Abstract
Background
Mentoring of medical students remains a core pillar of medical education, yet the changing landscape of medicine has called for new and innovative mentoring models to guide students in professional development, career placement, and overall student well-being. The objective of this review is to identify and describe models of mentorship for US medical students.
Methods
We searched PubMed, PsycINFO, Education Resources Information Center, and Cochrane Databases of Systematic Reviews following PRISMA guidelines. We included original, English-language studies of any research design including descriptive studies that described a mentorship program at a US medical school designed for medical students.
Results
Our search yielded 3743 unique citations. Thirty articles met our inclusion criteria. There was significant diversity of the identified programs with regard to program objectives and size. The traditional dyad model of mentorship was the most frequently cited model, with a combination of models (dyad and group mentorship) cited as the second most common. Outcome measures of the programs were largely survey based, with satisfaction being the most measured outcome. Overall, satisfaction was highly rated throughout all the measured mentoring programs. Seven programs provided objective outcomes measures, including improved residency match data and increased scholarly productivity. The programs with objective outcomes measures were smaller, and 6/7 of them focused on a specific clinical area. Five of these programs relied on the traditional dyad model of mentorship. Cost and faculty time were the most frequently cited barriers to these programs.
Discussion
Our review demonstrates that mentoring programs for medical students can positively improve medical school satisfaction and career development. These results underscore the need for continued innovative mentoring programs to foster optimal student development in the setting of the increasingly competitive residency match process, growing expectations about student research productivity, and the national focus for overall student wellness.
Electronic supplementary material
The online version of this article (10.1007/s11606-019-05256-4) contains supplementary material, which is available to authorized users.
KEY WORDS: mentoring, medical, students, review
INTRODUCTION
Medical students face unique challenges during their education. They must assimilate into the medical community while confronting the multifaceted demands of medical education. These challenges can be facilitated through effective mentoring. Medical student mentoring has been associated with easier adaptation to the learning environment1, improved satisfaction with career advising2, and increased research productivity3. Additionally, the Liaison Committee on Medical Education (LCME) requires schools to have “an effective career advising system” and programs to “promote [medical students] well-being.”4 The data also suggest that medical students consider mentorship important to their education; however, only about a third of medical students report having a mentor5.
In response to these growing imperatives, medical schools have been forced to develop innovative programs to guide students throughout their medical school careers. Two previous reviews have reported on medical school mentoring programs through 20086,7. In the last decade, myriad new programs have been created to keep pace with the changing needs of medical students, including the increased competitiveness of the residency match process8.
The purposes of this review are to identify and describe models of mentorship for US medical students, to summarize the benefits and/or disadvantages of each, and to assess barriers to mentorship. Our definition of mentorship for this review is “a developmental partnership in which knowledge, experience, skills, and information are shared between mentor(s) and mentee(s) to foster the mentee’s professional development and, often, also to enhance the mentor’s perspectives and knowledge.”9
METHODS
Search Strategy and Study Selection
We searched PubMed including Medline (1966–present), PsycINFO (1957–present), the Education Resources Information Center (ERIC) (1966–present), and the Cochrane Database of Systematic Reviews (1992–present) following the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines to identify studies that describe mentorship programs for medical students. Additionally, the reference lists of previous reviews on this topic were hand-searched for any further papers meeting our inclusion criteria. A formal quality assessment of manuscripts was precluded, as neither the Cochrane Risk of Bias nor the Newcastle Ottawa Scale can be applied to the only type of study (descriptive) that exists in the mentorship literature. Search strategies were developed with a health sciences librarian (RT). Using each database platform’s subject headings and search fields, various combinations of the following subject headings and keyword groupings were investigated: mentoring, academic medicine, physicians (see Appendix online for full search strategy in the Electronic Supplementary Material). When building the search strategy, a wide range of specialty terms was tested. Only specialty terms that added unique records to the set were included in the final search strategy. Searches were finalized on June 27, 2017. Two reviewers (JA and AF) independently evaluated all records for eligibility using DistillerSR, a web-based systematic review data management system. Any discrepancies regarding inclusions were resolved by group consensus, and consultation with the senior author (JC). Additionally, in order to ensure that the review was up-to-date, the search was re-run on November 6, 2018. One additional study published after our original search date met inclusion criteria.
Study Eligibility Criteria
We included original, English-language published studies that met the following inclusion criteria: (1) described a mentorship program, exclusive of mentoring for a specific/procedural skill or scholarship/research program, (2) described a program designed for medical students or provided results for medical students, and (3) described a program conducted in the USA. Given the qualitative and/or descriptive nature of the majority of the mentorship literature, we decided a priori to include all research designs in the interest of generating a comprehensive review of this literature. Full inclusion and exclusion criteria are described in our protocol registered on PROSPERO and can be accessed at https://www.crd.york.ac.uk/PROSPERO/display_record.php?RecordID=83451
Data Abstraction
Two study authors (JA and AF) independently abstracted all data. Study abstraction forms consisted of fields including (1) the author and year the study was published; (2) program participants (mentees and mentors); (3) model of mentorship; (4) program objectives; (5) description of program components; (6) program evaluation including whether the program was evaluated and methods of evaluation; and (7) results of evaluation. Additionally, we evaluated facilitators and/or barriers including costs to these programs.
