Abstract
Most of the time, pediatrician is the first to see children with adenotonsillar hypertrophy (AH) and they mostly rely on clinical assessment with or without some investigation to refer these children to otorhinolaryngologist. Numerous methods have been described for evaluation of AH, but many of these methods are not possible to follow in busy pediatric outpatient unit either because of lack of cooperation from child or due to limited availability of test or due to cost constraints. This study has been conducted to determine the diagnostic accuracy of lateral neck X-ray (LNX) for assessing AH and to assess the correlation between adenoid size in LNX and clinical symptoms in a pediatric unit. Prospective study conducted in Department of ENT, Pathmavathy Medical Foundation, Kollam, Kerala, India from January 2015 to March 2016. 60 consecutive children of both genders, between the age group of 5 to 14 years, attending Department of Pediatrics with a provisional diagnosis of AH were included in the study. The symptom scores, radiographic ratio of adenoid to nasopharynx and endoscopic scorings were calculated. Lateral neck X-ray with calculation of adenoid-to-nasopharynx ratio is found to have significant correlation with patient reported symptoms and findings in nasal endoscopic examination (NE). LNX can be considered as a useful objective tool in evaluation of children with adenoid hypertrophy. Primary care physicians or pediatricians can confidently use lateral neck X-ray for making clinical decisions and can consider nasopharyngoscopy when clinical picture remains unclear or more evaluation is needed.
Keywords: Adenoids, Adenotonsillectomy, Adenotonsillar hypertrophy, Adenotonsillectomy, Neck X-ray
Introduction
Adenoids, also known as nasopharyngeal tonsils are normal lymphoid tissues present on posterior wall of nasopharynx, forming a part of Waldeyer’s ring at the entry of upper respiratory tract. Adenoids are the first site of immunological contact for inhaled antigens in early childhood. They produce B cells, which give rise to IgG and IgA plasma cells, provides natural acquired immunity in early childhood and appears to have an important role in development of an ‘immunological memory’ in younger children [1]. Adenoids become evident by 6 months to 1 year of life, increases rapidly in size during first 6–8 years of life and generally atrophies by 15 years of age in most children [2]. The growth of adenoid tissues is not in agreement with the growth of the bony nasopharynx, leading to nasal obstructive symptoms of adenoid hypertrophy (AH), which is described as the most common cause of nasal obstruction in pediatric populations [3, 4].
Most well-known clinical symptoms of AH are upper air way obstruction, reccurent otitis media, obstructive sleep apnoea, pediatric chronic rhinosinusitis, failure to thrive and craniofacial developmental anomalies. Other symptoms of AH are mouth breathing, snoring, cough, speech disturbance, lethargy and poor academic or scholastic performances. Recently children with AH are found to have increased association with nocturnal enuresis, attention deficit hyperactivity disorder, pulmonary hypertension and right heart failure. These clinical symptoms are more common in young pediatric population because of relatively small volume of nasopharynx and increased frequency of upper respiratory tract infections [3–6].
Most of the time, pediatrician is the first to see these children and they mostly rely on clinical assessment with or without some investigations to refer these children to otorhinolaryngologist. Numerous methods have been described for evaluation of AH, like history, physical examination, palpation, posterior rhinoscopic mirror examination (PR), nasal endoscopic examination (NE), lateral neck X-ray, magnetic resonance imaging (MRI) and acoustic rhinometry (AR). But most of these methods are not possible to follow in busy pediatric outpatient unit either because of lack of cooperation from child (palpation, PR, NPL) or due to limited availability of test or due to cost constraints (NE, MRI, AR) etc. [4, 7, 8].
Lateral neck X-rays (LNX) have long been used as a diagnostic tool in AH. They are simple, cost effective, readily available and reproducible [8]. This study has been conducted to determine the diagnostic accuracy of LNX for assessing AH and to assess the correlation between adenoid size in LNX and clinical symptoms in a pediatric unit.
