial considerations in facial transplantation. Burns. 2010;36:959–964. [DOI] [PubMed] [Google Scholar]
- 4.Sosin M, Rodriguez ED. The face transplantation update: 2016. Plast Reconstr Surg. 2016;137:1841–1850. [DOI] [PubMed] [Google Scholar]
- 5.Lindford AJ, Mäkisalo H, Jalanko H, et al. The Helsinki approach to face transplantation. J Plast Reconstr Aesthet Surg. 2019;72:173–180. [DOI] [PubMed] [Google Scholar]
- 6.Banerjee S. First Canadian face transplant: man doing well after life-changing surgery. https://globalnews.ca/news/4442946/first-canadian-face-transplant/. Accessed November 19, 2018.
- 7.Bound Alberti F. From face/Off to the face race: the case of Isabelle Dinoire and the future of the face transplant. Med Humanit. 2017;43:148–154. [DOI] [PubMed] [Google Scholar]
- 8.Bullen J. ‘Man with three faces’ becomes first patient in world to undergo two face transplants. https://www.mirror.co.uk/news/world-news/man-three-faces-becomes-first-12379067. Accessed November 19, 2018.
- 9.Beauchamp T, Childress J. Principles of Biomedical Ethics. 20015th ed New York, NY: Oxford University. [Google Scholar]
- 10.Hettiaratchy S, Butler PE. Face transplantation–fantasy or the future? Lancet. 2002;360:5–6. [DOI] [PubMed] [Google Scholar]
- 11.McDowell N. Surgeons struggle with ethical nightmare of face transplants. Nature. 2002;420:449. [DOI] [PubMed] [Google Scholar]
- 12.Kmietowicz Z. Face transplants should not be done without more research. BMJ. 2003;327:1184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Meningaud JP. [Facial grafts: the ethical issue]. Rev Stomatol Chir Maxillofac. 2003;104:131–132. [PubMed] [Google Scholar]
- 14.Full or partial face transplants. Bull Med Ethics. 2004:9–11. [PubMed] [Google Scholar]
- 15.Agich GJ, Siemionow M. Facing the ethical questions in facial transplantation. Am J Bioeth. 2004;4:25–27; discussion W23. [DOI] [PubMed] [Google Scholar]
- 16.Ankeny RA, Kerridge I. On not taking objective risk assessments at face value. Am J Bioeth. 2004;4:35–37; discussion W23. [DOI] [PubMed] [Google Scholar]
- 17.Banis JC, Barker JH, Cunningham M, et al. Response to selected commentaries on the AJOB target article “On the ethics of facial transplantation research” [1] (multiple letters). Am J Bioeth. 2004;4:W23–W31+W33W34. [DOI] [PubMed] [Google Scholar]
- 18.Barker JH, Vossen M, Banis JC., Jr The technical, immunological and ethical feasibility of face transplantation. Int J Surg. 2004;2:8–12. [Google Scholar]
- 19.Baylis F. A face is not just like a hand: pace Barker. Am J Bioeth. 2004;4:30–32; discussion W23. [DOI] [PubMed] [Google Scholar]
- 20.Butler PE, Clarke A, Ashcroft RE. Face transplantation: when and for whom? Am J Bioeth. 2004;4:16–17; discussion W23. [DOI] [PubMed] [Google Scholar]
- 21.Caplan A. Facing ourselves. Am J Bioeth. 2004;4:18–20; discussion W23. [DOI] [PubMed] [Google Scholar]
- 22.Check E. Surgeons seek go-ahead to perform first face transplant. Nature. 2004;431:389. [DOI] [PubMed] [Google Scholar]
- 23.Clark J. Face transplants technically possible, but “very hazardous”. CMAJ. 2004;170:323. [PMC free article] [PubMed] [Google Scholar]
- 24.Haughton P. Ethical considerations in face transplantation. Int J Surg. 2004;2:79–81; discussion 81. [DOI] [PubMed] [Google Scholar]
- 25.Maschke KJ, Trump E. Facial transplantation research: a need for additional deliberation. Am J Bioeth. 2004;4:33–35; discussion W23. [DOI] [PubMed] [Google Scholar]
- 26.Morreim EH. About face: downplaying the role of the press in facial transplantation research. Am J Bioeth. 2004;4:27–29; discussion W23. [DOI] [PubMed] [Google Scholar]
- 27.Morris PJ, Bradley JA, Doyal L, et al. Facial transplantation: a working party report from the Royal College of Surgeons of England. Transplantation. 2004;77:330–338. [DOI] [PubMed] [Google Scholar]
