Abstract
Although cutaneous tuberculosis (TB) is a rare form of extra-pulmonary TB, lupus vulgaris is the commonest variant of cutaneous TB. We present a 14 year female with non-healing ulcer over the upper lip extending and destroying the collumela and part of anterior nasal septum. Histopathological examination revealed TB as a possible cause of the lesion. Identification of acid-fast bacilli on direct stained smears confirms the diagnosis of TB. Complete healing of the ulcer was achieved with anti-tuberculous regime leaving a residual fibrosis over the site of the ulcer.
Keywords: Nose, Lupus vulgaris, Iraq
Introduction
Tuberculosis is the second most common infection, affecting the humans in the world [1]. Tuberculosis is more common in the developing countries, but an increment has also been reported even in developed nations due to AIDS (damages the cellular immunity) which consider as an essential risk factor for the reemergence of tuberculosis [1]. Involvement of the nose is rare. Nasal tuberculosis (NTB) is usually due to extension from primary pulmonary TB or from facial TB [2]. The first case was reported by the Italian anatomist in 1761 during the autopsy results of a young man with nasal ulcerative lesion [3]. The nose is also rarely involved by Primary TB. In 1852, the first case of primary NTB was reported [3]. In a recent study from Tunisia, 29 cases of lupus vulgaris were reported over 34 years [4]. Previous studies were presented few cases of NTB [2, 5–15]. In the present article, we present a case of nasal tuberculosis.
Case Report
A 14 year old female presented to our outpatient ENT department in AL-Hussein Teaching Hospital 1 year ago with non-healing ulcer covered by dry crustation on the central part of upper lip which extends and destroys the columella and part of anterior nasal septum. She also complains from pus coming out from the lesion and stuffiness of the nose. She received treatment in form of antibiotics and nasal douche from dermatologist and otolaryngologist but without benefit. Incisional biopsy was performed which revealed chronic non-specific inflammation. She denied any history of productive cough, fever, night sweating, loss of appetite and weight loss. Physical examination revealed dry crustation covering the ulcerative area (Fig. 1), No cervical lymphadenopathy, chest clear and no intraabdominal mass or organomegaly.
Fig. 1.

Photograph of patient before anti-tuberculous treatment showing ulcerative and crusted lesion over upper lip and columella
We put the differential diagnosis for this lesion lupus vulgaris as one on the top of the list followed by malignancy and Wegner’s granulomatosis.
The patient was sent for complete haematological and bio-chemical investigations which reveals normal findings. No abnormalities on chest X-ray were detected. Early morning sputum sample examinations on three consecutive days for AFB were negative. VDRL test for syphilis and ANCA test were negative too.
After disappearance of the crustation by nasal douche and antibiotics for the secondary bacterial infection, a second incisional biopsy under local anaesthesia was done and the specimen sent for histopathological examination. The pathological report revealed the possibility of tuberculosis or atypical mycobacterial infections (Fig. 2). The diagnosis of NTB was confirmed by the identification of the acid-fast bacilli on direct stained smears.
Fig. 2.
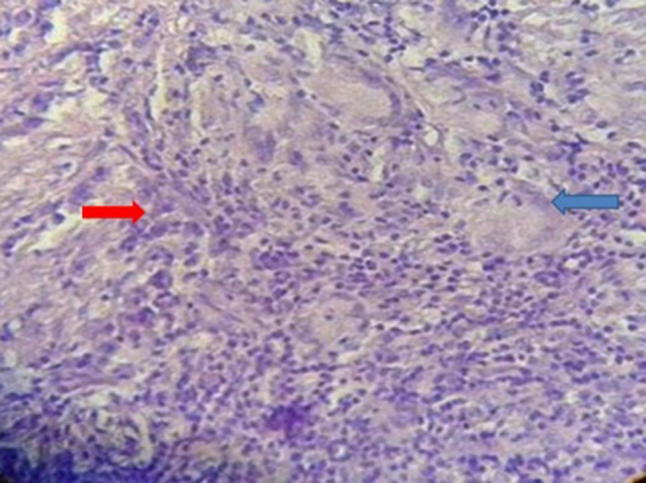
Showed irregular acanthosis with heavy sub-epithelial mononuclear inflammatory cell infiltrate and non-caseating confluent granulomatous reaction with foreign body and langhan’s giant cells. No definite LD bodies were noted. No malignancy was seen
The patient was sent for TB center in Sammawah city and received full treatment with anti-tuberculous regime. The ulcer was completely healed with residual fibrosis at the site of the ulcer (Fig. 3). The case report study was approved by scientific team of AL-Hussein Teaching Hospital in Sammawah city/Iraq.
Fig. 3.

