Abstract
Basal cell adenocarcinoma (BCAC) is a rare tumour entity. Despite its tendency to be infiltrative and destructive tumour with propensity to recur, it rarely metastasizes and long-term outcome following surgery is favourable. This paper presents a 42-year-old male with residual BCAC of parotid gland that had extended into infratemporal fossa and intracranial. The important aspect of this case is the rarity occurrence of BCAC of parotid with intracranial extension and its surgical approaches to achieve tumour clearance.
Keywords: Basal cell adenocarcinoma, Parotid tumour, Intracranial extension, Tumour resection
Introduction
Basal cell adenocarcinoma (BCAC) is a rare subtype of salivary gland neoplasm. It is a malignant counterpart of basal cell adenoma in which the behaviour of BCAC is invasive and destructive with perineural and vascular invasion [1]. It is classified as a low grade tumour in 2005 WHO classification [2] but with high recurrence rate [2, 3]. In general, BCAC has a good prognosis and metastasis is rare [4]. BCAC comprises 2.9% of malignant salivary gland neoplasm and 1.6% of all salivary gland neoplasm [1]. It can be divided into 4 subtypes: tubulotrabecular, solid, canalicular and membranous [5]. Most cases arise exclusively in major salivary glands except canalicular type which occurs almost always in intraoral minor salivary glands [5]. Intracranial extension from BCAC of parotid gland has not been reported in literature.
The present case will provide first documented BCAC of parotid gland with intracranial extension that required two surgical approaches—transparotid and transcranial approach, to achieve tumour clearance.
Case Report
A 42-year-old Malay male, diagnosed with right parotid BCAC had underwent subtotal parotidectomy at other centre, presented to us with recurrence of swelling over right parotid area which started about 2 months post-operatively. The swelling was gradually increased in size and painless. He also noticed new non-painful swelling over right upper cervical neck. Following the previous surgery, he had iatrogenic right temporal branch facial nerve palsy but other facial nerve branches were intact. Clinical examination revealed a firm and fixed non-tender mass at right parotid area measuring 3 × 3 cm with no overlying skin changes. There was also right level 2 firm cervical mass measuring 2 × 3 cm possibly matted lymph nodes. Computed tomography (CT) and magnetic resonance imaging (MRI) were performed and demonstrated right posterolateral neck soft tissue mass measuring 2.3 × 4 × 5 cm with extension into infratemporal fossa and intracranial (Figs. 1, 2). Both CT and MRI showed that the mass had diffused infiltrating pattern to adjacent structures in which it had infiltrated the right masseter muscle, eroded subjacent right zygomatic arch and right condylar process of mandible. An ENT and neurosurgery team had worked together to do the completion of parotidectomy with resection of infratemporal and intracranial mass via transparotid and transcranial approach (Fig. 3) with selective neck dissection. Histopathology result was reported as BCAC with no lymph nodes metastases. Patient is currently undergoing radiotherapy and presently still under follow-up.
Fig. 1.
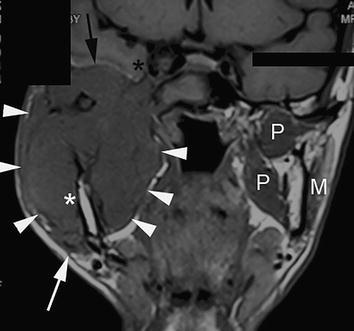
Coronal T1-weighted spin echo sequence of the head and neck region demonstrates the mass (white arrowheads) occupying almost the entire right infratemporal fossa, replacing the muscles of the masticator space i.e. right pterygoid and masseter muscles. The normal contralateral pterygoid and masseter muscles are annotated P and M respectively, for comparison. The parapharyngeal space (beneath the arrowheads) is effaced, whilst laterally the platysma muscle (white arrow) bulges with mass effect. The tumour also engulfs the ramus (white asterisk) and condylar process of the right mandible. Tumour encroachment into the right middle cranial fossa is noted (black arrow), with tumour proximity to the right cavernous sinus and cavernous ICA (black asterisk)
Fig. 2.
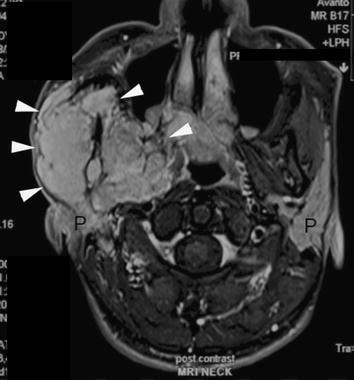
Axial fat suppressed post-Gadolinium sequence of the right neck shows the avid enhancement of the right infratemporal fossa mass, engulfing the ramus of the right mandible. Residual right and native left parotid glands are annotated as P
Fig. 3.
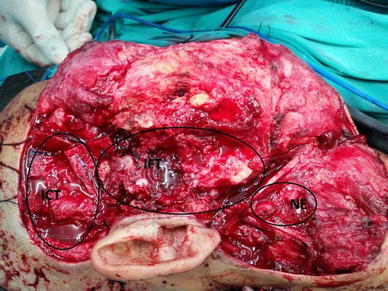
Intra-operative image demonstrates mass in the infratemporal fossa (IFT), area of intracranial extension of mass covered by neurosurgical patties (ICT) and extension of mass into cervical neck region (NF)
Discussion
Majority of more than 90% of BCAC involved the parotid gland [6]. It usually arises in adult above 60 years old and has no gender predilection [2]. BCAC shows high local recurrence rate of 28–76% due to its infiltrative and destructive nature [7]. While they are locally destructive and often recurred, metastases are rare and only have occurred in <10% of patient [8]. In term of biological behaviour, BCAC is a low grade salivary gland tumour and rarely results in mortality. Therefore, the overall prognosis is excellent [9] in which the long-term outcome following surgery is favourable [8]. Metastasis of parotid carcinoma to cervical lymph node, liver, lung, orbit and intracranial along with perineural invasion of facial nerve has been described in literature [10]. The intracranial involvement of salivary gland tumour is rare and most reported cases are from adenocystic carcinoma of parotid gland [11]. Our case will provide the first documented BCAC of parotid gland with intracranial extension and its management.