- 28.Petit F, Paraskevas A, Lantieri L. A surgeons’ perspective on the ethics of face transplantation. Am J Bioeth. 2004;4:14–16; discussion W23. [DOI] [PubMed] [Google Scholar]
- 29.Petit F, Paraskevas A, Minns AB, et al. Face transplantation: where do we stand? Plast Reconstr Surg. 2004;113:1429–1433. [DOI] [PubMed] [Google Scholar]
- 30.Rumsey N. Psychological aspects of face transplantation: read the small print carefully. Am J Bioeth. 2004;4:22–25; discussion W23. [DOI] [PubMed] [Google Scholar]
- 31.Strong C. Should we be putting a good face on facial transplantation? Am J Bioeth. 2004;4:13–14; discussion W23. [DOI] [PubMed] [Google Scholar]
- 32.Thorburn G, Hettiaratchy S, Ashcroft R, et al. Patient selection for facial transplantation III: ethical considerations. Int J Surg. 2004;2:118–119; discussion 119. [DOI] [PubMed] [Google Scholar]
- 33.Trachtman H. Facing the truth: a response to “On the ethics of facial transplantation research” by Wiggins et al. Am J Bioeth. 2004;4:W33–W34. [DOI] [PubMed] [Google Scholar]
- 34.Wiggins OP, Barker JH. Response to: P. Haughton: ethical considerations of facial transplantation. Int J Surg. 2004;2:81–82. [Google Scholar]
- 35.Wiggins OP, Barker JH. Response to: Thorburn et al: patient selection for facial transplantation III: Ethical considerations. Int J Surg. 2004;2:119. [DOI] [PubMed] [Google Scholar]
- 36.Martin J. [Patient satisfaction, measure of the ethical character of medical acts? About the face transplant in Amiens]. Rev Med Suisse. 2005;1:3003. [PubMed] [Google Scholar]
- 37.Agich GJ, Siemionow M. Until they have faces: the ethics of facial allograft transplantation. J Med Ethics. 2005;31:707–709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Butler PE, Clarke A, Hettiaratchy S. Facial transplantation. BMJ. 2005;331:1349–1350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Clark PA. Face transplantation: part II - An ethical perspective. Med Sci Monit. 2005;11:RA41–RA47. [PubMed] [Google Scholar]
- 40.Clark PA. Face transplantation: a medical perspective. Med Sci Monit. 2005;11:RA1–RA6. [PubMed] [Google Scholar]
- 41.Clarke A, Butler PE. Facial transplantation: adding to the reconstructive options after severe facial injury and disease. Expert Opin Biol Ther. 2005;5:1539–1546. [DOI] [PubMed] [Google Scholar]
- 42.Hartman RG. Face value: challenges of transplant technology. Am J Law Med. 2005;31:7–46. [DOI] [PubMed] [Google Scholar]
- 43.Siemionow M, Agaoglu G. Allotransplantation of the face: how close are we? Clin Plast Surg. 2005;32:401–409, vii. [DOI] [PubMed] [Google Scholar]
- 44.Renshaw A, Clarke A, Diver AJ, et al. Informed consent for facial transplantation. Transpl Int. 2006;19:861–867. [DOI] [PubMed] [Google Scholar]
- 45.Barker JH, Furr A, Cunningham M, et al. Investigation of risk acceptance in facial transplantation. Plast Reconstr Surg. 2006;118:663–670. [DOI] [PubMed] [Google Scholar]
- 46.Hutchison I. Face transplants: is the genie out of the bottle? South Med J. 2006;99:427–429. [DOI] [PubMed] [Google Scholar]
- 47.Walton RL, Levin LS. Face transplantation: the view from Duke University and the University of Chicago. South Med J. 2006;99:417–418. [DOI] [PubMed] [Google Scholar]
- 48.The French position: Comité consultatif national d’Ethique pour les sciences de la vie et de la santé: “Composite tissue allograftransplantation of the face (total or partial graft)”.South Med J. 2006;99:432–433. [PubMed] [Google Scholar]
- 49.The English position: Position paper of the Royal College of Surgeons of England. South Med J. 2006;99:431. [DOI] [PubMed] [Google Scholar]
