Abstract
Functional endoscopic sinus surgery is the mainstay of surgical management of nasal polyposis since 1975. The decision between the partial resection and preservation of the middle turbinate (MT) has stirred up considerable debate. Partial MTR permits easy access to the affected paranasal sinuses intraoperatively and postoperatively. However, there may be alteration of nasal function, frontal sinusitis and anosmia. Preservation of middle turbinate is precludes these complications, and allows the MT to serve as a vital anatomical landmark for revision surgery. Therefore, our study compared the outcomes of the two approaches to aid surgeons in deciding the best possible approach. Randomized control trial. 31 patients (60 sides of nasal cavity) with nasal polyposis were divided into two groups. Group I consisted of 30 sides of nasal cavity with middle turbinate resection, while group II consisted of 30 sides of nasal cavity without middle turbinate resection. Both the groups were compared postoperatively for 6 months. In group I and group II, 5 sides (16.6%) and 11 sides (36.6%) showed polypoidal changes respectively. 3 sides (10%) in group I and 8 sides (26.6%) in group II showed blockage of maxillary sinus ostia. All the sides in group I had patency of frontal sinus. In group II, 5 sides (16.6%) showed blockage of frontal sinus ostia. The maxillary antrostomy patency in group I and group II were 90% (27) and 73.33% (22) respectively. Assessment of symptomatic improvements for nasal obstruction, hyposmia, headache and rhinorrhoea was done using questionnaires. Symptomatic improvement was higher in group I compared to group II with statistical significance (p = 0.001). Our study demonstrated that partial resection of middle turbinate decreased the chances of recurrence of disease and post-operative complications and resulted in significantly better symptomatic improvements.
Keywords: Nasal polyposis, Middle turbinate, Functional endoscopic sinus surgery
Introduction
Nasal polyposis is the outcome of chronic inflammatory reaction of nose and paranasal sinus mucosa. It has a worldwide prevalence of 2% [1]. It is associated with inflammatory conditions like perennial allergic rhinitis, asthma, intolerance to acetyl salicylic acid, allergic fungal rhinosinusitis, cystic fibrosis and primary ciliary dyskinesia [1]. Both medical and surgical management are advocated for nasal polyposis. Medical management entails administration of systemic steroids. When this route fails, functional endoscopic sinus surgery (FESS) is recommended. FESS can be performed with or without partial middle turbinate resection (pMTR). Some surgeons advise performing pMTR for improved intraoperative access, decreased synechiae formation and better postoperative drug delivery [2, 3]. This view is opposed by those who recommend preservation of middle turbinate to avoid chance of complications of MTR such as atrophic rhinitis, iatrogenic frontal sinusitis, and anosmia [2]. As is mentioned, considerable evidence exists to support each view. Turning to scientific literature does not prove helpful, as limited studies provide a concrete scientific rationale for either method, further most available studies are based on retrospective non-randomised data [2–6]. The present study addressed these limitations with its randomised control design. Taking disease recurrence and postoperative symptomatic improvement as the evaluating criteria, the present study compared the outcome of partial resection of middle turbinate with its preservation in FESS.
Materials and Methods
We conducted the study at Vardhman Mahavir Medical College and Safdarjung Hospital, New Delhi, on 31 patients of primary cases of nasal polyposis, from July 2014 to January 2016. Adult patients, suffering from unilateral or bilateral nasal polyposis, not responding to medical treatment were included in the study. The patients were randomized by chit method with replacement. A total 60 sides of nasal cavity were divided into two groups with 30 sides each. Group I comprised FESS with partial middle turbinate resection (pMTR) and group II comprised FESS without MTR. Preoperatively, each patient completed a questionnaire to elicit severity of symptoms which were nasal obstruction, headache, hyposmia and rhinorrhoea. Disease severity was scored pre-operatively and post-operatively using the following criteria:
0-No complaints,
1-Mild,
2-Moderate,
3-Severe,
4-Intolerable [7].
Patients were followed up at the end of 1st, 2nd, 3rd, 12th and 24th weeks. The disease severity score was observed to improve by at least two ranks and hence, the outcome was considered successful. Endoscopic grading of nasal polyposis was done pre and postoperatively according to Meltzer et al. [8].
