Abstract
We present an interesting case of a 66-year-old male who had acute testicular infarction following a right common femoral artery to left profunda femoris artery bypass with advanced symptoms of claudication. Angiography in the preoperative period demonstrated the extent of peripheral arterial disease present, revealing a calcified aorta, partially occluded left hypogastric artery, occluded left external iliac, common femoral and superficial femoral arteries and an occluded right hypogastric artery. A bypass was performed without any initial complications and subsequent relief of symptoms of claudication and rest pain. Postoperative scrotal pain and follow-up duplex demonstrated lack of perfusion of the testicle necessitating orchiectomy. This case serves to illustrate the importance of preserving collateral vessels as a technical consideration, as well as presenting a rare potential complication.
INTRODUCTION
Atherosclerosis is a progressive disease that, when affecting the aorta and iliac arteries, manifests as symptomatic arterial insufficiency. These symptoms can vary from claudication to tissue loss. Historically, anatomic reconstructions were the treatment of choice. Introduced in the early 1950s, femorofemoral crossover bypass grafting became an alternative treatment option to those with prohibitive risk factors for anatomic reconstructions. Endovascular treatment for peripheral arterial disease began in the 1960s and has become the standard of care for revascularization. The primary indication for performing a femorofemoral bypass is the presence of symptomatic unilateral iliac artery occlusive disease unamenable to percutaneous transluminal balloon angioplasty [1, 2].
In chronic limb ischemia, the development of collateral blood supply compensates for the lack of inline blood flow. The process of neovascularization or arteriogenesis is the development of new blood vessels to supply chronically ischemic areas, bypassing a stenotic or occluded artery [3]. Preservation of end branch collaterals can be vital to prevent ischemia; however, the development of collateral vessels is unpredictable. This is highlighted by a unique complication of testicular infarction following femorofemoral bypass, a complication only previously described following endovascular infrarenal aortic aneurysm repair [4].
CASE REPORT
We present the case of a 66-year-old male with a several month history of left leg rest pain. Of note, the patient had a remote history of testicular seminoma as a child, for which he underwent a right orchiectomy.
Workup began with noninvasive studies of the left lower extremity displaying aortoiliac occlusive disease and infrainguinal disease. Aortogram demonstrated a severely calcified aorta, patent left common iliac and proximal hypogastric arteries, with occlusion of the left external iliac, left common femoral and left superficial femoral arteries (Fig. 1). The right iliac system was patent apart from an occluded right hypogastric artery. A selective left lower extremity angiogram demonstrated reconstitution of the mid-to-distal profunda femoris artery (Fig. 2) to the proximal above-knee popliteal artery at the adductor hiatus (Fig. 3). Extensive collateralization was appreciated in the pelvis and lower extremity, between the residual left hypogastric artery and profunda femoris artery. Endovascular revascularization attempts were unsuccessful.
Figure 1.
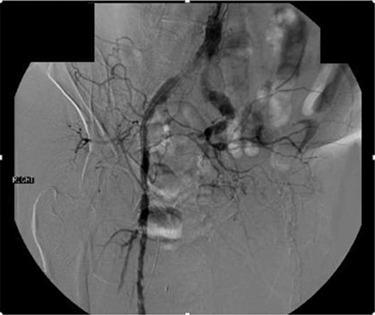
Aortogram demonstrating occlusion of left distal hypogastric, external iliac and common femoral arteries, as well as right hypogastric artery
Figure 2.
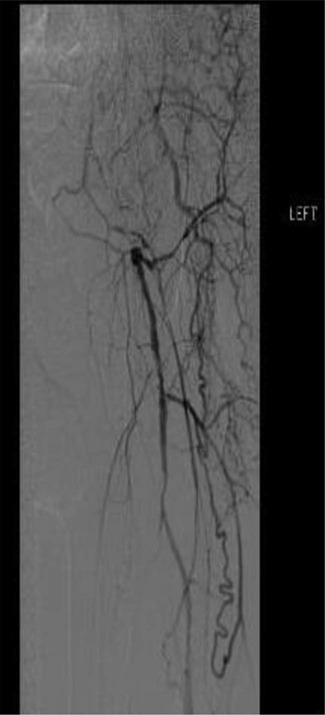
Selective left lower extremity angiogram demonstrating patent mid-to-distal profunda femoris artery and its collaterals
Figure 3.
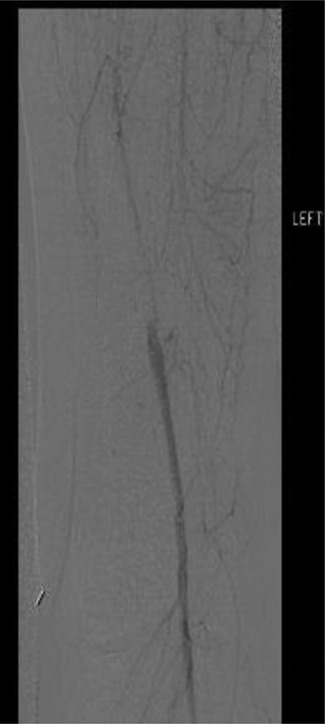
Selective left lower extremity angiogram demonstrating reconstitution of the above-knee popliteal artery at the adductor canal
A right common femoral to left profunda artery bypass was recommended to improve inflow to the left lower extremity with consideration that a left profunda to above-knee popliteal bypass may be needed if symptoms did not resolve.
The patient underwent a right common femoral to left profunda femoris artery bypass with a 6-mm ring polytetrafluoroethylene graft. During dissection of the left profunda femoris artery, many collateral vessels were appreciated, with care taken to preserve them. The procedure concluded uneventfully, with newly acquired posterior tibial artery signal in the left foot and continued signals in the right foot.
