Abstract
The management of oral carcinoma leads to both cosmetic and functional deficit to the patient and the confirmatory histopathology is a time consuming process which may be a reason for a reduced follow up and compliance of the patient. We hereby use this study as an opportunity to tell that narrow band imaging (NBI) serves both the above purposes in an earlier period and in a non-invasive manner and thereby improving the lifestyle of the patients. To find out a better non-invasive and time saving diagnostic tool in the management of premalignant and malignant oral lesions in its earlier period. A prospective cross sectional study of 38 patients presenting to the department of ENT, MGMMC, MYH, Indore was taken with suspicious lesions and subjected to endoscopic examination by both white light and NBI and samples were sent to histopathological examination for confirmation. The Intrapapillary Capillary Loop were identified through NBI with Type I (50%) and Type II (31%) to be the most common pattern both correlating with the histopathological squamous cell carcinoma. The sensitivity and specificity of White Light Endoscopy is to be 75.75% and 76.43% respectively and of NBI to be 93.93% and 80% respectively. Narrow band imaging is found to be an optical diagnostic tool in the diagnosis of the lesions at an earlier stage and preventing from further functional and structural deterioration by the disease progression.
Keywords: White light endoscopy, Narrow band imaging, Intrapapillary capillary loops, Histopathology
Introduction
Oral cancers are heterogenous group of cancers arising either synchronously or metachronously from different anatomical parts with different predisposing factors, prevalance and treatment outcomes. It is the eleventh most common cancer globally [1] and in the top three cancers in the Indian subcontinent with rate of 20 per 100,000 population accounting for over 30% of all cancers in the country [2]. About 80% of oral cancers are due to tobacco and alcohol and others could be due to Human Papilloma virus infection and rarely due to radiation or occupational exposure.
Over 90% of the oral cancers are squamous cell carcinoma. The treatment of choice for Stage I and II is surgical and/or radiotherapy and for Stage III and IV is a combined surgery and chemoradiotherapy. Despite the advances in surgical technique and the chemoradiotherapy drugs the 5 year survival rate is not so good in these patients and also leading to both cosmetic and functional deficits like difficulty in articulation, chewing and swallowing. Thus identification of these tumors in a very earlier stage is a challenge.
The efforts to achieve the earliest detection of these tumors has led to the invention of the newer endoscopic technique like autofluorescence, optical coherence tomography and narrow band imaging (NBI) [3, 4]. NBI which has already proved to be a better screening tool in the field of Gastroenterology and Urology, is emerging in the field of ENT and Head and Neck Surgery.
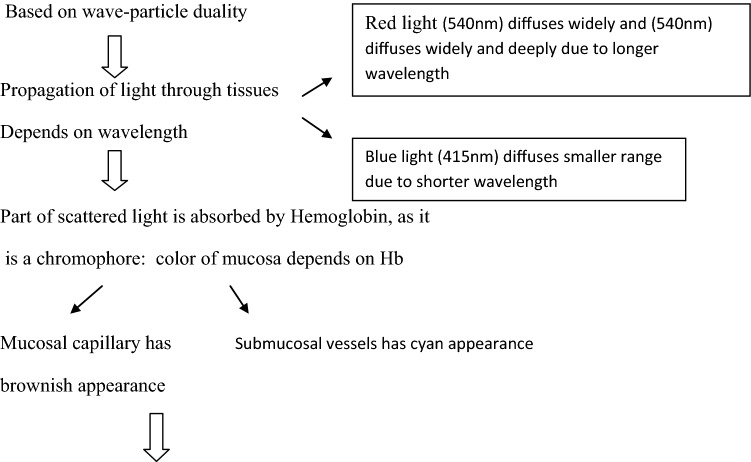
Principle of NBI
On the NBI image, the thin capillary network on the mucosal surface taken by blue light (415 nm) has a brownish appearance and thick blood vessels in the submucosal surface taken by red light (540 nm) have a cyan (blue) appearance [3].
Narrow Band Imaging
Earlier and Better Identification of the Malignant Changes Following Neovascularisation
Methods
The study was a prospective cross sectional study for a period of 1 year from April 2017 to April 2018 and was carried out in the Department of Otorhinolaryngology, Mahatma Gandhi Memorial Medical College and M.Y. Hospital, Indore, Madhya Pradesh (M.P).
Inclusion Criteria
Age group between 20 and 70 years.
Patients with suspected oral premalignant and malignant lesions, who presented with complaints of ulcers in oral cavity, pain over the ulcers, pain on swallowing, difficulty in opening mouth and swelling in cheek and neck.
