Abstract
Lymphoid papillary hyperplasia of the tonsils is a rare, benign lesion and is characterized by a papillomatous appearance with reactive follicular hyperplasia. Our case was unique because the lesion involved the unilateral and focal palatine tonsil, as the lesion usually involves the bilateral and entire palatine tonsils.
Keywords: Lymphoid papillary hyperplasia, Palatine tonsil, Squamous cell papilloma, Condyloma acuminatum
Introduction
Lymphoid papillary hyperplasia (LPH) of the tonsils is a rare, benign disorder that is frequently accompanied by dysphagia. LPH is characterized by a papillary, papillomatous, or multiple polypoid gross appearance with reactive follicular hyperplasia covered by a non-atypical squamous epithelium [1–9]. Bilateral involvement of the palatine tonsils seems to be more common for LPH [1]. The involved tonsil appeared to be entirely polypoid or papillary. Our case was rare because LPH involved the unilateral palatine tonsil and only a portion of the affected tonsil; these findings resulted in a clinical diagnosis of neoplasm.
Case Report
A 47-year-old Japanese female was referred to our hospital with a lesion of the left palatine tonsil. She had noticed the lesion six months prior to her referral. The lesion had enlarged slightly, and the patient had recently noticed dysphagia. Repeated tonsillitis was considered unlikely. The patient had a medical history of atopic dermatitis. No familial history relevant to the patient’s tonsillar lesion was found. Grossly, the upper portion of the left palatine tonsil showed a polypoid projection with a cobblestone appearance (Fig. 1). The other tonsillar regions were intact. Squamous cell papilloma of the left palatine tonsil was suspected. Biopsy of the tonsillar lesion showed neither squamous cell papilloma nor neoplasm. Left tonsillectomy was performed to relieve the patient’s symptoms and to confirm the absence of a neoplastic condition through a pathological evaluation.
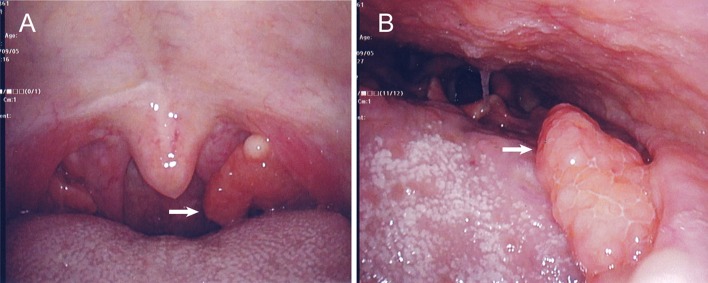
Fig. 1.
Gross images of lymphoid papillary hyperplasia of the left palatine tonsil. A polypoid lesion (arrowheads) is seen at the upper portion of the left tonsil (a) and demonstrates a cobblestone appearance when magnified by transnasal endoscopy (b). No polypoid lesion was seen in the right tonsil (a)
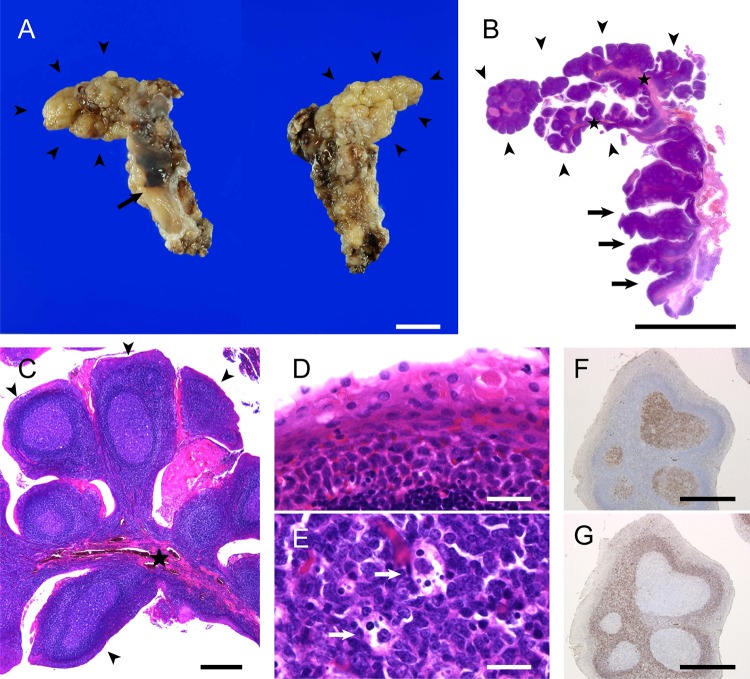
Grossly, the polypoid lesion with the cobblestone appearance projected from the upper portion of the palatine tonsil (Fig. 2a). Histologically, the polypoid lesion showed that many dome-shaped papillae with abundant lymphoid stroma projected from a few central stalks (Fig. 2b, c). The other portion of the resected tonsil had a smooth, not papillary, surface (Fig. 2a) with slightly dilated crypts (Fig. 2b, arrows). The overlying epithelium of the polypoid lesion lacked apparent atypia, koilocytosis, and hyperkeratosis (Fig. 2d) and was focally involved by lymphocytes, as was the background tonsillar epithelium. The lymphoid stroma of the polypoid lesion, which contained many reactive lymphoid follicles (Fig. 2c, e) immunohistochemically positive for CD10 (Fig. 2f) and negative for BCL2 (Fig. 2g), was also similar to that of the background non-polypoid tonsillar region. Bacterial colonies and neutrophilic infiltrate were not apparent in the papillary lesion or non-papillary area. No cells positive for human papilloma virus (HPV) antibody were immunohistochemically found. No Epstein-Barr virus (EBV)-encoded small RNA (EBER)1 was found via in situ hybridization (ISH). Therefore, LPH of the left palatine tonsil was diagnosed. The patient was disease-free 3 months following surgery.