The grading was as follows:
Grade 0—no visible nasal polyposis,
Grade I—small amount of polypoid disease confined within the middle meatus,
Grade II—multiple polyps occupying the middle meatus,
Grade III—polyp extending beyond middle meatus,
Grade IV—polyps completely obstructing the nasal cavity [8].
Only those cases of nasal polyposis meeting endoscopic criteria of grades III & IV were considered for surgery. All patients underwent a pre-op non-contrast computerised tomographic scan of nose and paranasal sinuses and were categorized according to Kennedy CT grading system which follows:
Stage I—opacity of a single sinus or bilateral opacity limited to middle meati,
Stage II—opacity of both middle meati and one adjacent sinus,
Stage III—bilateral ethmoidal opacity with involvement of one or two adjacent sinuses,
Stage IV—diffuse opacity of all the paranasal sinuses [4].
To achieve near identical disease involvement between two groups, only Kennedy grades III and IV were included in the study.
All the cases in the study underwent functional endoscopic sinus surgery (FESS) under local or general anaesthesia. In group I, the anterior two-thirds of the middle turbinate preserving ground lamella was resected. Postoperatively, both groups were given antibiotics, anti-histaminics, saline nasal spray and non-steroidal anti-inflammatory drugs for seven days. Alkaline nasal douching and oral steroids were also given. Oral prednisolone was administrated within 48 h of surgery at a dose of 0.4 mg/kg per day for 4 days. The dose was decreased by 0.1 mg/kg per day for 4 days until a dose of 20 mg/day was reached. After maintaining stage 0 nasal mucosa at a dose of 0.2 mg/kg per day for 4 months, prednisolone was reduced to 0.1 mg/kg per day. If stage 0 nasal mucosa was maintained for additional 2 months, prednisolone was tapered to zero [9].
At each follow up, the partially resected middle turbinate, its lateralization, medialization, central position, recurrence of polyposis, patency of maxillary and frontal sinuses and synechiae formation were assessed endoscopically. Subjective improvement was assessed by enquiring about symptoms of nasal obstruction, headache, hyposmia and rhinorrhoea. Both the objective and subjective improvements of group I and group II were compared pre and post-operatively. There were no intraoperative complications.
The statistical analysis was done in SPSS v 21.0. The qualitative data was analysed using Chi square test. Differences were considered significant when p < 0.05.
Results
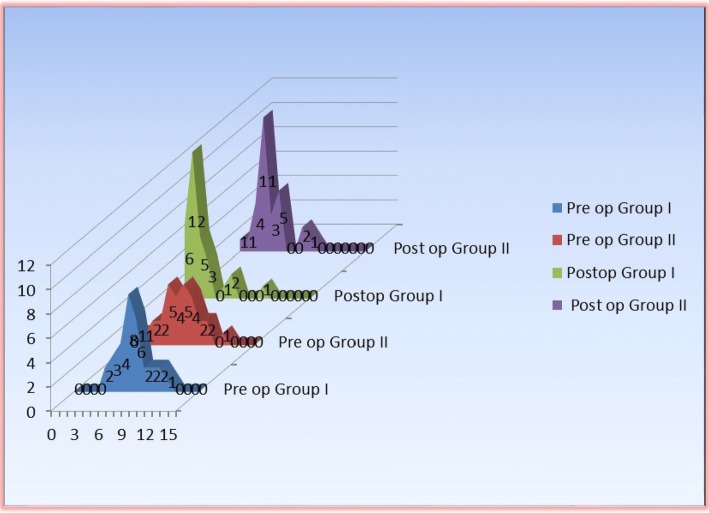
A total of 31 patients (60 sides of nasal cavity) who met the inclusion criteria were enrolled for the study. Pre-operatively most cases had endoscopic grade III nasal polyposis which was 66.67% (n = 20) and 63.33% (n = 19) in group I and group II respectively. Both the groups improved postoperatively, with group I showing 83.33% (n = 25) and group II 63.33% (n = 19) grade 0 nasal mucosa at the end of 6 months follow up (p = 0.161) (Table 1, Figs. 1, 2).
Table 1.