Exclusion Criteria
Age group below 20 years and above 70 years
Patients who did not give consent for the study
Patients who presented with oropharyngeal and laryngeal lesions
Already biopsy proven cancer patients
Patients who came with recurrent lesions
Though many patients present to the ENT department with symptoms of various head and neck tumors, only a total of 38 patients who fit into the inclusion criteria were taken for the study because this study is mainly on oral cavity tumors. After taking proper consent, the patients were subjected to a detailed clinical history regarding symptoms and substance abuse including its duration. Then they were subjected to endoscopic examination, initially by the conventional white light endoscopy followed by narrow band imaging through OLYMPUS VISERA ELITE OTV-S190 VIDEO SYSTEM. The lesions showing neovascularisation were classified into four types based on the capillary loops and the submucosal vessels changes [5] as;
Type 1: Regularly distributed intra epithelial capillary loop
Type 2: Dilated and tortuous intra epithelial microvasculature
Type 3: Elongated and twisted intra epithelial microvasculature
Type 4: Intraepithelial papillary capillary loop destruction
Punch biopsy was taken from the area showing abnormal vascular loops and the sample was sent for histopathological confirmation and finally the NBI IPCL types and the histopathological diagnosis were correlated with each other.
Results
The most common affected age group is the 5th decade of 36.84% followed by 4th and 6th decade each with 21.05%. The male population constitute about 60.52% with a Male:Female ratio of 1.5:1
Based on the topographical location, the most commonly affected anatomical structure is the buccal mucosa with 21 cases followed by tongue, more specifically dorsolateral border with 9 cases.
Among the 38 cases, 32 cases showed neovascularisation with 50% showing Intrapapillary Capillary Loop (IPCL) Type I, 31% showing IPCL type II and 19% IPCL type III. The lesions showing Type I and II IPCL group correlated with the low grade histopathological finding and the lesions with Type III correlated with high grade histopathology (Figs. 1, 2, 3).
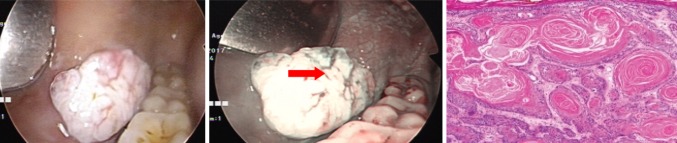
Fig. 1.
Type I IPCL—showing significant brown dots with regularly distirbuted capillary loops
Fig. 2.
Type II IPCL—showing dilated vessels
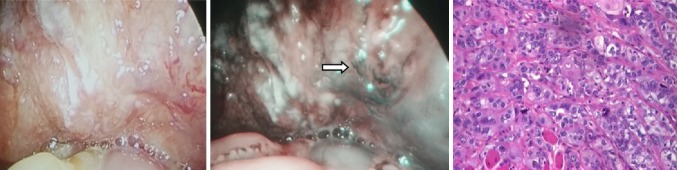
Fig. 3.
Type III IPCL—showing elongated and branching vascular pattern
Discussion
In this study, the most common age group affected is the 5th decade followed by 4th and 6th decade. Akilesh Krishna et al. [6] also found that most of the squamous cell carcinoma are common in the age group between 51 and 60 years followed by 41–50, which is consistent with this study (Tables 1, 2).
Table 1.
Correlation between IPCL type and histopathological diagnosis
| IPCL type I | IPCL type II | IPCL type III | |
|---|---|---|---|
| Hyperplasia/dysplasia | 1 | – | – |
| Carcinoma in situ | 3 | – | – |
| Well differentiated squamous cell CA | 12 | 9 | – |
| Moderately differentiated squamous cell CA | – | 1 | 4 |
| Poorly differentiated squamous cell CA | – | – | 2 |
| Total | 16 | 10 | 6 |
* 6 out of 38 patients showed no neovascularisation in NBI
Table 2.
Statistical analysis between wle and NBI
| Sensitivity (%) | Specificity (%) | Positive predictive value (%) | Negative predictive value (%) | |
|---|---|---|---|---|
| WLE | 75.75 | 76.43 | 0 | 33.33 |
| NBI | 93.93 | 80 | 3.125 | 66.66 |
The sensitivity, specificity, PPV and NPV of WLE is found to be 75.75%, 76.43%, 0% and 33.33% respectively and with NBI to be 93.93%, 80%, 3.125%, 66.66% respectively
About 60.52% patients were males with M:F of 1.5:1, is correlating with Aroquiadasse et al. [7] study. They found that, among the 112 patients of potentially malignant oral disease included in their study, 71% were males and 29% were females.
The male predominance is due to the more prevalent habit of tobacco chewing and smoking among them. Due to the increased prevalence of tobacco addiction and the lifestyle changes the common age group affected has decreased to 5th decade from the earlier 6th and 7th decade.
