Abstract
Foreign body airway is a common cause of morbidity and mortality in children. Virtual bronchoscopy is a new investigative technique useful in locating non radiopaque FB missed on plain radiography. The aim of the study was to study the clinical profile of patients with suspected foreign body aspiration and to evaluate the changing trends in the diagnosis and quicker management of foreign body aspiration as a way of virtual bronchoscopy. This was a retrospective and prospective cross sectional study conducted in the Department of Otorhinolaryngology M.G.M.M.C. and M.Y. Hospital Indore for a period of 10 years. The medical records of patients with foreign body aspiration, from August 2006 to September 2016 were reviewed. Data was collected regarding their clinical presentation, examination and chest X-ray, virtual bronchoscopy, rigid bronchoscopy findings. Patients with suspected foreign body aspiration were subjected to virtual bronchoscopy and rigid bronchoscopy was performed. The techniques and methods to extract different types of foreign bodies has been elaborated in this study. In the 150 subjects, we observed mean age group of presentation was 2.1 years, male is to female ratio was 4.1, 70% of the cases came from the rural areas, 86% were vegetative foreign bodies, and remaining non vegetative were aspirated mostly during the winter season. Betel nut was the most common aspirated foreign body 0.63% had a positive history of foreign body aspiration, where as 37% had a negative history. Right main bronchus was the most common site of lodgement. Breathlessness and reduced air entry were the most common symptoms and signs. We also observed, that chest radiograph were normal in as many as 40% cases. Hence negative chest radiographs does not rule out FB. In 150 patients with foreign body aspiration, which was detected by virtual bronchoscopy, 148 patients were diagnosed to have foreign body on rigid bronchoscopy. This amounts to a positive predictive value of 97.3% which was similar to the positive predictive value of rigid bronchoscopy which was 99%. Virtual bronchoscopy is the only imaging modality which gives 99.9% reassurance about the presence or absence of a foreign body, because of its high sensitivity and specificity, hence proves to be a life saving tool.
Keywords: Foreign body aspiration, Virtual bronchoscopy, Life saving tool
Introduction
Aspiration of foreign bodies in children is a common problem around the world, which is a leading cause of accidental death among children younger than 4 years Christina et al. [1]. According to Reilly et al. [2] children less than 4 years are susceptible to FB injuries due to lack of molar teeth, oral exploration, and poor swallowing coordination. In India, children between the ages of 1 and 3 years are vulnerable for aspiration [2].
Foreign bodies in the tracheobronchial tree are mainly two types, either vegetative or non vegetative. Vegetative are dangerous as they swell up to 3–4 fold of their size Bhatt and Hegde [3]. Because of the high risk associated with an overlooked aspirated foreign body, rigid bronchoscopy is often performed for definitive diagnosis and treatment, even when there is little suspicion or a doubtful history. Rigid bronchoscopy remains the gold standard in managing these cases. But repeated removal attempts are likely to result in increased complications. Therefore, the availability of a non invasive, harmless technique to locate the foreign body pre operatively would greatly minimise morbidity and mortality [4].
Virtual bronchoscopy is a new investigative technique and is particularly useful in locating non radiopaque FB missed or remain undetected on plain radiography. Virtual bronchoscopy is providing a software solution for visualization and measurement of the human airway tree with data derived from multirow detector X-ray CT scans as the common data source [5]. This was a retrospective and prospective study with the aim of analysing the changing trends in the quicker diagnosis and, management of foreign body airway emergencies and methods to extract unusual foreign bodies.
Materials and Methods
This was a retrospective and prospective study, over a period of 10 years from 2006 to 2016, in the Department of Otorhinolaryngology, Head and Neck Surgery, Mahatma Gandhi Memorial Medical College Indore, Madhya Pradesh in central India. Study subjects included patients of the age group 1 month–15 years referred to the Emergency and Paediatric department with suspected foreign body aspiration and sudden onset respiratory distress. These suspected cases were subjected to X-ray and Virtual Bronchoscopy. In confirmed cases after taking high risk consent, rigid bronchoscopy was performed and foreign body was removed within 24 h of the virtual bronchoscopy. Ethical approval was obtained from the institutional ethics board.