- 50.Bermudez L. Face transplant: is it worth it? Plast Reconstr Surg. 2006;117:1891–1896. [DOI] [PubMed] [Google Scholar]
- 51.Clarke A, Simmons J, White P, et al. Attitudes to face transplantation: results of a public engagement exercise at the Royal Society summer science exhibition. J Burn Care Res. 2006;27:394–398. [DOI] [PubMed] [Google Scholar]
- 52.Gaba A. Face transplants and the difficulties of obtaining research approval. J Biolaw Bus. 2006;9:54–55. [PubMed] [Google Scholar]
- 53.Hamdy RC. Face transplantation: a brave or maverick surgery? South Med J. 2006;99:410–411. [DOI] [PubMed] [Google Scholar]
- 54.Lantieri LA. Face transplantation: the view from Paris, France. South Med J. 2006;99:421–423. [DOI] [PubMed] [Google Scholar]
- 55.Li Y, Li Q, Zhang D. [Review on progress of facial allotransplantation]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2006;20:1262–1265. [PubMed] [Google Scholar]
- 56.Peled ZM, Pribaz JJ. Face transplantation: the view from Harvard Medical School. South Med J. 2006;99:414–416. [DOI] [PubMed] [Google Scholar]
- 57.Powell T. Face transplant: real and imagined ethical challenges. J Law Med Ethics. 2006;34:111–115, 4. [DOI] [PubMed] [Google Scholar]
- 58.Rohrich RJ, Longaker MT, Cunningham B. On the ethics of composite tissue allotransplantation (facial transplantation). Plast Reconstr Surg. 2006;117:2071–2073. [DOI] [PubMed] [Google Scholar]
- 59.Shack B. Face transplantation: the view from Vanderbilt University. South Med J. 2006;99:419–420. [DOI] [PubMed] [Google Scholar]
- 60.Toure G, Meningaud JP, Bertrand JC, et al. Facial transplantation: a comprehensive review of the literature. J Oral Maxillofac Surg. 2006;64:789–793. [DOI] [PubMed] [Google Scholar]
- 61.Wigmore SJ. Face transplantation: the view from Birmingham, England. South Med J. 2006;99:424–426. [DOI] [PubMed] [Google Scholar]
- 62.Barker JH, Furr A, McGuire S, et al. On the ethics of composite tissue allotransplantation (facial transplantation). Plast Reconstr Surg. 2007;119:1621–1622. [DOI] [PubMed] [Google Scholar]
- 63.Barker JH, Stamos N, Furr A, et al. Research and events leading to facial transplantation. Clin Plast Surg. 2007;34:233,ix–250, ix. [DOI] [PubMed] [Google Scholar]
- 64.Brown CS, Gander B, Cunningham M, et al. Ethical considerations in face transplantation. Int J Surg. 2007;5:353–364. [DOI] [PubMed] [Google Scholar]
- 65.Hurlburt M. Facial transplantation: understanding the interests of patients and hurdles to informed consent. Med Sci Monit. 2007;13:RA147–RA153. [PubMed] [Google Scholar]
- 66.Masquelet AC. [Philosophical and ethics aspects of the composite tissues allotransplantations (CTA)]. Ann Chir Plast Esthet. 2007;52:519–523. [DOI] [PubMed] [Google Scholar]
- 67.Pushpakumar SB, Banis JC, Jr, Knopf D, et al. Face transplantation: putting on a new face. Biochemist. 2007;29:20–23. [Google Scholar]
- 68.Sacks JM, Keith JD, Fisher C, et al. The surgeon’s role and responsibility in facial tissue allograft transplantation. Ann Plast Surg. 2007;58:595–601. [DOI] [PubMed] [Google Scholar]
- 69.Siemionow M, Bramstedt KA, Kodish E. Ethical issues in face transplantation. Curr Opin Organ Transplant. 2007;12:193–197. [Google Scholar]
- 70.Swindell JS. Facial allograft transplantation, personal identity and subjectivity. J Med Ethics. 2007;33:449–453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Barker JH, Brown CS, Cunningham M, et al. Ethical considerations in human facial tissue allotransplantation. Ann Plast Surg. 2008;60:103–109. [DOI] [PubMed] [Google Scholar]
- 72.Chenggang Y, Yan H, Xudong Z, et al. Some issues in facial transplantation. Am J Transplant. 2008;8:2169–2172. [DOI] [PubMed] [Google Scholar]