RESULTS
Study Selection
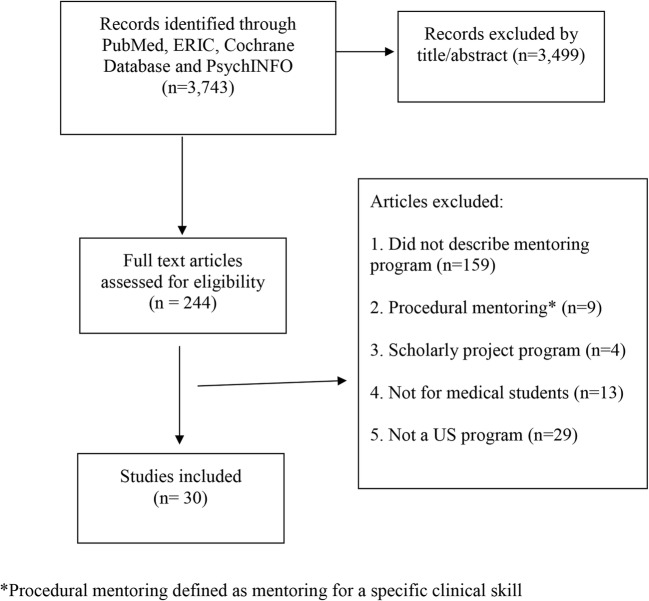
We retrieved 3625 citations in June 2017 and an additional 436 in November 2018 for a total of 4061 citations. After screening for duplicate records, 3743 remained. A total of 3499 records were excluded based on title and abstract, and 244 underwent full text review. In total, 30 papers describing 29 programs met our inclusion criteria (Fig. 1). Two papers described the same mentoring program10,11.
Fig. 1.
PRISMA diagram.
Program Description
The description of these programs including participants, mentorship model, program objectives, and program components is found in a table included in the supplemental material online.
Mentoring Models
The most common model of mentorship used was the traditional dyad model, which was used exclusively by 16 programs10–25.
Four programs used a group model of mentorship26–29. Three of these utilized traditional group mentorship wherein faculty members would meet with groups of medical students periodically26,27,29. Another program used what they described as a “tiered” group mentorship model in which the mentors were a combination of faculty, resident, and fourth year medical students and the mentees were junior medical students28. The goal of the tiered model was to offer mentorship across the spectrum of academic position so that the residents and fourth year medical students who were serving as mentors to more junior students could also receive mentorship from the faculty. An additional program that used multiple models of mentorship also described a “vertical” approach with a similar goal of providing mentorship across the spectrum of academic position30.
Seven of the 28 programs used a combination of models, specifically dyad and group mentoring2,30–35. Four of these programs were part of larger longitudinal initiatives by the medical school within the context of an advisory college/dean program. In these programs, faculty members were often assigned a group of medical students whom they met with in groups and individually to offer mentorship and assist with professional development and career planning2,30,32,33. In general, group mentoring was used to discuss broadly applicable topics, which then allowed the one-on-one meetings to be more specific to the individual needs of the student.
Program Objectives
Most programs stated broad objectives including assisting medical students with career development/career planning2, 10,12,14,30, professional development 11,12,19,23,24,26,30,32,33, and well-being29,32.
Many of the programs had the specific objective of mentoring either underrepresented minorities (URM) or female medical students. Seven of the programs were for URM students12,13,21,29,31,35,36. The majority of these were only for URM medical students12,13,21,29,31; however, two of the programs were part of a larger initiatives involved mentees from pre-medical students through faculty35,36. There were two programs whose stated objectives were to provide mentoring to female medical students22,27.
Tweleve14,15,17,18,20–23,25,28,34,37 provided mentorship that was specific to a certain field of medicine with the objective of recruiting students and providing career and research mentorship for that specialty.