Virtual Bronchoscopy
Virtual bronchoscopy is rapidly providing a software solution for visualization and measurement of the human airway tree with data derived from multirow detector X-ray CT scans as the data source. For single slice CT scanners, a slice thickness of 3–5 mm is preferred while pitch values up to 2 are usually acceptable for the volumetric depiction of pathology. Most published protocols prefer a pitch of 1 for virtual bronchoscopy using a single slice scanner. With the advent of multislice scanning, improved and gantry rotation times of 500 ms, VB imaging can now be routinely performed with 1 mm slice collimation [5].
In addition to being non invasive and not requiring sedation, an MDCT scan can reveal both a FB in tracheobronchial tree and secondary pulmonary changes that can be useful in making diagnosis. While VB is also useful in evaluating the tortuous structure, detecting anatomic variations and visualizing the bronchial system distal to obstruction [5].
Rigid Bronchoscopy
Bronchoscopy was performed after induction of general anaesthesia after adequate preoxygenation, intravenous anesthetic drugs and skeletal muscle relaxants were used, using paediatric Karl Storz bronchoscope, which was introduced with the help of Macintosh laryngoscope, under direct vision and was advanced past the vocal folds. The foreign body was then visualized on the affected side and extracted using grasping forceps. A check bronchoscopy was performed to identify any retained fragments, any secretions were removed by suction. Post operatively, the children were kept under observation for complications such as subglottic oedema.
Results
Demography
In our study of 150 cases, we found that 72% of the cases belonged to the rural areas. Male predominance was seen with the ratio of 4:1. 63% of the patients came from lower socio economic strata. 62% of the cases belonged to the age group from 1 to 5 years. Vegetable foreign bodies formed the major chunk with the most common were the betel nut (27%) and groundnut (24%), non vegetable foreign bodies consisted 14% of the total number of cases. Most of the cases were reported during the winter season that is 30% during October to November, 19% during January and February (Fig. 1).
Fig. 1.
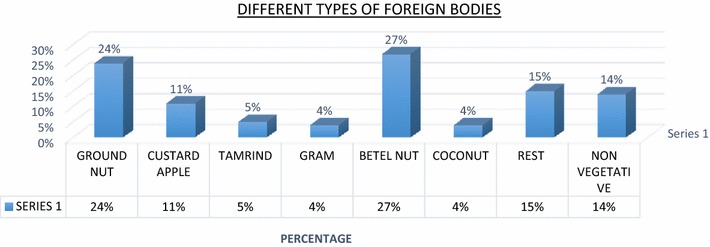
Graph showing different types of foreign bodies
Clinical Symptoms
In the present series 63% cases, showed definite history of FB inhalation whereas 37% cases had no definite history of FB Inhalation. 32% of the patients turned to hospital within 24 h after inhalation of FB, while 20% of the patients came after five or more days. Only 4% patients came within 6 h. 47% of the patients had oxygen saturation between 80 and 90%, while only 15% had saturation below 80%. Breathlessness was the most common symptom (95%), it included varying degree from mild, moderate to severe seen in majority of the cases, followed by cough (65%). The most common clinical sign was decreased air entry in about 91% of the patients, followed by chest retractions 57%, rhonchi 36%, stridor 32% (Fig. 2).
Fig. 2.
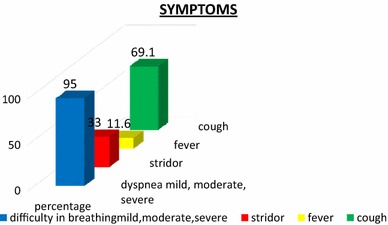
Graph showing symptoms
Investigative Findings
Chest X-ray findings showed that 44% of the cases had obstructive emphysematous changes suggestive of a foreign body, whereas 40% of the cases had a normal chest X-ray, hence a negative chest radiograph doesn’t rule out a foreign body. Virtual bronchoscopy had a positive predictive value of 97.3% where as chest X-ray had a positive predictive value of only 58%. Chest xrays had a sensitivity of 60% and specificity of 66% in comparison with virtual bronchoscopy which had sensitivity of 98% and specificity of 50. Rigid bronchoscopy which is the gold standard in the diagnosis of foreign body airway, had a positive predictive value of 99.1%, sensitivity of 98% and specificity of 50%, which was in close similar to the virtual bronchoscopic findings. Only in one case where intraluminal filling defect was seen in the right main bronchus but on rigid bronchoscopy mucus plug was found (Figs. 3, 4, 5).
