Abstract
Intraoral schwannomas account for 1% of head and neck schwannoma, with tongue base schwannoma being reported rarely. In an English literature search from 1988 to 2014, not more than 38 cases of tongue base schwannoma have been reported. Large tongue base schwannomas pose a significant risk to airway, thereby calling for an early intervention. We report a rare case of tongue base schwannoma in a 25 year old female managed surgically by lateral pharyngotomy approach.
Keywords: Schwanomma, Tongue base, Lateral pharyngotomy
Introduction
Schwannomas account for 20–40% of benign tumours of head and neck. Schwannomas are benign nerve sheath tumours characterised by Antoni type A and type B cells. Intraoral schwannomas are rare with tongue base being a rare site. The common presentations of tongue base schwannoma are breathing difficulty, difficulty in swallowing and change in voice.
Case Report
A 25 year old female patient presented to otolaryngology outpatient department of our hospital with complaints of difficulty in swallowing, foreign body sensation in throat and change in voice for 2 years. There was no complaint of breathing difficulty even during supine position. There was no history of hematemesis or bleeding from oral cavity. On clinical examination, patient was comfortable without any breathing difficulty. Oral examination was unremarkable. On indirect laryngoscopy, a diffuse bulge was seen in the vallecula on right side extending onto base of tongue. Epiglottis and rest of the endolarynx was not visualised on indirect laryngoscopy. On fibreoptic laryngoscopy the larynx was found to be normal.
MRI scan of oral cavity and neck was ordered which revealed well defined mass measuring 4.6 × 3.8 × 4.1 cm in the oropharynx which shows heterogenous signal enhancement on T2W images and isohyperintense on T1W images (Fig. 1). The mass was completely obliterating the vallecula causing downward displacement of epiglottis and upward displacement of base tongue. Thyroid gland was found normal in position. FNAC could not be done in view of inaccessibility of intraoral mass and subsequent risk of aspiration. Lateral pharyngotomy approach was planned with elective tracheostomy to avoid airway compromise postoperatively. Elective tracheostomy was done preoperatively under local anesthesia with the patient lying supine. A mid tracheostomy was done and cuffed 8 mm I.D PVC tracheostomy tube was inserted. Patient was anesthetised through the tracheostomy. Cervical incision was given at the level of hyoid and the pharynx opened at the level of pyriform fossa. The mass was slowly dissected out the surrounding tongue and the entire mass was excised in toto. The mass was found to be well encapsulated and we could not identify any nerve macroscopically originating this lesion. Postoperative period was uneventful and patient was decannulated in 48 h. There was no cranial nerve palsy postoperatively and patient is on regular follow up for last 6 months without any recurrence. On gross examination the mass measured 4 × 4 × 2 cm. Histopathological examination of the specimen showed features consistent with schwannoma with tumour cells positive for S-100 (Fig. 2).
Fig. 1.

MRI neck showing the mass in the vallecula completely obliterating it and displacing base tongue upwards
Fig. 2.