Program Evaluation
Seven of the programs reported objective outcomes related to clerkship grades, research productivity, and residency match (Table 1). Five were subspeciality specific15,17,18,23,34, one focused on URM students36, and one program was aimed at developing a pipeline of URM students in a surgical subspeciality21. Two studies reported a significant increase in presentations and publications18,34. One program for primary care reported that in each year of the program, more students who participated in the mentoring program matched into a primary care specialties compared to non-participating students from the same medical school graduating class (year 1 87.5% vs 55.8% and year 2 78.9% vs 35.9%)15. A program that was part of the obstetrics and gynecology clerkship found an increase in the number of students applying to the obstetrics and gynecology residency program at the same institution (from 2 applications prior to 11 applications after implementation of the program)17. A surgical program reported that 50% of the participants received a grade of honors during their surgical clerkship versus only 31.5% of non-participants (p value 0.05)23. A neurology specific mentoring program demonstrated an increase in the number of students entering neurology from an average of 2.8 per year to 7.5 per year34. A program for students interested in radiation oncology reported that over a 10-year period, they had 100% match rate for the students in the program compared to a national match rate of 85.1% additionally as an indicator of success, they reported that for each year more student participated with 3 students participating in the first year of the program and 11 students in the 10th year of the program18. A program for URM students within otolaryngology found that six of the seven students who applied to otolaryngology residency matched successfully and that the URM representation among residents at the host institution increased from 9% of the total residents prior to the program to 16% after the program21. Finally, one program for URM students tracked academic outcomes and found that the percent of URM students obtaining honors increased in three of the five required clerkships compared to prior to the initiation of the program36.
Table 1.
Program Evaluation Methods and Evaluation Results for Programs with Objective Outcomes
| Study, year | Program evaluation | Evaluation results |
|---|---|---|
| Nellis, 201621 |
Survey and retrospective review |
• Students rated the mentorship highly 4.85/5 • 7/15 students applied to otolaryngology residencies • 6/7 matched successfully • URM* representation among the residents at the host institution increased from 9% of the total residents before the program to 16% |
| Day, 201623 | Survey and retrospective review |
• 50% of participants received a grade of honors during their surgical clerkship vs. 31.5% non-participants (p value = 0.05) • Participants reported that their resident mentor strongly impacted their decision to pursue surgery |
| Sobbing, 201523 | Survey and retrospective review |
• Increase in the number of medical students applying to the residency program vs. prior to the program (2 to 11 applicants) • 56% reported receiving advice on personal development/support • 40% reported feeling well/extremely well connected with their mentor |
| Zuzarregui, 201534 | Retrospective review |
• Increase in the number of medical students entering neurology from an average of 2.8 per year to 7.5 per year (p value < 0.05) • Increased the number of medical student research projects, posters and publications vs. prior to the program from 7 to 22 (p value < 0.05) |
| Hirsch, 201518 | Retrospective review |
• 17/58 participants (29.3%) applied to and matched into radiation oncology (100% match rate) vs. national match rate of 85.1% (p value 0.14) • Over 10 years mentee research productivity: 53 publications, 75 national presentations, 10 national awards |
| Indyk, 201118 | Post-residency match survey and annual focus groups |
• For each year of the program, participants were more likely to match into primary care vs. non-participants (year 1 87.5% vs 55.8% and year 2 78.9% vs 35.9%) • 61.0% of participants reported that the mentor influenced their career • Themes from qualitative analysis: (1) impact on the understanding of primary care and (2) facilitators and inhibitors of the mentoring relationship |
| Johnson, 199836 | Retrospective review | • Percent of URM students obtaining honors increased for 3 of the 5 required third-year clerkships vs. prior to the program |
*Underrepresent minorities
Nineteen of the programs provided subjective outcome measures of success (Table 2). As is true of much of the mentorship literature39, the evaluations of the programs were largely measured by ratings of satisfaction. In general, the students rated the programs highly.
Table 2.
Program Evaluation Methods and Evaluation Results for Programs with Subjective Outcomes
| Study, year | Program evaluation | Evaluation results |
|---|---|---|
| Brueckner-Collins, 201825 | Survey |
• Participants provided positive comments • Noted that connections made with senior faculty mentors later helped advance their career |
| Andre, 201730 | Annual all-student survey |
• Year to year increase in satisfaction with medical school experience (p value < 0.0001) • 94.3% of students felt the groups and 4th year medical student mentors provided them with peer support |
| Maursetter, 201620 | Survey |
• Students rated the mentoring experience a mean of 7.1/10 • 70% had > 10 interactions with their mentor in a year • 41.6% increase in interest in a nephrology fellowship vs prior to participating |
| Khan, 201622 | Survey | • 80% of mentees felt that surgeons had a manageable lifestyle |
| DeFilippis, 201527 | Survey |
• 71% of participants ranked the program as 4 or 5/5 for satisfaction • 77% felt the program provided opportunities for mentorship • 82% felt it filled an institutional need |
| Weiner, 201438 | Survey |
• 28% of students used the database • 46% of participants felt it helped them identify a mentor |
| Stein, 201337 | Pre and post-survey |
• Increase in knowledge of child and adolescent psychiatry (p value < 0.01) • Increase in perception of mentorship for research guidance (p value < 0.05) • Increase in perception of mentorship for career guidance (p value < 0.05) • No change in desire to enter child or adolescent psychiatry |
| Kman, 201328 | Survey |
• Increase in the number of medical students who could identify a mentor vs prior to the program (77.6% vs 28%) • 70% had more interest in emergency medicine as a career vs. prior to participation |
