Abstract
The facial area is one of the most frequently injured parts of the body (Abiose in Br J Oral Maxillofac Surg 24(1):319, 1986; Adi et al. in Br J Oral Maxillofac Surg 28(3):1949, 1990; Allan and Daly in Int J Oral Maxillofac Surg 19(5):26871, 1990), and the mandible is one of the most commonly fractured maxillofacial bones (1990; Azevedo et al. in J Trauma 45(6):10847, 1998; Bremerich et al. in Acta Stomatol Belg 93:511, 1996). Mandible is the only mobile bone of the skeleton, and hence vulnerable to fracture. This is a retrospective study of 50 mandibular fracture cases managed at the Department of ENT, Govt. Medical College Bhavnagar during the 2 years period from 2014 to 2016. Maximum subjects were in age group 21–30 years with a male preponderance. Road traffic accident is the main cause followed by falls and assault. Symphysis is the most common site of Mandibular fracture. Mandible fracture is a common entity in Road traffic accidents. Multiple fractures are seen in 40% of mandibular fracture cases. The results were equally good in patients requiring only MMF (Maxillo Mandibular Fixation) and inpatients requiring MMF and Plating, during the follow up up to 8 weeks. Physiotherapy was advised for all the post op patients after 2 months.
Keywords: Mandible fracture, Road traffic accidents, Maxillo mandibular fixation
Introduction
HIPPOCRATES “Displaced but incomplete fractures of the mandible where continuity of the bone is preserved should be reduced by pressing the lingual surface with the fingers while counterpressure is applied from the outside. Following the reduction, teeth adjacent to the fracture are fastened to one another using gold wire.”
The first ever inscription on mandibular fractures dates back to 1650 BC [1]. Modern life is very fast which includes high speed travel and a violent, intolerant society making everyone susceptible to facial trauma. The facial area is one of the most frequently injured parts of the body [2, 3, 4] and hence vulnerable to fracture. The presence of teeth in the mandible is the most important anatomical factor, which makes its fracture different from fractures elsewhere in the body.
Boole et al. [7], the fracture is defined as “breach in the continuity of bone” [8].The energy required to fracture it being of the order of 44.6–74.4 kg/m, which is about the same as the zygoma and about half that for the frontal bone [9, 10, 11, 12]. It is four times as much force is required to fracture maxilla [13]. Understanding the demographic patterns of mandibular fractures will assist health care providers to plan and manage the treatment of traumatic maxillofacial injuries and also can be used to guide the future funding of public health programs geared toward prevention. This study attempts to evaluate the patterns of mandibular fracture retrospectively, based on patient age, sex, and mechanism of injury and to define current, predictable patterns of fracture based on patient demographics and mechanism of injury in the western part of the country.
Anatomy and Pathophysiology
There are various muscle groups acting on the mandible which bring about its actions and also explain the reason behind such various types of fractures in mandible.
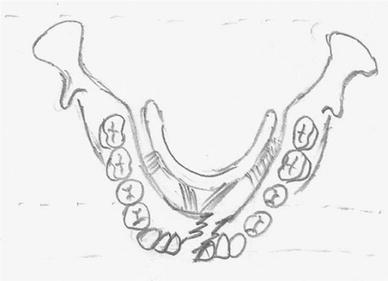
Various muscle groups attached to the mandible (Fig. 1):
Fig. 1.
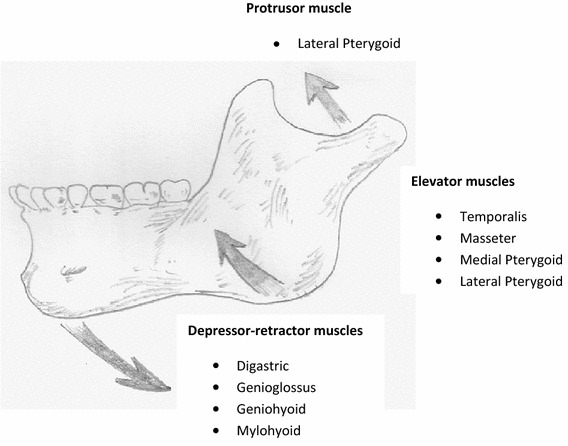
Various muscle groups attached to the mandible
Jaw depressors: mylohyoid, digastric, geniohyoid.