In central India, as tobacco chewing is the most common cause of oral carcinoma and the habit of keeping tobacco in the oral vestibular region, buccal mucosa and the dorsolateral border of tongue has got a longer contact period making them the most vulnerable region. The saliva in the vestibular region dilutes the carcinogens (mainly NITROSAMINES) and releasing it slowly adding to the vulnerability of the region. This above result is found to be correlating with both the following study:
Kandath et al. [8] found that buccal mucosa was the most affected site with 42.6% among oral squamous cell carcinoma patients as with this study.
Znaor et al. [9] found relationship between the tobacco chewing and smoking in relation to oral, pharyngeal and oesophageal cancer. He found that tobacco chewing is associated with 2–3 fold increased risk of oral cancer.
Though most of the patients presented with ulcerative or proliferative growth, the NBI IPCL types gave us an idea about the histopathological grading of the lesions which helped in further treatment. Among the 16 cases of Type I IPCL, 12 cases were well differentiated squamous cell carcinoma, 3 cases were carcinoma in situ lesions, 1 case of dysplasia lesion. Among the type II IPCL of 10 cases, 9 cases were well differentiated squamous cell carcinoma and 1 case was moderately differentiated carcinoma. Among the 6 cases of Type III IPCL, 4 cases were moderately differentiated squamous cell carcinoma and 2 cases were poorly differentiated carcinoma.
The sensitivity, specificity, PPV and NPV of WLE is found to be 75.75%, 76.43%, 0% and 33.33% respectively and with NBI to be 93.93%, 80%, 3.125%, 66.66% respectively.
In finding the malignant lesions, the diagnostic ability of the narrow band imaging is almost equal to the Histopathology and superior compared to white light endoscopy making the diagnosis more accurate in less time and yielding good results in a non-invasive manner.
Vu et al. [10] in 2014 studied the efficacy of NBI for the detection of potentially malignant and malignant oral and oropharyngeal lesions. The sensitivity, specificity, PPV, NPV and accuracy for White Light Endoscopy ranged between 56 and 96%, 60–100%, 33–100%, 87–99% and 66–89% respectively, whereas it was 87–96%, 94–98%, 73–96%, 97–98% and 92–97% respectively for NBI. Thus they proved that NBI is much more efficacious than standard endoscopy which correlated with our study [11, 12].
Yang et al. [5] found that the sensitivity, specificity, positive predictive value, negative predictive value, and accuracy were 80.95%, 78.43%, 60.71%, 90.91%, and 79.17%, respectively, which was significant (p < 0.001).
Vu et al. [10] in 2018 found that the pooled sensitivity, specificity, positive likelihood rate, negative likelihood rate of NBI were 88.5%, 95.6%, 12.33 and 0.11, respectively. The overall area under the curve of summary receiver operating characteristic (SROC) was 96.94%, thus proving that NBI is a promising endoscopic tool in diagnosis of head and neck tumors [13–19].
Conclusion
The results obtained by visualizing the vascular loops called the intrapapillary capillary loop is comparable with the histopathology, which is the gold standard but report comes with a waiting time thereby making NBI an optical confirmatory test for identification of the lesion in the premalignant stage.
In the field of otorhinolaryngology, use of NBI is at a rudimentary level and this study is a sincere attempt to open the gates to initiate and stimulate its utility in this field. Still more studies should be done in the future involving NBI more routinely so that more premalignant lesions can be picked up and appropriate care be instituted with best results for our patients by preventing the further progression of the disease and also preventing the structural and functional deformity in our patients.
