Abstract
The increase awareness and advent of anti-tuberculosis therapy led to decline in tuberculosis. Now a resurgence of tuberculosis is with immunosuppression and with resistant strains. The detection rate of extrapulmonary is increased with the advent of newer modalities of detection, imaging, and better testing. This case series documents our experience with seven cases of primary spheno-petro-clival lesion and details of the clinical and radiological presentations of these patients. Intraoperative obtained tissue was send for histopathological and microbiological evaluation. The most common symptoms were headache and nasal discharge. The final diagnosis of spheno-petro-clival tuberculosis was confirmed in all cases with histopathology and by culture post-operatively. Skull base tuberculosis is relative rare entity in past because of late occurrence of specific symptom, incomplete radiological evaluation and it may present as neck swelling by travelling through various neck spaces. (1) Tubercular infection should be considered as differential in skull base lesion as pickup rate is increasing with advancement in technology. (2) Two of our cases had retropharyngeal abscess have focus in skull base bone. The skull base, hence, may be one of foci in undetermined sites of tuberculous infections and should be searched for.
Keywords: Tuberculosis, Spheno-petro-clival region, Skull base, Infection, Paranasal sinuses
Introduction
The tuberculosis, though common in Indian Subcontinent, is a perplexing problem if presentation is at Otolaryngology subsides. The presentation of patients with lesions at sites of middle skull base in region of petro-spheno-clival complex prompts the clinicians for considering aggressive surgical excisions which are often fraught with complications and morbidity. The resurgence of tuberculosis is being a grave concern with prolonged suppression with immunosuppression and better longevity of HIV cases [1]. Obviously, since the tumours and fungal infections are much more common in these subsides, the diagnosis of Tuberculosis is not “clinched” easily in most cases. With the advent of newer modalities of detection, imaging, and better testing, the clinicopathologic pick up rates of this masquerade have increased [2, 3].
Here we describe our experience with cases of spheno-petro-clival tuberculosis noted in our practice.
Case Series
Chart review of all cases of spheno-petro-clival tuberculosis diagnosed over last 15 years was performed. All the patients were evaluated by our normal protocol which includes history, systemic and local examination. The symptoms and sign are summarized in Tables 1 and 2. The patients were referred to us with prior radiological investigations. Out of 7 referred patients, three patients came with CT of nose and paranasal sinuses (PNS) and two patients with MRI. The radiological picture consistently revealed heterogeneous mass with erosion of surrounding bone in spheno-petro-clival region (Figs. 1, 2, 3). The possibility of clival cordoma, invasive aspergillosis and low grade malignancies were kept in these cases. The patient with retropharyngeal bulge, the differential diagnosis was schwannoma and low grade malignancy. Intraoperative cheesy material with granulation was found in sphenoid sinus. The cases with retropharyngeal bulge, pus and straw colour fluid came out via puncture site for transoral local infiltration. The granulation tissue with cheesy material and fluid were send for histopathological and microbiological evaluation.
Table 1.
Summary of clinical features and diagnosis
| S. no. | Age/sex | Duration of symptoms (months) | Signs | Systemic symptoms | Local symptoms | Imaging | |
|---|---|---|---|---|---|---|---|
| Scan | Finding | ||||||
| 1 | 24/F | 3 |
Pallor Projection of light in left eye Left lateral rectus palsy |
Occipital headache, mild fever, weight loss | Progressive decrease in vision and diplopia—left eye | CT brain and PNS (C and A cuts) | Heterogenous expensile mass eroding petro-clivus with extension into sphenoid sinus posterior part |
| 2 | 35/f | 3 | No | Occipital headache, fever and weight loss | Post nasal discharge | Ct Scan Pns And nose | Heterogenous mass involving sphenoid sinsus with extension in paraclival lesion |
| 3 | 62/M | 4 | Smooth bulge in posterior wall of oropharynx, nasopharynx and hypopharynx | No | Dysphagia and bilateral nasal obstruction | CECT-PNS | Heterogenous well defined mass in front of vertebre from clivus to hypopharynx with clival erosion |
| 4 | 15/M | 24 | Nasal endoscopy showed granulation in sphenoid sinus | Headache | Ear discharge/nasal discharge history of right MRM | No | No |
| 5 | 41/F | 2 | Grade 1 nystagmus | Global headache | No | MRI | Hypointense mass in right petrous bone, with extension in sphenoid sinus right side |
| 6 | 16/m | 5 | No | Weight loss decrease appetite | Blood stained nasal discharge | MRI | ISOINTENSE mass in sphenoid and paraclival region |
| 7 | 16/m | 12 | Left side level 2 and 3 smooth soft swelling with bulge in posterior pharyngeal wall | No | Swelling neck | CECT | Heterogenous expensile mass eroding petro apex with extension into retropharyngeal and left parapharyngeal space |
Table 2.