Jaw elevators: temporalis, masseter, medial pterygoid, lateral pterygoid.
Jaw protruder: lateral pterygoid.
Muscle Attachments and Displacement of Fractures
The periosteum is very important in determining the stability of mandible. The periosteum of the mandible is stout and unyielding and gross displacement of fragments cannot occur if it remains attached to the bone. Only after the periosteum is removed or stripped from the bone the displacement occurs and hence to reduce the fracture also we need to strip off the periosteum completely to realign the bone.
Fractures at the Angle of the Mandible
The Medial pterygoid–masseter ‘sling’ acts on the fractures of the angle of the mandible. Masseter muscle is the weaker component. Following are the types of fractures in this region (Fig. 2).
Fig. 2.
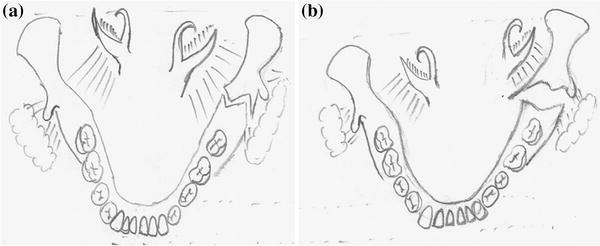
a Vertically favourable, b vertically unfavourable
If the vertical direction of the fracture line favours the unopposed action of the medial pterygoid muscle, the posterior fragment is pulled lingually. If the horizontal direction of the fracture line favours the unopposed action of the masseter and medial pterygoid muscle in the upward direction, the posterior fragment will be displaced upwards. The periosteum must be stripped to displace a fracture (Fig. 3).
Fig. 3.
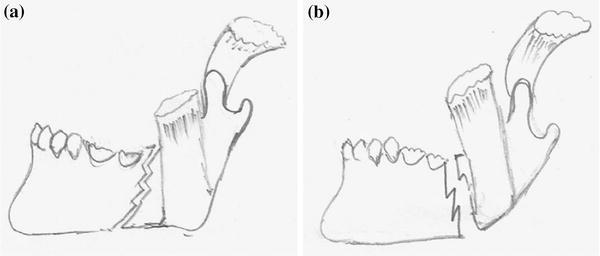
a Horizontally favourable, b horizontally unfavourable as depicted in the following images
Fractures at Symphysis and Parasymphysis
There are important muscle attachments in the symphysis region. The mylohyoid muscle is the diaphragm between the hyoid bone and the mylohyoid ridge on the inner aspect of the mandible. In the transverse midline fracture of the symphysis the mylohyoid and the geniohyoid muscles acts as a stabilizing force (Fig. 4). An oblique fracture in this region will overlap due to the influence the geniohyoid/mylohyoid diaphragm (Fig. 5).
Fig. 4.
Fracture in the midline of the mandible. Minimal displacement occurs in such injuries as the fracture line passes between the genial tubercles
Fig. 5.
Fracture lateral to the midline in the incisor area. The fracture with the genial tubercles is displaced lingually by the pull of the geniohyoid and mylohyoid muscles
A considerable force that disrupts the periosteum causes bilateral parasymphyseal fracture. Such a fracture is readily displaced posteriorly due to the genioglossus muscle and to a lesser extent the geniohyoid (Fig. 6).
Fig. 6.
Bilateral fracture of the body of the mandible. The anterior fragment is displaced backwards by the pull of the muscles attached to the genial tubercles
The only situation in which tongue fall causing a threat to the airway is when the consciousness of the patient is depressed in patients of detached symphysis.
Materials and Methods
This is a retrospective study of 100 mandibular fracture cases managed at the Department of ENT, Govt. Medical College Bhavnagar during the last 10 years. Data (clinical records, patients’ files) were reviewed and analyzed in terms of age, gender, etiology, anatomical site of fracture and treatment methods.