In general, primary management of BCAC is surgical resection with negative margin to ensure complete removal of mass [1]. Regional lymph node dissection is recommended only if there is evidence of significant lymphadenopathy on clinical or radiologic examination, and postoperative radiation is recommended for a closed surgical margin or following surgical excision of recurrent tumour [12]. Radiotherapy also has been proposed for lesion in minor salivary gland, or for tumour with diffuse infiltrating pattern to adjacent tissue [3, 4, 12]. Therefore, most studies advocate surgical excision with wide margin and close follow-up [3, 4, 6].
In the present case, the tumour bulk has grown into infratemporal fossa and intracranial. In order to achieve tumour clearance, we utilized two separate surgical approaches—transparotid and transcranial. In combination with neurosurgery team, 2 surgical incisions were made: first is extended modified blair incision for the transparotid approach and second is temporal flap incision for transcranial approaches to remove the intracranial tumour. In the middle of procedure, both incisions were incorporated. With these surgical approaches, we managed to achieve total tumour clearance. We also proceeded with ipsilateral selective neck dissection for level II, III and IV as there was initially suspected cervical lymph nodes metastases on clinical examination, but after biopsy confirmed, it is an extension of tumour. Post-operatively, patient was subjected for radiotherapy as the tumour showed diffused infiltrating pattern to adjacent tissue.
Conclusion
Here a rare case of BCAC of parotid with intracranial extension and its surgical approaches to achieve tumour clearance is presented.
Compliance with Ethical Standards
Conflict of interest
Mohamad Norkahfi Razali declares that he has no conflict of interest. Marina Mat Baki declares that she has no conflict of interest. Kew Thean Yean declares that he has no conflict of interest. Mohd Razif Mohamad Yunus declares that he has no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
References
- 1.Sharma R, Saxena S, Bansal R. Basal cell adenocarcinoma: report of a case affecting the submandibular gland. J Oral Maxillofac Pathol. 2007;11:56–59. doi: 10.4103/0973-029X.37382. [DOI] [Google Scholar]
- 2.Barnes L, Eveson JW, Reichart P, Sidransky D. Pathology and genetics of tumours of the head and neck. Lyon: IARC Press; 2005. pp. 229–230. [Google Scholar]
- 3.Farrell T, Chang YL. Basal cell adenocarcinoma of minor salivary glands. Arch Pathol Lab Med. 2007;131:1602–1604. doi: 10.5858/2007-131-1602-BCAOMS. [DOI] [PubMed] [Google Scholar]
- 4.Ward BK, Seethala RR, Barnes EL, Lai SY. Basal cell adenocarcinoma of a hard palate minor salivary gland: case report and review of the literature. Head Neck Oncol. 2009;1:41. doi: 10.1186/1758-3284-1-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ellis GI, Wischvitch JG. Basal cell adenocarcinomas of the major salivary gland. Oral Surg Oral Med Oral Pathol. 1990;69:461–469. doi: 10.1016/0030-4220(90)90380-B. [DOI] [PubMed] [Google Scholar]
- 6.Parashar P, Baron E, Papadimitriou J, Ord R, Nikitakis N. Basal cell adenocarcinoma of the oral minor salivary glands: review of the literature and presentation of two cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol. 2007;103:77–84. doi: 10.1016/j.tripleo.2005.12.021. [DOI] [PubMed] [Google Scholar]
- 7.Kudo S, Sawai T, Ikeda K, Watanabe M, Oshima T, Nakabayashi T, Takasaka T. A case of basal cell adenocarcinoma of the parotid gland. Tohoku J Exp Med. 1998;186:51–59. doi: 10.1620/tjem.186.51. [DOI] [PubMed] [Google Scholar]
- 8.Elvey MH, Aghasi M, Wasrbrout Z, Avisar E. Metastasis of parotid basal cell adenocarcinoma to the hand—a case report. Hand. 2011;6:321–323. doi: 10.1007/s11552-011-9333-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Faquin WC, Powers C. Salivary gland. Cytopathology. 2008;268:164–176. [Google Scholar]
- 10.Franzen A, Koegel K, Knieriem HJ, Pfaltz M. Basal cell adenocarcinoma of the parotid gland: a rare tumor entity: case report and review of the literature. HNO. 1998;46:821–825. doi: 10.1007/s001060050319. [DOI] [PubMed] [Google Scholar]
- 11.Wilson JR, Kumar R, van Hille PT. Cerebellopontine angle metastasis of a parotid mucoepidermoid carcinoma arising from perineural invasion along the facial nerve. Br J Neurosurg. 2012;26(3):417–419. doi: 10.3109/02688697.2011.625061. [DOI] [PubMed] [Google Scholar]
- 12.Hirsch DL, Miles C, Dierks E. Basal cell adenocarcinoma of the parotid gland: report of a case and review of the literature. J Oral Maxillofac Surg. 2007;65:2385–2388. doi: 10.1016/j.joms.2006.07.021. [DOI] [PubMed] [Google Scholar]


