Abstract
We evaluated the benefit of glossopharyngeal nerve block with long acting local anaesthetic like bupivacaine. It was a randomized prospective study. Sixty-four patients were selected and divided into two groups. Group A received bilateral nerve block and Group B received no block. Pain score using Visual Analog Scale (0–100 mm) was assessed at 30 min, 2, 6 and 12 h. In the immediate post operative period pain scores of Group A at rest and swallowing was significantly lower than Group B (p < 0.001 and p < 0.01). Glossopharyngeal nerve block is an important method of reducing post-tonsillectomy pain.
Keywords: Pain, Bupivacaine, Glossopharyngeal nerve block, VAS
Introduction
Tonsillectomy is one of the most frequently performed procedure by an otolaryngologist. Haemorrhage, airway obstruction due to edema are the most serious complications observed post operatively after tonsillectomy. Pain is the most common complaint in early post-operative period. Pain causes anxiety and fear with individual variations and predisposes to delayed food intake, limits respiratory effort with increased chance of pulmonary complications and lengthens stay in hospital [1]. Pain intensity differs with surgical techniques and pharmacological treatment [2–4]. There are different patterns of pain; mostly presents with decreasing score, few have increased score during first week while others have pain from beginning decreasing gradually [5].
Post-operative pain begins with surgical trauma. In addition to trauma stimulation of peripheral pain receptors, central sensitization plays an important role. The inhibition of central sensitisation by local or systemics drugs is known as pre-emptive analgesia that helps to control post-operative pain [6]. Pre-emptive analgesia has been tried with opiods, steroids and NSAIDS as well as local anaesthetics sprays and infiltration in tonsillar fossa [7–10].
Controversy regarding efficacy of Glossopharyngeal nerve block (GNB) have been reported. Few studies reported GNB or modified peritonsillar infiltration to be effective [11, 12]. Others have reported block with 0.5% bupivacaine have no effect on post-operative pain [13, 14]. In view of this setting, we decided to carry out this study to see whether any benefit of GNB can be seen over conventional techniques using opiods, steroids or analgesics in reduction of pain.
Aims and Objectives
To evaluate the efficacy of glossopharyngeal nerve block using Visual Analog Scale (VAS 0–100 mm) in immediate post-operative period.
Materials and Methods
This was a prospective randomised controlled study carried out in Department of Otolaryngology in a Tertiary Care Hospital from January 2016 to November 2017. Institutional Ethical Committee permission was taken previously. Informed written consent was taken from every participating patients. We selected patients more than 18 years with ASA 1 category. The patients who presented to us with Chronic Tonsillitis or recurrent quinsy patients were included in our study. We excluded those patients who had cardiac, liver or renal impairment, swallowing difficulty, allergy, acute infection, bleeding disorders, pain due to other chronic disease and neoplastic changes of tonsil.
After detailed history taking, clinical examination and investigation patients were randomly assigned into two groups. Everyone involved in the study was blinded to group allocation except for the surgeon. Group A would receive 0.5% bupivacaine nerve block whereas Group B would receive no block.
All patients were pre-operatively explained how to express pain score using Visual Analog Scale (0–100 mm). Patients were premedicated with coamoxyclav, ondansetron and pantoprazole injections.
2% Povidone Iodine gargle was given the night before operation and coming morning. The nerve block was given pre-incisionally (waiting period of 5 min).
The glossopharyngeal nerve (cranial nerve IX) is a mixed function nerve with motor, sensory, and special sensory fibers. The rootlets originate in the upper part of the post-olivary sulcus and exit the cranium with parasympathetic nerve fibers from the salivatory nucleus, the vagus and spinal accessory nerves (CN X and XI) via the jugular foramen. All three cranial nerves lie between the internal jugular vein and the internal carotid artery. The glossopharyngeal nerve has many distributive branches including the tympanic, carotid, pharyngeal, muscular, tonsillar, and lingual of which the pharyngeal branch carries sensory nerve from the walls of the pharynx, the tonsillar branch transmits sensory nerves from the tonsils and the lingual branch innervates the anterior surface of the epiglottis, the posterior third of the tongue, and the vallecula. The motor component innervates the stylopharyngeus muscle, which elevates the pharynx during talking and swallowing. Sensory portion innervates the palatine tonsils, posterior third of the tongue, and mucous membranes of the oropharynx. Special sensory afferent fibers transmit taste sensation from posterior third of tongue.
