Abstract
Obstructive sleep apnoea syndrome is a chronic condition characterized by frequent episodes of collapse of upper airways during sleep. Prevalence of the disease is settled at about 3–7%. Today, palatal surgery is a reference point in OSAHS treatment and there are many different surgical techniques. The purpose of our work is to compare post-operative results of palate surgery techniques used in our practice in OSAHS patients, studying the degree of patients’ satisfaction with a recent score recommended by Rashwan et al. called PPOPS (Palate Post-Operative Problems Score). A retrospective study was performed on a sample of 40 patients subject to different palate surgery techniques for OSAS. Analysed surgical techniques were: Expansion Sphincter Pharyngoplasty (ESP), Uvulopalatopharyngoplasty (UPPP), Anterior Pharyngoplasty (AP), Barbed Reposition Pharyngoplasty (BRP). Patients answered the PPOPS and the results for each of the four techniques were compared. Group differences in the questionnaire total score were evaluated through Tukey’s honest significance test for multiple (pairwise) comparisons. Overall average scores in the four groups were: AP 2.21, ESP 5.92, UPPP 2.8 and BRP 2.4. Comparing ESP with the other techniques (BRP, AP and UPPP) the scores were significantly higher (P < 0.05). Pairwise comparisons between the other three techniques (FA, UPPP and BRP) had a P value higher than 0.05, allowing to state that questionnaire results, in these cases, were similar to each other. Our work shows that different surgical techniques, even with the same purpose, could have different characteristics during follow-up. PPOPS is useful in post-operative for a better surgical practice.
Keywords: OSAS, PPOPS, Palate surgery, Sleep apnoea, Pharyngoplasty
Introduction
OSAHS (Obstructive Sleep Apnoea-Hypopnea Syndrome) is a disease characterized by upper airways obstruction causing oro-nasal air Flux absence or reduction [1] in thoraco-abdominal movements presence.
The disease prevalence is settled at about 3–7% and there are many factors predisposing to this disorder, such as age, male gender, obesity [2], family history, menopausal, craniofacial abnormalities, and voluptuary habits such as cigarette smoke and alcohol abuse [3].
Today, palatal surgery is a reference point in OSAHS treatment, and most used surgical techniques are: Uvulopalatopharyngoplasty (UPPP) [4–6], Expansion sphincter pharyngoplasty (ESP) [7, 8], Barbed reposition pharyngoplasty (BRP) [9] and Anterior pharyngoplasty (AP) [10, 11]. UPPP (Uvulopalatopharyngoplasty) is based on soft palate section and on uvula removal.
ESP (Expansion sphincter pharyngoplasty) is performed after tonsillectomy [12] and is based on “palatal pharingeal muscle section” and its re-positioning.
BRP (Barbed reposition pharyngoplasty) needs barbed sutures, which are inside soft palate to wide pharynx lateral wall. AP (Anterior pharyngoplasty) is based on a rectangular section between soft palate and hard palate expanding pharyngeal wall anterior–posterior space.
These three different techniques are very different for surgeon but especially for patients.