Photograph of patient after treatment with anti-tuberculous drugs showing complete resolution of ulceration and crusting with residual fibrosis
Discussion
There is an increase in cases of extra-pulmonary TB in the past few decades reaching to about 15–20% of patients with TB in immunocompetent patients and more than 50% of subjects with positive human immunodeficiency virus (HIV) and other immunocompromised conditions. Lymph nodes is the most common site of extra pulmonary TB, followed by pleura but other organs also affected like bones, genito-urinary tract, abdomen, and meninges in a fair number of patients [14].
Extra-pulmonary tuberculosis presenting on rare locations is a challenge for the diagnosis by physicians and tuberculosis of the nose is one of them due to nonspecific signs and symptoms [16]. Tuberculosis of the nose is usually due to pulmonary tuberculosis or to lupus vulgaris of facial skin [17]. While Primary NTB is rare because of many factors: presence of the cilia, effect of bactericidal nasal secretions, filtering by nasal vibrissae and the inherent resistance offered by the mucosa of the nose [16].
Lupus vulgaris is a TB of the skin seen in peoples who have a previous infection by TB bacilli, and those with moderate, and higher tuberculin sensitivity. The infection can reach the skin via endogenous route (hematogenous, lymphogenous) or by direct exogenous route from an infected site by tuberculosis infection like verrucous TB, scrofuloderma scar, and BCG vaccination site. Lupus vulgaris is characterized by red-brown plaques like lesions which spread to the periphery leaving a scar in the middle through the process of healing. On discopic evaluation of these plaques appear like apple jelly. There may be another lesions develop on atrophic sites. As a result of ulcerations, scars, and complications occurring due to the effect of the disease, lupus vulgaris can describe in 5 clinical entities; plaque or planar form, ulcerative or mutilant form, vegetant form, tumor-like form and papulonodular form [18, 19].
It is difficult to diagnose NTB owing to nonspecific signs and symptoms of the disease [16]. The diagnosis is established by isolating acid-fast bacilli from tissue excised during biopsy. Examination of nasal secretions and swab specimens carry a very low result and should not be used to diagnose this disease. On pathological evaluation, granulomas of both caseation and non-caseation have been identified. Non-caseation granuloma is confusing histologically, and may be misdiagnosed as Wegener’s granuloma [1, 3]. Identification of Acid-fast bacilli on Ziehl–Neelsen staining culture of excised biopsies are more often positive than are smears. It is essential to send a piece of excised tissue for culture, together with an identification of the suspected organisms [20]. The anti-tuberculous drugs and their duration was standardized by WHO which involves a combination of 4 drugs: daily INH (5–10 mg/kg), ethambutol (25 mg/kg), rifamycin (like rifampin) (10–12 mg/kg) and pyrazinamide (35 mg/kg) for 2 months and daily rifamycin (like rifampin) and INH only for another 4 months except in TB of the bones and meninges which requires prolongation of the duration of therapy to 1 year. Streptomycin (30 mg/kg) is used only in relapsing cases. The ulcerative nasal lesion in this patient was diagnosed as NTB according to the demonstration of acid-fast bacilli on smear together with complete healing of the ulcer on 6 months anti-tuberculous therapy. During the 18 months follow-up, there is no relapse of the lesion.
Conclusion
NTB is a rare entity of extra-pulmonary TB and most commonly encountered in endemic countries like India. The diagnosis of NTB is challenging owing to non-specific presentations, which is required a high suspicion from the dealing otolaryngologist and a thorough history with proper physical examination and panoramic investigations including haematological and biochemical tests, chest X-ray, biopsy for pathological evaluation, direct smear for acid-fast bacilli, culture and PCR test in order to confirm the diagnosis. In this case the pathological examination doesn’t confirm the diagnosis but on direct smear acid-fast bacilli was found and complete cure of the lesion was successfully achieved by a 6 months regime of anti-tuberculous drugs.
Acknowledgements
I am grateful to thank the pathologist Dr. Ameer Dhahir for his kind preparation of the picture of the microscopic slide for the pathological specimen. I am also to give my thanks to the pathologist Assistant Professor Dr. Arkan Al-Essawi for his help in the interpretation of the pathological slide. I would like to thank the chief and sub-staffs of Tuberculosis and Chest Diseases Health Center in Al-Samawah City for their kindness cooperation in treatment and follow-up of the presenting case.
Compliance with Ethical Standards
Conflict of interest
The author declares that he has no conflict of interests.
Ethical Approval
The research is involving a human participant.
Informed Consent
Informed consent was taken from her father but unfortunately in Arabic language.