| Drusin, 201319 | Survey |
• 79.5% of students met with their advisor at least once • 66.7% were satisfied with their advisor |
| Thomas-Squance, 201129 | Survey |
• 89% rated the program as valuable • 84% felt it was relevant to professional development • 54% valued meeting mentors |
| Oelschlager, 201124 | Survey |
• 48.1% reported that they had contact with the mentor once per quarter • 73% reported that their mentor was helpful/very helpful |
| Drolet, 201010* | Anecdotal evidence | • Students report satisfaction with the program |
| Fleming, 201311* | AAMC† Graduation Questionnaire | • Increase in satisfaction with faculty mentoring vs prior to the program 87.5% from 75.6% (p value 0.81) and career planning 82.9% from 67.5% (p value = 0.037) |
| Coates, 20082 | Internal survey and AAMC Graduation Questionnaire | • Compared to before the program: (1) increase in number of students who identified a career mentor vs prior to the program (73% vs 37%) and (2) increase in the number of students satisfied/very satisfied with faculty mentoring vs prior to the program (79.4% vs 58.1% vs 65.4% national average) |
| Macaulay, 200733 | Survey | • 89% of respondents reported the Advisor Dean program as valuable |
| Kosoko-Lasaki, 200635 | Survey |
• 89% agree that the mentoring program is effective • Medical students reported that mentors helped with their choice of residency programs |
| Coates, 200414 | Qualitative survey | • 67% of students offered positive comments about the program |
| Abernethy, 199931 | Survey |
• Students met with their mentor an average of 3 times per year • Student satisfaction with mentor mean rating 5.1 out of 7 |
| Flach, 198216 | Survey | • 63% of students were satisfied with their mentor |
*Drolet and Fleming articles represent the same program described in two separate papers; therefore, they have been listed together in the table
†Association of American Medical Colleges
Two programs used the Association of American Medical Colleges (AAMC) graduation questionnaire to help evaluate their programs and were able to track changes over time versus national averages. One institution, using the AAMC data, reported increases in satisfaction with both faculty mentoring from 75.6% prior to the program to 87.5% after the program and career planning from 67.5% prior to the program to 82.9%11. Another program reported that 79.4% of their students were satisfied/very satisfied with faculty mentoring compared to 58.1% of their students prior to the program and a national average of 65.4%2.
In general, the programs that were smaller and subspeciality specific provided more objective measures of success. Six15,17,18,21,23,34 of the 12 subspeciality programs offered objective outcomes measures whereas none of the subspeciality programs with greater than 100 participating students14,28,37 or the programs that enrolled all medical students in a school provided objective outcomes measures.
Program Cost
Many of the studies discussed the costs of these programs. For those that were part of an advisory dean/college programs, faculty salary support was a significant cost. One program listed faculty salary support as $500,000 per year with an additional $80,000 in other costs11. For another program, the Dean’s office provided 25% salary support to each of the mentors24. Other advisor dean/college programs report salary support of 15–20% for the main faculty32,33. Of note, these larger and more costly programs did not report on any objective outcomes measures of success, although one did provide some pre/post data that demonstrated an overall improvement in satisfaction with faculty mentorship and career planning11. Four of the programs were funded by external grants,15,28,35,37 one of which was a small grant of $500 from a national speciality organization that was matched by the department at the local institution28.
While several programs used students and/or residents as mentors, two specifically commented on the costs aspect of using more junior mentors. One program that used fourth year medical students as mentors commented that using students helped reduce costs30. A second program that relied on one faculty and one resident to oversee the program commented that each invested approximately 15 h per month on the program;34 therefore, having the resident effectively doubled the hours invested.
Barriers of Programs
Beyond costs, several of the papers described other barriers. Two articles cited faculty members’ busy schedules as barriers,19,27 while those that utilized residents and students as mentors noted competing demands and responsibilities17,30.
For mentoring programs that were aimed at URM students, the small number of URM faculty was reported as a barrier31,36. One program attempted to address this by utilizing non-URM faculty mentors31. Another program recruited URM physician mentors from local private practices12 in order to expand the number of possible mentors.
Some programs cited mentor skill development as a barrier. One program using residents as primary mentors reported that they often lacked optimal mentorship training17. Several programs included a variety of trainings aimed at improving mentorship quality24,31. Two programs provided mentors with written guidelines delineating mentorship roles14,28. One program offered an introductory training session for both mentors and mentees in which the objectives of the program were explained and expectations of both mentor and mentees were discussed25. Finally, one program reported that while there was no formal training, the mentors met monthly to discuss “best practices.”2
DISCUSSION
Our systematic review identified 30 separate articles describing 29 mentorship programs for medical students and demonstrated several important themes. The traditional dyad model of mentorship was used most commonly, which is consistent with previous literature6,39,40. The second most common model was a combination of dyad and group mentorship. Many of these programs described that group sessions were used to discuss broadly applicable issues and one-on-one sessions were used for the personal needs of the mentee. Given that both faculty time and salary support were commonly cited constraints, using a combination of mentorship models may reduce faculty time and associated costs by improving the efficiency of individual meetings. While there may be improvement in efficiency of mentorship, of the seven programs with objective measures of success five used exclusive dyad mentorship15,17,18,21,23 which suggests that the intensity of traditional dyad mentorship may result in more tangible measures of success.