Fig. 3.
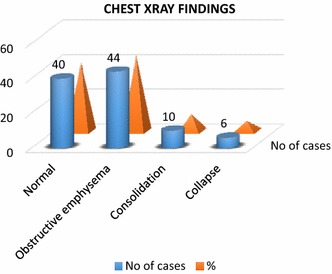
Graph showing chest xray findings
Fig. 4.
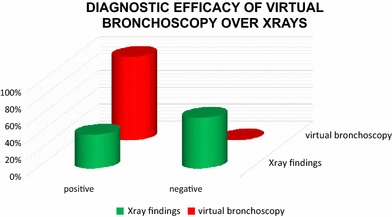
Graph showing the diagnostic efficacy of virtual bronchoscopy in comparison with chest X-ray
Fig. 5.
A picture depicting the efficacy of Vb in diagnosing FBA. a Two years female presented with respiratory distress, b CXR was normal. Vb showed FB in the right main bronchus. RB was done Fb corn seed extracted
Therapeutic Findings
Majority of FB in airway i.e. 148 cases were removed by rigid bronchoscopy and only 2 case needed rigid bronchoscopy and tracheostomy (plastic pen cap and tamarind). Majority of FB in air passage were in right main bronchus 57%, followed by larynx and trachea (22%) and left main bronchus (21%). We found that in long standing cases, foreign bodies were found in the left main bronchus. Vegetative foreign bodies non friable were 76 cases where peanut grasping forceps was used. Vegetative friable foreign bodies were 51 cases, crocodile forceps was used. Non vegetative metallic, and non metallic foreign bodies were removed by peanut grasping forceps 17 cases, sharp foreign bodies were removed using inward rotation method was used. Only two patients patient required tracheostomy for removal of foreign body as the foreign body was difficult to pass through the glottis (Fig. 6).
Fig. 6.
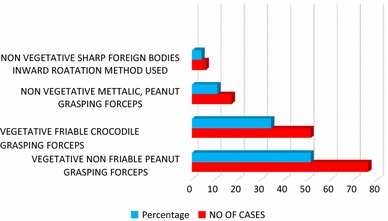
Methods of extraction of foreign bodies
Discussion
In our study of 150 cases, incidence of FB was quite higher in low socio economic status group (63%) and the rural areas 73%. This directly reflected the surrounding and personal care of the young children by parents. Social education and personal habit also determines the incidence rate of FB in airways. Male predominance was seen with a ratio of 4:1. In the review by Shlizerman et al. [6], two-thirds of the 136 FB patients were male and two-thirds were younger than 2 years of age, this was similar with our study.
Food items, especially peanuts, are the most common items aspirated in infants, whereas older children are more likely to aspirate non-food items such as pen caps, pins, and paper clips. Most of the cases were vegetative foreign bodies that was 86% in comparison to the non vegetative which were 14%. Most of the aspirations were seen in the age group between 1 and 5 years owing to the development of pincer grasp, following which they develop a habit of picking up random objects and putting them in their mouth, leading to increased risk of aspiration [4].
According to Williams et al. [7] peanuts are relatively cheap and freely available during the festive season in India, which is the reason for them being the most common aspirated FB in the series. This study has reported that most 81%, of the aspirated foreign bodies are organic materials, including nuts (especially peanuts) and seeds (mainly sunflower and watermelon) which was similar to our study.
Most common among the vegetable foreign body was betel nut and groundnut, this was due to the betel quid chewing habit of the elders in the vicinity of the children. Most of the aspirations occurred during the winter season that is October to January owing to the festive season in India and the abundance of groundnut and custard apple during this season.
32% of the patients turned to hospital within 24 h after inhalation of FB, while 20% of the patients came after five or more days. Only 4% patients came within 6 h. It is dependent upon the severity of symptoms, age of patients, socio economic status, education status, awareness of family, transportation system and treating doctor. Majority of the FB were in air passage were in right main bronchus 57%. This is because right main bronchus is shorter, wider and more in line with trachea.
