Abstract
Spontaneous onset pneumomediastinum, pneumothorax and subcutaneous emphysema are rare presentations of a foreign body in the airway. The possible mechanism for unexplainable and non traumatic subcutaneous emphysema can be attributed to “Air leak syndrome” following inhalation of foreign body in the airway.
Keywords: Foreign body bronchus, Foreign body airway, Foreign body unusual presentation, Subcutaneous emphysema foreign body bronchus
Introduction
Foreign body (FB) in the airway is a common cause of respiratory complaints in children. Initial symptoms are choking, gagging, transient aphonia, coughing and wheezing, often followed by a symptomless interval. Pneumomediastinum, pneumothorax and subcutaneous emphysema are uncommon presentations of FB in the airway. Only a very few cases have been reported till date [1–3].
Case Report
A two and half year old female child was brought to the hospital emergency service with history of respiratory distress, fever and cough for last 3 days and swelling over the neck and chest since last 1 day. There was no history suggestive of FB aspiration like choking, gagging or coughing bouts. Also there was no history suggestive of recent trauma, intubation or any infective pathology.
On examination, the child was conscious, irritable, febrile and tachypnoeic. There was diffuse swelling over the lower face, neck, anterior chest and abdomen with subcutaneous crepitus. Auscultation revealed diminished breath sounds in the right sided lung. There were no intercostal retractions or utilisation of accessory muscles of respiration.
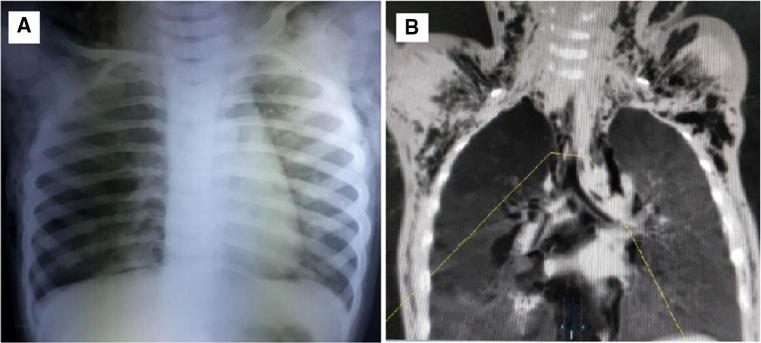
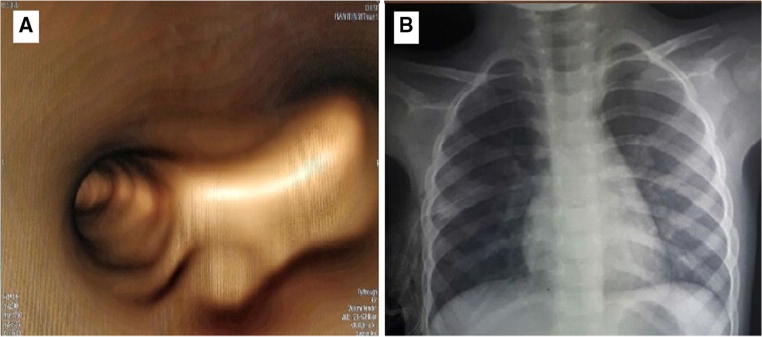
Her chest X-ray revealed hyperlucency of right lung and subcutaneous emphysema along the bilateral chest walls, axilla and supraclavicular areas (Fig. 1a). Computed tomography of neck and thorax showed diffuse subcutaneous emphysema, pneumomediastinum and mild right pneumothorax with areas of consolidation and atelectasis in the right lower lobe (Fig. 1b). A virtual bronchoscopy was done which revealed an abrupt cut off of right main bronchus that represented intrabronchial lesion, most likely foreign body (Fig. 2a). An intercostal drain was inserted to decompress the pneumothorax.
Fig. 1.
a Chest X-ray revealing hyperlucency of the right lung and subcutaneous emphysema along the bilateral chest walls, axilla and supraclavicular areas. b CECT scan of neck and thorax revealing diffuse subcutaneous emphysema, pneumomediastinum and mild right pneumothorax
Fig. 2.
a Virtual bronchoscopy showing an abrupt cut off of right main bronchus suggestive of intrabronchial foreign body. b Postoperative chest X-ray depicting normal lucency of the right lung and resolution of the subcutaneous emphysema
A rigid bronchoscopy under general anaesthesia with intermittent positive pressure ventilation (IPPV) was done with paediatric surgery backup in the operating room that revealed a vegetative FB (peanut) in the right main bronchus. After the FB was removed with a forceps, there was evidence of minimal pus just distal to the site of lodgement. There was no obvious erosion or discontinuity of the walls of the airway. Rest of the distal airway appeared normal.
Intravenous antibiotics and bronchodilators were continued postoperatively. A chest X-ray was repeated after 24 h that showed normal lucency of the right lung and resolution of the subcutaneous emphysema (Fig. 2a). The child showed gradual symptomatic improvement and good lung expansion. She was discharged after 5 days of hospital stay and was advised regular follow up.