Summary of management and outcome
| S. no. | Surgical treatment | Finding | Medical treatment | Duration in months | Follow up | Outcome |
|---|---|---|---|---|---|---|
| 1 | Endoscopic Endonasl biopsy | Casseous material in sphenoid sinus | ATT | 18 | Regular | Improvement in symptoms and vision |
| 2 | Endoscopic Endonasl biopsy | Casseous material in sphenoid sinus | ATT | 18 | Regular | Improved |
| 3 | Transoral incision and drainage | Yellow colour pus | ATT | 18 | Regular | Improved |
| 4 | Endoscopic Endonasl biopsy | Granulation in sphenoid sinus | ATT | 18 | Regular | Improved |
| 5 | Endoscopic Endonasl biopsy | Granulation with yellow discharge in sphenoid sinus | ATT | 18 | Regular | Improved |
| 6 | Endoscopic Endonasl biopsy | Casseous material in sphenoid sinus | ATT | 18 | Regular | Improved |
| 7 | Transoral incision and drainage | Straw colour fluid | ATT | 18 | Regular | On treatment, Improvement in symptoms continue |
Fig. 1.
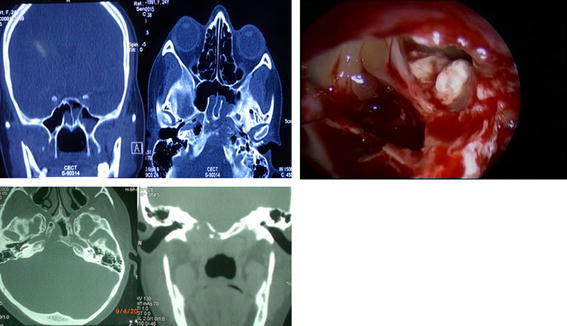
(Patient 1 and 2) NCCT revealed heterogenous mass in sphenoid sinus with erosion of posterior wall and roof and extension in right petrous apex region. The intraoperative photograph of patient 1 revealing white colour cheesy mass in sphenoid sinus
Fig. 2.
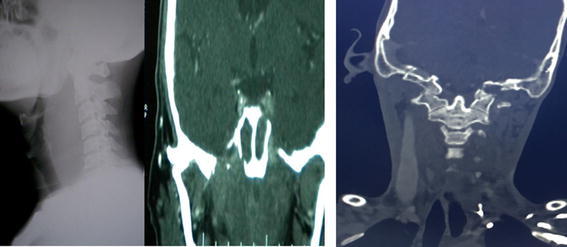
(Case 3 and 7) X ray soft tissue neck (lateral view) showing smooth bulge of prevertebral tissue and CECT revealed heterogenous mass in spheno-petero-clival region with erosion of surrounding bones
Fig. 3.

(Case 5 and 6) MRI showing isointense mass in spheno-clival region
Results
The age was ranged from 15 to 62 years with male preponderance. The symptoms and signs are none specific for spheno-petro-clival involvement. The patients were well educated with good socioeconomic background without co-morbidities. The most common symptoms were headache and nasal discharge. The 4th number patient in Table 1 was came with history of persistent ear discharge post modified radical mastoidectomy. Other patients had not complaint of ear symptoms and local examination including position of tympanic membrane was normal.
The final diagnosis of spheno-petro-clival tuberculosis was confirmed in all cases with histopathology and by culture post-operatively. After histopathology report, the patients were evaluated clinic-radiologically for primary site. The radiological investigations were X ray chest and USG abdomen. No extra focus was identified in all cases other than skull base bones. The serological testing and PCR were in positive for acid fast bacilli in all cases. The antitubercular therapy was started after audiological assessment. Five patients received complete anti-tubercular therapy (ATT) for 18 months and disease free from 5 to 10 years. The 2 patients are taking treatment and showing progressive improvement of symptoms.
Discussion
The diagnosis of skull base tuberculosis is difficult because of unusual presentation with similar symptomatology with malignancies, complex anatomy of region and less familiarity with otolaryngologist. On searching Pubmed and Google, the literature had documented tuberculosis involvement of the skull/calvarium in 0.1–3.7% of all cases of skeletal TB [4] and another report has noted of only two reported cases of isolated involvement of the skull base [5]. Recent years have however seen several case reports of skull base tuberculosis [6–8].