Compliance with Ethical Standards
Conflict of interest
The authors hereby disclose that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Human and Animal and Rights
This article does not contain any studies with animals performed by any of the authors.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ghantous Y, Yaffi V, Abu-Elnaaj I. Oral cavity cancer: epidemiology and early diagnosis article in Hebrew. Refuat Hapeh Vehashinayim. 2015;32(3):55–63. [PubMed] [Google Scholar]
- 2.Coelho KR. Challenges of the oral cancer burden in India. J Cancer Epidemiol. 2012;2012:701932. doi: 10.1155/2012/701932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gono K. narrow band imaging: technology basis and research and development history. Clin Endosc. 2015;48:476–480. doi: 10.5946/ce.2015.48.6.476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee MM, Enns R, et al. Narrow band imaging in gastroesophageal reflux disease and barrett’s esophagus. Can J Gastroentrol. 2009;23(2):84–87. doi: 10.1155/2009/732481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yang S, Lee Y, Chang L, Hwang C, Luo C, Chen T. Clinical characteristics of narrow-band imaging of oral erythroplakia and its correlation with pathology. BMC Cancer. 2015;15:406. doi: 10.1186/s12885-015-1422-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Krishna A, Singh RK, Singh S, Verma P, Pal US, Tiwari S. Demographic risk factors, affected anatomical sites and clinicopathological profile for oral squamous cell carcinoma in a north indian population. Asian Pac J Cancer Prev. 2014;15(16):6755–6760. doi: 10.7314/APJCP.2014.15.16.6755. [DOI] [PubMed] [Google Scholar]
- 7.Aroquiadasse M, Daniel MJ, Srinivasan SV, Jimsha VK. Correlation of degree of dysplasia in potentially malignant disorders with tobacco use: a cross-sectional study. Clin Cancer Investig J. 2016;5:398–402. doi: 10.4103/2278-0513.197870. [DOI] [Google Scholar]
- 8.Kandath S, John B, Shobitha G. Oral cancer profile among patients who underwent oral biopsy in a tertiary referral center in central kerala. Indian J Multidiscip Dent. 2017;7:14–20. doi: 10.4103/ijmd.ijmd_66_16. [DOI] [Google Scholar]
- 9.Znaor A, Brennan P, Gajalakshmi V, Mathew A, Shanta V, Varghese C, Boffetta P. Independent and combined effects of tobacco smoking, chewing and alcohol drinking on the risk of oral, pharyngeal and esophageal cancers in indian men. Int J Cancer. 2003;105:681–686. doi: 10.1002/ijc.11114. [DOI] [PubMed] [Google Scholar]
- 10.Vu AN, Farah CS. Efficacy of narrow band imaging for detection and surveillance of potentially malignant and malignant lesions in the oral cavity and oropharynx: a systematic review. Oral Oncol. 2014;50(5):413–420. doi: 10.1016/j.oraloncology.2014.02.002. [DOI] [PubMed] [Google Scholar]
- 11.Garofolo S, et al. Intraloperative narrow band imaging better delineates superficial resection margins during transoral laser microsurgery for early glottis cancer. Ann Otol Rhinol Laryngol. 2015;124(4):294–298. doi: 10.1177/0003489414556082. [DOI] [PubMed] [Google Scholar]
- 12.Tirelli G, Piovesana M, Gatto A, Torelli L, Di Lenarda R, Boscolo Nata F. NBI utility in the pre-operative and intra-operative assessment of oral cavity and oropharyngeal carcinoma. Am J Otolaryngol. 2017;38(1):65–71. doi: 10.1016/j.amjoto.2016.09.020. [DOI] [PubMed] [Google Scholar]
- 13.Piazza C, Dessouky O, Peretti G, Cocco D, De Benedetto L, Nicolai P, et al. Narrow-band imaging: a new tool for evaluation of head and neck squamous cell carcinomas. Review of the literature. Acta Otorhinolaryngol Italica. 2008;28:49–54. [PMC free article] [PubMed] [Google Scholar]
- 14.Gono K, Obi T, Yamaguchi M, et al. Appearance of enhanced tissue features in narrow-band endoscopic imaging. J Biomed Opt. 2004;9:568–577. doi: 10.1117/1.1695563. [DOI] [PubMed] [Google Scholar]
- 15.Hamamoto Y, Endo T, Nosho K, et al. usefulness of narrow-band imaging endoscopy for diagnosis of barrett’s esophagus. J Gastroenterol. 2004;39:14–20. doi: 10.1007/s00535-003-1239-z. [DOI] [PubMed] [Google Scholar]
- 16.Muto M, Nakane M, Katada C, Sano Y, Ohtsu A, Esumi H, et al. squamous cell carcinoma in situ at oropharyngeal and hypopharyngeal mucosal sites. Cancer. 2004;101:1375–1381. doi: 10.1002/cncr.20482. [DOI] [PubMed] [Google Scholar]
- 17.Watanabe A, Tsujie H, Taniguchi M, Hosokawa M, Fujita M, Sasaki S. Laryngoscopic detection of pharyngeal carcinoma in situ with narrowband imaging. Laryngoscope. 2006;116:650–654. doi: 10.1097/01.mlg.0000204304.38797.34. [DOI] [PubMed] [Google Scholar]
- 18.Lin Y, Watanabe A, Chen W-C, Lee K-F, Lee I-L, Wang W-H. Narrowband imaging for early detection of malignant tumors and radiation effect after treatment of head and neck cancer. Arch Otolaryngol Head Neck Surg. 2010;136(3):234–239. doi: 10.1001/archoto.2009.230. [DOI] [PubMed] [Google Scholar]
- 19.Zhou H, Zhang J, Guo L, Nie J, Zhu C, Ma X. The value of narrow band imaging in diagnosis of head and neck cancer: a meta-analysis. Sci Rep. 2018;8:515. doi: 10.1038/s41598-017-19069-0. [DOI] [PMC free article] [PubMed] [Google Scholar]