Abstract
Yoga is an ancient Indian practice of mental and physical exercises (syn: asanas), postures (syn: mudras), movements and breathing techniques which sustain healthy living of the body and the mind. It incorporates various exercises of breathing, oropharyngeal structures and facial expressions, the physiology and effect of which are comparable to international physiotherapy recommendations in treatment of obstructive sleep apnea (OSA) i.e. to preserve upper airway patency by maintaining airway dilator muscle tone. Preliminary results show that yoga can be an effective and constructive alternative to physiotherapy for sleep apnea and snoring patients. To compare the physiotherapy recommendations in snoring patients with various yoga exercises postures. To determine the efficacy of yoga in treatment of sleep apnea. To formulate a standardized yoga protocol for universal usage in sleep apnea. We studied the available literature on physiotherapy recommendations for OSA and yoga asanas involving the nasal, oropharynx and facial structures and perceived a noteworthy similarity in physiological basis of both. A set of these yogasanas were put together and patients presenting with snoring and diagnosed with mild to moderate sleep apnea were presented and encouraged to perform the standardized set of yoga exercises for a period of 3 months. A total of 23 patients were recommended yoga protocols as initial form of treatment in snoring and mild to moderate sleep apnea. Clinical and statistically significant improvement gauzed by recommended score chart was discerned in majority of subjects. The results were comparable to the efficacy of existing physiotherapy regimen published in international literature. The benefits of yoga in sleep disorders go beyond the scope of measured outcomes. Standardizing the protocols for yoga in treatment for snoring and sleep apnea is the need of the hour. Further studies on efficacy of yoga need to be performed to understand its full realm of potential.
Keywords: Snoring, Obstructive sleep apnea (OSA), Yoga, Yogasana, Physiotherapy, Oropharyngeal muscle
Introduction
Obstructive sleep apnea syndrome (OSAS) is a significant public health problem characterized by repetitive episodes of upper airway occlusion during sleep associated with sleep fragmentation, daytime hyper somnolence, and increased cardiovascular risk [1, 2]. Recurrent apnea, hypoxia, and hypercapnia, as well as sleep fragmentation, together with increased negative intrathoracic pressure—which results from increased inspiratory muscle work in order to reopen the collapsed airways—result in impaired central nervous system, cardiovascular system, and metabolic function [3, 4]. Excessive daytime sleepiness, nocturia, morning headache, decreased libido, attention deficit, impaired concentration, neurocognitive impairment, irritability, and depression are common in patients with OSA and greatly reduce their work efficiency and quality of life [5]. Snoring, though not specific for OSA patients, is regularly seen in these patients. The etiology of OSA and snoring is multifactorial, and include anatomical changes, neuromuscular factors, and genetic predisposition. Upper airway dilator muscles are crucial to the maintenance of pharyngeal patency [6] as they oppose the negative endopharyngeal pressure caused by the diaphragmatic contraction to maintain the caliber of the pharyngeal lumen and prevent OSA. Pharyngeal lumen regulators, such as the genioglossus and digastric muscles and several upper airway dilator muscles, such as the sternohyoid and omohyoid muscles play a vital role to prevent airway collapse during sleep [7]. The modus operandi of physiotherapy in OSA is to improve the tone of these muscles by regular and systemic oropharyngeal exercises. These exercises thus form a vital treatment option for snoring and OSA in addition to continuous positive airway pressure (CPAP), oral appliances and airway surgical procedures.
Yoga is an ancient Indian exercise regimen consisting of a range of exercises (syn: asanas) and postures (syn: mudras) which sustain healthy living of the entire body and the mind. Pranayama, probably the best known yogasana has been known since centuries to benefit in nasal obstructions, sinusitis and other nasal airway pathologies. Yoga also incorporates a range of asanas and postures that affect the musculature and structures involved in pathophysiology of snoring and OSA. Regular practice of yogasana may thus, contribute to improve the symptomatology of these pathological conditions. While the role of exercise, oropharyngeal maneuvers and weight loss has been extensively studied, the exploration of benefits of yoga in snoring and OSA is conspicuous by its absence.