Majority of the patients had breathlessness as the most common symptom varying from mild, moderate, severe. Choking after aspiration was invariably a sign of aspiration of a foreign body. Cough was the second most symptom. When FB was in upper airway (subglottis, trachea) child presented with severe respiratory distress, as subglottis is narrowest portion of airway in the pediatric age group. Shubha et al. [8] observed in their retrospective study that the clinical triad of cough, respiratory distress and stridor was highly predictive of foreign body aspiration. In our study, the most common clinical sign was decreased air entry of the lungs in about 91% of the patients, followed by Chest Retractions, Rhonchi, Stridor.
We observed that chest radiograph was normal in as many as 40% cases 0.44% of the cases had obstructive emphysema, consolidation in 10% and collapse in 6% of the cases. Hence negative chest radiographs does not rule out FB, rather each suspected case of foreign body aspiration should be considered for virtual bronchoscopy whenever possible and should be subjected to diagnostic and therapeutic bronchoscopy accordingly.
Virtual bronchoscopy had a positive predictive value of 97.3% in detecting foreign body which was similar to the gold standard rigid bronchoscopy which it self had a positive predictive value of 99.1%. Chest xrays had a sensitivity of 60% and specificity of 66% in comparison with virtual bronchoscopy which had sensitivity of 98% and specificity of 50%. This hence proves that virtual bronchoscopy is a boon in detecting foreign bodies pre operatively before rigid bronchoscopy. Silver men et al. in a recent study comparing VB and conventional bronchoscopy, the sensitivity and specificity of VB were 96 and 58%, respectively. Hasan et al. [9] study showed that MDCT had a negative predictive value of 100%, whereas its positive predictive value was 75%. Behera et al. [10] also had similar results were virtual bronchoscopy had a positive predictive value of 98%, which was close similar to the gold standard of rigid bronchoscopy a ppv of 99%, one of the case had a mucous plug, which was positive on virtual bronchoscopy.
It is useful as it stimulates the endoscopists view of the airway using 3D reconstruction it takes advantage of the natural contrast between the airway and the surrounding tissues to detect the exact location, size and shape of the foreign body. Unlike the flexible bronchoscope virtual bronchoscopy can provide images beyond the level of obstruction such as a stenosed part. This also helps the surgeon plan the procedure of rigid bronchoscopy as he is sure of the position, size nature of the foreign body, type of forceps also can be decided with the help of virtual bronchoscopy [10]. A negative virtual bronchoscopy can prevent a patient from unnecessary hazards due to rigid bronchoscopy and general anesthesia because it is the only imaging modality which gives 99.9% reassurance about the presence or absence of a foreign body, as it can study the tracheobronchial tree as far as the segmental bronchi and sometimes also the sub segmental bronchi and the bronchi below a closed obstruction [10].
According to Bhat et al. [3], many poorer patients in developing countries are unaware of the symptoms of foreign body aspiration and do not give a correct history hence many cases present with late symptoms related to pneumonia, bronchiectasis, which are unresolved due to medical treatment, these patients when subjected to virtual bronchoscopy revealed a hidden foreign body which was removed the patient improved symptomatically. Hence in cases of a long standing foreign body missed on chest radiography which present with non resolving pneumonia, bronchiectasis virtual bronchoscopy helps in detecting the foreign body. In this study we here by see the change in the trend of diagnosis over a decade from chest X-ray to virtual bronchoscopy which gives an accurate non invasive picture of the foreign body pre operatively, and helps in the accurate and quicker diagnosis and management, hence can be considered a life saving tool.
Management and Post Operative Period
In this study out of 150 cases 148 cases were managed by rigid bronchoscopy as a therapeutic technique and two cases that is extraction of foreign body tamarind seed required tracheostomy to secure the airway and as an anchor to prevent the foreign body from slipping back into the main bronchus. According to the types of foreign bodies different methods and forceps were used to extract the foreign body. Vegetative foreign bodies non friable were 76 cases such as betel nut, chikku seed, where peanut grasping forceps was used. Vegetative friable foreign bodies such as groundnut, corn seed, gram etc. were 51 cases, crocodile grasping forceps was used. Non vegetative metallic, and non metallic hollow foreign bodies were removed by peanut grasping forceps 17 cases, sharp foreign bodies were removed using inward rotation method.