Results
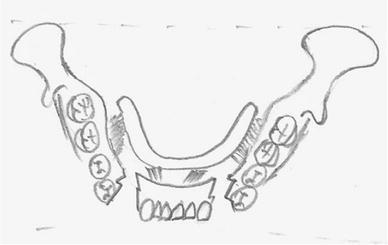
Agewise Distribution of Study Subjects
Maximum number of subjects were in the age group 21–30 years (30%, n = 100) followed by 11–20 (26%, n = 100), 31–40 (18%, n = 100), < 10 (12%, n = 100), 41–50 (6%, n = 100), and 50 years and above (8%, n = 100). Around three fourth (74%) of patients were in the age range 11–40 years.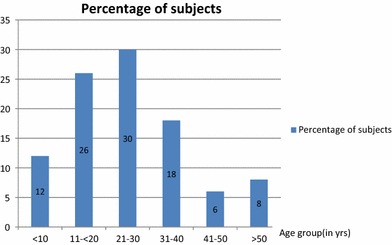
Distribution According to Sex
Around 3/4th (78%, n = 100) were males and 1/4th (22%, n = 100) were females. The male to female ratio is 3.5:1
Unilateral or Bilateral Fractures
Among the fractures 60% (60, n = 100) were unilateral and 40% (40, n = 100) were bilateral. Among the unilateral fractures right side were 50% were right side and 35% were on left side.
Etiology of Mandibular Fractures
Most common cause was Road Traffic Accident 70(70%), followed by Accidental falls 20(20%) and Assault 10(10%).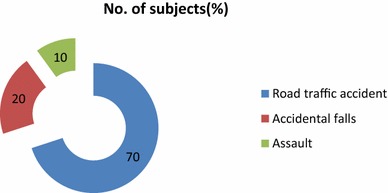
Site of Mandibular Fracture
Order of Fracture site Most Common being Symphysis (Inc. parasymphysis) (50%, n = 100), followed by Angle (30%, n = 100), Body (14%, n = 100) least common is the Condyle and Ramus.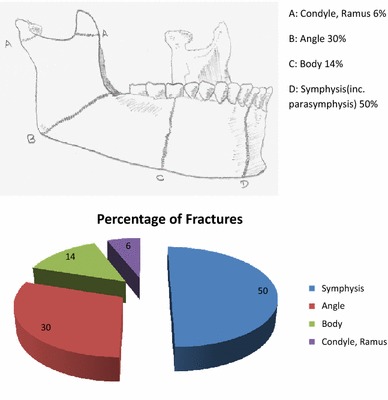
Combinations of Fractures
Multiple fractures were seen in 40 cases (40%, n = 100) and single fractures in 60 cases (60%, n = 100). Multiple fractures most commonly involved Body and Angle 14 (35%, n = 40) followed by Body and body 10 (25%, n = 40), Symphysis and Condyle 8 (20%, n = 40), Symphysis and angle 4 (10%, n = 40), Symphysis and Ramus 4 (10%, n = 40).
| Sl. no. | Site | No. of cases | Percentage |
|---|---|---|---|
| 1. | Body + Angle | 14 | 35 |
| 2. | Body + body | 10 | 25 |
| 3. | Symphysis + Condyle | 8 | 20 |
| 4. | Symphysis + Angle | 4 | 10 |
| 5. | Symphysis + Ramus | 4 | 10 |
Association of Site of Mandibular Fractures with Etiology
| Sl. no | Site | No. of sites | RTA no. | RTA% | Falls no. | Falls% | Assault no. | Assault% |
|---|---|---|---|---|---|---|---|---|
| 1. | Angle | 50 | 44 | 88 | 2 | 4 | 4 | 8 |
| 2. | Body | 30 | 14 | 46.6 | 14 | 46.6 | 2 | 6.8 |
| 3. | Symphysis | 14 | 8 | 57.1 | 2 | 14.2 | 4 | 28.7 |
| 4. | Condyle and Ramus | 6 | 4 | 66.6 | 2 | 33.4 | – | 0 |
Angle fractures are most commonly seen in Road traffic accidents (RTA) whereas body fracturese seen equally in both RTA and Falls. Symphysis and Condyle fractures are both seen maximum in RTA.
Age Group and Number of Fracture Sites
Single fracture sites were seen in age group of less than 10 and greater than 50. 80% of cases between 10 and 50 years of age had multiple fractures and maximum between 21 and 30 years of age.
