Abstract
In the era of globalisation, numerous technical methods have emerged in the management of benign laryngeal lesions. Still cold knife endolaryngeal surgery holds the basic and effective position in providing excellent voice outcome. The aim of this study is to assess the cold knife as a tool for excision of benign laryngeal lesions by protocol of voice assessment. Fifty-five patients with benign vocal fold lesions were included (26 women and 29 men), with age ranging from 22 to 56 years. Each patient was subjected to endoscopic microlaryngeal surgery with cold instruments. Voice assessment was done preoperatively and 3 weeks postoperatively and 3 month post-operatively. The patients were assessed subjectively by Voice Problem Self-Assessment Scale and objectively by laryngoscopy, stroboscopy, and acoustic analysis. Outcome was measured by comparing preoperative and postoperative groups. Significant improvement (< 0.05) was observed in the voice handicap index, acoustic parameters and video stroboscopy parameters between the preoperative and the postoperative groups. The cold knife endo-laryngoscopic surgery still stands out to be a simple, cost effective yet efficient way in treating majority of benign vocal fold lesions causing hoarseness of voice.
Keywords: Benign vocal lesion, Stroboscopy, PRAAT, Objective voice analysis, VHI, GRB, MPT
Introduction
As Richard Strauss quotes “the human voice is the most beautiful instrument of all, but it is the most difficult to play”; it is quite evident how pivotal role voice holds in our lives. Although this is an era of text messages thankfully, the primary mode of communication both socially and personally is vocal. Voice impairment due to benign vocal fold lesions is not only functional difficulty as in ICD-79 but reason of social problems too.
Benign vocal fold lesions are the commonest laryngeal lesions that lead to hoarseness and further affect the quality of life [1]. Surgical excision of vocal fold lesions like cyst, polyp, hard nodule and papilloma is a very effective way to improve voice in these conditions.
Various surgical techniques have been established in the management of these lesions i.e., cold knife surgery, laser that can be carbon dioxide laser [2] or diode laser [3] etc. But in a developing country with limited facilities, laryngeal surgeries with cold knife is an affordable measure, with an easy learning curve, less operative time and without having any deterioration in the quality of treatment.
In this study we measured the improvement in patients with benign vocal cord lesion underwent cold knife endolaryngeal surgeries with voice assessment by subjective/objective measures and using video stroboscopy to analyse condition of vocal folds [4].
Aim of study to assess the improvement of vocal fold and voice after cold knife endolaryngeal surgery using subjective, objective and video- stroboscopic parameters.
Materials and Methods
This prospective study was conducted in department of ENT, MGM Medical College, Indore (M.P.), which is a tertiary referral center. Duration of study was taken as 2012–2018.
Inclusion criteria Participants of the study were selected from adult patients who attended ENT OPD with the history of change in voice/hoarseness of voice/heaviness of voice as a predominant symptom for minimum 3 months or associated symptoms of other complaints like voice fatigue, cough, chronic throat pain, foreign body sensation, dryness of throat will be taken up for the study.
Exclusion criteria Fluency and articulation disorder, functional and psychological dysphonia, with co-morbidities like uncontrolled diabetes or hypertension and malignant lesions of vocal cord, systemic conditions affecting voice, Patients who did not give consent for the study were excluded from the study.
On further examination via indirect laryngoscopy benign lesions of vocal cord like vocal fold polyps, nodules, papilloma, cysts and Reinke’s oedema were diagnosed and confirmed by video laryngoscopy using Karl Storz 70° rigid endoscope and stroboscopy [5] was performed.
Brief Procedure
Fifty-five cases of benign vocal fold lesions were prospectively assessed by voice handicap index (VHI), maximum phonation time(MPT), Acoustic measures using PRAAT software and video laryngoscopy–stroboscopy. Participants were explained the details regarding the study and informed consent taken.
VHI i.e. voice handicap index was done by Hindi version of VHI [6] (mother tongue of the patient) a form with 30 simple questions regarding voice was given to the patient. During VHI testing the individual has to read each question and indicate how severely each statement applies to individual situation. Responses were scored from 0 to 4 for each question. Rating is done as 0 = never to always = 4, which can give a maximum score of 120. On completion of the Voice Handicap Index, the scores were tabulated for total score.