The GNB was carried out by anterior tonsillar pillar method (ATP). In this method, the tongue is displaced medially, forming a gutter (glossogingival groove). A 25-gauge spinal needle is inserted at the base of the anterior tonsillar pillar, just lateral to the base of the tongue, to a depth of 0.5 cm. After negative aspiration for blood or air, 0.5% Bupivacaine in a dose of 2 mg/kg mixed in 2.5 ml normal saline is injected. The process is then repeated on the contralateral side.
Two other methods are present for this block. Extraoral (Peristyloid technique)—The patient is placed supine with the head rotated slightly opposite from the affected side. The styloid process is used to identify the course of the GPN. Once identification of the mastoid process and the ipsilateral angle of the mandible is performed, the styloid process can be found equidistant between these structures. A small skin wheal is made over the styloid process using a 25-gauge, 1.5-in. needle and 3–4 mL of 1% plain lidocaine. Next, a 22-gauge, 1.5–2 in blunt-tipped needle may be advanced perpendicular to the skin toward the process, aiming for its posterior aspect. The styloid process should be met at a depth approximating 1.5–4 cm. Once the styloid process is encountered, the needle is slightly withdrawn and “walked off” posteriorly. Aspiration should be performed to ensure that there is no blood or cerebrospinal fluid. Next, 1 mL of water-soluble, iodinated contrast media should be incrementally injected under live continuous fluoroscopy. Since live fluoroscopy is required we avoided this method.
Posterior tonsillar pillar—The patient is asked to open the mouth widely. The tongue is depressed down with a laryngoscope blade or else with a tongue blade as described above. A 22-gauge, 3.5-in. spinal needle bent 1 cm from the distal end is directed laterally into the submucosa along the caudal aspect of the PTP (palatopharyngeal fold). After careful aspiration for blood and cerebrospinal fluid, 2 mL of local anesthetic and/or steroid is injected. The PTP method becomes more difficult in patients with large tongues or small oral opening and may cause greater gag reflex.
Cold steel method was used for all patients undergoing tonsillectomy.
Pain scores were measured at 30 min in recovery room and 2, 6 and 12 h post operatively. Post-operatively patient received:
Inj. Coamoxyclav
Inf. Metrogyl
Inf. Paracetamol (1 gm BD)
Inj. Pantoprazole
Statistical Analysis
To present a 25-mm pain score difference as significant at the 0.05 level with a power of > 90%, a minimum of 30 patients is required in each group. The comparison of variables for pain score at rest and swallowing and time by GNB treatment interaction was calculated using a general linear model (ANOVA).
Results
A total of 64 patients were included in our study. The mean age in Group A was 28.5 (SD ± 4.2) and in Group B was 30.4 (SD ± 3.6). The demographic pattern is expressed in Table 1. In Group A the gender ratio (M:F) was 20:12 and in Group B 18:14. The mean weight in Group A was 58.4 (SD ± 6.2) and in Group B 62.5 (SD ± 7.4).
Table 1.
Demographic pattern [Data in Table expressed as mean (SD)]
| Group A | Group B | |
|---|---|---|
| Age | 28.5 (4.2) | 30.4 (3.6) |
| Gender (M/F) | 20/12 | 18/14 |
| Weight | 58.4 (6.2) | 62.5 (7.4) |
The VAS score at rest for Group A continuously decreased for first 6 h and then at 12 h pain increased which was due to weaning effect of action of bupivacaine. There was no such relation between pain scores in Group B at 6 and 12 h.
The VAS score at rest is expressed in following Table 2 and Fig. 1.
Table 2.
VAS score at rest [data expressed as mean (SD)]
| Group A | Group B | |
|---|---|---|
| 30 min | 11.45 (7.28) | 52.46 (9.90) |
| 2 h | 8.31 (6.66) | 50.25 (10.20) |
| 6 h | 6.90 (4.78) | 51.74 (9.68) |
| 12 h | 14.63 (8.34) | 49.63 (8.72) |
Fig. 1.