Surgical Management
Plating and Wiring were done in 90 cases (90%, n = 100) and only Plating (Fig. 2) in 10 cases(10%, n = 100).
Surgical Technique of Mandible Fracture by Wiring and Plating
Whenever there is a displaced fracture of mandible causing malocclusion of teeth irrespective of the site of fracture, then the following surgical technique is followed to achieve the best possible occlusion for the patient. Both plating and wiring are done. First wiring is done followed by plating and lastly wires are tightened.
Technique
Necessary Instruments
26 g Wire, 4-hole micro plates, 2-hole micro plates, Drill bit, Hand motor, Screw driver, Wire cutter.
Interdental Eyelet Wiring
Eyelets are made with 6 in. (15 cm) length of 26 g metallic wire and holding it with a needle holder in the midline and then giving 2 quick twists so that it forms a loop in the midline and two long arms of equal length.
As shown in the Fig. 7 these eyelets are fitted in between 2 teeth and twisted to become tight. Care must be taken to push the wire well down on the lingual and palatal aspect of the teeth before twisting the free ends tight, as the eyelet will tend to be displaced up the tooth and become loose. About five eyelets are applied in the upper and five in the lower jaw and then the eyelets are connected with tie wires passing through the eyelets from the upper to the lower jaw.
Fig. 7.
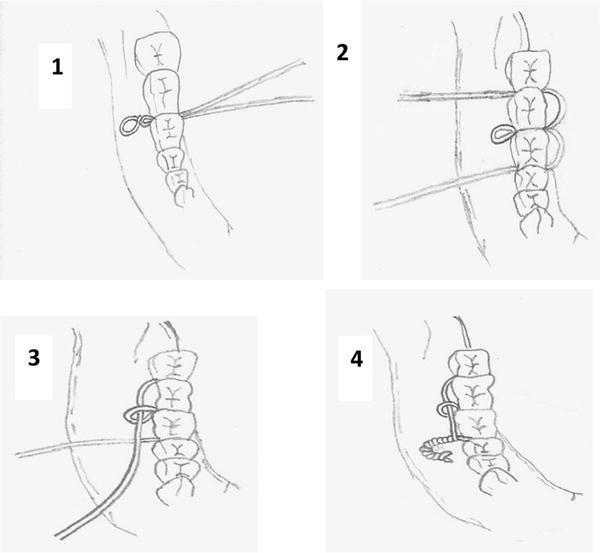
Diagram of the stages involved during the insertion of an eyelet wire
The eyelets should be positioned in the upper and the lower jaw that when the tie wires are threaded through them a cross bracing effect is achieved (Fig. 8).
Fig. 8.
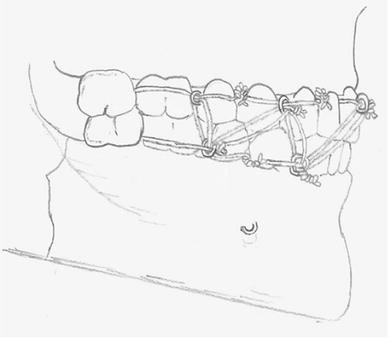
A completed eyelet wiring showing how the eyelets are connected by the wires
If cross-bracing is not done complete immobilization is not achieved and there is slight mobility of the mandible. The wire is very sharp and springy and careless handling can traumatize the patient’s eyeball.
After fixing the eyelet wires the tie wires are threaded through the eyelets to connect the eyelets of the upper and lower jaw, but twisting of the tie wires is done at a later stage. Teeth requiring extraction are removed, the throat pack is removed after which the fracture is reduced and the tie wire fixation is tightened.
Some patients have abnormal occlusion pre operatively and this must be understood by the operator before performing the surgery because an attempt to achieve a theoretically correct occlusion in such cases may result in gross derangement of the bony fragment. First the tie wires in the molar area are tightened on one side and then on the other, so working round to the incisor area. If wires are tightened on one side first a cross-over bite is produced and if the anterior wires are tightened before the wires in the molar area a posterior open bite results. In multirooted teeth the wires are twisted very tight. First the tie wires are loosely tightened and after the occlusion is checked the final tightening is done. We must make sure the tongue is not trapped between the cusps of teeth. After the inter dental eyelet wiring is completed a finger is run round the patient’s mouth to check for any loose ends of wire which may have been left projecting and may ulcerate the soft tissue.