Patient’s voice was recorded in a sound proof room at most comfortable pitch, each subject was asked to count numbers in Hindi and say vowel “ee” and to measure maximum phonation time by asking patient to speak same vowel in a single breath in most comfortable pitch 3 times, the best of all attempt was recorded.
For perceptual analysis done by GRB Score which is a modification of GRBAS scale proposed by Hirano [7] but as the behavioural parameters ‘asthenicity’ and ‘strain’ are currently less reliable and have been omitted from the basic protocol. The remaining simplified scale, GRB [4] audios were recorded digitally and played for 3 observers: a speech language pathologist, an experienced ENT surgeon and the author grade of hoarseness, roughness and breathiness in 4 point scale of 0–3.
For objective analysis Voice sample was subjected to PRAAT application [8] which is a software to analyze voice to measure acoustic measurements.
Video laryngoscopy-stroboscopy was done under local anaesthesia spray in same sitting with Karl Storz 70° rigid laryngoscope and stroboscope. Videos were rated blindly by an experienced otorhinolaryngologist, the author and a speech language pathologist in different sitting.
All patients underwent endolaryngeal microsurgery on vocal fold that was performed using Kantor berci operating laryngoscope and 15° Storz endoscope fixed with chest piece over mayo’s stand .3 chip camera attached with monitor placed in front of surgeon for a wide and clear vision as shown in Figs. 1 and 2.
Fig. 1.

Endoscopic cold knife vocal cord surgery setup
Fig. 2.

Instruments used for the surgery
In all cases Hydro dissection [8] was done and micro flap incision technique used. After blunt dissection lesion was excised. Remaining mucosa was rewrapped over vocal fold (Fig. 3).
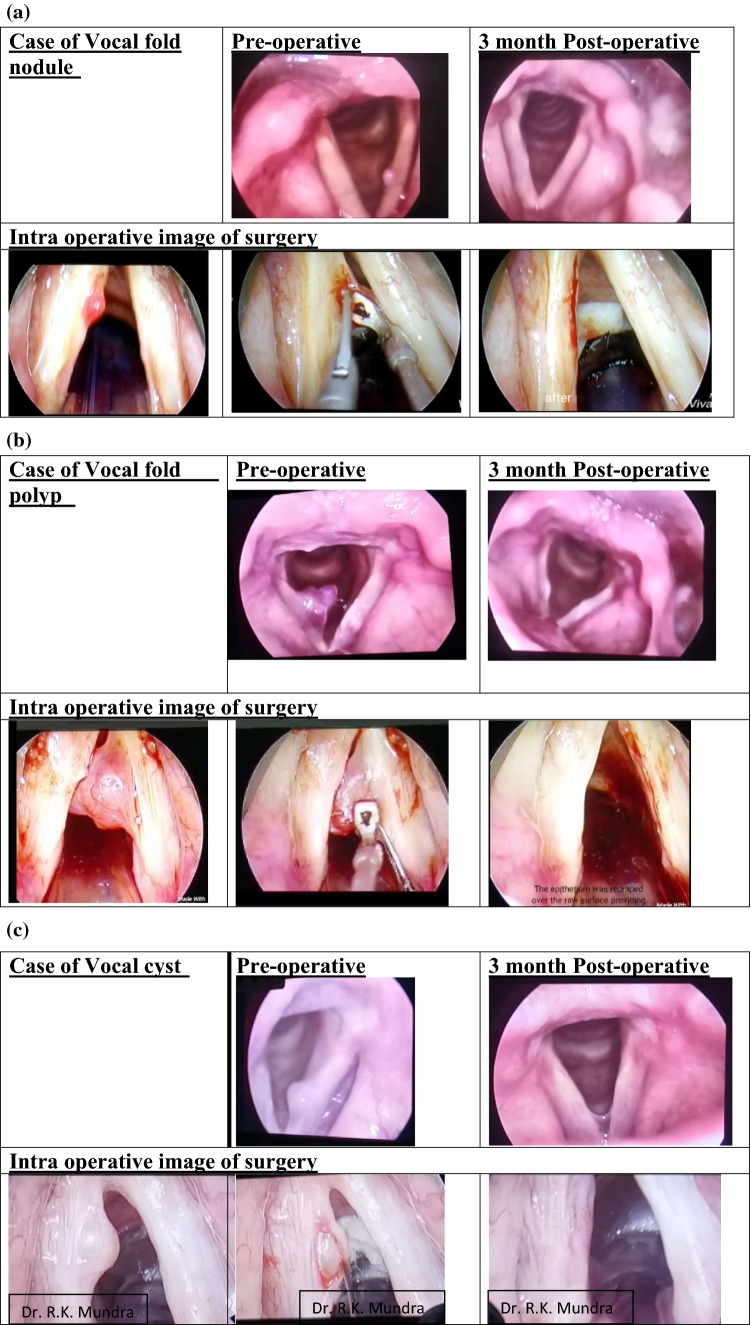
Fig. 3.