Pre and postoperative polyp grade in Group I and Group II
| Polyp grade | Pre-op | Post-op | ||||||
|---|---|---|---|---|---|---|---|---|
| Group I (%) | Group II (%) | Group I | Group II | |||||
| 4 weeks (%) | 3 months (%) | 6 months (%) | 4 weeks (%) | 3 months (%) | 6 months (%) | |||
| 0 | – | – | 86.67 | 83.33 | 83.33 | 66.67 | 63.33 | 63.33 |
| I | – | – | 13.33 | 3.33 | 0.00 | 33.33 | 6.67 | 3.33 |
| II | 3.33 | 10.00 | – | 13.33 | 16.67 | – | 26.67 | 23.33 |
| III | 66.67 | 63.33 | – | 0.00 | 0.00 | – | 3.33 | 10.00 |
| IV | 30.00 | 26.67 | – | – | – | – | – | – |
Fig. 1.
Pre and Post operative disease severity score in Group I and Group II
Fig. 2.
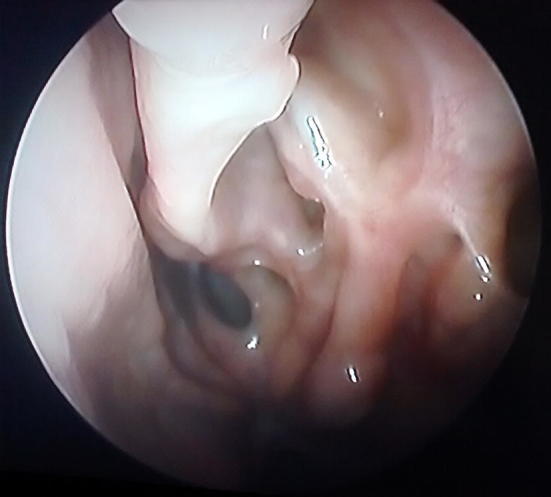
Postoperative endoscopic picture showing no evidence of polyp in a case of group I at the end of 6 months follow up
On comparing post-op patency of frontal and maxillary sinus ostia in both groups, we found that all (100%; n = 30) sides in group I (pMTR) had patency of frontal sinus ostia whereas only 83.33% (n = 25) sides of group II (without MTR) had patent frontal sinus ostia at the end of 6 months follow up (Table 2). This was statistically significant (p = .052). Maxillary antrostomy patency was 90% (n = 27) and 73.33% (n = 22) in group I and II respectively (p = 0.181).
Table 2.
Post-operative maxillary and frontal sinus ostial patency in Group I and Group II
| Post-operative sinus ostial patency | Group I | Group II | ||||
|---|---|---|---|---|---|---|
| 4 weeks (%) | 3 months (%) | 6 months (%) | 4 weeks (%) | 3 months (%) | 6 months (%) | |
| Maxillary | ||||||
| Absent | 0.00 | 10.00 | 10.00 | 6.67 | 26.67 | 26.67 |
| Present | 30.00 | 90.00 | 90.00 | 93.33 | 73.33 | 73.33 |
| Frontal | ||||||
| Absent | 0.00 | 0.00 | 0.00 | 3.33 | 16.67 | 16.67 |
| Present | 100.00 | 100.00 | 100.00 | 96.67 | 83.33 | 83.33 |
We found that 73.33% (n = 22) sides of group II showed central MT with 26.67% (n = 8) sides with lateralized or medialized MT. However all the sides in group I (100%; n = 30) had a central MT stump at end of 6 months follow up (p = 0.010) (Table 3).
Table 3.
Middle turbinate (MT) stump/middle turbinate in Group I and Group II
| MT stump/MT at the end of 6 months | Group I (%) | Group II (%) |
|---|---|---|
| Central | 100 | 73.33 |
| Lateralized | 0 | 23.33 |
| Medialized | 0 | 3.33 |
The disease severity score was computed for each individual side of nasal cavity using questionnaire method with the four variables. Preoperatively, the maximum number of sides (n = 8; 26.67%) in group I had disease severity score 7. Whereas in group II, most sides (n = 5; 16.67%) showed disease severity score either 5 or 7. Successful outcome was defined as improvement of disease severity score in at least two ranking systems. Disease severity score improved in both the groups (Tables 4, 5). There was aggravation of symptoms in three sides in group II (without MTR). The disease severity score improvement was found significantly more in group I (pMTR) in comparison to group II (p = 0.001) (Fig. 3). There were no major intraoperative complications such as haemorrhage needing blood transfusion, CSF leak, orbital injury or postoperative frontal sinus ostial stenosis in either group. However, in group I, one side (3.33%) and group II, 6 sides (20.00%) had synechiae.