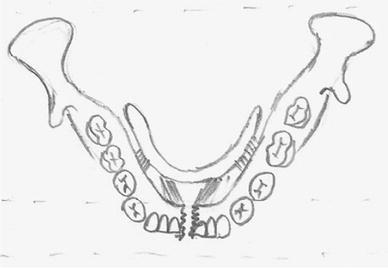
For plating Fig. 9 the fracture site is either reached intraorally or externally depending on where the fracture site is.
Fig. 9.

Plating of mandible fracture
If intraoral method is used, then a 15 no. knife is used to put an incision over the lower gum mucosa after local infiltration, whereas in the extra oral route incision is given over the skin at the fracture site. This incision is deepened till the periosteum is reached. Then the periosteum elevator is used to elevate the periosteum completely exposing the fracture site completely, avoiding injury to the mental vessels and nerve. Then one of the operating surgeons holds the displaced mandible in perfect alignment while the other surgeon fixes the 4-hole micro plates over the fracture site by drilling.
Post Op
Patient is asked to take feed through Ryle’s tube for 4–5 days, followed by straw feeding with proper instructions for maintaining oral hygiene. At any point of time if patient feels nauseating or vomiting, he is advised to come to hospital immediately to remove wiring to avoid aspiration. The MMF wires are removed after 21 days and the plates are kept in situ. Patient is asked to take semisolid diet for 1 month after wire removal.
Discussion
This study evaluated the patterns of mandibular fractures along with the relationship with the mechanism of injury and site of the fracture. Consequences of facial trauma include feeling embarrassed to smile, laugh and show one’s teeth, difficulty in maintaining social relationships, irritability and an inability to maintain a healthy emotional state and negative impact on the quality of life [14, 15, 16].
In the literature, the frequency of facial fractures is lower in the young population than in the adult Population [17, 18]. However, the data on which this premise is based may be subject to alternative interpretations, and the true incidence of facial fractures in this region, especially in the young population, is much higher than previously reported. The reasons cited for this high incidence include the greater size of the young population, socioeconomic problems, and parents’ careless attitudes.
Males were predominantly affected, which is in agreement with other studies [19, 20] due to more involvement in outdoor activities. The peak incidence is occurring between 20 and 25 years and least being in the age above 50 years. This is in conformity with Adi et al. [21], Bataineh [22], Dongas and Hall [23]. Most frequent cause of fracture mandible in this study was RTA, which is in accordance with Luce et al. [24], Bataineh [22]. The anatomic distribution and incidence of mandibular fracture are widely variable [25]. Many authors reported symphysis [26] as the most frequently affected site whereas, others reported this to be mandibular body [20], angle [23, 27] and condyle [28]. In our study the most common site of fracture is symphysis (inc. Parasymphysis) (50%, n = 100).The reason why parasymphysis is very common is due to the presence of permanent tooth buds in the pediatric mandible presenting a high tooth to bone ratio, while in adults it is partly to the length of canine root weakening the structure.
Also bone is fractured at this site due to high tensile strain since their resistance compressive force is greater. Mandible is like an architectural arch which distributes the applied force along its length. But not being a smooth curve in a uniform cross-section. There are parts like symphysis at which force per unit area developed is greater resulting in increased concentration of tensile strength leading to a fracture at the site of maximum convexity of the curvature.
Among multiple fracture site we observed that the body was commonly associated with angle, which is in accordance with the study by Ogundare et al. [27] and contrary to Dongas and Hall [23] have reported symphysis with angle as the most common combination.
Surgical management include either plating or both wiring and plating. In our study both plating and wiring were done in 90% of cases and only plating in 10%. Only plating was done in favourable fractures in paediatric age group. Favourable fractures have the muscle groups acting with the surgeon to realign the fracture and hence wiring is not needed. In paediatric age group patients don’t understand nausea, vomiting (to prevent aspiration in cases of wiring) and also the deciduous teeth in children are not very strong to withhold wiring.
Within the limitation of our study, we could conclude that mandibular fractures can be complicated, demanding and have a compelling impact on patient’s quality of life. The prevalence of various types of mandibular fractures from the anatomic standpoint and their correlation to etiology can be helpful to the clinician for effective early management.