a–c Preoperative, intraoperative and 3 month post-operative images of vocal nodule, polyp and cyst respectively
Patients were reassessed by subjective analysis as VHI and Perceptual analysis objective analysis of voice by maximum phonation time and acoustic analysis and videostroboscopy during followup at 3 weeks and 3 months.
The results were statistically assessed and compared preoperative and 3 month post-operative by paired t test for quantitative data and Chi square test for qualitative data.
Results
In this study of 55, all patients underwent endoscopic micro laryngeal surgery with 29 males and 26 females (M:F is 1.11).
40% subjects were in 3rd decade (30–40) while 34% in 4th decade (40–50).
Most common lesion was vocal fold cyst in 20 patients, 17 with vocal fold polyp, 6 with papilloma, 7 with vocal nodule refractory to conservative management, 3 with anterior glottis web, 1 arytenoid granuloma and 1 with intubation granuloma (Table 1; Fig. 4).
Table 1.
Type of lesion and gender distribution in the study
| Lesions | No. of cases | Total | |
|---|---|---|---|
| Male | Female | ||
| Vocal polyps | 10 | 7 | 17 |
| Vocal nodule | 2 | 5 | 7 |
| Vocal fold cysts | 8 | 12 | 20 |
| Arytenoid granulomas | 1 | 0 | 1 |
| Vocal fold papilloma | 5 | 1 | 6 |
| Anterior glottis web | 2 | 1 | 3 |
| Intubation granuloma | 1 | 0 | 1 |
Fig. 4.
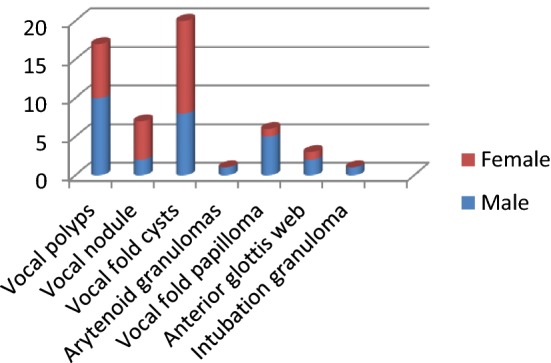
Vocal fold lesion and gender distribution in the study
In 31 cases lesion was found in anterior one-third of the vocal fold which sometimes need additional outer pressure on laryngeal framework during surgery for better visualisation. 15 cases had lesion over middle one-third and 9 cases had posterior one-third vocal fold lesion (Fig. 5).
Fig. 5.
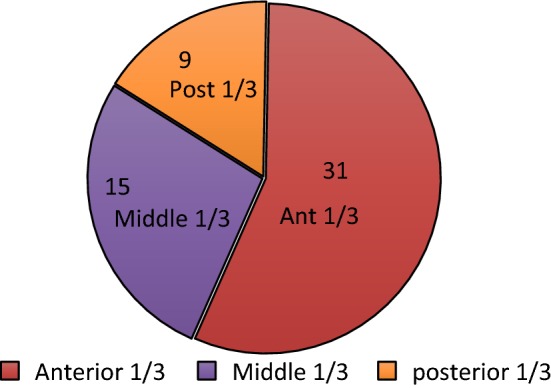
Site of lesions
Subjective Voice Assessment
Voice handicap index (VHI) is currently the most widely used parameter [9] to assess voice subjectively. It consists of 30 items which assess the impact of voice disorder on physical, functional and emotional aspects of the patient’s quality of life [9].