- 73.Fitchett JR. Facial reconstruction–the impact of facial allograft transplantation on surgery. Int J Surg. 2008;6:439–440. [DOI] [PubMed] [Google Scholar]
- 74.Johnson SE, Corsten MJ. Facial transplantation in a new era: what are the ethical implications? Curr Opin Otolaryngol Head Neck Surg. 2009;17:274–278. [DOI] [PubMed] [Google Scholar]
- 75.Lengelé BG. Current concepts and future challenges in facial transplantation. Clin Plast Surg. 2009;36:507–521. [DOI] [PubMed] [Google Scholar]
- 76.O’Neill H, Godden D. Ethical issues of facial transplantation. Br J Oral Maxillofac Surg. 2009;47:443–445. [DOI] [PubMed] [Google Scholar]
- 77.Park EE, Genden EM. Facial transplantation: the next frontier in head and neck reconstruction. Facial Plast Surg Clin North Am. 2009;17:271–277. [DOI] [PubMed] [Google Scholar]
- 78.Cypher JM. Agency and the dominant face: facial transplantation and the discourse of normalcy. Am Commun J. 2010;12. [Google Scholar]
- 79.Kalliainen LK. Supporting facial transplantation with the pillars of bioethics. J Reconstr Microsurg. 2010;26:547–554. [DOI] [PubMed] [Google Scholar]
- 80.Perpich D. Vulnerability and the ethics of facial tissue transplantation. J Bioeth Inq. 2010;7:173–185. [Google Scholar]
- 81.Strong C. An ongoing issue concerning facial transplantation: editorial. Am J Transplant. 2010;10:1115–1116. [DOI] [PubMed] [Google Scholar]
- 82.Paradis C, Siemionow M, Papay F, et al. Ethical considerations in the first American face transplant. Plast Reconstr Surg. 2010;126:896–901. [DOI] [PubMed] [Google Scholar]
- 83.Edwards JA, Mathes DW. Facial transplantation: a review of ethics, progress, and future targets. Transplant Research and Risk Management.2011;3:113–125. [Google Scholar]
- 84.Evans LA. A historical, clinical, and ethical overview of the emerging science of facial transplantation. Plast Surg Nurs. 2011;31:151–157. [DOI] [PubMed] [Google Scholar]
- 85.Kruvand M, Vanacker B. Facing the future: media ethics, bioethics, and the world’s first face transplant. J Mass Media Ethics. 2011;26:135–157. [Google Scholar]
- 86.Pirnay P, Hervé C, Meningaud JP. [Face allotransplantation: experimental? Care? How does one pass from one to another?]. Presse Med. 2011;40(12 Pt 1):1097–1099. [DOI] [PubMed] [Google Scholar]
- 87.Prior JJ, Klein O. A qualitative analysis of attitudes to face transplants: contrasting views of the general public and medical professionals. Psychol Health. 2011;26:1589–1605. [DOI] [PubMed] [Google Scholar]
- 88.Siemionow M. Ethical considerations in face transplantation: ethical issues related to inclusion criteria for face transplant candidates. Arch Immunol Ther Exp (Warsz). 2011;59:157–159. [DOI] [PubMed] [Google Scholar]
- 89.Arno A, Barret JP, Harrison RA, et al. Face allotransplantation and burns: a review. J Burn Care Res. 2012;33:561–576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Carty MJ, Bueno EM, Lehmann LS, et al. A position paper in support of face transplantation in the blind. Plast Reconstr Surg. 2012;130:319–324. [DOI] [PubMed] [Google Scholar]
- 91.Lantieri L. Face transplant: a paradigm change in facial reconstruction. J Craniofac Surg. 2012;23:250–253. [DOI] [PubMed] [Google Scholar]
- 92.Losee JE, Fletcher DR, Gorantla VS. Human facial allotransplantation: patient selection and pertinent considerations. J Craniofac Surg. 2012;23:260–264. [DOI] [PubMed] [Google Scholar]
- 93.Mardoyan S, Pinelli N. Reconstructive surgery and face transplants, reconstruction or creation? Soins. 2012;57:37–39. [PubMed] [Google Scholar]
- 94.Pirnay P, Foo R, Hervé C, et al. Ethical questions raised by the first allotransplantations of the face: a survey of french surgeons. J Craniomaxillofac Surg. 2012;40:e402–e407. [DOI] [PubMed] [Google Scholar]