Materials and Methods
Study Setting
This prospective study was conducted by Department of Otolaryngology in association with Department of Pediatrics at Padmavathy Medical Foundation, Kerala during the period January 2015 to March 2016. The study was approved by institutional ethics committee and informed consents were obtained from the parents.
Study Population
60 consecutive children of both genders, between the age group of 5 to 14 years, attending Department of Pediatrics with a provisional diagnosis of AH for the first time were included in the study.
Children with history of previous adenotonsillectomy, having acute respiratory tract infections, septal deviations, nasal polyps, anatomic abnormalities like cleft palate, syndromic children or those with mental retardation were excluded from the study. Parents of children who were not willing to enroll for study or those children presenting directly to department of otorhinolaryngology were also excluded from the study.
Symptom Scores
Structured questionnaires were administered to parents or caregivers to collect the demographic data and clinical information about presence or absence of symptoms of AH as described by Contencin P [9]—explained in Table 1.
Table 1.
Contents of medical questionnaire for parents
| Day time symptoms | ||
| Failure to thrive | Yes | No |
| Thinness (general aspect) | Yes | No |
| Rhinolalia clausa | Yes | No |
| Permanent mouth breathing | Yes | No |
| Reccurent rhinitis/rhinopharyngitis | Yes | No |
| Sleepiness | Yes | No |
| Night time symptoms | ||
| Observed apneas (respiratory obstructions) | Yes | No |
| Snoring: in case of URTI | Yes | No |
| Intermittent (even with no infection) | Yes | No |
| Habitual, permanent | Yes | No |
The original questionnaire was modified by the authors, so that, instead of “Yes” or “No” answers, a score of “1” or “0” was given. The total score was then calculated which ranges between 0 (minimum) to 10 (maximum). Based on the final symptom score (SS), the children were categorized into four different groups – Groups S1/Mild symptoms (score ranging between 0 and 2), Group S2/Moderate symptoms (score between 3 and 5), Group S3/Moderate to severe (score of 6 or 7) and Group S4/Severe symptoms (score between 8 and 10).
Radiogarphic Grading
Enrolled children were advised to have a digital X-ray of neck lateral view, in standing position, such that Frankfurt plane is parallel to floor and the X-ray beams are centered to external auditory meatus. The children were instructed to breathe through the nose, keeping the mouth closed and teeth occluded [10]. All images were acquired with the same machine, with identical settings and by same radiologist. Those children with significant rotation of head or elevated soft palate were later excluded from the study group.
The LNX were interpreted as per guidelines provided by Fujioka et al. [11], which is the most accepted and commonly followed method of interpreting LNX for assessing the AH. To avoid inter-observer variations, all LNX were evaluated by the same pediatrician. Adenoid depth (AD) thickness was measured by drawing a perpendicular line from a line drawn along the straight part of anterior margin of basi-occiput to the most convex part of adenoid pad. Nasopharyngeal depth (ND) was calculated by drawing another line between the spheno-occipital synchondrosis to posterosuperior edge of hard palate—Fig. 1.
Fig. 1.
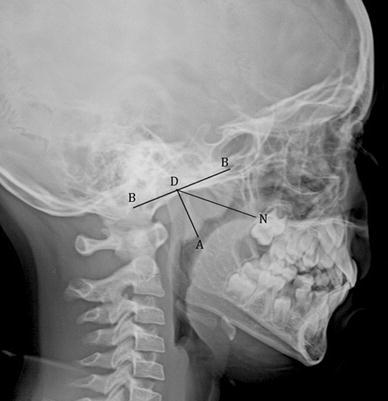
Plain radiograph of nasopharynx lateral view (LNX) showing how adenoidal—nasopharyngeal ratio was calculated. BB: Line drawn along straight part of anterior margin of basiocciput; AD: Adenoid depth (perpendicular line from BB to most convex part of adenoid pad); ND: Nasopharyngeal depth (line between spheno-occipital synchondrosis to posterior edge of hard palate); ANR calculated by dividing AD with ND
The adenoid-to-nasopharyngeal ratio (ANR) was then calculated from all images by dividing AD with ND. The value was then documented in percentage by multiplying with 100. Based on the ANR, the subjects were then categorized into 4 groups; Group X0—0–25%, Group X1—25–50%, Group X2—50–75% and Group X3—75–100%.