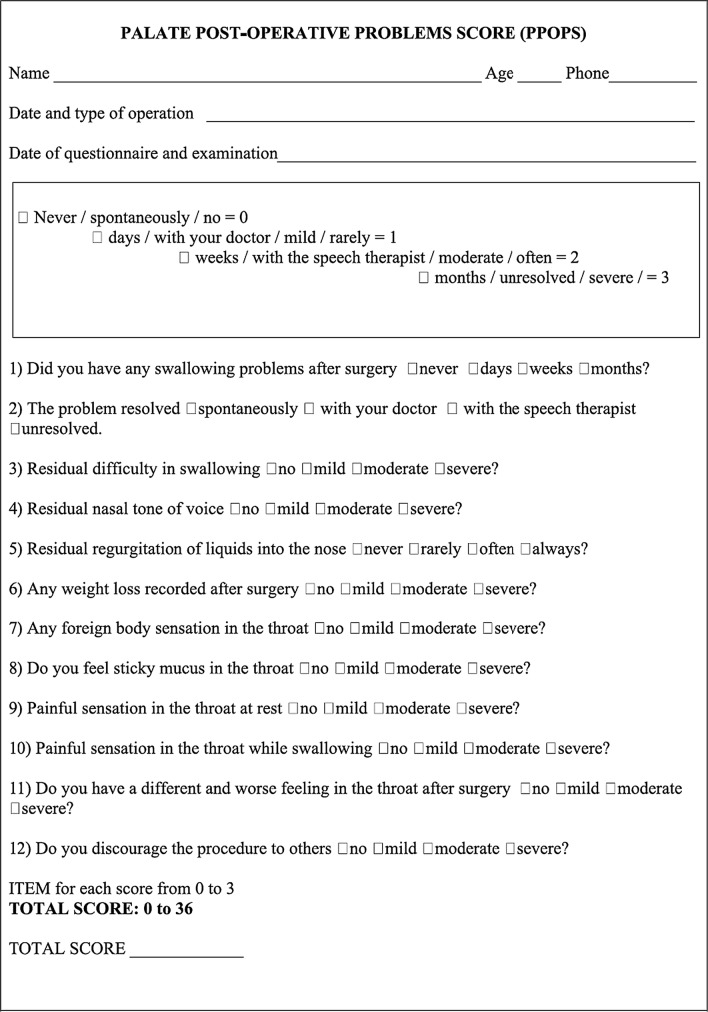
The purpose of our work is to compare palatal surgery techniques results used in our practice in OSAHS patients, in particular we evaluated every surgical technique post-operative course, studying the degree of patient’s satisfaction, so we made use of a recent score recommended by Rashwan et al. called PPOPS (Palate Post-Operative Problems Score) [13] (Table 1).
Table 1.
PPOPS Questionnaire (Rashwan et al.)
Materials and Methods
A retrospective study was performed on a sample of 40 patients subjected to palate surgery for OSAHS, 37 males and 3 females, mean age 49.8 years old, followed-up by the Palermo University Otolaryngology Unit from January 2013 to December 2017.
Surgical techniques we analysed were: Expansion Sphincter Pharyngoplasty (ESP), Uvulopalatopharyngoplasty (UPPP), Anterior Pharyngoplasty (AP), Barbed Reposition Pharyngoplasty (BRP). We gathered 40 patients fairly allocated in 4 surgical categories. Mean age was 49.8 years; in each surgical category mean age was: ESP: 56.7; UPPP: 46.4; AP: 46.7; BRP: 43.4.
PPOPS survey (Palate Post-Operative Problems Score) was recently recommended by Rashwan et al., as a valid instrument to assess palate surgery patients’ post-operative perception. It is composed by 12 questions investigating swallowing problems after surgery, nasal voice, weight loss and swallowing pain or discomfort over time. The last question has the purpose of identifying the degree of satisfaction and probability of discouraging the procedure to others. Each answer is scored from 0 to 3 where 0 is the best result and 3 is the worst; the survey can have a total score ranging from 0 to 36.
All patients answered to all questions, so we had a homogeneous context and we could compare group results. Group differences in the questionnaire total score were evaluated through Tukey’s honest significance test for multiple (pairwise) comparisons. Tukey’s test, is a single-step multiple comparison procedure and statistical test. Tukey’s test compares the means of every treatment to the means of every other treatment; that is, it applies simultaneously to the set of all pairwise comparisons μi − μj and identifies any difference between two means that is greater than the expected standard error. The confidence coefficient for the set, when all sample sizes are equal, is exactly 1 − α for any 0 ≤ α ≤ 1. For unequal sample sizes, the confidence coefficient is greater than 1 − α. In other words, the Tukey method is conservative when there are unequal sample sizes. Adjusted P values lower than 0.05 were considered significant.