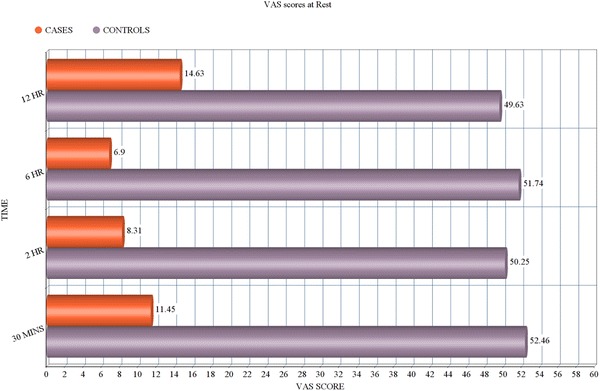
VAS score at rest
The VAS score at swallowing was comparatively more than at rest at all interval of measurement. However the score similarly showed decrease for 1st 6 h and then increased at 12 h. The pain score of Group B had did not show decrease as in Group A.
The VAS score at swallowing is expressed in Table 3 and Fig. 2.
Table 3.
VAS score at swallowing [data expressed as mean (SD)]
| Group A | Group B | |
|---|---|---|
| 30 min | 15.26 (7.83) | 53.14 (9.15) |
| 2 h | 16.62 (9.10) | 54.76 (7.56) |
| 6 h | 18.52 (9.47) | 54.95 (7.24) |
| 12 h | 25.46 (8.74) | 56.41 (9.21) |
Fig. 2.
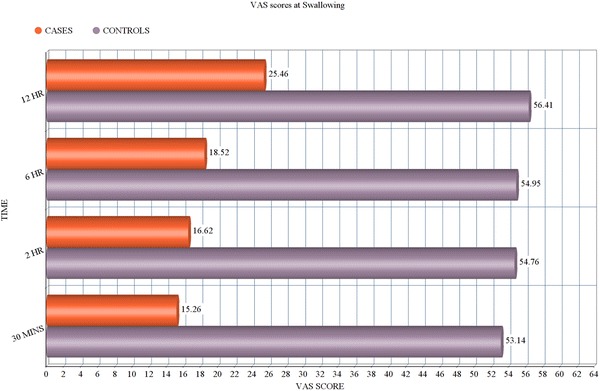
VAS Score at swallowing
The time-by-GNB treatment interaction was statistically significant (P < 0.01 at rest and P < 0.01 at swallowing).
The P value (Group A v/s Group B) for VAS at rest was < 0.001 and VAS at swallowing was < 0.01
The gag reflex observed in recovery room was absent in 10 patients in Group A (31.25%) and in 2 patients in Group B (6.25%).
The Adverse reactions are tabulated below which shows bupivacaine toxicity in the form of hypotension and bradycardia in 2 patients among group A. Foreign body sensation seen in 14 patients of group A while 11 patients of group B. Dysphagia is seen among 7 patients of group a and 4 patients of group B. Dyspnea and hoarseness are found among 2 and 1 patient of group A while no patients of group B had such complications.
| Group A | Group B | |
|---|---|---|
| Bupivacaine toxicity (hypotension, bradycardia) | 2 | 0 |
| Foreign body sensation | 14 | 11 |
| Dysphagia | 7 | 4 |
| Dyspnea | 2 | 0 |
| Hoarsesness | 1 | 0 |
Discussion
This single blinded randomized controlled trial demonstrated a statistical benefit of GNB in patients undergoing tonsillectomy. Previously Jebes et al. [15] had demonstrated the benefit of GNB in children among 22 patients undergoing tonsillectomy. However their sample size was small. They also included children in their study so, their study become less reliable. Our study included adults who could complete their own VAS scores.
Though gag reflex was absent in 10 patients no correlation could be obtained with VAS scores at swallowing. Successful GNB is an important factor for post tonsillectomy pain relief. Hee-Pyoung Park [16] had demonstrated statistical correlation between gag reflex and extent of post tonsillectomy pain. However we did not observe such effect in our study.