- 95.Siemionow M, Ozturk C. Face transplantation: outcomes, concerns, controversies, and future directions. J Craniofac Surg. 2012;23:254–259. [DOI] [PubMed] [Google Scholar]
- 96.Siemionow M, Gharb BB, Rampazzo A. Successes and lessons learned after more than a decade of upper extremity and face transplantation. Curr Opin Organ Transplant. 2013;18:633–639. [DOI] [PubMed] [Google Scholar]
- 97.Kiwanuka H, Bueno EM, Diaz-Siso JR, et al. Evolution of ethical debate on face transplantation. Plast Reconstr Surg. 2013;132:1558–1568. [DOI] [PubMed] [Google Scholar]
- 98.Le Clainche-Piel M. Surgical innovation ethics and practices: the case of face transplantation. Sciences Sociales et Sante. 2013;31:59–85. [Google Scholar]
- 99.Taylor-Alexander S. On face transplantation: Ethical slippage and quiet death in experimental biomedicine (Respond to this article at http://www.therai.org.uk/at/debate). Anthropology Today. 2013;29:13–16. [Google Scholar]
- 100.Coffman KL, Siemionow MZ. Ethics of facial transplantation revisited. Curr Opin Organ Transplant. 2014;19:181–187. [DOI] [PubMed] [Google Scholar]
- 101.Flynn J, Shaul RZ, Hanson MD, Borschel GH, Zuker R. Pediatric facial transplantation: Ethical considerations. Can J Plast Surg. 2014;22:67–69. [PMC free article] [PubMed] [Google Scholar]
- 102.Khalifian S, Brazio PS, Mohan R, et al. Facial transplantation: the first 9 years. Lancet. 2014;384:2153–2163. [DOI] [PubMed] [Google Scholar]
- 103.Taylor-Alexander S. Bioethics in the making: “ideal patients” and the beginnings of face transplant surgery in Mexico. Sci Cult. 2014;23:27–50. [Google Scholar]
- 104.Garrett GL, Beegun I, D’souza A. Facial transplantation: historical developments and future directions. J Laryngol Otol. 2015;129:206–211. [DOI] [PubMed] [Google Scholar]
- 105.Petrini C. Facial transplants: current situation and ethical issues. Clin Ter. 2015;166:215–217. [DOI] [PubMed] [Google Scholar]
- 106.Bartlett SP, Chang B, Levin LS. Discussion: ethical issues in pediatric face transplantation: should we perform face transplantation in children? Plast Reconstr Surg. 2016;138:455–457. [DOI] [PubMed] [Google Scholar]
- 107.Marchac A, Kuschner T, Paris J, et al. Ethical issues in pediatric face transplantation: should we perform face transplantation in children? Plast Reconstr Surg. 2016;138:449–454. [DOI] [PubMed] [Google Scholar]
- 108.Molitor M. Transplantation of vascularized composite allografts. Review of current knowledge. Acta Chir Plast. 2016;58:18–28. [PubMed] [Google Scholar]
- 109.Russo JE, Genden EM. Facial transplantation. Facial Plast Surg Clin North Am. 2016;24:367–377. [DOI] [PubMed] [Google Scholar]
- 110.Siemionow M. The miracle of face transplantation after 10 years. Br Med Bull. 2016;120:5–14. [DOI] [PubMed] [Google Scholar]
- 111.Vasudeva Murthy CR, Nagashekhara M, Chyn LT, et al. Ethical, social and legal intricacies on facial transplant. Anthropologist. 2016;25:117–121. [Google Scholar]
- 112.Benghiac AG, Garrett JR, Carter BS. Ethical issues in pediatric face transplantation. Pediatr Transplant. 2017;21. [DOI] [PubMed] [Google Scholar]
- 113.Caplan A, Purves D. A quiet revolution in organ transplant ethics. J Med Ethics. 2017;43:797–800. [DOI] [PubMed] [Google Scholar]
- 114.Giatsidis G, Sinha I, Pomahac B. Reflections on a decade of face transplantation. Ann Surg. 2017;265:841–846. [DOI] [PubMed] [Google Scholar]
- 115.Lee J. Face transplantation for the blind: more than being blind in a sighted world. J Med Ethics. 2018;44:361–365. [DOI] [PubMed] [Google Scholar]
- 116.Pearl S. Saving faces. CMAJ. 2018;190:E511–E512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Tasigiorgos S, Kollar B, Krezdorn N, et al. Face transplantation-current status and future developments. Transpl Int. 2018;31:677–688. [DOI] [PubMed] [Google Scholar]