Notably, none of the programs used a traditional peer model of mentorship. While some of the programs referenced peer mentoring28,30, these were not traditional peer mentoring programs in which two individuals at the same level of training provide mentorship to each other. Instead, these programs assigned fourth year students along with faculty and/or residents to help mentor more junior level students and applied a tiered model of mentorship to provide mentorship across academic positions. Other programs that used group mentoring commented that one benefit of group mentoring was that the students developed peer relationships, which could be used as a source of support27–29. The literature has documented that peer mentorship is occurring in medical schools,1 and it is likely that peer mentorship plays an important role in medical education, but it appears to be to an underutilized model in formal mentorship programs. This is in contrast to models of mentorship for physicians wherein peer models are more common39. Additionally, given that most of the associated costs were due to faculty salary support, further use of peer and/or senior student mentorship might help minimize this barrier to development of mentorship programs.
Mentorship of specific subsets of medical students (i.e., a certain race, ethnicity, gender, or clinical area of interest) emerged as a theme throughout our review with seven programs providing mentorship to URM students12,13,21,29,31,35,36, two programs to female students22,27, and 12 programs focusing specific clinical specialities14,15,17,18,20–23,25,28,34,37. It is well-established that individuals from some racial minorities remain underrepresented in medicine41,42. Additionally, mentorship programs may be a key factor in improving the recruitment and retention of URM physicians, as demonstrated by the success that one of the programs had at increasing the number of URM residents in their residency after the initiation of the mentorship program21. It was therefore surprising that the majority of these URM mentoring programs are over 10 years old12,13,31,35,36 and that there was a lack of more modern programs aimed at reducing the known disparities in URM physicians’ recruitment, promotion, and retention. Although the current literature does not assess whether improved mentorship of URM physicians may help reduce these disparities, this is an important area for future study.
Women also remain underrepresented in academic medicine, particularly in leadership positions and surgical fields43 and are less likely to have mentors compared to their male counterparts44,45. As such, the existence of mentorship programs for female students is notable. Of note, these programs used group mentorship27,28 to counteract the lack of senior female physicians serving as mentors. However, prior work has found that preference for gender concordance may be overstated40,46 and that preferences for other factors germane to the mentoring relationship such as shared career interest may matter more47. Additionally, there may be limitations to gender concordant mentoring. In fact, one program planned to no longer use female-only groups after receiving feedback from students that felt they were unable to find a mentor in the all women groups28. As gender roles continue to evolve in society, the importance of gender concordance may continue to decline. This may occur as more women assume leadership positions that have historically been more occupied by men, and more men gain experience with mentorship of women across the academic spectrum, including in fields that have traditionally had fewer women. Overall, the results of our review and others suggest that academic communities are making efforts to improve mentorship of women, and that a potential lack of senior female mentors should not be considered a barrier.
The lack of objective outcomes and comparison data is a common theme in the mentorship literature39 and makes it difficult to assess the long-term impact of these mentorship programs. Smaller programs that were developed for specific clinical interests were able to demonstrate objective outcomes based on recruitment, publications, or improved grades. For the remaining programs, the vast majority, including the larger and more costly programs, measured student satisfaction as the main outcome. While student satisfaction is important to measures of medical school quality and incorporated into evaluation tools from the AAMC Graduation Questionnaire and LCME, having objective outcomes data such as residency match data, board scores, or clinical evaluations would offer a more standard evaluation of success and possible help justify the cost of these programs. However, it is important to remember that many aspects of mentorship may not lend themselves to objective quantitative measures of success, and that even without objective outcomes, these programs are likely to have a positive impact on the participants.
While the cost of several of these programs was significant, the upfront investment may be justified if mentorship can help reduce burnout, given the significant cost of having to extend medical school training. It was therefore disappointing that despite three studies10,29,32 noting student wellness as an objective, these issues were not assessed as an outcome in any program. As medical student burnout continues to rise48, effective ways to improve wellness should be developed. While mentorship of physicians has been associated with career satisfaction and faculty retention3, to our knowledge, there is no data that looks of the impact of mentorship on medical student burnout. While it is unlikely that mentorship alone will reduce burnout without more comprehensive and systemic reforms, it may help improve factors associated with burnout including isolation and feelings of powerlessness. Future research to explore the use of mentoring to enhance student wellness would be a significant contribution to the mentorship literature and may help justify the cost of these large mentorship programs.