Pre operatively the mean voice handicap index (VHI) was 88.15 which declined to 26.5 3 month post operatively, showing a statistically significant (< 0.001) improvement.
Perpetual analysis [10] evaluates severity and grading of distinct voice qualities by a trained listener. The simplified scale, GRB [4] audios were recorded digitally and played for 3 observers: a speech language pathologist, an experienced ENT surgeon and the author grade of hoarseness, roughness and breathiness in 4 point scale of 0–3.
On rating voice of 55 patients in grade 0–3 for overall grade of dysphonia, roughness of voice and breathiness.
The mean Pre operatively GRB score was 6 which reduce significantly to 1.6 3 month post operatively, this improvement was statistically significant (< 0.001).
Objective Voice Assessment
Acoustic measures: using PRAAT program [11], the jitter/frequency perturbation threshold for pathological voice is > 1.04 and shimmer/amplitude perturbation threshold for pathological voice is 3.81 [12]. All 55 patients preoperatively had jitter and shimmer values above normal threshold. But in post-operative testing the number reduced to just two patient (3.63%) 3 month post operatively which was statistically significant (< 0.05). Harmonic to noise ratio was increased from preoperative mean value of 9.25 to post-operative mean value of 15.58 which was statistically significant (< 0.05).
Maximum phonation time (MPT) [13]: Maximum phonation time was a function of vital capacity of person and efficacy of vocal cord, Preoperative mean MPT was 8.58 which significantly increased to 12.46 3 month post-operative (< 0.05).
Video Stroboscopic Analysis
Glottic closure patterns and mucosal wave studies was done in all the patients, incomplete glottic closure was hallmark in all 55 patients pre operatively which was improved to complete closure in 98%. One patient had papilloma involving large surface of vocal fold and sub glottis which resulted scarring postoperatively.
Preoperatively mucosal wave focal absence and asymmetry was found in all patients. Amplitude was decreased due to bulk effect of lesion in 35 patients (63%). Postoperative stroboscopy reveals regular, symmetrical and normal amplitude mucosal wave in all cases except that one papilloma patient.
Figure 3 show still images of preoperative, 3 months postoperative and intraoperative images of vocal nodule, vocal polyp and vocal cyst cases respectively treated using cold knife endolaryngeal surgery.
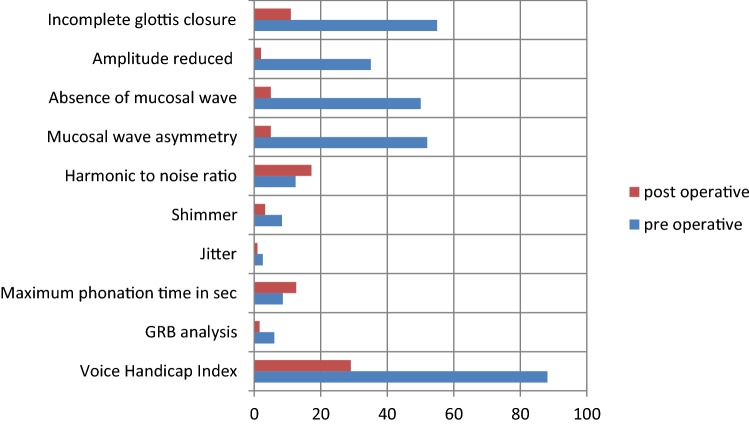
Table 2 showing summery of result and Fig. 6 graphical representation of improvement in various parameters.
Table 2.