In this study, we endeavor to evaluate the utility of yoga in snoring and OSA, compare the efficacy with oropharyngeal physiotherapy recommendations in international literature and propose standardized protocols for yoga for universal usage.
Materials and Method
Patients with history of snoring and mild to moderate degree of obstructive sleep apnea were included in this study. The diagnosis of degree of OSA was made using detailed history taking, clinical examinations, anthropometric findings, standardized questionnaires and polysomnography (PSG) study. The questionnaire utilized in this study were Berlin questionnaire [8], Epsworth sleepiness score [9] and Pittsburgh sleep quality questionnaire [10]. Berlin questionnaire consists of three categories related to the risk of having sleep apnea and patients are classified into high low risk based on their responses to the individual items and their overall scores in the symptom categories. It specifically measures snoring frequency, ranging from 0 (never) to 4 (every day) and intensity 1 (similar to breathing) to 3 (very loud). Epsworth sleepiness score aims to objectively quantify daytime sleepiness by evaluating the propensity to sleep from no (0) to intense (3) in eight different day to day situations. Pittsburgh sleep quality questionnaire appraises sleep quality through seven sleep components on a scale of 0–3. Polysomnography is a multi parametric test which is applied in OSA cases to assess number of apnea events, associated desaturation, sleep stage and microarousals. PSG includes electroencephalogram, electrocardiogram, oximetry, and recordings of the respiratory rate, respiratory sounds, thoracoabdominal movements and movements of the subject. The utilization of PSG IN all patients was restrained in our study due to factors of accessibility and affordability.
The exclusion criteria were history of buccopharyngeal surgery, major morphologic abnormality (retrognathia, Pierre-Robin syndrome), body mass index (BMI) 40 kg/m2 or greater, use of hypnotic medications, presence of severe systemic disorders and history of drug or alcohol addiction.
The patients were introduced to a set of yoga exercises (yogasana) perceived to be of benefit in snoring and OSA patients. These encompassed nasal breathing exercises, oropharyngeal exercises, and facial musculature exercises along with traditional yoga exercises. The following exercise protocol was adopted and individually tailored to suit the patients requirement as per clinical examination.
Bhramari Pranayama (Humming Bee Pranayama)
In this asana ears are closed with thumb while placing index finger on forehead and other three fingers on the base of nose softly touching the eyes. One is supposed to inhale deeply and holding the breath for some time and then exhaling forcibly through nostrils with humming/buzzing sound like a bee. This inhalation/exhalation should be from lungs with minimal abdominal movements. It is started by doing it 10–12 times and gradually increased to 25–30 times.
Ujjayi Pranayama (Victory Breath Pranayama)
In Ujjayi pranayama eyes are closed and lips are sealed. Deep breaths are taken through nose. Contracting muscles in the back of throat one inhales and exhales while keeping mouth closed. Breaths will make a sound like the waves of an ocean. It is repeated 10 times.
Kapalbhati (Shining Skull Pranayama)
While performing Kapalbhati spine is kept erect with palms on knees facing downwards. As one exhales through nose stomach is pulled in towards spine. As one loosens his stomach he automatically breaths in. Stomach should be quickly contracted again and one should exhale. Stomach muscles should be doing the work of pushing out and pulling in air. Repeat at least 50 times.
Simhasana (Roaring Lion Pose)
In this pose one is supposed to kneel down and lean backwards so that hips are resting on heels. Palms are placed faced up in the between knees with fingers spread open. While keeping your head tilted back one should slightly lean forward while taking large, slow breath through nose. Breath is held for few seconds, then mouth is opened and tongue is stuck out, before exhaling forcefully while making a loud AHHH, which should sound like a roaring noise (the louder the better). These breaths are repeated for at least a few minutes.
Bhujangasana (Cobra Pose)
In this pose one is supposed to kneel down and lean backwards so that hips are resting on heels. Palms are placed faced up in the between knees with fingers spread open. While keeping your head tilted back one should slightly lean forward while taking large, slow breath through nose. Breath is held for few seconds, then mouth is opened and tongue is stuck out, before exhaling forcefully while making a loud AHHH, which should sound like a roaring noise (the louder the better). These breaths are repeated for at least a few minutes.