In the past retropharyngeal abscess, has been attributed to a focus in the cervical vertebrae. This report documents two patients with tubercular retropharyngeal abscess with a tubercular focus in the petro-clival region and throws open the possibility that some patients with no documented vertebral lesion in association with retropharyngeal cold abscess would have their primary focus not in the vertebrae but in the petrous bone. Previous anatomical texts have documented the pathways by which suppuration in the petrous may gravitate to the retropharyngeal and parapharyngeal space [9].
The common clinical manifestation of cranio-cervical vertebrae tuberculosis is pain, stiffness of neck by involved paraspinal muscles which was not seen in our case series as cervical vertebrae was not involved in any case. The possible pathology behind primary sphenoidal and clival bone involvement and secondary extension to petrous bone is entrapment of tubercular bacilli in mucosa of this region as these bones come in respiratory route. For appearance of radiolucent lesion on plain radiology, 30% demineralization of bone is required [10]. Plain radiology though a specific tubercular focus in the cervical vertebrae can localize lesion in 91–99% [11]. The advent of sectional imaging with CT and MR has probably resulted in increasing localisation of infection to the skull base as seen in this series.
Acknowledgements
We are thankful to Director and Head of Department for allowing us to use data.
Author Contribution
Dr Hitesh Verma was involved in designing, collection of data and drafting of article. Dr Smriti Panda, Dr Kapil Sikka and Dr David Victor Kumar Irugu were contributes in analysing and interpretation of data. Dr Alok Thakar was substantial contributions in conception, design, and final approval of article.
Compliance with Ethical Standards
Ethical Approval
This article does not contain any studies with human participants performed by any of the authors.
Informed Consent
The study is based on radiological finding and patient case file.
References
- 1.Miziara D. Tuberculosis affecting the oral cavity in Brazilian HIV-infected patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;100:179–182. doi: 10.1016/j.tripleo.2004.10.017. [DOI] [PubMed] [Google Scholar]
- 2.Lee DK, Cho K-T, Im S-H, Hong S-K. Craniovertebral junction tuberculosis with atlantoaxial dislocation: a case report and review of the literature. J Korean Neurosurg Soc. 2007;42:406–409. doi: 10.3340/jkns.2007.42.5.406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Suslu HT, Gulec L, Bozbua M. Frontal bone and epidural tuberculosis. Turkish Neurosurg. 2008;18(1):78–81. [PubMed] [Google Scholar]
- 4.Sethi A, Sethi D, Mrig S, Passey JC, Srivastav N. Coexistent acute pyogenic and tubercular petrous apicitis: a diagnostic dilemma. J Laryngol Otol. 2006;120(10):875–878. doi: 10.1017/S0022215106000843. [DOI] [PubMed] [Google Scholar]
- 5.Sharma SC, Baruah P. Sphenoid sinus tuberculosis in children-a rare entity. Int J Pediatr Otorhinolaryngol. 2003;67(4):399–401. doi: 10.1016/S0165-5876(02)00381-6. [DOI] [PubMed] [Google Scholar]
- 6.Turel MK, Rajshekhar V. Sphenoid sinus tuberculosis: a rare cause of visual dysfunction in an adolescent girl. Neurol India. 2013;61(2):179–180. doi: 10.4103/0028-3886.111138. [DOI] [PubMed] [Google Scholar]
- 7.Shenoy SN, Raja A. Tuberculous granuloma of the spheno-clival region. Neurol India. 2004;52(1):129–130. [PubMed] [Google Scholar]
- 8.Nayak B, Patnaik S, Sahoo PK, Biswal D. Craniocervical junction tuberculosis: usual pathology at an unusual site. Surg Neurol Int. 2015;6:115. doi: 10.4103/2152-7806.159835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hollinshead WH. Anatomy for surgeons: vol 1: the head and neck. 3. Philadelphia: Harper and Row; 1982. p. 275. [Google Scholar]
- 10.Chauhan A, Gupta BB. Spinal tuberculosis. Indian Acad Clin Med. 2007;8:110–114. [Google Scholar]
- 11.Dass B, Puet TA, Watanakunakorn C. Tuberculosis of the spine (Pott’s disease) presenting as ‘compression fractures’. Spinal Cord. 2002;40:604–608. doi: 10.1038/sj.sc.3101365. [DOI] [PubMed] [Google Scholar]