Result
| Parameter | Before treatment | 3 month After treatment | p value | |
|---|---|---|---|---|
| Subjective analysis | Voice handicap index | 88.15 | 29.05 | < 0.001 |
| Perpetual analysis | GRB analysis | 6 | 1.6034 | < 0.001 |
| Aerodynamic analysis | Maximum phonation time (s) | 8.58 | 12.6245 | < 0.001 |
| Acoustic analysis | Jitter | 2.5444 | 0.9543 | < 0.001 |
| Shimmer | 8.2817 | 3.2039 | < 0.001 | |
| Harmonic to noise ratio | 12.4225 | 17.2032 | < 0.001 | |
| Mean fundamental frequency (Hz) | 176.1241 | 181.4916 | .432 | |
| Video laryngo-stroboscopic analysis | Mucosal wave asymmetry | 52 patients | 5 patients | < 0.001 |
| Absence of mucosal wave | 50 patients | 5 patients | < 0.001 | |
| Amplitude reduced | 35 patients | 2 patients | < 0.001 | |
| Incomplete glottis closure | 55 patients | 11 patients | < 0.001 |
Fig. 6.
graphical representation of improvement in paramenters after cold knife endolaryngeal surgery
Discussion
Mucosal movement over vocal folds is extremely important for the quality of voice [14]. Lesions over vocal fold restrict the mucosal movement which results in voice impairment. Benign vocal lesions such as vocal fold nodules, cyst and papilloma are among the commonest causes of hoarseness of voice which requires surgical intervention.
Surgery for removal of benign vocal fold lesion is also an injury to the vocal fold. Voice improvement after surgery depends on the mucosal and sub epithelial wound healing. In order to heal a primary wound, the margins of epithelium should be clean cut to initiate process of wound healing and to avoid scarring.
Use of cold instruments in micro laryngeal vocal fold surgery results in clean cut wound over mucosa of vocal cold and at the same time makes the margins of wound fresh whereas new techniques such as the lasers often cause thermal injury to the structure near wound margins which delay wound healing [15].
Among various benign vocal fold lesion excisions by micro-laryngeal surgery Virmani et al. [16] recruited 30 patients into their study, out of which 19 were males and 11 were females. The benign lesions observed were 16 vocal polyps, 7 vocal nodules, 5 vocal fold cyst, 1 vocal fold papilloma and 1 sulcus vocalis. Thomas et al. [17] in their study of 30 patients found 19 vocal polyp, 5 vocal nodule, 1 vocal polyp with cyst, 4 vocal cyst and 1 scar over vocal fold.
In our study of 55 patients, 20 cases had vocal fold cyst (most common) followed by 17 vocal polyps, 7 vocal nodules, 6 vocal fold papilloma, 3 anterior glottis web, 1 arytenoid granuloma and 1 intubation granuloma.
Subjective analysis by VHI (Voice Handicap Index) aimed at the self-assessment of the severity of the vocal alterations of patients with dysphonia [11]. A difference in total score of 18 or more between pre and postoperative scores or 8 or more for the subscales is considered significant.
Thomas et al. [17] in their study found pre operative mean 43.93 and 3 month post operative 30.70, which was not statistically significant but they found more than 8 reduction in the emotional scale.
In our study pre operatively, the mean voice handicap index (VHI) was 88.15 which declined to 26.5 3 month post operatively, showing a statistically significant (< 0.001) improvement.
Objective voice analysis by Maximum phonation time (MPT) was found to be statistically significant in our study with mean preoperative (MPT) 8.58 s and 3 month post-operative 12.6245 s.
Virmani et al. [16] had preoperative 9.43 ± 1.89 and 3 month post-operative 14.16 ± 1.7 which was also statistically significant.
Acoustic analysis by PRAAT (software) has been analysed by many clinicians. Stajner-Katusić [18] and Petrović-Lazic [8] showed significant improvement in jitter, shimmer and HNR (harmonic to noise ratio) after the surgery. Ragab et al. [8], in a randomized controlled trial on 50 patients with benign vocal fold lesions observed that both “jitter” and “shimmer” decreased significantly after surgery in both cold knife and radio surgical excision groups (p < 0.001), with no significant difference in HNR being noticed between the two groups (p > 0.05). Dejonckere et al. [4] observed that there was a statistically significant (p < 0.001) improvement in mean jitter, shimmer, and normalized noise energy (NNE) indices as measured from the preoperative to postoperative performance. In the studies by both Virmani et al. [16] and Thomas et al. [17] showed improvement in numerical values of jitter, shimmer and harmonic to noise ratio (HNR) but they were not statistically significant.