Table 4.
Pre operative disease severity score in Group I and Group II
| Group I | Group II | p value | |
|---|---|---|---|
| Pre-operative disease severity score | |||
| Mean ± SD | 7.43 ± 2.01 | 6.57 ± 2.84 | 0.18 |
| Median | 7 | 6.5 | |
| Min–max | 4–12 | 1–14 | |
| Inter quartile range | 6–8 | 5–8 | |
Table 5.
Post-operative disease severity score in Group I and Group II
| Post-operative disease severity score | Group I | Group II | p value | |
|---|---|---|---|---|
| 4 weeks | Mean ± SD | 1.77 ± 1.3 | 3.03 ± 2.7 | 0.088 |
| Median | 1.5 | 2 | ||
| Min–max | 0–6 | 0–9 | ||
| Inter quartile range | 1–2 | 1–4 | ||
| 3 months | Mean ± SD | 1.23 ± 0.94 | 3.03 ± 2.72 | 0.004 |
| Median | 1 | 2 | ||
| Min–max | 0–3 | 0–10 | ||
| Inter quartile range | 1–2 | 1–5 | ||
| 6 months | Mean ± SD | 1.93 ± 2.23 | 4.47 ± 3.47 | < .0005 |
| Median | 1 | 3 | ||
| Min–max | 0–10 | 0–15 | ||
| Inter quartile range | 1–2 | 3–5 |
Fig. 3.

Postoperative endoscopic picture showing polypoidal mucosa in a case of group II at the end of 6 months follow up
Discussion
A large number of clinical studies have been conducted to determine the efficacy of middle turbinate (MT) resection in FESS. Middle turbinate resection is performed in patients having extensive polypoidal disease with additional comorbidities like asthma and aspirin intolerance [6]. Our study was conducted as a randomized control trial in patients having near identical severity of disease burden based on clinical, radiologic and endoscopic features.
The recurrence of nasal polyposis which is a commonly encountered scenario in clinical practice may occur up to 40–90% of cases [10, 11]. Anterior part of middle turbinate has been found to be an important area in secretion of vasoactive neuropeptides which predispose mucosal edema and polyp formation. The unmyelinated sensory fibres in nasal mucosa secretes neuropeptides, calcitonin gene related peptides, substance P and neurokinin A. Mechanical or contact stimulation of anterior part of middle turbinate mucosa provokes secretion of these substances [12]. Patients with chronic non allergic rhinosinusitis have a two fold increase in calcitonin gene related peptide in their middle turbinate mucosa [13]. Partial MTR facilitates drug delivery to frontal and sphenoid sinuses postoperatively, thus decreasing formation of polypoidal mucosa [3]. It has been described that the interval to revision surgery is longer in patients who underwent FESS with MTR [10]. In our study, endoscopic grade 0 mucosa was found more in group I (83.33%; n = 25) than group II (63.33%; n = 19). The result was not statistically significant (p = 0.161). This may be attributed to smaller sample size coupled with 6 months duration of follow up.
It has been described that there is 10% chance frontal sinusitis following MTR [14]. In our study, the 30 (100%) resected sides of group I showed central middle turbinate stump not obscuring frontal recess area with 100% patency of frontal sinus ostia. In group II only 83.33% (n = 25) sides that showed frontal sinus patency with lateralized or medialized MT (26.67%; n = 8). Adhesion formation occurs when two raw mucosal surfaces approximate with each other. The space of frontal recess widened and it is unlikely to form adhesion following MTR. Thus frontal sinusitis following FESS is a consequence of disease process of inflammatory nasal mucosa, not due to middle turbinate resection.
Middle turbinate acts as important anatomical landmark in functional endoscopic sinus surgery. Partial antero-inferior resection of middle turbinate leaves behind the bulk of middle turbinate as useful anatomical landmark [15].