- 118.Warnke PH. Repair of a human face by allotransplantation. Lancet. 2006;368:181–183. [DOI] [PubMed] [Google Scholar]
- 119.Morris P, Bradley A, Doyal L, et al. Face transplantation: a review of the technical, immunological, psychological and clinical issues with recommendations for good practice. Transplantation. 2007;83:109–128. [DOI] [PubMed] [Google Scholar]
- 120.Siemionow M, Papay F, Alam D, et al. Near-total human face transplantation for a severely disfigured patient in the USA. Lancet. 2009;374:203–209. [DOI] [PubMed] [Google Scholar]
- 121.Bramstedt KA, Plock JA. Looking the world in the face: the benefits and challenges of facial transplantation for blind patients. Prog Transplant. 2017;27:79–83. [DOI] [PubMed] [Google Scholar]
- 122.Bosch X. Surgeon denied ethics approval for face transplantation. Lancet. 2004;363:871. [DOI] [PubMed] [Google Scholar]
- 123.Robertson JA. Face transplants: enriching the debate. Am J Bioeth. 2004;4:32–33; discussion W23. [DOI] [PubMed] [Google Scholar]
- 124.Huxtable R, Woodley J. Gaining face or losing face? Framing the debate on face transplants. Bioethics. 2005;19:505–522. [DOI] [PubMed] [Google Scholar]
- 125.Martin J. [Face transplantation: psychological, social, ethical and legal considerations]. Rev Med Suisse. 2005;1:583–584. [PubMed] [Google Scholar]
- 126.Carosella ED, Pradeu T. Transplantation and identity: a dangerous split? Lancet. 2006;368:183–184. [DOI] [PubMed] [Google Scholar]
- 127.Colas-Benayoun MD, Fidelle G, Favre JD. From disfigurement to transfiguration: is a face’s transplant the solution? Annales Medico-Psychologiques. 2006;164:687–691. [Google Scholar]
- 128.Daly CC. Saving face. South Med J. 2006;99:412–413. [DOI] [PubMed] [Google Scholar]
- 129.Delaporte F. [Partial facial transplantation. A surgical breakthrough]. Rev Prat. 2007;57:2314–2317. [PubMed] [Google Scholar]
- 130.Furr LA, Wiggins O, Cunningham M, et al. Psychosocial implications of disfigurement and the future of human face transplantation. Plast Reconstr Surg. 2007;120:559–565. [DOI] [PubMed] [Google Scholar]
- 131.Lengelé B. The rebuilt face: ethics, techniques and results of the first face allograft. Bull Mem Acad R Med Belg. 2007;162:179–191. [PubMed] [Google Scholar]
- 132.Lengelé BG, Testelin S, Dakpe S, et al. [”Facial graft”: about the first facial allotransplantation of composite tissues]. Ann Chir Plast Esthet. 2007;52:475–484. [DOI] [PubMed] [Google Scholar]
- 133.Szajerka T, Jabłecki J, Szajerka A. Face transplantation - new possibilities and risks. Adv Clin Exp Med. 2007;16:323–328. [Google Scholar]
- 134.Tobin GR, Breidenbach WC, 3rd, Pidwell DJ, et al. Transplantation of the hand, face, and composite structures: evolution and current status. Clin Plast Surg. 2007;34:271, ix–278, ix. [DOI] [PubMed] [Google Scholar]
- 135.Grayling AC. Face transplantation and living a flourishing life. Lancet. 2008;371:707–708. [DOI] [PubMed] [Google Scholar]
- 136.White BE, Brassington I. Facial allograft transplants: where’s the catch? J Med Ethics. 2008;34:723–726. [DOI] [PubMed] [Google Scholar]
- 137.Edgar A. The challenge of transplants to an intersubjectively established sense of personal identity. Health Care Anal. 2009;17:123–133. [DOI] [PubMed] [Google Scholar]
- 138.Cunningham MR, Barker JH. Response to: Clarke and Butler: patient selection for facial transplantation II: psychological considerations. Int J Surg. 2004;2:117–118. [DOI] [PubMed] [Google Scholar]