Discussion
FB in the airway is a common pediatric emergency, especially in children less than 3 years. The FB in the airway can either be endogenous like vomitus or a tooth or exogenous like a vegetative particle or metallic objects. The children are vulnerable to aspiration of foreign bodies into the airway due to difficulty in swallowing hard foodstuff and inadequately developed protective respiratory reflexes [4]. The one drawback of these protective respiratory reflexes is the impulse to take a deep inspiration preparatory to the cough initiated by the contact of a FB that promotes aspiration.
Initial symptoms of FB in the bronchus are cough bouts, choking and gagging. However, these symptoms might not be reported in all the cases as the children might have experienced them in the absence of their parents. These initial symptoms may be followed by a symptomless phase for few days to weeks. In some cases, this may last a few hours, especially in vegetative FB that swells up gradually leading to complications. Air leak syndrome, comprising pneumothorax, pneumomediastinum, and subcutaneous emphysema, is seen in 1–2% of cases; and 25% of cases may remain asymptomatic for long periods [5, 6]. The exact mechanism for the cause of air leak in case of FB in airway is unknown. However two mechanisms have been put forward to explain the air leak leading to development of pneumothorax, pneumomediastinum, and subcutaneous emphysema.
The first mechanism is that the FB in airway tends to behave as a “one-way valve” that allows the air to enter but not exit out of the affected part of the lung causing air trapping, thereby gradually increasing the distal volume and pressure. This leads to formation of a sufficient pressure gradient across the alveoli leading to rupture of the alveolar membrane through which the air travels along the blood vessels to the mediastinum [7, 8].
The second mechanism is related to the mechanical disruption of the mucosal membrane of bronchus or airway through which air enters in the tissue under pressure. During the cough or respiratory strain, high pressure gradient is generated which tends to push the air through disrupted mucosal membrane which then travels along the perivascular and peribronchial interstitial tissue to the mediastinum leading to pneumomediastinum [9].
Air in the mediastinum tends to migrate to the subcutaneous tissue under pressure gradient through a peculiar arrangement of fascial planes in the neck, chest and abdomen which leads to the development of subcutaneous emphysema [8]. Coughing, high airway pressure, valsalva maneuver, positive end expiratory pressure (PEEP) etc. are the risk factors for subcutaneous emphysema [10].
Conclusion
In conclusion, our case showed that although subcutaneous emphysema, pneumomediastinum and pneumothorax are rare presentations of FB in the airway, a high index of suspicion should be maintained in a child with unequal air entry and a rigid bronchoscopy should be considered to rule out a foreign body in a child presenting with the same.
Compliance with Ethical Standards
Conflict of interest
All authors declare that they have no conflict of interest.
Human and Animal Rights
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed Consent
Informed consent for publication was obtained from the family member of the subject included in the case.
References
- 1.Narasimhan KL, Chowdhary SK, Suri S, Mahajan JK, Samujh R, Rao KL. Foreign body airway obstruction in children: lessons learnt from a prospective audit. J Indian Assoc Pediatr Surg. 2002;7:184–189. [Google Scholar]
- 2.Mehta AK, Sarin D. Subcutaneus emphysema: an unusual presentation of foreign body bronchus. Med J Armed Forces India. 2007;63:71–72. doi: 10.1016/S0377-1237(07)80117-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ramadan HH, Bu-Saba N, Baraka A, Mroueh S. Management of an unusual presentation of foreign body aspiration. J Laryngol Otol. 1992;106:751–752. doi: 10.1017/S0022215100120791. [DOI] [PubMed] [Google Scholar]
- 4.David SS, Subbiah B. Foreign bodies in the air and food passages in children. Indian Paediatr. 1973;10:183–185. [PubMed] [Google Scholar]
- 5.Wolach B, Raz A, Weinberg J, et al. Aspirated foreign bodies in respiratory tract of children-11 years experience with 127 patients. Int J Pediatr Otolaryngol. 1994;30:1–10. doi: 10.1016/0165-5876(94)90045-0. [DOI] [PubMed] [Google Scholar]
- 6.Svedstorm E, Puhakka H, Kero P. How accurate is chest radiography in the diagnosis of tracheobronchial foreign bodies in children? Pediatr Radiol. 1989;19:520–522. doi: 10.1007/BF02389562. [DOI] [PubMed] [Google Scholar]
- 7.Maunder RJ, Pierson DJ, Hudson LD. Subcutaneous and mediastinal emphysema. Pathophysiology, diagnosis, and management. Arch Intern Med. 1984;144:1447–1453. doi: 10.1001/archinte.1984.00350190143024. [DOI] [PubMed] [Google Scholar]
- 8.Saoji R, Ramchandra C, D’Cruz AJ. Subcutaneous emphysema: an unusual presentation of foreign body in the airway. J Pediatr Surg. 1995;30:860–862. doi: 10.1016/0022-3468(95)90765-3. [DOI] [PubMed] [Google Scholar]
- 9.Waldhausen JA, Pierce WS. Johnson’s surgery of the chest. Chicago: Year Book Medical Publishers Inc; 1985. pp. 6–7. [Google Scholar]
- 10.Wong DT, McGuire GP. Subcutaneous emphysema following trans-cricothyroid membrane injection of local anesthetic. Can J Anaesth. 2000;47:165–168. doi: 10.1007/BF03018854. [DOI] [PubMed] [Google Scholar]