In group I there was maxillary sinus antrostomy patency in 90.00% (n = 27) sides and in group II this was 73.33% (n = 22). Our findings were comparable to Davis et al. and Biedlingmaier et al. who reported 92–96% chance of maxillary antrostomy patency with resection of middle turbinate [15, 16]. Similarly Lamear et al. [14] reported middle meatal antrostomy patency of 92.5% after partial resection of middle turbinate. Scangas et al. [2] also concluded improved sinonasal passages with resection of MT. We believe that both frontal and middle meatal antrostomy patency improve with pMTR.
Postoperatively at the end of 6 months follow up, nasal obstruction was seen in 43.33% (n = 13) sides of group I and 6.67% (n = 2) sides of group II. None of the side of group I had grade 4 nasal obstruction, whereas 10% (n = 3) sides of group II had grade 4 nasal obstruction.
Study showed improvement in nasal airflow (p < .001) and significant decrease in nasal resistance (p < .001) in resected middle turbinate group [17]. Our study showed similar improvement of nasal obstruction in both the groups but it was more evident in group I than group II (p = .0007). Postoperatively, hyposmia improved in both the groups. Resection of antero-inferior portion of middle turbinate leaving superior aspect unaffected may improve olfactory score due to better airflow to olfactory cleft. The space between midportion of the septum and MT correlates strongly with olfaction [18].
Both the groups showed symptomatic improvement of headache postoperatively without any statistical significance. There was no complaint of rhinorrhoea in 66.67% (n = 20) sides of group I and 50.00% (n = 15) sides of group II respectively. It was not statistically significant (p = 0.603).
The symptomatic improvement was more in group I in comparison with group II with at the end of 6 months follow up (p = 0.001). The study conducted by Daniele et al. also showed improved quality of life among both the resected and preserved middle turbinate group (p < .001). The recurrence of nasal polyposis was less in MT resected group than MT preserved group (p = .0055) [5].
In the current study, there were no significant incidences of haemorrhage, CSF leak or orbital injury in either group. Other studies have also shown no significant difference in the incidence of complications like epistaxis requiring return to operation theatre, orbital haematoma or CSF rhinorrhoea in either group [19]. Hence, our study supports that pMTR remains a safe procedure with surgical competency.
It is important to consider the limitations of the study as well. The study was conducted with a sample size of 31 patients which was sufficient for carrying out a quantitative analysis but a larger sample size is necessary to ensure that the sample is representative of the population.
Association with allergy, asthma, cystic fibrosis, aspirin intolerance were not included in the present study. The follow-up was limited to 6 months. Therefore, a larger sample considering associated disease processes and a prolonged follow-up may be considered for further evaluation of efficacy of pMTR.
Conclusion
In the present study, both the groups showed improved endoscopic assessment of nasal mucosa. Comparing middle turbinate resection and preservation, we could not arrive at a statistically significant outcome regarding recurrence of nasal polyposis suggesting that short-term outcomes are similar for both the groups. The group, in which the middle turbinate was resected, showed a better and statistically significant symptomatic improvement than the group in which middle turbinate was preserved with no increased risk of complications. So, partial resection of middle turbinate may be relevant in cases of endoscopic sinus surgery resulting in symptomatic improvement without affecting course of the disease or increased risk of complications.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures involving human participants were in accordance with the ethical standards of the institution.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
References