Naukasana (Boat Pose)
Naukasana is done by lying on back with feet together and arms beside body. After taking a deep breath, while exhaling chest and feet are lifted off ground, stretching arms towards feet. As one feels tension in the navel area as abdominal muscles contract, one continues deep breathing and easily while maintaining the pose. While exhaling one comes back to the ground slowly and relaxes.
Dhanurasana (Bow Pose)
In this asana person is made to lie down on his stomach with feet hip-width apart and arms by side of body. With knees folded, person is supposed to take his hands backwards and hold his ankles. While breathing in, chest is lifted off the ground and legs are pulled up and back. Person should look straight ahead and keep the pose stable while paying attention to his breathing. With Body curved and taut as a bow. Deep breaths are taken. After 15–20 s, while exhaling legs and chest are brought to ground.
Nadi Shodhana (Alternative nostril breathing)
In nadi shodhana left hand is placed on left knee with palm facing the sky or pressing the thumb and index finger together. Now, place your number one and number two fingers of the right hand between your eyebrows. Place your ring and little finger on you left nostril and your thumb on the right. Take a deep breath in and out. When exhaling, close the right nostril with your thumb and breathe through your left nostril. Breathe in through your left nostril. Once you have filled your lungs, switch to close your left nostril and exhale through your right nostril. Inhale through your right nostril. Complete 10 rounds of this move in conjunction with your yoga routine.
Kechari mudra (The Tongue Lock)
This is an advanced practice and requires prolonged efforts. Beginners are expected to perform only the initial stages. The tongue should be rolled up to touch the upper palate. Initially it may be able to touch only the hard palate. With practice, it can go further behind to touch the soft palate. Later it can touch the uvula at the back of the throat. With practice, the tongue can go beyond the uvula and enters the nasal cavity to stimulate certain points inside the cavity. This may take months or years of practice,
Chanting of OM
After closing eyes and controlling breathing for few seconds, one should begin chanting the word OM over and over for few minutes. The word should be said in two separate, first with a very deep OOOOOO that comes from as far within as possible, then a lighter MMMM. Om sound is a form of energy made up of vibrations which are felt during the chant.
After fulfillment of the inclusion criteria, the patients were given a comprehensive demonstration by a skilled yoga instructor. Various postures to perform the asanas were taught and instruction related to timing, duration and compatibility with supplementary exercises, other treatments and daily routine were discussed individually. Required consent was obtained after explaining the objective of entire exercise. Patients who failed to return for three consecutive weeks or failed to comply with the exercises at home (performing < 75% of the exercises) were excluded from the study.
The patients were asked to observe the changes induced by the intervention after a period of 3 months and compare it with their physical and mental well being prior to the induction of yoga. The patients thus acted as their own control. The same questionnaires and PSG, if viable, that were utilized in initial assessment were repeated and compared. Both subjective and objective assessment therefore were made and interpreted.
Results
A total of 37 patients presenting to the Department of Otorhinolaryngology outpatient wing fulfilled the inclusion criteria for our study. These patients were diagnosed cases of mild to moderate OSA or complained of snoring. Eight patients were excluded due to low adherence to our yoga protocol as defined in the methodology section. Hence 29 patients were incorporated in our final analysis.
There was a preponderance of middle age, overweight or obese male patients in our series. The demographic characteristics and anthropological measurements are depicted in Fig. 1.
Fig. 1.
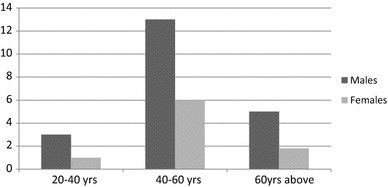
Age and sex distribution
The average body mass index before the start of therapy was 28.86, which came down to 25.93 after 3 months as depicted in Fig. 2 with a P value of 0.0014. The individual BMI variations and the t test assuming equal and unequal variances have been shown in Fig. 2 and Table 1
Fig. 2.