One possible limitation our paper is the subjective nature of mentorship, the variety of forms that mentorship can take, and its inherent potential for overlap with advising. While we applied our stated and previously published definition of mentorship to our search protocol, we are limited by the word choice that the authors of each manuscript choose to describe the programs and relationships between the students and proposed mentors. We do not feel that this potential limitation influenced our results, as the majority of our studies describe a similar definition of mentorship. Additionally, we limited our review to programs offered within the USA as the training structure in the USA is unique compared to other countries49. This is consistent with previous reviews on mentorship of physicians39 but may limit the generalizability of our results internationally. Another possible limitation is that additional data may exist which meet our inclusion criteria but was unable to be included if results were not stratified with medical student-specific data.
CONCLUSION
Our review describes a range of successful mentorship programs for medical students. The most common mentorship model is the dyad approach, which may also produce greater success in terms of measureable outcomes, while group mentorship may help to control cost of larger mentorship programs. Additionally, medical schools recognize the need for mentorship to help address the dearth of URM physicians in medicine as a whole, and the lack of women in specific fields and leadership positions. Smaller clinically focused programs are more likely to produce measurable results, while larger programs demonstrate that effective mentoring benefits students’ overall medical school experience and career development. Overall, our review has demonstrated that no clear best practices for medical student mentorship exist in the literature. One conclusion, therefore, is that institutions can individualize their mentorship programs and models to available resources and goals. Additionally, our results demonstrate the importance of further development and objective evaluation of medical student mentorship programs to more effectively enhance the experience and development of medical students across the spectrum.
Electronic Supplementary Material
(DOCX 48 kb)
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Pinilla S, Nicolai L, Gradel M, et al. Undergraduate Medical Students Using Facebook as a Peer-Mentoring Platform: A Mixed-Methods Study. JMIR Med Educ. 2015;1(2):e12. doi: 10.2196/mededu.5063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Coates WC, Crooks K, Slavin SJ, Guiton G, Wilkerson L. Medical school curricular reform: fourth-year colleges improve access to career mentoring and overall satisfaction. Acad Med. 2008;83(8):754–760. doi: 10.1097/ACM.0b013e31817eb7dc. [DOI] [PubMed] [Google Scholar]
- 3.Sambunjak D, Straus SE, Marusic A. Mentoring in academic medicine: a systematic review. JAMA. 2006;296(9):1103–1115. doi: 10.1001/jama.296.9.1103. [DOI] [PubMed] [Google Scholar]
- 4.Liasion Committee on Medical Education. Functions and Structure of a Medical School: Standards for Accrediation of Medical Education Programs Leading to the MD Degree. 2018; http://lcme.org/publications/. Accessed June 16, 2019
- 5.Aagaard EM, Hauer KE. A cross-sectional descriptive study of mentoring relationships formed by medical students. J Gen Intern Med. 2003;18(4):298–302. doi: 10.1046/j.1525-1497.2003.20334.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Frei E, Stamm M, Buddeberg-Fischer B. Mentoring programs for medical students--a review of the PubMed literature 2000-2008. BMC Med Educ. 2010;10:32. doi: 10.1186/1472-6920-10-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Buddeberg-Fischer B, Herta KD. Formal mentoring programmes for medical students and doctors--a review of the Medline literature. Med Teach. 2006;28(3):248–257. doi: 10.1080/01421590500313043. [DOI] [PubMed] [Google Scholar]
- 8.Association of American Medical Colleges. Results of the 2017 Medical School Enrollment Survey; Washington, DC; 2018. https://store.aamc.org/downloadable/download/sample/sample_id/183/
- 9.Beech BM, Calles-Escandon J, Hairston KG, Langdon SE, Latham-Sadler BA, Bell RA. Mentoring programs for underrepresented minority faculty in academic medical centers: a systematic review of the literature. Acad Med. 2013;88(4):541–549. doi: 10.1097/ACM.0b013e31828589e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Drolet BC, Rodgers S. A comprehensive medical student wellness program--design and implementation at Vanderbilt School of Medicine. Acad Med. 2010;85(1):103–110. doi: 10.1097/ACM.0b013e3181c46963. [DOI] [PubMed] [Google Scholar]