Endoscopic Grading
All children were then referred to department of otorhinolaryngology for a nasal endoscopic (NE) examination the same day. All children were examined by a single senior otorhinolaryngologist who was blinded to the clinical data and X-ray findings. The nasal endoscopy was performed with a 2.7 mm rigid pediatric nasal endoscope by Karl Storz (Germany) after achieving topical decongestion and anesthesia with 4% xylocaine with 1:10,000 adrenaline solutions. Choanal images were obtained with help of a Storz HD camera unit.
The images were analyzed using Adobe photoshop CS5 version 12 software (Adobe, USA). Based on the degree of AH, patients were categorized into 4 grades (I–IV) as described by Ysunza [12] et al. Grade I (None) consists less than 25% of scarce tissue at choanal opening, Grade II (Mild) with more than 25% but less than 50% of obstruction confined to upper half of nasopharynx cavity and with a patent choanae. Grade III (Moderate) with more than 50% but less than 75% obstruction, with free airway only in inferior area. Grade IV (Severe) was more than 75% or practically complete choanal obstruction.
Correlation of Data
Statistical analysis was done among different groups to find the correlation between SS and ANR, ANR and NE, SS and NE. Considering NE Scores as the gold standard, the sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and diagnostic accuracy (DA) of ANR in LNX was assessed.
Statistical Analysis
Statistical analysis was performed with SPSS software (SPPS 16.0, SPSS Inc, Chicago, IL). Correlation between symptoms scores, LNX grades and NE grades were calculated with Pearson correlation. A value of p < 0.05 was considered statistically significant.
Results
After applying the exclusion criteria, a total of 48 patients were evaluated. They aged between 5 and 14 years with a mean age of 5.2 and standard deviation of 2.3 years. There were 26 (54.16%) males and 22 (45.83%) females.
Nasal obstruction followed by snoring was the most common symptoms in the study population. Many children had more than one symptom. These details are summarized in Table 2.
Table 2.
Presenting symptoms
| Symptoms | Present in | |
|---|---|---|
| n | % | |
| Nasal obstruction | 44 | 91.66 |
| Mouth breathing | 42 | 87.50 |
| Snoring | 38 | 79.16 |
| Reccurent rhinitis | 37 | 77.08 |
| Sleepiness | 22 | 45.83 |
| Failure to thrive | 4 | 8.33 |
When the symptom scores were calculated, majority were of Group S4 (n = 22, 45.83%) and Group S3 (n = 18, 37.5%). 6 (12.5%) were of Group S2 and 2 (4.16%) were from Group S1.
When ANR was calculated majority of subjects were of Group X3 (n = 24, 50.00%) and X4 (n = 21, 43.75%). 3 (6.25%) subjects belonged to Group X2. No subjects were registered in Group X1.
During NE, 2 (4.16%) subjects were having Grade I hypertrophy, 3 (6.25%) had Grade II, 21 (43.75%) having Grade III and 22 (45.83%) were having Grade IV adenoid hypertrophy. These results are summarized in Table 3.
Table 3.
Summarization of symptom score groups, ANR groups and NPL groups
| SS groups | n | % | ANR groups | n | % | NPL groups | n | % |
|---|---|---|---|---|---|---|---|---|
| Group S1 | 2 | 4.16 | Group X1 | 0 | 0 | Grade I | 2 | 4.16 |
| Group S2 | 6 | 12.5 | Group X2 | 9 | 18.75 | Grade II | 3 | 6.25 |
| Group S3 | 18 | 37.5 | Group X3 | 19 | 39.58 | Grade III | 21 | 43.75 |
| Group S4 | 22 | 45.83 | Group X4 | 20 | 41.66 | Grade IV | 22 | 45.83 |
When statistical analysis was done, there was a highly significant correlation between SS and ANR groups (p < 0.005). When ANR results were compared with NE groups, the result was statistically significant (p = 0.027). We also did a correlation analysis between SS and NE groups, which was also found to be statistically significant (p < 0.001).