- 1.Gleeson M. Scott-Brown’s otorhinolaryngology, head and neck surgery. 7. London: Hodder Arnold; 2008. p. 1550. [Google Scholar]
- 2.Scangas GA, Remenschneider AK, et al. Does the timing of middle turbinate resection influence quality-of-life outcomes for patients with chronic rhinosinusitis. Otolaryngol Head Neck Surg. 2017;157(5):874–879. doi: 10.1177/0194599817706929. [DOI] [PubMed] [Google Scholar]
- 3.Halderman AA, Stokken J, et al. The effect of middle turbinate resection on topical drug distribution into paranasal sinuses. Int Forum Allergy Rhinol. 2016;6(10):1056–1061. doi: 10.1002/alr.21791. [DOI] [PubMed] [Google Scholar]
- 4.Daniele M, Matteo AC, Francesco M, Alessio M, Gordana J, Federica M, et al. Middle turbinate resection versus preservation in endoscopic surgical treatment of nasal polyposis. Acta Oto Laryngol. 2008;128:1019–1026. doi: 10.1080/00016480701827541. [DOI] [PubMed] [Google Scholar]
- 5.Havas TE, Lowinger DS. Comparison of functional endonasal sinus surgery with and without partial middle turbinate resection. Ann Otol Rhinol Laryngol. 2000;109:634–637. doi: 10.1177/000348940010900704. [DOI] [PubMed] [Google Scholar]
- 6.Solar ZM, Hwang PH, Mace J, Smith TL. Outcomes after middle turbinate resection: revisiting a controversial topic. Laryngoscope. 2010;120:832–836. doi: 10.1002/lary.20812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Damm M, Quante G, Jungehuelsing M, Stennert E. Impact of functional endoscopic sinus surgery on symptoms and quality of life in chronic rhinosinusitis. Laryngoscope. 2002;112:310–315. doi: 10.1097/00005537-200202000-00020. [DOI] [PubMed] [Google Scholar]
- 8.Meltzer EO, Hamilos DL, Hadley JA, et al. Rhinosinusitis: developing guidance for clinical trials. Otolaryngol Head Neck Surg. 2006;135(5 Suppl):S31–S80. doi: 10.1016/j.otohns.2006.09.014. [DOI] [PubMed] [Google Scholar]
- 9.Kuhn FA, Javer AR. Allergic fungal rhinosinusitis-our experience. Arch Otolaryngol Head Neck Surg. 1998;124:755–757. doi: 10.1001/archotol.124.10.1179. [DOI] [PubMed] [Google Scholar]
- 10.Wu AW, Ting JY, Platt MP, et al. Factors affecting time to revision sinus surgery for nasal polyps: a 25 year experience. Laryngoscope. 2014;124:29–33. doi: 10.1002/lary.24213. [DOI] [PubMed] [Google Scholar]
- 11.Wynn R, Har-El G. Recurrence rates after endoscopic sinus surgery for massive sinus polyposis. Laryngoscope. 2004;114:811–813. doi: 10.1097/00005537-200405000-00004. [DOI] [PubMed] [Google Scholar]
- 12.Pochon N, Lacroix JS. Incidence and surgery of concha bullosa in chronic rhinosinusitis. Rhinology. 1994;32:11–14. [PubMed] [Google Scholar]
- 13.Lacroix JS, Kurt AM, Pochon N, et al. Neutral endopeptidase activity and concentration of sensory neuropeptide in the human nasal mucosa. Eur Arch Otorhinolaryngol. 1995;252:465–468. doi: 10.1007/BF02114752. [DOI] [PubMed] [Google Scholar]
- 14.Fortune DS, Duncavage JA. Incidence of frontal sinusitis following partial middle turbinectomy. Ann Otol Rhinol Laryngol. 1998;107:447–453. doi: 10.1177/000348949810700601. [DOI] [PubMed] [Google Scholar]
- 15.Davis WE, Templer JW, LaMear WR, Davis WE, Jr, Craig SB. Middle meatus antrostomy: patency rates and risk factors. Otolaryngol Head Neck Surg. 1991;104:467–472. doi: 10.1177/019459989110400407. [DOI] [PubMed] [Google Scholar]
- 16.Biedlingmaier JF, Whelan P, Zoarski G, Michael R. Histopathology and CT analysis of partially resected middle turbinate. Laryngoscope. 1996;106:102–104. doi: 10.1097/00005537-199601000-00020. [DOI] [PubMed] [Google Scholar]
- 17.Cook PR, Ali B, Cullen B, Davis E. Effect of partial middle turbinectomy on nasal airflow and resistance. Otolaryngol Head Neck Surg. 1995;113:413–419. doi: 10.1016/S0194-5998(95)70078-1. [DOI] [PubMed] [Google Scholar]
- 18.Leopold DA. The relationship between nasal anatomy and human olfaction. Laryngoscope. 1988;98:1232–1238. doi: 10.1288/00005537-198811000-00015. [DOI] [PubMed] [Google Scholar]
- 19.Choby GW, Hobson CE, Lee S, et al. Clinical effects of middle turbinate resection after endoscopic sinus surgery: a systematic review. Am J Rhinol Allergy. 2014;28:502–507. doi: 10.2500/ajra.2014.28.4097. [DOI] [PubMed] [Google Scholar]