In few studies use of normal saline as placebo has been tried [17]. However in our study we did not use normal saline because comparison between placebo with non-intervention has been associated with bleeding [18].
Previous studies using electrocautery as dissection method have shown to increase post-operative morbidity in terms of pain when compared with blunt dissection technique [19]. Hence we used blunt dissection technique in our study.
We encountered some adverse effects due to glossopharyngeal nerve block which may be explained by following reasoning: As we are blocking bilateral Glossopharyngeal nerve, Dysphagia may be seen due to (7 patients in Group A) due to weakness of stylopharyngeus. As well as protective reflexes (gag reflex) was absent in 10 patients in Group A. We found hoarseness in 1 patient of Group A which may be explained due to secondary vagus nerve block and ipsilateral vocal cord paralysis temporarily. Out of 32 patients, 2 patients were found to have hypotension and bradycardia which can be explained due to toxicity of bupivacaine.
Our study had few limitations. Firstly we did not follow the pain score beyond 12 h. Studies that have measured pain score at 24 h and even till 1 week have not found any statistical benefit [20]. Secondly our study population did not include paediatric patients because of the complex method of assessment of pain.
Conclusion
At present use of LA in controlling pain after tonsillectomy is a subject of controversy. Our assessment of pain is still not accurate. Pain is an expression that is affected by many factors that show considerable inter-individual variations. Though our study has shown statistical benefit however randomized, prospective and double blinded studies are very very few in number and requires further exploration as different institutes have different methods of management and surgical approach.
Compliance with Ethical Standards
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical Approval
The permission was taken from Institutional Ethics Committee prior to starting the project. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual Participants included in the study.
References
- 1.Topal K, Aktan B, Sakat MS, Kilic K, Gozeler MS. Post-operative pain control after tonsillectomy: dexametasone vs tramadol. Acta Otolaryngol. 2017;137(6):618–622. doi: 10.1080/00016489.2016.1269945. [DOI] [PubMed] [Google Scholar]
- 2.Kamal SA, Basu S, Kapoor L, Kulandaivelu G, Talpalikar S, Papasthatis D. Harmonic scalpel tonsillectomy: a prospectivestudy. Eur Arch Otorhinolaryngol. 2006;263(449–54):3. doi: 10.1007/s00405-005-1022-2. [DOI] [PubMed] [Google Scholar]
- 3.Ozkiris M, Kapusuz Z, Saydam L. Comparison of three techniques in adult tonsillectomy. Eur Arch Otorhino-laryngol. 2013;270:1143–1147. doi: 10.1007/s00405-012-2160-y. [DOI] [PubMed] [Google Scholar]
- 4.Ragab SM. Six years of evidence-based adult dissection tonsillectomy with ultrasonic scalpel, bipolar electrocautery, bipolarradiofrequency or ‘cold steel’ dissection. J Laryngol Otol. 2012;126:1056–1062. doi: 10.1017/S0022215112002022. [DOI] [PubMed] [Google Scholar]
- 5.Sarny S, Habermann W, Ossimitz G, Stammberger H. Significant post-tonsillectomy pain is associated with increased risk of hemorrhage. Ann Otol Rhinol Laryngol. 2012;121:776–781. doi: 10.1177/000348941212101202. [DOI] [PubMed] [Google Scholar]
- 6.Kissin I. Preemptive analgesia. Anesthesiology. 2000;93:1138–1143. doi: 10.1097/00000542-200010000-00040. [DOI] [PubMed] [Google Scholar]