One of the problems raised by Rashwan et al. was the possibility that the time spent between surgery and questionnaire could be influenced by recall bias, so we decided to focus our attention on a 5-year period. During the study, we realized there were no differences in the results of the patients who made the surgery in different years.
Results
The first question investigates swallowing problems after surgery. Mean scores were: ESP 1.54, UPPP 1.2, AP 1.14 and BRP 0.6 as shown in Table 2.
Table 2.
Outcomes from PPOPS questionnaire
| Question | AP (means) | ESP (means) | UPPP (means) | BRP (means) |
|---|---|---|---|---|
| No. 1 | 1.14 | 1.54 | 1.2 | 0.6 |
| No. 2 | 0 | 0.46 | 0 | 0 |
| No. 3 | 0 | 0.61 | 0.2 | 0.2 |
| No. 4 | 0 | 0.3 | 0 | 0 |
| No. 5 | 0 | 0.23 | 0 | 0.2 |
| No. 6 | 0.71 | 0.61 | 0.8 | 1.2 |
| No. 7 | 0.07 | 0.38 | 0 | 0 |
| No. 8 | 0.14 | 0.54 | 0.2 | 0.2 |
| No. 9 | 0 | 0.23 | 0 | 0 |
| No. 10 | 0 | 0.08 | 0 | 0 |
| No. 11 | 0 | 0.38 | 0.4 | 0 |
| No. 12 | 0.14 | 0.54 | 0 | 0 |
| Total | 2.21 | 5.92 | 2.8 | 2.4 |
The second question tries to know how these swallowing problems, investigated with the previous question, were solved. Mean scores were: ESP 0.46, UPPP 0, AP 0 and BRP 0.
The third question investigates the residual difficulty in swallowing because it is one of the most important discomforts of postoperative period. Mean scores were: was ESP 0.61, UPPP 0.2, AP 0 and BRP 0.2.
Question 4 investigates the voice residual nasal tone. Mean scores were: ESP 0.3, UPPP 0, AP 0 and BRP 0.
Question 5 analyses if after surgery there are nasal secretions, we asked to answer not considering flu period or other causes that could explain these liquids. Mean scores were: ESP 0.23, UPPP 0, AP 0 and BRP 0.2.
Question 6 investigates the weight loss recorded after surgery, related to just after surgery period and so it is strictly linked to nutrition those people had during this phase. Mean scores were: ESP 0.61, UPPP 0.8, AP 0.71 and BRP 1.2.
Question 7 investigates the foreign body sensation that is variable according to surgery technique. Mean scores were: ESP 0.38, UPPP 0, AP 0.07 and BRP 0.
Question 8 investigates the sensation of sticky mucus in the throat. Mean scores were: ESP 0.54, UPPP 0.2, AP 0.14 and BRP 0.2.
Question 9 investigates the painful sensation in the throat at rest. Mean scores were: ESP 0.23, UPPP 0, AP 0 and BRP 0.
Question 10 investigates the painful sensation in the throat while swallowing. Mean scores were: ESP 0.08, UPPP 0, AP 0 and BRP 0.
Question 11 investigates if there is a different and worse feeling in the throat after surgery and analyses the differences between before and after surgery. Mean scores were: ESP 0.38, UPPP 0.4, AP 0 and BRP 0.
Question 12 investigates if the patient discourages the procedure to others. Mean scores were: ESP 0.54, UPPP 0, AP 0.14 and BRP 0.
Overall, mean scores in the four groups were: AP 2.21, ESP 5.92, UPPP 2.8 and BRP 2.4.
Statistically significant differences were found among the four techniques as showed in Table 3.
Table 3.
Outcomes of comparing the mean total score of each surgical techiniques
| Comparazione tecniche | P value |
|---|---|
| ESP-BRP | 0.0065* |
| AP-ESP | 0.03* |
| UPPP-ESP | 0.02* |
| AP-BRP | 0.99 |
| UPPP-BRP | 0.99 |
| UPPP-AP | 0.97 |
*Significance with P < 0.05
ESP scores were statistically higher with respect to other techniques (BRP, AP and UPPP) (P < 0.05). Pairwise comparisons among the other three techniques (AP, UPPP and BRP) had a P > 0.05, allowing to state that questionnaire scores were similar for these techniques.