Fig. 2.
Macro- and microscopic findings of lymphoid papillary hyperplasia of the left palatine tonsil. a A polypoid lesion (arrowheads) with a cobblestone appearance is projected from the upper portion of the left palatine tonsil (left, anterior view; right, posterior view). No polypoid lesion is noted in the lower portion (arrow). b–e Microscopic appearance of hematoxylin-and-eosin-stained sections of the tumor. A longitudinally cut section of the resected tonsil demonstrates that the lesion consists of dome-shaped papillae with lymphoid stroma (arrowheads) protruding from fibrous central stalks (stars) (b–c). High magnification of the stratified squamous epithelium of the papillae demonstrates parakeratosis and no apparent atypia (d). Germinal centers have tangible body macrophages (e, arrows). f, g Immunohistochemically, the germinal centers are positive for CD10 (f) and negative for BCL2 (g). Scale bars in a and b: 1 cm; scale bars in c, f, and g: 500 µm; and scale bars in d and e: 20 µm
Discussion
Enomoto et al. [1] described 40 cases of LPH of the palatine tonsil(s) in Japanese patients in 1980, but more recent reports of tonsillar LPH are rare in Japan. Outside of Japan, only 8 cases of LPH of the palatine (n = 6) or lingual (n = 2) tonsils have been reported [2–9]. The palatine tonsils appeared to be the most involved site of LPH in Waldeyer’s ring. The previously reported 48 cases of tonsillar LPH, which include those from the available literature [1–9], occurred in 28 females and 20 males [1–9] with an age ranging from 4 to 40 years (mean age: 17.8 years). The clinical diagnosis of tonsillar LPH includes both benign and malignant disorders; oral squamous cell papilloma is the main differential diagnosis, with the other differential diagnoses including papillomatosis, squamous cell carcinoma, and lymphoma [2, 6, 8]. The available follow-up data on cases of tonsillar LPH show no recurrence [3, 5, 6, 8].
Clinical diagnosis of tonsillar LPH is often difficult possibly due to its rarity. The clinical differential diagnoses of tonsillar LPH and squamous cell papilloma have not been discussed. In previously reported cases and our case, the papillary portions of the tonsillar LPH were dome-shaped and appeared not to be spiky or finger-like [1–9]. Hyperkeratosis might be a minor histological finding of tonsillar LPH. Thus, a white and spiky/finger-like papillary appearance may be indicative of squamous cell papilloma rather than tonsillar LPH. Condyloma acuminatum may not be clinically distinguishable from tonsillar LPH because both entities overlap with respect to exophytic dome-shaped papillae. We have added a previously undescribed gross feature of tonsillar LPH: a polypoid lesion with a cobblestone appearance. The crowded dome-shaped papillae seemed to induce the cobblestone gross appearance in our case.