- 7.Hanasono MM, Lalakea ML, Mikulec AA, Shepard KG, Wellis V, Messner AH. Perioperative steroids in tonsillectomy using electrocautery and sharp dissection techniques. Arch Otolaryngol Head Neck Surg. 2004;130:917–921. doi: 10.1001/archotol.130.8.917. [DOI] [PubMed] [Google Scholar]
- 8.Naesh O, Niles LA, Gilbert JG, Ammar MM, Phibbs PW, Phillips AM, Khrapov AV, Robert AJ, McClintock A. A randomized, placebo-controlled study of rofecoxib with paracetamol in early post-tonsillectomy pain in adults. Eur J Anaesthesiol. 2005;7(22):768–773. doi: 10.1017/S0265021505001274. [DOI] [PubMed] [Google Scholar]
- 9.Valijan A. Pain relief after tonsillectomy. Effect of benzydamine hydrochloride spray on postoperative pain relief after tonsillectomy. Anaesthesia. 1989;44:990–991. doi: 10.1111/j.1365-2044.1989.tb09205.x. [DOI] [PubMed] [Google Scholar]
- 10.Ginstrom R, Silvola J, Saarnivaara L. Local bupivacaineepinephrine infiltration combined with general anesthesia for adult tonsillectomy. Acta Otolaryngol. 2005;125:972–975. doi: 10.1080/00016480510043413. [DOI] [PubMed] [Google Scholar]
- 11.Spence AG. Single injection field block of tonsillar fossa. Anaesth Intensive Care. 1996;24:621–623. [PubMed] [Google Scholar]
- 12.Bruin G. Glossopharyngeal nerve block for tonsillectomy or uvulopalatopharyngoplasty. Can J Anaesth. 1994;41:1236. doi: 10.1007/BF03020671. [DOI] [PubMed] [Google Scholar]
- 13.Bell KR, Cyna AM, Lawler KM, Sinclair C, Kelly PJ, Millar F, Flood LM. The effect of glossopharyngeal nerve block on pain after elective adult tonsillectomy and uvulopalatoplasty. Anaesthesia. 1997;52:597–602. doi: 10.1111/j.1365-2222.1997.131-az0127.x. [DOI] [PubMed] [Google Scholar]
- 14.El-Hakim H, Nunez DA, Saleh HA, MacLeod DM, Gardiner Q. A randomised controlled trial of the effect of regional nerve blocks on immediate post-tonsillectomy pain in adult patients. Clin Otolaryngol. 2000;25:413–417. doi: 10.1046/j.1365-2273.2000.00397.x. [DOI] [PubMed] [Google Scholar]
- 15.Jebeles JA, Reilly JS, Gutierrez JF, Bradley EL, Jr, Kissin I. The effect of preincisional infiltration of tonsils with bupivacaine on the pain following tonsillectomy under general anaesthesia. Pain. 1991;47:305–308. doi: 10.1016/0304-3959(91)90220-R. [DOI] [PubMed] [Google Scholar]
- 16.Park H-P, Hwang J-w, Park S-H, Jeon Y-T, Bahk J-H, Oh Y-S. The effects of glossopharyngeal nerve block on postoperative pain relief after tonsillectomy: the importance of the extent of obtunded gag reflex as a clinical indicator. Anesth Analg. 2007;105:267–271. doi: 10.1213/01.ane.0000266440.62424.f1. [DOI] [PubMed] [Google Scholar]
- 17.Schoem SR, Watkins GL, Kuhn JJ, Alburger JF, Kim KZ, Thompson DH. Control of early postoperative pain with bupivacaine in adult local tonsillectomy. Arch Otolaryngol Head Neck Surg. 1993;119(3):292–293. doi: 10.1001/archotol.1993.01880150040007. [DOI] [PubMed] [Google Scholar]
- 18.Broadman LM, Patel RI, Feldman BA, Sellman GL, Milmoe G, Camilon F. The effects of peritonsillar infiltration on the reduction of intraoperative blood loss and post-tonsillectomy pain in children. Laryngoscope. 1989;99:578–581. doi: 10.1288/00005537-198906000-00002. [DOI] [PubMed] [Google Scholar]
- 19.Atallah N, Kumar M, Hilali A, Hickey S. Post-operative pain in tonsillectomy: bipolar electrodissection technique vs dissection ligation technique. A double-blind randomized prospective trial. J Laryngol Otol. 2000;114(9):667–670. doi: 10.1258/0022215001906679. [DOI] [PubMed] [Google Scholar]
- 20.Sharifian HA, Fathololoomi MR, Bafghi AF, Naini SAS. Effect of local bupivacaine infiltration on post-tonsillectomy pain. Tanaffos. 2006;5(1):45–49. [Google Scholar]