On postoperative day 3, the patient developed bilateral incisional and scrotal erythema with fever and leukocytosis. Despite empiric antibiotic treatment, the patient became increasingly septic. No signs of graft infection were demonstrated on ultrasound or computed tomography scan. A testicular ultrasound duplex displayed the absence of arterial perfusion of the left testis. As a result, simple left orchiectomy was performed. An infarcted testis without evidence of torsion or malignancy was identified on final pathology. Following the procedure, the sepsis resolved, and the patient remained free of rest pain.
DISCUSSION
The treatment of aortoiliac occlusive disease is typically done by endovascular techniques, hybrid endovascular-surgical approach or open surgical bypass. Open surgical techniques involve anatomic aortofemoral bypass or extra-anatomic axillofemoral bypass versus femorofemoral bypass. Reported patency rates for femorofemoral bypass compared with aortobifemoral bypass are 60 versus 83%, respectively, at 3 years [5]. Despite its lower patency rate, femorofemoral bypass is the most widely used primary procedure for reconstruction of unilateral iliac artery disease when compared with bypasses originating in the aorta [6]. Reported surgical complications of femorofemoral bypass include superficial and deep wound infections, graft thrombosis, lymphocele, perigraft hematoma, groin/scrotal hematoma, graft infection, pseudoaneurysm, femoral nerve injury, development of inguinal hernias and femoral steal syndrome [7]. This case illustrates a rare potential complication of acute testicular infarction following femorofemoral bypass.
The blood supply to the testicles provides insight to how this complication may have arisen. The testicular arteries receive their blood supply directly from the infrarenal aorta before descending through the inguinal canal. Collaterals may develop through the cremasteric artery, a branch of the inferior epigastric off the external iliac or the artery to the vas deferens, a branch of the inferior vesical artery off the internal iliac artery [8]. We suspect that the testicular artery was occluded as the infrarenal aorta was severely calcified. There was no visualization of the inferior vesical artery when the angiogram was reviewed retrospectively. The proximal left internal iliac arteries were patent; therefore, the artery to the vas deferens may have been patent. Extensive collaterals in the region were seen; however, identification of blood supply to the testicle was inconclusive.
The cruciate anastomosis provides a connection between the internal iliac and femoral arteries. It involves the inferior gluteal, medial femoral circumflex, lateral femoral circumflex and first perforating arteries, which are branches of the profunda femoris [9]. With occlusion of the external iliac and common femoral arteries, this cruciate anastomosis provides blood flow to the deep femoral system. The presence of this anastomosis and extensive collateral network provided perfusion to the lower extremity and tenuous perfusion to the testis.
At some point during the femorofemoral bypass, collateral blood flow was compromised resulting in ischemia to the testicle. Damage to collaterals can be a result of inadvertent clamping, tunneling or ligation during exposure. Excessive manipulation or traction injury can cause thrombosis of small collaterals. Gentle handling of the tissues, careful vascular manipulation and intraoperative preservation of all vessel branches may aid in preventing this type of complication.
Presently, femorofemoral bypass is the most widely used primary procedure for reconstruction of unilateral iliac artery disease. This case highlights the importance of collateral blood supply with a unique complication of testicular infarction. Meticulous care should be taken to preserve all collateral blood flow in a patient with compromised native vessels. While this is not a routine complication following femorofemoral bypass, it is essential to point out the importance of surgical technique.
Conflict of Interest STATEMENT
None declared.
REFERENCES
- 1. Stanley JC, Veith FJ, Wakefield TW. Current Therapy in Vascular and Endovascular Surgery, 5th edn. Philadelphia, PA: Elsevier Saunders, 2014; 452–458. [Google Scholar]
- 2. Criado E, Burnham SJ, Tinsley EA Jr, Johnson G Jr, Keagy BA. Femorofemoral bypass graft: analysis of patency and factors influencing long-term outcome. J Vasc Surg 1993;18:495–505. [PubMed] [Google Scholar]
- 3. Cronenwett JL, Johnston KW. Rutherford’s Vascular Surgery, 8th edn. Philadelphia, PA: Elsevier Saunders, 2014, [Google Scholar]
- 4. McKenna MB, Gambardella I, Collins A, Harkin DW. Testicular infarction: a rare complication of endovascular aneurysm repair treatment for aortoiliac aneurysm. J Vasc Surg 2009;50:1487–9. [DOI] [PubMed] [Google Scholar]
- 5. Schneider JR, Besso SR, Walsh DB, Zwolak RM, Cronenwett JL. Femorofemoral versus aortobifemoral bypass: outcome and hemodynamic results. J Vasc Surg 1994;19:43–55. [DOI] [PubMed] [Google Scholar]
- 6. Piotrowski JJ, Pearce WH, Jones DN, Whitehill T, Bell R, Patt A, et al. Aortobifemoral bypass: the operation of choice for unilateral iliac occlusion? J Vasc Surg 1988;8:211–8. [DOI] [PubMed] [Google Scholar]
- 7. Kawamura YJ, Futakawa N, Oshiro H, Yasuhara H, Shigematsu H, Muto T. Bilateral inguinal hernia repaired by laparoscopic technique: a rare complication of femorofemoral bypass. Surg Endosc 1999;13:1157–9. [DOI] [PubMed] [Google Scholar]
- 8. McDougal WS, Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA. Campbell-Walsh Urology, 11th edn. Philadelphia, PA: Elsevier Saunders, 2011; 498–515. [Google Scholar]
- 9. Snell RS. Clinical Anatomy: By Regions, 9th edn. Baltimore, MD: Lippincott, Williams, and Wilkins, 2012; 461–465. [Google Scholar]