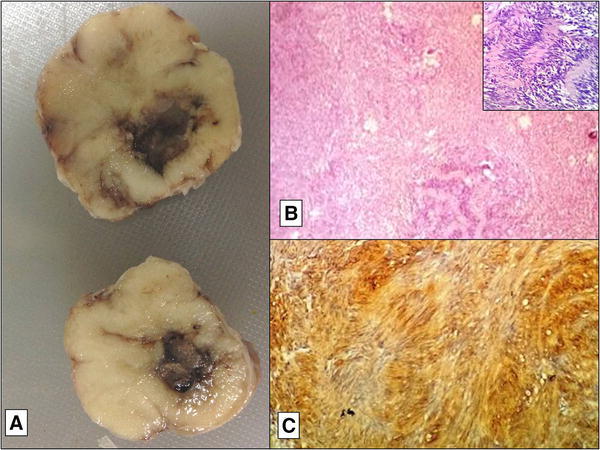
a Gross photograph of soft tissue mass, showing grey white glistening cut surface with a focal area of hemorrhage. b Mcrophotograph of the same showing benign appearing spindled out cells in hypo and hypercellular areas (inset verocay bodies), H&E stain, ×40. c Immunohistochemical stain for S-100 showing strongly positive tumor cells
Discussion
Schwannoma was first reported by Virchow in 1908. Schwannomas or neurilemmas are benign encapsulated tumours arising from Schwann cell of nerve sheath of autonomic, peripheral or cranial nerve. Multiple lesions may occur in association with Von Recklinghausen’s disease with a predilection for malignant transformation in 15% of cases [1]. Most common site for head and neck schwannoma is the vestibular nerve. Most common site for non vestibular schwannoma in head and neck is parapharyngeal space. Originating nerve is identified in only 50% of cases [2]. Sympathetic trunk and vagus nerve were the two most common nerves identified [3]. Base tongue schwanommas are very rarely seen. The common differential diagnosis are lipoma, hemangioma, eosinophilic granuloma, epidermoid and dermoid cysts, epithelial hyperplasia, granular cell tumor, benign salivary gland tumors, rhabdomyoma, leiomyoma, lingual thyroid, and lymphangioma [1].
They are commonly seen in 20–40 years of age without any sex predilection. Clinically, they are slow growing masses and are asymptomatic. They present symptomatically only when they attain a significant size. The common presenting features are: dysphagia, hot potato voice, respiratory obstruction and intraoral bleeding (rarely seen in cases of infected schwannomas or inadvertent trauma). In order of frequency, intraoral peripheral schwannomas are most commonly located in the tongue, followed by the palate, floor of the mouth, cheek mucosa and gums [4]. Surgical management is the treatment of choice for tongue base schwannomas. Urgent surgical intervention is necessary to avoid airway problems.
Radiologically, most schwannomas on CT appear as well-circumscribed, dense, homogeneous soft-tissue masses which exhibit contrast enhancement. Calcification or hemorrhage is uncommon, but cystic or fatty degeneration is frequent. MRI is superior to CT for schwannomas. Most schwannomas appear hypointense or isointense relative to muscle on T1-weighted images, hyperintense on T2-weighted images, and show strong enhancement after contrast administration [5].
Histologically, two different patterns are recognised. Antoni A, with high cellularity and little stromal matrix is the commonest form. Antoni typeA tissue shows well-developed cylindrical bands of Schwann’s cells and connective tissue fibres with a tendency towards pallisading of the nuclei about a central mass of cytoplasm (Verocay bodies) and Antoni type B tissue is a loosely arranged stroma in which the fibres and cells form no distinctive pattern [6]. S100 proteins are currently the most sensitive marker for tumors with schwannian differentiation.
Various surgical techniques have been described for management of tongue base schwannomas [7]. Transoral robotic surgery, CO2 Laser excision, intraoral excision using diathermy, suprahyoid pharyngotomy, lateral pharyngotomy, submandibular approach and midline mandibulotomy have been described. There have been attempts to excise base tongue mass via midline tongue spit incision also. Transoral excision has various advantages: (1) avoids external scar, (2) improved preservation of sensation and function, (3) earlier swallow rehabilitation and (4) decreased frequency of fistula formation. It has the disadvantage of limited exposure and less optimal visualisation of deeper structures. Pharyngotomy approach has the advantage of preservation of mandibular continuity, avoidance of lip splitting incision and ability to close defect primarily. In our case, we preferred lateral pharyngotomy approach over midline mandibulotomy to avoid postoperative morbidity due to faulty occlusion. We did not consider to excise by intraoral approach because it was a big mass which was merging in the base of the tongue.
Tongue base schwannomas pose a great challenge for anesthetists as well due to airway compromise as well as risk of trauma and subsequent bleeding from the mass during intubation [8]. Skilled anesthetists are required for awake fibreoptic intubation in such cases. We recommend preoperative tracheostomy in such cases especially in very large tongue base masses. Tracheostomy has the advantage of providing a safe airway, prevents the risk of trauma to mass during intubation and is very helpful in dealing with the complications of tongue base oedema and bleeding postoperatively. Awake fibreoptic nasotracheal intubation is the most common method used in such cases. But in these cases, otolaryngologists should be prepared for an emergency tracheostomy if the need arises. In cases, where the mass is very huge and patient is not able to lie supine, the following methods have been described: transtracheal jet ventilation (TTJV) and the esophageal tracheal combitube (ETC) [9].