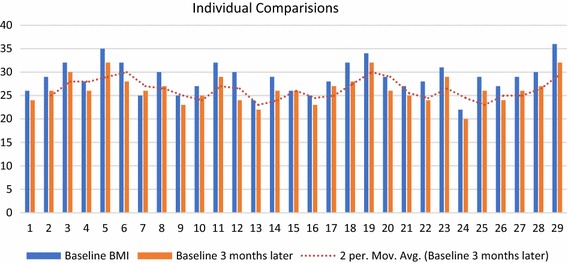
Body mass index
Table 1.
Body mass index
| Variable 1 | Variable 2 | |
|---|---|---|
| t test: two-sample assuming unequal variances | ||
| Mean | 28.86206897 | 25.93103 |
| Variance | 10.98029557 | 7.923645 |
| Observations | 29 | 29 |
| Hypothesized mean difference | 0 | |
| df | 56 | |
| t Stat | 3.63031033 | |
| P (T ≤ t) one-tail | 0.001468 | |
| t critical one-tail | 1.673033965 | |
| P (T ≤ t) two-tail | 0.000621878 | |
| t critical two-tail | 2.004044783 | |
| t test: two-sample assuming equal variances | ||
| Mean | 28.86206897 | 25.93103 |
| Variance | 10.98029557 | 7.923645 |
| Observations | 29 | 29 |
| Pooled variance | 9.451970443 | |
| Hypothesized mean difference | 0 | |
| df | 56 | |
| t Stat | 3.63031033 | |
| P (T ≤ t) one-tail | 0.000307149 | |
| t critical one-tail | 1.672522303 | |
| P (T ≤ t) two-tail | 0.000614298 | |
| t critical two-tail | 2.003240719 | |
The average neck and abdominal circumference were 37.5 and 97 cm. 24% of the patients had a positive history of tobacco consumption in some form and 27.5% had history of regular alcohol intake. Epsworth sleepiness score, snoring intensity, snoring frequency and Pittsburgh sleep quality score were also charted out. Average Epsworth sleepiness score were found out to be 14.2 before the start of therapy which later reduced to 7.34 after 3 months of therapy as depicted in Fig. 3 and Table 2 with a P value of 0.00018.
Fig. 3.
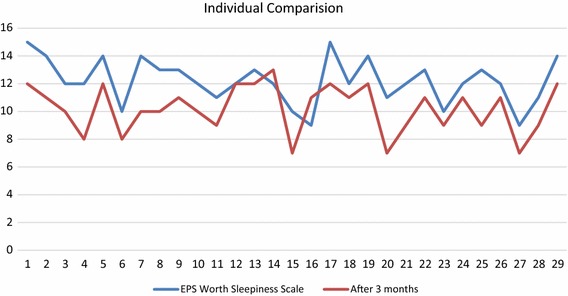
Epsworth sleepiness score
Table 2.
Epsworth score
| Variable 1 | Variable 2 | |
|---|---|---|
| t test: two-sample assuming unequal variances | ||
| Mean | 14.20689655 | 7.344827586 |
| Variance | 9.74137931 | 10.16256158 |
| Observations | 29 | 29 |
| Hypothesized mean difference | 0 | |
| df | 56 | |
| t Stat | 8.282940485 | |
| P (T ≤ t) one-tail | 0.000182 | |
| t critical one-tail | 1.673033965 | |
| P (T ≤ t) two-tail | 2.65242E−11 | |
| t critical two-tail | 2.003240719 | |
| Test: two-sample assuming equal variances | ||
| Mean | 14.20689655 | 7.344827586 |
| Variance | 9.74137931 | 10.16256158 |
| Observations | 29 | 29 |
| Pooled variance | 9.951970443 | |
| Hypothesized mean difference | 0 | |
| df | 56 | |
| t Stat | 8.282940485 | |
| P (T ≤ t) one-tail | 1.32621E−11 | |
| t critical one-tail | 1.672522303 | |
| P (T ≤ t) two-tail | 2.65242E−11 | |
| t critical two-tail | 2.003240719 | |
The BMI and neck circumference indices showed mild improvement after a 3 months period. Abdominal circumference of the group, however, did not show any significant change over the study period. In contrast, patients introduced to yoga exercises had a significant decrease (P < 0.05) snoring frequency 0.45, snoring intensity 0.39, sleep quality score. PSG measurements, when performed in few opting patients also demonstrated a reduction in OSA severity by diminution of apnea–hypopnea index 3.3. Yoga exercises thus appreciably lessen OSA severity and snoring symptoms in our study and show potential as a promising treatment options for these conditions.