According to Shepherd [11] that removal of foreign bodies with a flexible bronchoscope is successful in 60–90% of cases, but it can be time-consuming and result in a second procedure with a rigid bronchoscope. Because multiple removal attempts are often required with flexible bronchoscopy, a foreign body is more likely to be pushed distally. A foreign body may also drop into an unaffected area of the lung as a result of inadequate grasping with flexible instruments. Rigid bronchoscopy is better suited for large aspirated items because of the size of the working channel and the ability to use larger instruments, such as optical grasping forceps.
Compliance with Ethical Standards
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical Approval
This study has been Granted ethical clearance.
Informed Consent
This study has been performed after taking high risk consent for performing rigid bronchoscopy from the patients parents also permission to use the data for research work.
Contributor Information
Aishwarya Ullal, Email: casiopia_17@yahoo.co.in.
Sanjeev Mishra, Email: sanjeev1818@gmail.com.
References
- 1.Fdkowski CW, Zheng H, Firth PG. The anaesthetic considerations of tracheobronchial foreign bodies in children: a literature review of 12979 cases. Anesth Analg. 2010;111(4):1016–1025. doi: 10.1213/ANE.0b013e3181ef3e9c. [DOI] [PubMed] [Google Scholar]
- 2.Reilly JS, Cook SP, Stool D, et al. Prevention and management of aerodigestive foreign body injuries in childhood. Pediatr Clin N Am. 1996;43:1403–1411. doi: 10.1016/S0031-3955(05)70525-3. [DOI] [PubMed] [Google Scholar]
- 3.Bhatt KV, Hegde JS. Evaluation of CT virtual bronchoscopy in paediatric tracheo-bronchial foreign body aspiration. J Laryngol Otol. 2010;124:875–879. doi: 10.1017/S0022215110000769. [DOI] [PubMed] [Google Scholar]
- 4.Seghal A, Singh V, Chandra J, Mathur N. Foreign Body Aspiration. Indian J Pediatr. 2002;39:1006–1010. [PubMed] [Google Scholar]
- 5.Cuk V, Belina S, Fure R, Buković D, Lovrić D, Seso I. Virtual bronchoscopy and 3D spiral CT reconstructions in the management of patient with bronchial cancer–our experience with Syngo 3D postprocessing software. Coll Antropol. 2007;31(1):315–320. [PubMed] [Google Scholar]
- 6.Shlizerman L, Ashkenazi D, Mazzawi S, et al. Foreign body aspiration in children: ten-years experience at the Ha’Emek Medical Center. Harefuah. 2006;145:569–571. [PubMed] [Google Scholar]
- 7.Williams A, George C, Atul PS, Sam S, Shukla S. An audit of morbidity and mortality associated with foreign body aspiration in children from a tertiary level hospital in Northern India. Afr J Paediatr Surg. 2014;11(4):287–292. doi: 10.4103/0189-6725.143129. [DOI] [PubMed] [Google Scholar]
- 8.Shubha AM, Das K. Tracheobronchial foreign bodies in infants. Int J Pediatr Otorhinolaryngol. 2009;73(10):1385–1389. doi: 10.1016/j.ijporl.2009.06.021. [DOI] [PubMed] [Google Scholar]
- 9.Hassan MA, Youssef TA, El-Gharib M. Role of virtual bronchoscopy in foreign body inhalation in children. Egypt J Otorhinolaryngol. 2009;29(4):249–253. [Google Scholar]
- 10.Behera G, Tripathy N, Maru YK, Mundra RK, Gupta Y, Lodha M. Role of virtual bronchoscopy in children with a vegetable foreign body in the tracheobronchial tree. J Laryngol Otol. 2014;128:1078–1084. doi: 10.1017/S0022215114002837. [DOI] [PubMed] [Google Scholar]
- 11.Shepherd RW, Beamis JF. Understanding the basics of rigid bronchoscopy. J Respir Dis. 2006;27(3):100–113. [Google Scholar]