We got a sensitivity of 88.37%, specificity of 80.00%, positive predictive value of 97.43% (86.81–99.54% at 95% confidence interval), negative predictive value of 44.44% (18.87–73.33% at 95% confidence interval) for ANR in LNX. The overall diagnostic accuracy of the ANR in LNX for detecting AH was 87.50%.
Discussion
LNX are generally used by pediatricians to estimate AH in clinics, based on which they may decide to choose the treatment, which can be follow-up or operation [13]. Fourteen studies were done previously between the period 1992-2016, to assess AH by using ANR in LNX. They all reported conflicting results [3, 13–24]. All these studies used NE as the reference standard to which LNX data were compared. Results of ten of these studies [3, 13–21] were similar to that of ours, showing a significant correlation between ANR in LNX and AH in NE. Four authors [12, 22–24] reported that there exist no correlation between ANR in LNX and AH in NE.
Only four authors [12, 15, 17, 24] calculated sensitivity, specificity, positive predictive value, negative predictive value of AH to LNX. There values were ranging between 41 and 100%, 55 and 95%, 66.7 and 94%, 41 and 75%. Our values for these indices were 88.37, 80.00, 97.43 and 44.44% respectively.
Only Kurien et al. [17] and Barbosa et al. [21] calculated the diagnostic accuracy of AH to LNX in literature. They estimated 65 and 83.3% respectively. Our value 87.5% calculated was very close to that of Barbosa et al.
The variations in results of our study with the previous studies may be due to differences in standardization of clinical symptoms or usage of different methods (objective [16, 19, 20] or subjective [12, 15]) for radiological and endoscopic classification of AH. The main strength of our study is that we used an objective measure for both index test (LNX) and reference test (NE).
Although nasopharyngoscopy examination (flexible or rigid) is the gold standard for diagnosis of AH, this is not easily available in many centers. When it is available, it is an invasive procedure and many children mayn’t cooperate for an endoscopic examination. The cost of undergoing an endoscopic examination also is higher. These factors limit the use of nasopharyngoscopy examination in diagnosis of AH [3].
In contrast to nasal endoscopy, lateral neck Xrays are cheap, readily available, non-invasive option for evaluation of AH. Different methods are available for estimation of adenoid size in LNX [3, 8]. In our study and various other studies [3, 13– 21], ANR measurement is found to be a very reliable and valid diagnostic test for AH.
The limitations of LNX are risk of exposure to radiations, the adenoid shadow obtained is a two-dimensional image of a three-dimensional structure which may not correctly represent the adenoid hypertrophy in all planes. There may be superimposition of anatomic structures and inter-observer variations in interpreting the X-rays [3]. Positional changes and respiratory movements may also affect the X-ray images [13].
Conclusions
Adenoid hypertrophy is the most common cause of nasal obstruction in pediatric population having a negative impact on quality of life of children and caregivers. Various diagnostic modalities are available for determination of adenoid hypertrophy. But the limited availability, increased cost, lack of cooperation from child etc. limits the use of these in routine practive. LNX with calculation of adenoid-to-nasopharynx ratio is found to have significant correlation with endoscopic examination and can be considered as a useful objective tool in evaluation of children with adenoid hypertrophy. Pediatricians can confidently rely on LNX for making clinical decisions and can consider nasopharyngoscopy when clinical picture remains unclear or more evaluation is needed.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from parents of all individual participants included in the study.