Our study has statistically significant reduction in jitter (pre op 2.5444 to post op 0.9543) and shimmer (pre op 8.2817 to post op 3.2039) 3 month post operatively with statistically significant increase in harmonic to noise ratio (pre op 12.4225 to post op 17.2032) (Table 2).
The improvement in the acoustic parameters can be explained on the basis of improved contact between vocal cords and better vibratory characteristic. Divakaran et al. [2] in 2016 analysed outcome analysis of Co2 laser and found mean shimmer 4.6 and 5 in males and females respectively which is above the threshold for PRAAT software by Teixeira et al. [12]. In our study this value is less than 3.81 in both genders which is considered as better improvement. Post-operative jitter and HNR was found below the threshold for pathological voice in both studies (Table 2).
Stroboscopy provides excellent real time mucosal wave movement endoscopically and helps in evaluating pattern of mucosal fold vibration. Ivey et al. [19] in their study of benign lesions of larynx observed that complete glottic closure results in greater vocal fold contact because of a regular edge, with generation of a greater subglottic pressure and better amplitude of cord vibration [11]. Thomas et al. found 29/30 patients had incomplete glottic closure pre operatively. In our study incomplete glottic closure was hallmark in all the 55 patients pre operatively which was improved to complete closure in 98%. One patient had papilloma involving large surface of vocal fold and sub glottis which resulted scarring postoperatively.
Surgical removal of a mass lesion can improve vibratory function. It will restore the vocal fold modulation of the air flow, airflow leakage is decreased, and glottal efficiency is increased. The symmetry of the vocal fold mass is restored, resulting in the stability and vibratory symmetry of each vocal fold. A smooth edge is created, facilitating improved vocal fold contact, and thereby allowing the normal generation of subglottic pressure and better amplitude of vocal fold vibrations [20].
Conclusion
Health care for low-income groups in India is all about affordability & availability without giving up on the quality. The lasers was determined to be a safe, accurate, and reliable method in removal of benign vocal fold lesions but the standard instruments offer excellent voice improvement due to very less post-operative scarring. Hence the cold knife video endo-laryngoscopic surgery still stands out to be a simple, cost effective yet efficient way in treating majority of benign vocal fold lesions causing hoarseness of voice.
Funding
This study was not funded by any source.
Compliance with Ethical Standards
Conflict of interest
The authors hereby disclose that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Human and Animal Rights
This article does not contain any studies with animals performed by any of the authors.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Upadhyay A, Zaidi AK, Mundra RK. A Comprehensive analysis of benign vocal fold lesions causing hoarseness of voice and our experience with cold knife endolaryngeal surgery in a tertiary healthcare centre. Indian J Otolaryngol Head Neck Surg. 2018;4:5–6. doi: 10.1007/s12070-018-1377-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Divakaran S, Alexander A, Vijayakumar S, Saxena SK. Voice outcome following carbon dioxide laser assisted microlaryngeal surgery. Indian J Otolaryngol Head Neck Surg. 2015;67:361–365. doi: 10.1007/s12070-015-0853-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Singhal P, Bhandari A, Chouhan M, Sharma MP, Sharma S. Benign tumors of the larynx: a clinical study of 50 cases. Indian J Otolaryngol Head Neck Surg. 2009;61(Suppl 1):26–30. doi: 10.1007/s12070-009-0013-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dejonckere PH, Bradley P, Clemente P, Cornut G, Crevier-Buchman L, Friedrich G, et al. A basic protocol for functional assessment of voice pathology, especially for investigating the efficacy of (phonosurgical) treatments and evaluating new assessment techniques. Eur Arch of Otorhinolaryngol. 2001;258(2):77–82. doi: 10.1007/s004050000299. [DOI] [PubMed] [Google Scholar]