- 139.Huxtable R, Woodley J. (When) will they have faces? A response to Agich and Siemionov. J Med Ethics. 2006;32:403–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Freeman M, Abou Jaoudé P. Justifying surgery’s last taboo: the ethics of face transplants. J Med Ethics. 2007;33:76–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Lengelé B, Testelin S, Cremades S, et al. Facing up is an act of dignity: lessons in elegance addressed to the polemicists of the first human face transplant. Plast Reconstr Surg. 2007;120:803–806. [DOI] [PubMed] [Google Scholar]
- 142.Meningaud JP. [Ethical and juridical context of the facial allotransplant]. Ann Chir Plast Esthet. 2007;52:513–518. [DOI] [PubMed] [Google Scholar]
- 143.Pirnay P, Herve C, Meningaud JP. [Have we answered all the ethical issues concerning composite tissue allotransplantation of the face?]. Rev Stomatol Chir Maxillofac Chir Orale. 2013;114:53–56. [DOI] [PubMed] [Google Scholar]
- 144.Parent B. Faces as organ donations: who has the last word? Hastings Cent Rep. 2014;44:1p following 48. [DOI] [PubMed] [Google Scholar]
- 145.Gilman SL. Facial transplants: what are authentic faces? Acta Hist Leopoldina. 2016:171–182. [PubMed] [Google Scholar]
- 146.‘Social anonymity’: The ethics of facial transplantation. Br Dent J. 2016;221:126. [DOI] [PubMed] [Google Scholar]
- 147.Rifkin WJ, Manjunath A, Kimberly LL, et al. Long-distance care of face transplant recipients in the United States. J Plast Reconstr Aesthet Surg. 2018;71:1383–1391. [DOI] [PubMed] [Google Scholar]
- 148.Goering S. Facing the consequences of facial transplantation: individual choices, social effects. Am J Bioeth. 2004;4:37–39; discussion W23. [DOI] [PubMed] [Google Scholar]
- 149.Cabrera AE, Kimberly LL, Kantar RS, et al. Perceived esthetic outcomes of face transplantation: a survey of the general public. J Craniofac Surg. 2018;29:848–851. [DOI] [PubMed] [Google Scholar]
- 150.Chambers T. How to do things with AJOB: the case of facial transplantation. Am J Bioeth. 2004;4:20–21. [DOI] [PubMed] [Google Scholar]
- 151.Devauchelle B, Badet L, Lengelé B, et al. First human face allograft: early report. Lancet. 2006;368:203–209. [DOI] [PubMed] [Google Scholar]
- 152.The United States position: position paper of the American Society for Reconstructive Microsurgery on facial transplantation. South Med J. 2006;99:430. [DOI] [PubMed] [Google Scholar]
- 153.Guo S, Han Y, Zhang X, et al. Human facial allotransplantation: a 2-year follow-up study. Lancet. 2008;372:631–638. [DOI] [PubMed] [Google Scholar]
- 154.Lantieri L, Meningaud JP, Grimbert P, et al. Repair of the lower and middle parts of the face by composite tissue allotransplantation in a patient with massive plexiform neurofibroma: a 1-year follow-up study. Lancet. 2008;372:639–645. [DOI] [PubMed] [Google Scholar]
- 155.Alam DS, Papay F, Djohan R, et al. The technical and anatomical aspects of the world’s first near-total human face and maxilla transplant. Arch Facial Plast Surg. 2009;11:369–377. [DOI] [PubMed] [Google Scholar]
- 156.ANSA R. Face transplant- rejection suspected. http://www.ansa.it/english/news/science_tecnology/2018/09/24/face-transplant-rejection-suspected_00a4ecc7-c630-438e-a6b1-c35ee9fd522b.html. Accessed November 19, 2018.
- 157.Cooney CM, Siotos C, Aston JW, et al. The ethics of hand transplantation: a systematic review. J Hand Surg Am. 2018;43:84.e1–84.e15. [DOI] [PubMed] [Google Scholar]
- 158.Siemionow M, Gatherwright J, Djohan R, et al. Cost analysis of conventional facial reconstruction procedures followed by face transplantation. Am J Transplant. 2011;11:379–385. [DOI] [PubMed] [Google Scholar]
- 159.Theodorakopoulou E, Meghji S, Pafitanis G, et al. A review of the world’s published face transplant cases: ethical perspectives. Scars Burn Heal. 2017;3:2059513117694402. [DOI] [PMC free article] [PubMed] [Google Scholar]