Discussion
Obstructive sleep apnea (OSA) is a public health problem with a variable and underestimated prevalence. The first recorded knowledge about sleep disordered breathing goes back to prehistoric times. However, the first physicians to recognize the syndrome in 1956 suggested Pickwick syndrome as nomenclature [11], to honor the character described by Charles Dickens in Posthumous Papers of Pickwick Club. Our understanding and perceptions about OSA has grown considerably since that time, but there is still a lot left to be done.
OSA is a therapeutic challenge due to its multifactorial genesis that includes anatomical and physiological factors. Snoring, though not specific for OSA patients, is regularly seen in these patients. The mechanism is attributed to a complete or partial obstruction of the upper airway (UA) during sleep which can occur at the level of nose, nasopharynx, oral cavity, oropharynx, larynx and laryngopharynx or may have multiple sites in the same patient. Obesity, thick neck, use of alcohol, sedatives, sedentary life style and anxiety are important contributing factors. Repetitive episodes of upper airway occlusion during sleep results in recurrent apnea, hypoxia, and hypercapnia leading to sleep fragmentation (microarousals), daytime hypersomnolence, impaired central nervous system, cardiovascular system, and metabolic function. Excessive daytime sleepiness, nocturia, morning headache, reduced libido, concentration deficit, blighted concentration, neurocognitive impairment, irritability, and depression are common in these patients and significantly diminish their work competence and quality of life. OSA is associated with a plethora of cardiovascular disorders, including systemic arterial hypertension (SAH), myocardial ischemia, cardiac arrhythmia, stroke, and increased arterial stiffness [12]. It is the diversity of etiology, site of obstruction, varied presentation and array of complications that necessitates a multipronged strategy to treat this condition. The different treatment options available testify to the fact that no intervention on its own is acceptable in all the cases.
Continuous Positive Airway Pressure (CPAP) has long being the recommended as the frontline treatment for OSA cases [13]. It maintains a positive pharyngeal transmural pressure and increases end-expiratory lung volume, contributing to the maintenance of an open airway [14]. Although quite efficient, it is unfortunately not always well tolerated by a significant proportion of patients over a period of time. The alternatives, bilevel positive airway pressure ventilation (BPAP) and autotitrating PAP (APAP) fair only marginally better. Intraoral devices like Mandibular advancement devices (MAD) and Tongue Retraining Devices (TRD) are well tolerated but are ineffective in a sizeable patient population. Surgical interventions like septal deviation correction, adenotonsillectomy, uvulopalatopharyngoplasty (UPPP) though helpful in milder cases cannot be done in all cases. Extensive surgeries like advancement pharyngoplasty, tongue base reduction, mandibular osteotomy, hyoid suspension myotomy and maxillomandibular advancement osteotomy come with their own set of complications. In such a scenario, sleep hygiene and changes in lifestyle habits, including weight loss, discontinuation or replacement of sedatives drugs, reducing alcohol consumption, smoking cessation, regular physical activity, and changing body position during sleep assume greater significance [15, 16]. One such alternative therapy is oropharyngeal exercises and physiotherapy which has gained significant momentum in recent years in initial and supporting treatment of snoring and mild to moderate OSA.
The application of oropharyngeal physiotherapy is governed by the pathophysiological basis of upper airway collapse, the patency of which is maintained by delicate balance between the compressive forces and the pharynx dilators [13]. An inspiratory drive results in a contraction of the diaphragm which induces a negative endopharyngeal pressure and added to the weight of the tissues surrounding the pharynx, tends to induce the closure of UA, especially at the oropharyngeal and velopharyngeal levels [16]. This trend toward pharyngeal collapse is compensated by the activation and contraction of several upper airway dilator muscles, such as the sternohyoid and omohyoid muscles, and pharyngeal lumen regulators, such as the genioglossus and digastric muscles [7]. In the presence of OSA, the compressive forces on the pharynx exceed those that tend to dilate the UA. Oropharyngeal physiotherapy helps by maintaining the muscle tone of pharyngeal dilator muscles and is also hypothesized to reduce fluid accumulation in the neck to prevent airway collapsibility. We list some of the oropharyngeal physiotherapy maneuvers which have been recommended in the literature.