- 5.Jahn A, Blitzer A. A short history of laryngoscopy. Logoped Phoniatr Vocol. 1996;21(3–4):181–185. doi: 10.3109/14015439609098887. [DOI] [PubMed] [Google Scholar]
- 6.Datta R, Sethi A, Singh S, Nilakantan A, Venkatesh MD. Translation and validation of the voice handicap index in Hindi. J Laryngol Voice. 2011;1(1):12. doi: 10.4103/2230-9748.76131. [DOI] [Google Scholar]
- 7.Hirano M, Hirano M. Surgical anatomy and physiology of the vocal folds. Chicago: Mosby-Year Book; 1993. pp. 125–158. [Google Scholar]
- 8.Petrovic-Lazic M, Jovanovic N, Kulic M, Babac S, Jurisic V. Acoustic and perceptual characteristics of the voice in patients with vocal polyps after surgery and voice therapy. J Voice. 2015;29(2):241–246. doi: 10.1016/j.jvoice.2014.07.009. [DOI] [PubMed] [Google Scholar]
- 9.Jacobson BH, Johnson A, Grywalski C, Silbergleit A, Jacobson G, Benninger MS, et al. The voice handicap index (VHI): development and validation. Am J Speech Lang Pathol/Am Speech Lang Hear Assoc. 1997;6(3):66–69. doi: 10.1044/1058-0360.0603.66. [DOI] [Google Scholar]
- 10.Karnell MP, Melton SD, Childes JM, Coleman TC, Dailey SA, Hoffman HT. Reliability of clinician-based (GRBAS and CAPE-V) and patient-based (V-RQOL and IPVI) documentation of voice disorders. J Voice. 2007;21(5):576–590. doi: 10.1016/j.jvoice.2006.05.001. [DOI] [PubMed] [Google Scholar]
- 11.Patel R, Awan S, Barkmeier-Kraemer J, Courey M, Deliyski D, Eadie T, et al. Recommended protocols for instrumental assessment of voice: American speech-language-hearing association expert panel to develop a protocol for instrumental assessment of vocal function. Am J Speech Lang Pathol. 2018;1(27):1–19. doi: 10.1044/2018_AJSLP-17-0009. [DOI] [PubMed] [Google Scholar]
- 12.Teixeira JP, Gonçalves A. Accuracy of jitter and shimmer measurements. Procedia Technol. 2014;1(16):1190–1199. doi: 10.1016/j.protcy.2014.10.134. [DOI] [Google Scholar]
- 13.Cesari U, Galli J, Ricciardiello F, Cavaliere M, Galli V. Dysphonia and laryngopharyngeal reflux. Acta Otorhinolaryngol Ital. 2004;24(1):13–19. [PubMed] [Google Scholar]
- 14.Rajput SD, Poriya MJ. Stroboscopy: an evolving tool for voice analysis in vocal cord pathologies. Int J Otorhinolaryngol Head Neck Surg. 2017;3(4):927–931. doi: 10.18203/issn.2454-5929.ijohns20173265. [DOI] [Google Scholar]
- 15.Zeitels SM. Laser versus cold instruments for microlaryngoscopic surgery. Laryngoscope. 1996;106:545–552. doi: 10.1097/00005537-199605000-00006. [DOI] [PubMed] [Google Scholar]
- 16.Virmani N, Sharma A, Dabholkar JP. Outcome analysis in patients with benign vocal fold lesions. Int J Phonosurg Laryngol. 2016;6:8–13. doi: 10.5005/jp-journals-10023-1111. [DOI] [Google Scholar]
- 17.Thomas G, Mathews SS, Chrysolyte SB, Rupa V. Outcome analysis of benign vocal cord lesions by videostroboscopy, acoustic analysis and voice handicap index. Indian J Otolaryngol Head Neck Surg. 2007;59(4):336–340. doi: 10.1007/s12070-007-0096-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stajner-Katusić S, Horga D, Zrinski KV. A longitudinal study of voice before and after phonosurgery for removal of a polyp. Clin Linguist Phon. 2008;22(10–11):857–863. doi: 10.1080/02699200802130813. [DOI] [PubMed] [Google Scholar]
- 19.Ivey CM, Woo P, Altman KW, Shapshay SM. Office pulsed dye laser treatment for benign laryngeal vascular polyps: a preliminary study. Ann Otol Rhinol Laryngol. 2008;117:353–358. doi: 10.1177/000348940811700505. [DOI] [PubMed] [Google Scholar]
- 20.Shi ZP, Wang HW. Objective analysis of voice after microlaryngoscopic surgery in patients with vocal polyps at different anatomical sites. J Med Sci (Taipei, Taiwan) 2007;27(6):265–269. [Google Scholar]