Conclusion
This study evaluated and analyzed clinical and statistical data of patients who were treated with open reduction and internal fixation for mandible fractures at the Department of otorhinolaryngology in Govt Medical College and Sir. T. Hospital Bhavnagar between 2014 and 2016. The following results were summarized in this study.
Mandible fracture was more in males compared to females by a ratio of 3.5:1.
Mandible fracture was commonly seen in patients in their 20 s, followed by patients in their 10 and 30 s.
The most common etiologic factors of mandible fracture were road traffic accidents, accidental falls followed by assault.
The symphysis (inc. parasymphysis) was the most affected region followed by the angle and body.
The ratio of multiple fractures with two or more fracture lines was 40%, the body and angle was the most affected site followed by the body and body.
Interdental eyelet wiring is simple to apply and very effective in operation. Excellent immobilization is effected as the operator can see that the occlusion is perfectly restored.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no competing interests.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
References
- 1.Ogundare BO, Bonnick A, Bayley N. Pattern of mandibular fractures in an urban major trauma center. J Oral Maxillofac Surg. 2003;61:7138. doi: 10.1053/joms.2003.50118. [DOI] [PubMed] [Google Scholar]
- 2.Abiose BO. Maxillofacial skeleton injuries in the western states of Nigeria. Br J Oral Maxillofac Surg. 1986;24(1):319. doi: 10.1016/0266-4356(86)90037-9. [DOI] [PubMed] [Google Scholar]
- 3.Adi M, Ogden GR, Chisholm DM. An analysis of mandibular fractures in Dundee, Scotland 1977 to 1985. Br J Oral Maxillofac Surg. 1990;28(3):1949. doi: 10.1016/0266-4356(90)90088-3. [DOI] [PubMed] [Google Scholar]
- 4.Allan BP, Daly CG. Fractures of mandible: a 35 year retrospective study. Int J Oral Maxillofac Surg. 1990;19(5):26871. doi: 10.1016/S0901-5027(05)80417-5. [DOI] [PubMed] [Google Scholar]
- 5.Azevedo AB, Trent RB, Ellis A. Population based analysis of 10,766 hospitalizations for mandibular fractures in California 1991 to 1993. J Trauma. 1998;45(6):10847. doi: 10.1097/00005373-199812000-00020. [DOI] [PubMed] [Google Scholar]
- 6.Bremerich A, Freidl S, Gellrich NC. Mandibular fractures. An epidemiological study of a 10 year cohort. Acta Stomatol Belg. 1996;93:511. [PubMed] [Google Scholar]
- 7.Boole JR, Holtel M, Amoroso P, Yore M. 5196 mandible fractures among 4381 active duty army soldiers, 1980 to 1998. Laryngoscope. 2001;111(10):16916. doi: 10.1097/00005537-200110000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Kruger GO. Textbook of oral and maxillofacial surgery. 6. New Delhi: Jaypee Brothers; 1990. [Google Scholar]
- 9.Swearingen JJ. Tolerance of the human face to crash impact. Stillwater: Office of Aviation Medicine, Federal Aviation Agency; 1965. [Google Scholar]
- 10.Hodgson VR. Tolerance of the facial bones to impact. Am J Anat. 1967;120:113–122. doi: 10.1002/aja.1001200109. [DOI] [Google Scholar]
- 11.Nahum AM. The biomechanics of maxillofacial trauma. Clin Plast Surg. 1975;2(1):59–64. [PubMed] [Google Scholar]
- 12.Luce EA, Tubb TD, Moore AM. Review of 1000 major facial fractures and associated injuries. Plast Reconstr Surg. 1979;63(1):26–30. doi: 10.1097/00006534-197901000-00005. [DOI] [PubMed] [Google Scholar]
- 13.Huelke DF. Location of mandibular fractures related to teeth and edentulous regions. J Oral Surg Anesth Hosp Dent Serv. 1964;22:396–405. [PubMed] [Google Scholar]