References
- 1.Wysocka J, Hassmann E, Lipska A, Musiatowicz M. Naive and memory T cells in hypertrophied adenoids in children according to age. Int J Pediatr Otorhinolaryngol. 2003;67(3):237–241. doi: 10.1016/S0165-5876(02)00374-9. [DOI] [PubMed] [Google Scholar]
- 2.Vogler RC, Ii FW, Pilgram TK. Age-specific size of the normal adenoid pad on magnetic resonance imaging. Clin Otolaryngol Allied Sci. 2000;25(5):392–395. doi: 10.1046/j.1365-2273.2000.00381.x. [DOI] [PubMed] [Google Scholar]
- 3.Adedeji TO, Amusa YB, Aremu AA. Correlation between adenoidal nasopharyngeal ratio and symptoms of enlarged adenoids in children with adenoidal hypertrophy. Afr J Paediatr Surg. 2016;13(1):14. doi: 10.4103/0189-6725.181701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pagella F, Pusateri A, Chu F, Cairello F, Benazzo M, Matti E, Marseglia GL. Adenoid assessment in paediatric patients: the role of flexible nasal endoscopy. Int J Immunopathol Pharmacol. 2011;24(4 suppl):49–54. doi: 10.1177/03946320110240S410. [DOI] [PubMed] [Google Scholar]
- 5.Somuk BT, Bozkurt H, Göktaş G, Demir O, Gürbüzler L, Eyibilen A. Impact of adenotonsillectomy on ADHD and nocturnal enuresis in children with chronic adenotonsillar hypertrophy. Am J Otolaryngol. 2016;37(1):27–30. doi: 10.1016/j.amjoto.2015.08.003. [DOI] [PubMed] [Google Scholar]
- 6.Tezer MS, Karanfil A, Aktaş D. Association between adenoidal–nasopharyngeal ratio and right ventricular diastolic functions in children with adenoid hypertrophy causing upper airway obstruction. Int J Pediatr Otorhinolaryngol. 2005;69(9):1169–1173. doi: 10.1016/j.ijporl.2005.01.001. [DOI] [PubMed] [Google Scholar]
- 7.Baldassari CM, Choi S. Assessing adenoid hypertrophy in children: X-ray or nasal endoscopy? Laryngoscope. 2014;124(7):1509–1510. doi: 10.1002/lary.24366. [DOI] [PubMed] [Google Scholar]
- 8.Lertsburapa K, Schroeder JW, Sullivan C. Assessment of adenoid size: a comparison of lateral radiographic measurements, radiologist assessment, and nasal endoscopy. Int J Pediatr Otorhinolaryngol. 2010;74(11):1281–1285. doi: 10.1016/j.ijporl.2010.08.005. [DOI] [PubMed] [Google Scholar]
- 9.Contencin P, Malorgio E, Noce S, Couloigner V, Vigo A. Questionnaire and nocturnal oxymetry in children with adenotonsillar hypertrophy. Eur Ann Otorhinolaryngol Head Neck Dis. 2010;127(4):137–142. doi: 10.1016/j.anorl.2010.06.001. [DOI] [PubMed] [Google Scholar]
- 10.Feres MF, de Sousa HI, Francisco SM, Pignatari SS. Reliability of radiographic parameters in adenoid evaluation. Braz J Otorhinolaryngol. 2012;78(4):80–90. doi: 10.1590/S1808-86942012000400016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fujioka M, Young LW, Girdany BR. Radiographic evaluation of adenoidal size in children: adenoidal-nasopharyngeal ratio. AJR Am J Roentgenol. 1979;133(3):401–404. doi: 10.2214/ajr.133.3.401. [DOI] [PubMed] [Google Scholar]
- 12.Ysunza A, Pamplona MC, Ortega JM, Prado H. Video fluoroscopy for evaluating adenoid hypertrophy in children. Int J Pediatr Otorhinolaryngol. 2008;72:1159–1165. doi: 10.1016/j.ijporl.2008.03.022. [DOI] [PubMed] [Google Scholar]