- 11.Fleming A, Cutrer W, Moutsios S, et al. Building learning communities: evolution of the colleges at Vanderbilt University School of Medicine. Acad Med. 2013;88(9):1246–1251. doi: 10.1097/ACM.0b013e31829f8e2a. [DOI] [PubMed] [Google Scholar]
- 12.Peterson SE, Carlson P. A mentorship program for minority students. Acad Med. 1992;67(8):521. doi: 10.1097/00001888-199208000-00009. [DOI] [PubMed] [Google Scholar]
- 13.Cregler LL. A second minority mentorship program. Acad Med. 1993;68(2):148. doi: 10.1097/00001888-199302000-00010. [DOI] [PubMed] [Google Scholar]
- 14.Coates WC, Ankel F, Birnbaum A, et al. The virtual advisor program: linking students to mentors via the world wide web. Acad Emerg Med. 2004;11(3):253–255. doi: 10.1111/j.1553-2712.2004.tb02205.x. [DOI] [PubMed] [Google Scholar]
- 15.Indyk D, Deen D, Fornari A, Santos MT, Lu WH, Rucker L. The influence of longitudinal mentoring on medical student selection of primary care residencies. BMC Med Educ. 2011;11:27. doi: 10.1186/1472-6920-11-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Flach DH, Smith MF, Smith WG, Glasser ML. Faculty mentors for medical students. J Med Educ. 1982;57(7):514–520. doi: 10.1097/00001888-198207000-00002. [DOI] [PubMed] [Google Scholar]
- 17.Sobbing J, Duong J, Dong F, Grainger D. Residents as Medical Student Mentors During an Obstetrics and Gynecology Clerkship. J Grad Med Educ. 2015;7(3):412–416. doi: 10.4300/JGME-D-14-00667.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hirsch AE, Agarwal A, Rand AE, et al. Medical student mentorship in radiation oncology at a single academic institution: A 10-year analysis. Pract Radiat Oncol. 2015;5(3):e163–168. doi: 10.1016/j.prro.2014.08.005. [DOI] [PubMed] [Google Scholar]
- 19.Drusin LM, Gerber LM, Miller CH, Storey-Johnson CL, Ballard BL. An advisory program for first- and second-year medical students: the Weill Cornell experience. Med Educ Online. 2013;18:22684. doi: 10.3402/meo.v18i0.22684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Maursetter LJ, Stern LD, Sozio SM, et al. Enhancing Nephrology Career Interest through the ASN Kidney TREKS Program. J Am Soc Nephrol. 2016;27(6):1604–1607. doi: 10.1681/ASN.2015101086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nellis JC, Eisele DW, Francis HW, Hillel AT, Lin SY. Impact of a mentored student clerkship on underrepresented minority diversity in otolaryngology-head and neck surgery. Laryngoscope. 2016;126(12):2684–2688. doi: 10.1002/lary.25992. [DOI] [PubMed] [Google Scholar]
- 22.Khan S, Ferrada P. Empowering Surgical Residents as Mentors: A Pilot Program for Female Medical Students. Am Surg. 2016;82(11):313–314. [PubMed] [Google Scholar]
- 23.Day KM, Schwartz TM, Rao V, et al. Medical student clerkship performance and career selection after a junior medical student surgical mentorship program. Am J Surg. 2016;211(2):431–436. doi: 10.1016/j.amjsurg.2015.10.007. [DOI] [PubMed] [Google Scholar]
- 24.Oelschlager AM, Smith S, Tamura G, Carline J, Dobie S. Where do medical students turn? The role of the assigned mentor in the fabric of support during medical school. Teach Learn Med. 2011;23(2):112–117. doi: 10.1080/10401334.2011.561664. [DOI] [PubMed] [Google Scholar]
- 25.Brueckner-Collins JK, Stratton TD, Conigliaro RL. Inspiring the next generation of academic physicians: the academic health careers program. Med Educ online. 2018;23(1):1530559. doi: 10.1080/10872981.2018.1530559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kalet A, Krackov S, Rey M. Mentoring for a new era. Acad Med. 2002;77(11):1171–1172. doi: 10.1097/00001888-200211000-00041. [DOI] [PubMed] [Google Scholar]
- 27.DeFilippis E, Cowell E, Rufin M, Sansone S, Kang Y. Innovative mentoring for female medical students. Clin Teach. 2016;13(5):381–382. doi: 10.1111/tct.12408. [DOI] [PubMed] [Google Scholar]
- 28.Kman NE, Bernard AW, Khandelwal S, Nagel RW, Martin DR. A tiered mentorship program improves number of students with an identified mentor. Teach Learn Med. 2013;25(4):319–325. doi: 10.1080/10401334.2013.827976. [DOI] [PubMed] [Google Scholar]
- 29.Thomas-Squance GR, Goldstone R, Martinez A, Flowers LK. Mentoring of students from under-represented groups using emotionally competent processes and content. Med Educ. 2011;45(11):1153–1154. doi: 10.1111/j.1365-2923.2011.04133.x. [DOI] [PubMed] [Google Scholar]