| Pronounce an oral vowel intermittently (isotonic exercise) and continuously (isometric exercise) |
| Brushing the superior and lateral surfaces of the tongue while the tongue is positioned in the floor of the mouth |
| Placing the tip of the tongue against the front of the palate and sliding the tongue backward |
| Forced tongue sucking upward against the palate, pressing the entire tongue against the palate |
| Forcing the back of the tongue against the floor of the mouth while keeping the tip of the tongue in contact with the inferior incisive teeth |
| Move the jaw up and down in a chewing motion for a minute or two at a time |
| Try and stick your lower jaw out past the upper jaw and hold it there for around ten seconds at a time |
| Orbicularis oris muscle pressure with mouth closed (isometric exercise) |
| Forced nasal inspiration and oral expiration in conjunction with phonation of open vowels, while sitting |
| Alternate bilateral chewing and deglutition, using the tongue in the palate, closed teeth, without perioral contraction, whenever feeding. The supervised exercise consisted of alternate bread mastication |
The efficacy of these oropharyngeal exercises is a much deliberated topic of investigation in the western literature and has shown promising results in few statistical analyses that have been performed.
The author noted remarkable similarity in the physiology and effect of these exercises and certain yogasanas that have been performed through ages in Indian civilization. The effect of pranayama; anulom vilom, bhramri and ujjayi, as well as kapal bhati asana are relatively well known and are performed by abundant yoga practitioners regularly. These exercises facilitate increased circulation and lung capacity, as well as ensuring that nasal passages remain entirely open. These effects go a long way towards decreasing or even completely eliminating snoring problems by taking care of sinonasal etiologies. These yogasanas also target respiratory problems and significantly help with airflow in order to reduce the pathology. However, there are multiple other yogasanas and poses which are hitherto unknown, and can still contribute significantly for the better of patients. The role of set of yogasanas, as described in the methodology section, is based pharyngeal musculature by maintain oropharyngeal muscle tone. Along with this, the added benefits of yoga on the entire body further alleviate the burden of the condition. We scrutinized these yogasanas regarding their effects with regards to recommended orophayngeal exercises and discussed their direct effect in OSA.
Sinhasana (sinha = lion) It involves entire facial, tongue, jaw, oropharyngeal and neck muscles and greatly improves muscle tone. Thus, it encompasses several recommended exercises in one posture. It also stretches the platysma to keep it taut and relieves chest congestion.
Bhujangasana (bhujang = cobra) It strengthens the neck musculature along with all other muscles of upper body. It helps in clearing air passage and invigorates the heart.
Naukasana (nauka = boat) It facilitates suitable stretching, compressing and relaxation to the abdominal region to reduce abdominal fat and treat obesity and strengthens the diaphragm. It thus reduces co morbidities associated with OSA.
Dhanurasana (dhanu = bow) It is one of the best yoga poses for removing the hunching tendency of asthmatics, which aggravates ill health. Dhanurasana realigns the back thereby improves the breathing processes which leads to free flow of air through the nasal passages.
Nadi Shodhana (alternate nostril breathing) It is a brilliant asana to achieve clear and poised respiratory channels and to alleviate respiratory allergies. It also calms and rejuvenates the nervous and respiratory system and infuses them with oxygen. Regular practice of nadi shodhana has been shown to Increase breath holding time, increase peak expiratory flow rate, normalize pulse rate and set it at a reduced normal value and help to reduce excessive sympathetic tone.
Khechuri mudra (tongue lock) Kechari Mudra is considered the king among mudras and is given great importance in all the ancient yogic texts with unparalleled benefits. In OSA, it not only rejuvenates the tongue, palate and oral cavity muscles, but also aids in lowering basal metabolic rate (BMR), obesity, anti ageing properties and feeling of thirst and hunger. A relatively intricate asana even for experienced practitioners, ancient yogis are said to have mastered to attain supreme level of health and consciousness.