The pathogenesis of tonsillar LPH has not been determined. A familial case of tonsillar LPH has been reported [1], but most cases appear to be sporadic. Based on the literature review of tonsillar LPH, the Japanese race may be related to its etiology, and the slight female predominance and limitation to the younger generation suggest to a hormonal effect on the etiology of tonsillar LPH. In fact, growth hormone therapy can induce tonsillar enlargement [10]. In addition, a reactive lymphoid proliferation response to external factors is suspected, and infective agents appear to be the main candidate for the external factors. Streptococcal infection was detected in the involved tonsil in one case [9]. Repeated tonsillitis was reported in three cases of tonsillar LPH [3, 5, 8], which suggests that tonsillar LPH may be a rare form of chronic tonsillitis. HPV infection in tonsillar LPH has not been reported. EBV might be related to the cause of tonsillar LPH [9]. Although an atopic constitution might be related to the occurrence of tonsillar LPH in our case, allergic status has not been reported in the previously published case reports [1–9]. We could not reveal the precise factors related to its pathogenesis.
In conclusion, clinicians and pathologists should consider tonsillar LPH, a rare condition, in the differential diagnoses of squamous cell papilloma and condyloma acuminatum and be aware that LPH can present as focal and unilateral involvement of the tonsil.
Acknowledgements
We thank Ms. Keiko Mizuno, Mr. Kazuhiko Ohara, Ms. Kaoru Yasuoka, Ms. Yukari Wada, Ms. Hiroyuki Tsutsui for preparing the histological and immunohistochemical specimens. We would like to thank Editage (www.editage.jp) for English language editing.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interests.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Written informed consent was obtained from the patient for publication of this case report and the use of accompanying images.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Enomoto T, Enomoto T, Matsui K, Tabata T. Papillary hypertrophy of the palatine tonsils. Ann Otol Rhinol Laryngol. 1980;89:132–134. doi: 10.1177/000348948008900208. [DOI] [PubMed] [Google Scholar]
- 2.Schantz A, Goodman M, Miller D. Papillary hyperplasia of the lingual tonsil. Report of a case. Arch Otolaryngol. 1972;95:272–273. doi: 10.1001/archotol.1972.00770080414016. [DOI] [PubMed] [Google Scholar]
- 3.Carrillo-Farga J, Abbud-Neme F, Deutsch E. Lymphoid papillary hyperplasia of the palatine tonsils. Am J Surg Pathol. 1983;7:579–582. doi: 10.1097/00000478-198309000-00008. [DOI] [PubMed] [Google Scholar]
- 4.Johnson CP, Burns J. Papillary hyperplasia of the lingual tonsil and sudden death in epilepsy. Am J Forensic Med Pathol. 1992;13:335–337. doi: 10.1097/00000433-199212000-00014. [DOI] [PubMed] [Google Scholar]
- 5.Dias EP, Alfaro SE, De Piro SC. Lymphoid papillary hyperplasia: report of a case. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;95:77–79. doi: 10.1067/moe.2003.48. [DOI] [PubMed] [Google Scholar]
- 6.Zhao M, Yu J, Li C. Lymphoid papillary hyperplasia of the palatine tonsil: a Chinese case report. Int J Clin Exp Pathol. 2013;6:1957–1960. [PMC free article] [PubMed] [Google Scholar]
- 7.Singh S, Sucheta RK, Sen R. Lymphoid papillary hyperplasia of tonsil: a rare case report. Int J Health Sci Res. 2015;5:444–446. [Google Scholar]
- 8.Altun D, Arslan HH, Umudum H, Okur G, Ersal Y. Lymphoid papillary hyperplasia of palatine tonsils: a rare pediatric case from Turkey. Int J Pediatr Otorhinolaryngol Extra. 2015;10:25–27. doi: 10.1016/j.pedex.2015.01.002. [DOI] [Google Scholar]
- 9.Borromini A, Marchesi A, Golinelli G, Salvadore M, Verzeletti M, Bonarrigo FA, Martinelli N, Todeschini M, Mirri G. Unusual papillary lymphoid hyperplasia of the palatine tonsil associated with Ebstein Barr virus infection in a child: a case report. J Pediatr Care. 2016;2:16. doi: 10.21767/2471-805X.100021. [DOI] [Google Scholar]
- 10.Berini J, Spica Russotto V, Castelnuovo P, Di Candia S, Gargantini L, Grugni G, Iughetti L, Nespoli L, Nosetti L, Padoan G, Pilotta A, Trifiro G, Chiumello G, A Salvatoni. Growth hormone therapy and respiratory disorders: long-term follow-up in PWS children. J Clin Endocrinol Metab. 2013;98:1516–1523. doi: 10.1210/jc.2013-1831. [DOI] [PubMed] [Google Scholar]