- 30.Andre C, Deerin J, Leykum L. Students helping students: vertical peer mentoring to enhance the medical school experience. BMC Res Note. 2017;10(1):176. doi: 10.1186/s13104-017-2498-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Abernethy AD. A mentoring program for underrepresented-minority students at the University of Rochester School of Medicine. Acad Med. 1999;74(4):356–359. doi: 10.1097/00001888-199904000-00023. [DOI] [PubMed] [Google Scholar]
- 32.Murr AH, Miller C, Papadakis M. Mentorship through advisory colleges. Acad Med. 2002;77(11):1172–1173. doi: 10.1097/00001888-200211000-00042. [DOI] [PubMed] [Google Scholar]
- 33.Macaulay W, Mellman LA, Quest DO, Nichols GL, Haddad J, Jr, Puchner PJ. The advisory dean program: a personalized approach to academic and career advising for medical students. Acad Med. 2007;82(7):718–722. doi: 10.1097/ACM.0b013e3180674af2. [DOI] [PubMed] [Google Scholar]
- 34.Zuzuarregui JR, Hohler AD. Comprehensive Opportunities for Research and Teaching Experience (CORTEX): A mentorship program. Neurology. 2015;84(23):2372–2376. doi: 10.1212/WNL.0000000000001663. [DOI] [PubMed] [Google Scholar]
- 35.Kosoko LO, Sonnino RE, Voytko ML. Mentoring for women and underrepresented minority faculty and students: experience at two institutions of higher education. J Natl Med Assoc. 2006;98(9):1449–1459. [PMC free article] [PubMed] [Google Scholar]
- 36.Johnson JC, Jayadevappa R, Taylor L, Askew A, Williams B, Johnson B. Extending the pipeline for minority physicians: a comprehensive program for minority faculty development. Acad Med. 1998;73(3):237–244. doi: 10.1097/00001888-199803000-00011. [DOI] [PubMed] [Google Scholar]
- 37.Stein JA, Althoff R, Anders T, et al. Does early mentorship in child and adolescent psychiatry make a difference? The Klingenstein Third-Generation Foundation Medical Student Fellowship Program. Acad Psychiatry. 2013;37(5):321–324. doi: 10.1176/appi.ap.12070136. [DOI] [PubMed] [Google Scholar]
- 38.Weiner J, Small AC, Lipton LR, et al. Establishing an online mentor database for medical students. Med Educ. 2014;48(5):542–543. doi: 10.1111/medu.12458. [DOI] [PubMed] [Google Scholar]
- 39.Kashiwagi DT, Varkey P, Cook DA. Mentoring programs for physicians in academic medicine: a systematic review. Acad Med. 2013;88(7):1029–1037. doi: 10.1097/ACM.0b013e318294f368. [DOI] [PubMed] [Google Scholar]
- 40.Farkas AH TR, Bonifacino E, Tilstra SA, Corbelli JA. Mentoring Women in Academic Medicine: A Systematic Review. In. Abstract presented at the Society of General Internal Medicine National Meeting, Denver CO, 2018.
- 41.Nivet MA, Castillo-Page L. Diversity in the Physician Workforce: Facts & Figures. Association of the American Medical Colleges; Washington, DC; 2014. http://www.aamcdiversityfactsandfigures.org/ [DOI] [PubMed]
- 42.Association of American Medical Colleges . Altering the Course: Black Males in Medicine. Washington D.C.: Association of American Medical Colleges; 2015. [Google Scholar]
- 43.Lautenberge D, Dandar, VM., Raezer, CL., Sloane, RA. The State of Women in Academic Medicine: The Pipeline and Pathways to Leadership. Association of American Medical Colleges; Washington, DC; 2014.
- 44.Osborn EH, Ernster VL, Martin JB. Women's attitudes toward careers in academic medicine at the University of California, San Francisco. Acad Med. 1992;67(1):59–62. doi: 10.1097/00001888-199201000-00012. [DOI] [PubMed] [Google Scholar]
- 45.Stamm M, Buddeberg-Fischer B. The impact of mentoring during postgraduate training on doctors’ career success. Med Educ. 2011;45(5):488–496. doi: 10.1111/j.1365-2923.2010.03857.x. [DOI] [PubMed] [Google Scholar]
- 46.DeCastro R, Griffith KA, Ubel PA, Stewart A, Jagsi R. Mentoring and the career satisfaction of male and female academic medical faculty. Acad Med. 2014;89(2):301–311. doi: 10.1097/ACM.0000000000000109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Carapinha R, Ortiz-Walters R, McCracken CM, Hill EV, Reede JY. Variability in Women Faculty’s Preferences Regarding Mentor Similarity: A Multi-Institution Study in Academic Medicine. Acad Med. 2016;91(8):1108–1118. doi: 10.1097/ACM.0000000000001284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dyrbye LN, West CP, Satele D, et al. Burnout among U.S. medical students, residents, and early career physicians relative to the general U.S. population. Acad Med. 2014;89(3):443–451. doi: 10.1097/ACM.0000000000000134. [DOI] [PubMed] [Google Scholar]
- 49.Weggemans MM, van Dijk B, van Dooijeweert B, Veenendaal AG, ten Cate O. The postgraduate medical education pathway: an international comparison. GMS J Med Educ. 2017;34(5):Doc63. doi: 10.3205/zma001140. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 48 kb)