Chanting of OM Om is an actual vibration you create by chanting the four syllables of Om which are A, U, M, and the silent syllable. The benefits of chanting OM, as per yogic scriptures, goes beyond measurable outcomes. The mantra is said to bring a relaxing feeling to your entire body as your chest vibrates from making the sounds. Stomatognathic exercises of breathing, speech and swallowing are recommended in literature for OSA treatment [17]. Chanting of OM combines all these functions. It also helps in relaxation, relieves anxiety, improves concentration, ventilates the sinuses and strengthens the larynx.
Yoga is based on ancient Indian practices that date back to ancient culture during the 11th century. It’s a set of mental and physical exercises, movements, and breathing techniques that not only benefit you physically, but mentally. Yoga directs the mind to focus on specific body moments and breathing patterns in order to relax, strengthen, and sculpt the respiratory and nervous systems, as well as muscles in your body. Yoga is often performed for its health benefits and relieves stress and anxiety. Yoga is a remarkable natural remedy to lessen the severity of OSA and treat snoring as yogasanas rally round to improve control on movements of the oropharyngeal and respiratory system that contribute in the physiology of OSA and snoring. Strengthening these muscles is a key factor in overcoming sleep apnea. Yoga teaches regulation of breath through techniques and exercises that increase circulation, increase lung capacity, cures sinonasal, respiratory and allergic correlates of OSA. Yoga gives deep relaxation, reduces stress, slow down the body metabolism, increase self-awareness and also helps to breathe more freely that helps to control snoring. Thus, yoga is a multi pronged treatment strategy that has beneficial effect on multiple co morbidities and risk factors associated with OSA like obesity, anxiety, addictions and sedentary lifestyle. These features make practice of yoga a much healthier and superior alternative to simple oropharyngeal physiotherapy recommendations available in the literature.
Sleep apnea varies widely in its plethora of etiologies, pathogenesis, presentations and complications. Hence the management protocols also cannot adopt a one size fits all philosophy. In spite of availability of multiple treatment options, some patients do not endure any actual therapeutic approaches or do not accomplish the desired results. Therefore the role of alternative and indigenous treatment that includes diet, posture, lifestyle and exercise assume significant importance and must be encouraged by care giver. Innovative and exotic approaches like didgeridoo [18] (is a wind instrument developed by Indigenous Australians of northern Australia) and double wind reed instrument [19] playing are under extensive study at many centers. Introduction of yogasana, a time tested system, in a standardized and protocol based manner in patients with sleep apnea and snoring would be a welcome addition. Further studies are obligatory to determine to best yogasanas paradigms but undeniably, the role of yoga in sleep apnea is a very promising avenue.
Conclusion
Yoga is an efficacious, rational, economical and constructive addition to the treatment protocol in patients with sleep apnea. The benefits of yoga in sleep disorders go beyond the scope of measured outcomes. Yoga not only directly effects the oropharyngeal musculature, breathing patterns, nasal and respiratory pathologies, it also aids in alleviating risk factors like obesity, sedentary lifestyle, addictions, anxiety and allergies among others to provide symptomatic relief to the patients. Thus, it is a multi pronged, non surgical, non medicinal, alternative and indigenous approach to an equally diverse medical predicament. Standardizing the protocols for yoga in treatment for snoring and sleep apnea is the need of the hour. Further studies on efficacy of yoga need to be performed to understand its full realm of potential.
Compliance with Ethical Standards
Conflict of interest
None.
Ethical Approval
Departmental ethical clearance taken.
Informed Consent
Obtained.
Animal Subjects
No animal subjects were used.