- 13.Acar M, Kankilic ES, Koksal AO, Yilmaz AA, Kocaoz D. Method of the diagnosis of adenoid hypertrophy for physicians: adenoid-nasopharynx ratio. J Craniofac Surg. 2014;25(5):e438–e440. doi: 10.1097/SCS.0000000000000952. [DOI] [PubMed] [Google Scholar]
- 14.Wang DY, Bernheim N, Kaufman L, Clement P. Assessment of adenoid size in children by fibreoptic examination. Clin Otolaryngol Allied Sci. 1997;22:172–177. doi: 10.1046/j.1365-2273.1997.00002.x. [DOI] [PubMed] [Google Scholar]
- 15.Feres MF, Hermann JS, Cappellette M, Pignatari SS. Lateral X-ray view of the skull for the diagnosis of adenoid hypertrophy: a systematic review. Int J Pediatr Otorhinolaryngol. 2011;75(1):1–11. doi: 10.1016/j.ijporl.2010.11.002. [DOI] [PubMed] [Google Scholar]
- 16.Cho JH, Lee DH, Lee NS, Won YS, Yoon HR, Suh BD. Size assessment of adenoid and nasopharyngeal airway by acoustic rhinometry in children. J Laryngol Otol. 1999;113:899–905. doi: 10.1017/S0022215100145530. [DOI] [PubMed] [Google Scholar]
- 17.Kurien M, Lepcha A, Mathew J, Ali A, Jeyaseelan L. X-rays in the evaluation of adenoid hypertrophy: it’s role in the endoscopic era. Indian J Otolaryngol Head Neck Surg. 2005;57:45–47. doi: 10.1007/BF02907627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kindermann CA, Roithmann R, Lubianca JF. Neto, sensitivity and specificity of nasal flexible fiberoptic endoscopy in the diagnosis of adenoid hypertrophy in children. Int J Pediatr Otorhinolaryngol. 2008;72:63–67. doi: 10.1016/j.ijporl.2007.09.013. [DOI] [PubMed] [Google Scholar]
- 19.Caylakli F, Hizal E, Yilmaz I, Yilmazer C. Correlation between adenoid–nasopharynx ratio and endoscopic examination of adenoid hypertrophy: a blind, prospective clinical study. Int J Pediatr Otorhinolaryngol. 2009;73:1532–1535. doi: 10.1016/j.ijporl.2009.07.018. [DOI] [PubMed] [Google Scholar]
- 20.Monteiro EC, Pilon RR, Dall'Oglio GP. Study of enlarged adenoids: endoscopy versus radiography of the nasophrynx. Braz J Otorhinolaryngol. 2000;66:9–12. [Google Scholar]
- 21.Marcelo de Castellucci e Barbosa, Luégya Amorim Henriques Knop, Marcus Miranda Lessa, Telma Martins de Araujo (2009) Avaliação da rdiografia cefalométrica lateral como meio de diagnóstico da hipertrofia de adenóide. Revista Dental Press de Ortodontia e Ortopedia Facial 14(4):83–91
- 22.Mlynarek Alex, Tewfik Marc A., Hagr Abdulrahman, Manoukian John J., Schloss Melvin D., Tewfik Ted L., Choi-Rosen Jeanne. Lateral Neck Radiography versus Direct Video Rhinoscopy in Assessing Adenoid Size. The Journal of Otolaryngology. 2004;33(06):360. doi: 10.2310/7070.2004.03074. [DOI] [PubMed] [Google Scholar]
- 23.Ysunza Antonio, Pamplona M. Carmen, Ortega Juan M., Prado Héctor. Video fluoroscopy for evaluating adenoid hypertrophy in children. International Journal of Pediatric Otorhinolaryngology. 2008;72(8):1159–1165. doi: 10.1016/j.ijporl.2008.03.022. [DOI] [PubMed] [Google Scholar]
- 24.Wormald PJ, Prescott CAJ. Adenoids: comparison of radiological assessment methods with clinical and endoscopic findings. J Laryngol Otol. 1992;106(04):342–344. doi: 10.1017/S0022215100119449. [DOI] [PubMed] [Google Scholar]