Percutaneous transtracheal jet ventilation is provided by passing a large bore catheter through the cricothyroid membrane and providing high pressure oxygen through it. It buys time for the emergency tracheostomy and is safe too. The esophageal tracheal combitube is a device having twin lumen tube—one resembling an endotracheal tube and the other an esophageal obturator airway. There are two balloons: proximal and distal. Proximal balloon seals the mouth and nose whereas distal seals either the esophagus or the trachea. If the tube enters the trachea, the tracheal lumen is used to ventilate the lungs. If it enters the esophagus, perforations in the esophageal lumen above the level of the esophagus allow ventilation of the lungs.
Conclusion
Tongue base schwannoma, though a benign condition, can be challenging for an otolaryngologist. They pose a significant threat to airway, therefore early diagnosis and treatment are vital. Thus, it must be considered as one of the differential diagnosis in benign tumors of tongue base.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Contributor Information
Swati Tandon, Email: drswatitandon86@gmail.com.
Ravi Meher, Email: ravimeher@gmail.com.
Aditi Chopra, Email: aditi@gmail.com.
Anoop Raj, Email: dr.anoopraj@gmail.com.
Vikram Wadhwa, Email: drvikramwadhwa@yahoo.com.
Nidhi Mahajan, Email: Nidhi0615@gmail.com.
Avani Jain, Email: Avanijain87@hotmail.com.
References
- 1.George NA, Wagh M, Balagopal PG, Gupta S, Sukumaran R, Sebestian P. Shwannoma base tongue: case report and review of literature. Gulf J Oncol. 2014;1(16):94–100. [PubMed] [Google Scholar]
- 2.Sannikorn P, Praweswararat P, Jitpakdee S, Suphareokthaweechai R. Schwannoma at the base of tongue: a case report. Ann Otolaryngol Rhinol. 2014;1(3):1015. [Google Scholar]
- 3.Liu H-L, S-Y Yu, Li GK-H, Wei WI. Extracranial head and neck schwannomas: a study of the nerve of origin. Eur Arch Otorhinolaryngol. 2011;268(9):1343–1347. doi: 10.1007/s00405-011-1491-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sanchis JM, Navarro CM, Bagán JV, Onofre MA, Murillo J, De-Andrade CR, Díaz JM, Pereira-Filho VA. Intraoral Schwannomas: presentation of a series of 12 cases. J Clin Exp Dent. 2013;5(4):e192–e196. doi: 10.4317/jced.51176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim SH, Han MH, Park SW, Chang K-H. Radiologic-pathologic correlation of unusual lingual masses: part II: benign and malignant tumors. Korean J Radiol. 2001;2(1):42–51. doi: 10.3348/kjr.2001.2.1.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Philip R, Chong AW, Rosalind S, Gurdeep S, Kalyani S. Three cases of head and neck schwannomas: varied clinical presentation. Med J Malaysia. 2007;62(2):175. [PubMed] [Google Scholar]
- 7.Ying B, Zhu S, Qiao Y, Ye W, Maimaiti A, Hu J, Zhang Y. Surgical approaches for tongue base schwannoma. J Craniofac Surg. 2013;24(1):e9–e11. doi: 10.1097/SCS.0b013e3182668867. [DOI] [PubMed] [Google Scholar]
- 8.Batra UB, Usha G, Gogia AR. Anesthetic management of schwannoma of the base of the tongue. J Anaesthesiol Clin Pharmacol. 2011;27(2):241–243. doi: 10.4103/0970-9185.81830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jensen NF, Benumof JL. The difficult airway in head and neck tumor surgery. Anesthesiol Clin N Am. 1993;11:475. [Google Scholar]