References
- 1.American Academy of Sleep Medicine (AASM) Task Force Sleep-related breathing disorders in adults. Recommendation for syndrome definition and measurement techniques in clinical research. Sleep. 1999;22:667–668. doi: 10.1093/sleep/22.5.667. [DOI] [PubMed] [Google Scholar]
- 2.Marin JM, Carrizo SJ, Vicente E, Agusti AG. Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnea with or without treatment with continuous positive airway pressure: an observational study. Lancet. 2005;365:1046–1053. doi: 10.1016/S0140-6736(05)71141-7. [DOI] [PubMed] [Google Scholar]
- 3.Pham LV, Schwartz AR. The pathogenesis of obstructive sleep apnea. J Thorac Dis. 2015;7(8):1358–1372. doi: 10.3978/j.issn.2072-1439.2015.07.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jordan AS, McSharry DG, Malhotra A. Adult obstructive sleep apnoea. Lancet. 2014;383(9918):736–747. doi: 10.1016/S0140-6736(13)60734-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bradley TD, Floras JS. Obstructive sleep apnoea and its cardiovascular consequences. Lancet. 2009;373(9657):82–93. doi: 10.1016/S0140-6736(08)61622-0. [DOI] [PubMed] [Google Scholar]
- 6.Malhotra A, White DP. Obstructive sleep apnoea. Lancet. 2002;360:237–245. doi: 10.1016/S0140-6736(02)09464-3. [DOI] [PubMed] [Google Scholar]
- 7.Vincent HK, Shanely RA, Stewart DJ, Demirel HA, Hamilton KL, Ray AD, et al. Adaptation of upper airway muscles to chronic endurance exercise. Am J Respir Crit Care Med. 2002;166(3):287–293. doi: 10.1164/rccm.2104120. [DOI] [PubMed] [Google Scholar]
- 8.Netzer NC, Stoohs RA, Netzer CM, Clark K, Strohi KP. Using the Berlin Questionnaire to identify patients at risk for the sleep apnea syndrome. Ann Intern Med. 1999;131:485–491. doi: 10.7326/0003-4819-131-7-199910050-00002. [DOI] [PubMed] [Google Scholar]
- 9.Johns MW. A new method for measuring daytime sleepiness. The Epworth Sleepiness Scale. Sleep. 1991;14:540–559. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 10.Buysse DJ, Reynolds CF, III, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 11.Burwell CS, Robin ED, Whaley RD, Bickelmann AG. Extreme obesity associated with alveolar hypoventilation: a pickwickian syndrome. Am J Med. 1956;21:811–818. doi: 10.1016/0002-9343(56)90094-8. [DOI] [PubMed] [Google Scholar]
- 12.Pedrosa RP, Barros IM, Drager LF, Bittencourt MS, Medeiros AK, Carvalho LL, et al. OSA is common and independently associated with hypertension and increased arterial stiffness in consecutive perimenopausal women. Chest. 2014;146(1):66–72. doi: 10.1378/chest.14-0097. [DOI] [PubMed] [Google Scholar]
- 13.Young T, et al. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993;328:1230–1235. doi: 10.1056/NEJM199304293281704. [DOI] [PubMed] [Google Scholar]
- 14.Naughton MT. Sleep disorders in patients with congestive heart failure. Curr Opin Pulm Med. 2003;9(6):453–458. doi: 10.1097/00063198-200311000-00001. [DOI] [PubMed] [Google Scholar]
- 15.Peppard PE, Young T, Palta M, Dempsey J, Skatrud J. Longitudinal study of moderate weight change and sleep-disordered breathing. JAMA. 2000;284(23):3015–3021. doi: 10.1001/jama.284.23.3015. [DOI] [PubMed] [Google Scholar]
- 16.Weitzenblum E, Racineux JL. Syndrome d’apnées obstructives du sommeil. 2. Paris: Masson; 2004. [Google Scholar]
- 17.Guimarães KC, Drager LF, Genta PR, Marcondes BF, Lorenzi-Filho G. Effects of oropharyngeal exercises on patients with moderate obstructive sleep apnea syndrome. Am J Respir Crit Care Med. 2009;179(10):962–966. doi: 10.1164/rccm.200806-981OC. [DOI] [PubMed] [Google Scholar]
- 18.Guillemineault C, Tilkian A, Dement WC. The sleep apnea syndromes. Annu Rev Med. 1976;27:465–484. doi: 10.1146/annurev.me.27.020176.002341. [DOI] [PubMed] [Google Scholar]
- 19.Peppard PE, Young T, Palta M, Skatrud J. Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med. 2000;342:1378–1834. doi: 10.1056/NEJM200005113421901. [DOI] [PubMed] [Google Scholar]