References
- 1.Fitzgerald DW, Sterling TR, Haas DW. Mycobacterium tuberculosis. In: Mandell GL, Bennett JE, Dolin R, editors. Principle and practice of infectious diseases. 7. Philadelphia: Churchill Livingstone; 2010. pp. 3129–3163. [Google Scholar]
- 2.Choi YC, Park YS, Jeon EJ, Song SH. The disappeared disease: tuberculosis of the nasal septum. Rhinology. 2000;38:90–92. [PubMed] [Google Scholar]
- 3.Waldman SR, Levine HL, Sebek BA, Parker W, Tucker HM. Nasal tuberculosis: a forgotten entity. Laryngoscope. 1981;91:11–16. doi: 10.1288/00005537-198101000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Sellami K, Boudaya S, Chaabane H, Amouri M, Masmoudi A, Mseddi M, Turki H. Twenty-nine cases of lupus vulgaris. Med Mal Infect. 2016;46(2):93–95. doi: 10.1016/j.medmal.2015.12.007. [DOI] [PubMed] [Google Scholar]
- 5.Blanco Aparicio M, Verea Hernando H, Pombo F. Tuberculosis of the nasal fossa manifested by a polypoid mass. J Otolaryngol. 1995;24:317–318. [PubMed] [Google Scholar]
- 6.Singhal SK, Dass A, Mohan H, Venkataramana Y. Primary nasal tuberculosis. J Otolaryngol. 2002;31:60–62. doi: 10.2310/7070.2002.19258. [DOI] [PubMed] [Google Scholar]
- 7.Hup AK, Haitjema T, de Kuijper G. Primary nasal tuberculosis. Rhinology. 2001;39:47–48. [PubMed] [Google Scholar]
- 8.Batra K, Chaudhary N, Motwani G, Rai AK. An unusual case of primary nasal tuberculosis with epistaxis and epilepsy. Ear Nose Throat J. 2002;81:842–844. doi: 10.1177/014556130208101213. [DOI] [PubMed] [Google Scholar]
- 9.Alavi SM, Nashibi R. Nasal tuberculosis in a 56 year old woman. Casp J Intern Med. 2014;5(1):49–51. [PMC free article] [PubMed] [Google Scholar]
- 10.Garg A, Wadhera R, Gulati SP, Singh J. Lupus vulgaris of external nose with septal perforation—a rarity in antibiotic era. Indian J Tuberc. 2010;57(3):157–159. [PubMed] [Google Scholar]
- 11.Singal A, Arora R, Pandhi D. Lupus vulgaris leading to perforation of nasal septum in a child. Indian Dermatol Online J. 2015;6(3):196–197. doi: 10.4103/2229-5178.156401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bhandary SK, Ranganna BU. Lupus vulgaris of external nose. Indian J Otolaryngol Head Neck Surg. 2008;60:373–375. doi: 10.1007/s12070-008-0100-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Arunkumar JS, Naveen KN, Prasad KC, Santhosh SG, Hegde JS. Lupus vulgaris of external nose—a case report. J Indian Med Assoc. 2013;111(2):130-1, 134. [PubMed] [Google Scholar]
- 14.Bajaj DK, Verma AK, Jaiswal R, Kant S, Patel A, Asnani M. Tip of nose tuberculosis: a rare presentation of extra pulmonary tuberculosis. Intractable Rare Dis Res. 2016;5(2):133–136. doi: 10.5582/irdr.2015.01046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nair PA, Mehta MJ, Patel BB. Ulcerative lupus vulgaris over nose, leading to cosmetic deformity. Indian J Dermatol. 2015;60(1):104. doi: 10.4103/0019-5154.147856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hughes RG, Drake-Lee A. Nasal manifestations of granulomatous disease. Hosp Med. 2001;2:417–421. doi: 10.12968/hosp.2001.62.7.1612. [DOI] [PubMed] [Google Scholar]
- 17.Howard D (1997) Nonhealing granulomas. In: Mackay IS, Bull TR (eds) Scott Brown’s otolaryngology: rhinology, 6th edn. Butterworth and Heinemann, Oxford, p 4/20:1–11
- 18.Yates VM, Rook GAW. Mycobacterial infections. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook’s textbook of dermatology. 7. Turin: Blackwell Science; 2004. pp. 281–339. [Google Scholar]
- 19.Tappeiner G, Wolff K. Tuberculosis and other mycobacterial infections. In: Freedberg IM, Eisen AZ, Wollf K, Austen KF, Goldsmith LA, Katz S, editors. Fitzpatrick’s dermatology in general medicine. 6. New York: McGraw-Hill; 2003. pp. 1933–1949. [Google Scholar]
- 20.Goguen LA, Karmody CS. Nasal tuberculosis. Otolaryngol Head Neck Surg. 1995;113:131–135. doi: 10.1016/S0194-5998(95)70156-7. [DOI] [PubMed] [Google Scholar]