- 14.Barbosa TS, Gavião MB. Oral healthrelated quality of life in children: part I. How well do children know themselves? A systematic review. Int J Dent Hyg. 2008;6:939. doi: 10.1111/j.1601-5037.2007.00276.x. [DOI] [PubMed] [Google Scholar]
- 15.Cortes MI, Marcenes W, Sheiham A. Impact of traumatic injuries to the permanent teeth on the oral health related quality of life in 12–14 year old children. Community Dent Oral Epidemiol. 2002;30:1938. doi: 10.1034/j.1600-0528.2002.300305.x. [DOI] [PubMed] [Google Scholar]
- 16.RamosJorge ML, Bosco VL, Peres MA, Nunes AC. The impact of treatment of dental trauma on the quality of life of adolescents: a case control study in southern Brazil. Dent Traumatol. 2007;23:1149. doi: 10.1111/j.1600-9657.2005.00409.x. [DOI] [PubMed] [Google Scholar]
- 17.Ferreira PC, Amarante JM, Silva AC, Pereira JM, Cardoso MA, Rodrigues JM. Etiology and patterns of pediatric mandibular fractures in Portugal: a retrospective study of 10 years. J Craniofac Surg. 2004;15(3):38491. doi: 10.1097/00001665-200405000-00008. [DOI] [PubMed] [Google Scholar]
- 18.Haug RH, Foss J. Maxillofacial injuries in the pediatric patient. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90(2):12634. doi: 10.1067/moe.2000.107974. [DOI] [PubMed] [Google Scholar]
- 19.Ellis E, 3rd, Moos KF, elAttar A. Ten years of mandibular fractures: an analysis of 2137 cases. Oral Surg Oral Med Oral Pathol. 1985;59:120–129. doi: 10.1016/0030-4220(85)90002-7. [DOI] [PubMed] [Google Scholar]
- 20.Olson RA, Fonseca RJ, Zeitler DL, Osbon DB. Fractures of the mandible: a review of 580 cases. J Oral Maxillofac Surg. 1982;40:23–28. doi: 10.1016/S0278-2391(82)80011-6. [DOI] [PubMed] [Google Scholar]
- 21.Adi M, Ogden GR, Chisholm DM. An analysis of mandibular fractures in Dundee, Scotland (1977 to 1985) Br J Oral Maxillofac Surg. 1990;28:194–199. doi: 10.1016/0266-4356(90)90088-3. [DOI] [PubMed] [Google Scholar]
- 22.Bataineh AB. Etiology and incidence of maxillofacial fractures in the north of Jordan. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;86:31–35. doi: 10.1016/S1079-2104(98)90146-9. [DOI] [PubMed] [Google Scholar]
- 23.Dongas P, Hall GM. Mandibular fracture patterns in Tasmania, Australia. Aust Dent J. 2002;47:131–137. doi: 10.1111/j.1834-7819.2002.tb00316.x. [DOI] [PubMed] [Google Scholar]
- 24.Luce EA, Tubb TD, Moore AM. Review of 1000 major facial fractures and associated injuries. Plast Reconstr Surg. 1979;63:26–30. doi: 10.1097/00006534-197901000-00005. [DOI] [PubMed] [Google Scholar]
- 25.Imazawa T, Komuro Y, Inoue M, Yanai A. Mandibular fractures treated with maxillomandibular fixation screws (MMFS method) J Craniofac Surg. 2006;17:544–549. doi: 10.1097/00001665-200605000-00026. [DOI] [PubMed] [Google Scholar]
- 26.Chuong R, Donoff RB, Guralnick WC. A retrospective analysis of 327 mandibular fractures. J Oral Maxillofac Surg. 1983;41:305–309. doi: 10.1016/0278-2391(83)90297-5. [DOI] [PubMed] [Google Scholar]
- 27.Ogundare BO, Bonnick A, Bayley N. Pattern of mandibular fractures in an urban major trauma center. J Oral Maxillofac Surg. 2003;61:713–718. doi: 10.1053/joms.2003.50118. [DOI] [PubMed] [Google Scholar]
- 28.Al Ahmed HE, Jaber MA, Abu Fanas SH, Karas M. The pattern of maxillofacial fractures in Sharjah, United Arab Emirates: a review of 230 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;98:166–170. doi: 10.1016/j.tripleo.2004.01.020. [DOI] [PubMed] [Google Scholar]