Discussion
PPOPS score is a valid tool for an evaluation of post-operative patients for each single technique, but above all, it is useful to compare each individual surgical group results. In fact, it could show itself as a useful tool to promote and improve information exchange on surgical techniques among various surgeons. Moreover, we also think that it can also be a useful guide for the patient in the choice together with the surgeon of the type of procedure to be performed. In our study, we compared two more techniques: AP and UPPP as they are still carried out during the period considered and represent two important pillars of palatal surgery. Most patients had swallowing problems after surgery, but most of them quite solved them. Better results were in BRP group; the highest score, instead, was in ESP group. These data are predictable by surgical procedure type: BRP technique provides the use of suture raising soft palate; ESP technique provides to dissect palate-pharyngeal muscle and reposition it. Data analyses showed that ESP group had the highest incidence of residual difficulty in swallowing. In ESP group, two patients had moderate difficulties, the others mild difficulty in swallowing. In AP group, there were no residual difficulties in swallowing. We analysed OSAHS surgery specifically oriented in palatal area. We have to remember that this kind of surgery is often supported by other surgical treatment as tonsillectomy [12] or nasal surgery [1]. This is important to increase surgical results and improve air flux through superior airways. Only ESP group had residual nasal tone of voice in few patients. Few patients equally distributed in ESP and BRP groups told us about this residual regurgitation but it was a small number. ESP group had better results as to weight loss. Patients who underwent palate surgery necessarily ate liquid meal, later they were introduced semi-liquid food in their meal and at the end solid food. Caloric restriction that this kind of nutrition induces and swallowing difficulty are responsible for weight loss. We considered mild weight loss (0–5 kg), moderate (6–10 kg), severe (> 10 kg). All patients, after the reintroduction of a normal nutrition, went back to their pre-surgery weight; patients who had the higher weight loss were in BRP group.
BRP group had no foreign body sensation, no painful sensation and no swallowing.
BRP is characterized by internal sutures into soft palate, while ESP is characterized by muscular dissection, which traumatizes the palate.
Our data show only few patients had foreign body sensation, and when there was this sensation was mild or moderate, never severe.
In ESP group the sticky mucus sensation were worse than in all other groups.
Painful sensation at rest showed pain only for ESP group, it is important because these patients had pain daily and so they had a negative perception of surgery results.
UPPP group had the worst score in throat pain while swallowing, probably because this surgical procedure including soft palate dissection could be explained by the pain caused by throat muscles contraction or by bolus touching palatal and pharyngeal mucosa. However, we can state that there is no worse feeling in the throat after intervention in any of the techniques examined.
Procedure discourage was the worst result in ESP, while UPPP, AP and BRP had the same results. This is the most difficult question because it tries to understand if patients have a good post-operative course and if surgery solved OSAHS. Some people told us they preferred choosing surgery rather than using CPAP every night. We have to remember that sometimes surgery does not solve OSAHS, but it can be good at reducing CPAP pressure [1]. Patients who discouraged the procedure did not solve OSAHS or had a difficult post-operative course.
Conclusions
The work carried out shows that different surgical techniques, even if with the same purpose, could have different characteristics during follow-up.
Better results are in UPPP, AP and BRP. UPPP is a less used technique and AP is performed only in specific condition (anterior–posterior palatal collapse). In conclusion, Barbed Reposition Pharyngoplasty is the best choice both for post-operative results and for good patient compliance.
We know our work should be extended to a multi-center study to have a greater number of patients in each group.
Therefore we recommend PPOPS use because knowing patients’ post-operative is useful for a better surgical practice.
Compliance with Ethical Standards
Conflict of interest
The authors have no conflicts of interest to disclose.
Ethical Approval
This study was approved by Ethics Committee of University Hospital of Palermo.
Informed Consent
Our research involved human participants who had obtained informed consent.
References
- 1.Modica DM, Marchese D, Lorusso F, Speciale R, Saraniti C, Gallina S. Functional nasal surgery and use of CPAP in OSAS patients: our experience. Indian J Otolaryngol Head Neck Surg. 2018 doi: 10.1007/s12070-018-1396-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lorusso F, Dispenza F, Saraniti C, Sireci F, Modica DM, Gallina S. Sleep disordered breathing: evaluation of dynamic patterns of the upper airways in obese subjects. Otorinolaringologia. 2014;64(2):57–64. [Google Scholar]
- 3.Punjabi NM. The epidemiology of Adult Obstructive Sleep Apnea. Proc Am Thorac Soc. 2008;15;5(2):136–143. doi: 10.1513/pats.200709-155MG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fujita S, Conway W, Zorick F, Roth T. Surgical correction of anatomic abnormalities in obstructive sleep apnea syndrome: uvulopalatopharyngoplasty. Otolaryngol Head Neck Surg. 1981;89(6):923–934. doi: 10.1177/019459988108900609. [DOI] [PubMed] [Google Scholar]
- 5.Gallina S, Dispenza F, Kulamarva G, Ballacchino A, Speciale R. Uvulopalatopharyngoplasty with tonsillectomy in the treatment of severe OSAS. B-ENT. 2009;5(04):245–250. [PubMed] [Google Scholar]
- 6.Safaya A, Suri JC, Batra K. Uvulopalatopharyngoplasty—surgery for snoring. Indian J Otolaryngol Head Neck Surg. 2002;54(3):204–207. doi: 10.1007/BF02993104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pang KP, Woodson BT. Expansion sphincter pharyngoplasty: a new technique for the treatment of obstructive sleep apnea. Otolaryngol Head Neck Surg. 2007;137(1):110–1145. doi: 10.1016/j.otohns.2007.03.014. [DOI] [PubMed] [Google Scholar]
- 8.Lorusso F, Dispenza F, Modica DM, Gallina S. The role of modified expansion sphincter pharyngoplasty in multilevel obstructive sleep apnea syndrome surgery. Int Arch Otorhinolaryngol. 2018;22(04):432–436. doi: 10.1055/s-0038-1648248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vicini C, Hendawy E, Campanini A, Eesa M, et al. Barbed reposition pharyngoplasty (BRP) for OSAHS: a feasibility, safety, efficacy and teachability pilot study. “We are on giant’s shoulders”. Eur Arch Otorhinolaryngol. 2015;272(10):3065–3070. doi: 10.1007/s00405-015-3628-3. [DOI] [PubMed] [Google Scholar]
- 10.Pang KP, Raymond T, Puraviappan P, et al. Anterior palatoplasty for the treatment of OSAS: three-year results. Otolaryngol Head Neck Surg. 2009;141(2):253–256. doi: 10.1016/j.otohns.2009.04.020. [DOI] [PubMed] [Google Scholar]
- 11.Marchese D, Modica DM, Cancemi S, Speciale R, Gallina S. Anterior palatoplasty: effectiveness for treatment of simple snoring and mild osas. EuroMediter Biomed J. 2017;12:(12)057–60. doi: 10.3269/1970-5492.2017.12.12. [DOI] [Google Scholar]
- 12.Lorusso F, Gallina S, Modica DM, Di Salvo N, Riggio F. Bipolar quantum molecular resonance versus blunt dissection tonsillectomy. B-ENT. 2015;11(02):101–108. [PubMed] [Google Scholar]
- 13.Rashwan M, Montevecchi F, Firinua E, Dachuri S, Obaidat H, Gobbi R, Cammaroto G, Nuzzo S, Vicini C. Let’s know from our patients: PPOPS score for palate surgery evaluation/a pilot study. Eur Arch Otorhinolaryngol. 2018;275(1):287–291. doi: 10.1007/s00405-017-4795-1. [DOI] [PubMed] [Google Scholar]