Abstract
Cherubism might occur in solitary cases or in several members of the family, often in many generations. Treatment depends on the clinical course of the disease. The reported case is an example of solitary sporadic occurrence within a family, which is a less documented condition in the literature.
Keywords: Fibro-osseous lesions, Cherubism, Familial, Giant cells
Introduction
Fibro osseous lesions (FOLs) are poorly defined group of lesions which affect the craniofacial bones [1]. Cherubism is an uncommon fibro-osseous disorder of the jaws. It is an inherited autosomal dominant disorder affecting jaw characterized by replacement of normal bone by proliferation of fibro vascular tissue containing multinucleated giant cells [2]. Some cases also presented without familial histories [3, 4]. Although the condition is known to regress spontaneously at puberty, surgical management is sometimes required for cosmetic reasons.
Case Report
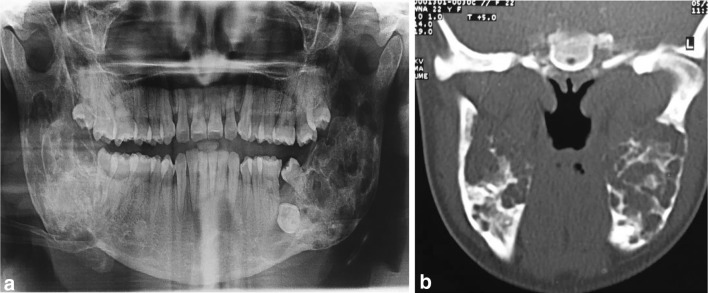
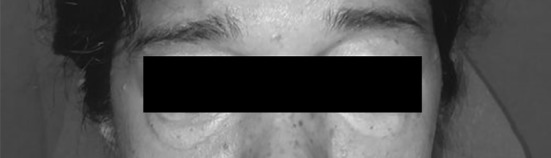
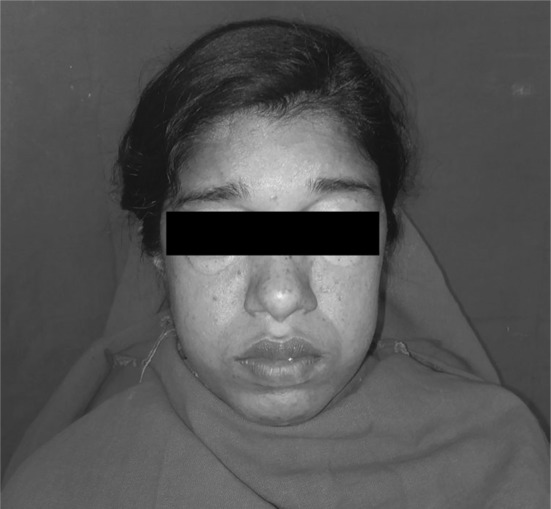
A 25 year old female patient presented with chief complaint of pain on the left side of face for the last 3–4 years. Patient gave history of raised cholesterol levels and was on medication for the same since 3 years and was also taking medication for swelling on both eyes. No Family history for any kind of bone disease was elicited. Soft tissue biopsy was taken from left vestibular region suggestive of intraosseous giant cell fibrosseous lesion 4 years back. On examination, there was presence of periorbital swelling (Fig. 1) and the skin was pale bilaterally (Fig. 2). On extraoral palpation, bilateral firm, hard, non tender swelling was present on the angle of mandible and the ramus region. Intraorally, firm, hard, non tender swelling was present in the right and left mandibular ramus and posterior alveolus. Expansion of both cortical plates, with normal overlying mucosa in mandible but maxilla was unaffected. Generalized gingival inflammation and bleeding on probing was present. On radiological examination, Orthopantamograph and CT scan (Fig. 3) bilateral, multilocular, radiolucent lesion with thinning of cortical plates were present and displacement of unerupted teeth. Thyroid function test and the calcium levels were within the normal range differentiating it from hyperparathyroidism. Diagnosis of Cherubism was made. Since the disorder spontaneously regress after puberty hence no surgical intervention was undertaken for the moment and follow-up evaluation was advised. Pain was of periodontal origin and appropriate treatment in the form of scaling and root planning was done.
Fig. 1.
Periorbital swelling
Fig. 2.
Bilaterally pale skin
Fig. 3.
a OPG showing multiple bilateral radiolucencies and displaced teeth. b Axial section of CT scan showing bilateral radiolucencies
Discussion
Cherubism was first recognized in 1933 by William A. Jones as gradually enlarging, painless, bilateral swelling of jaws and swollen cheeks accompanied by upward-looking of eyes. This condition gives patient the appearance of “cherubs” [2, 3].
Two forms exist hereditary (familial) and nonhereditary (nonfamilial) [2, 3]. The gene was mapped to chromosome 4P16.3. The clinically conspicuous disturbance in osteogenesis and possible relation to tooth development, as well as the location of the gene in an interval between D4S127 and the telomere of 4p, suggested that the genes FGFR3 and MSX1, are causative for this disease. There is an influence of SH3BP2 on the regulation of the receptor for PTH and PTH related protein (PTHrP) [2, 4].
Clinical or radiographic findings of cherubism are not evident until the age of 14 months to 3 years. Frequently, cherubism is accompanied by abnormalities in the configuration of dental arch and dental eruption. In severe cases, tooth resorption occurs. The signs and symptoms of disease depend on the severity of the condition, range from clinically, radiologically undetectable features to grossly deformed jaws, upright palate, respiratory obstruction and impairment of vision and hearing.
The syndromes associated with cherubism are neurofibromatosis type I, Noonan-like/multiple giant cell lesion syndrome, Ramon syndrome and Jaffe–Campanacci syndrome [4, 5].
Differential diagnosis should include, McCune—Albright syndrome, central giant cell reparative granuloma, brown tumors, true giant cell tumor, infantile hyperosteosis, familial gigantism cementoma, ameloblastoma, myxoma, lesions containing giant cells such as hyperparathyroidism and osteomalasia [2].
Biochemical investigations can show normal limits of serum calcium and phosphorus concentrations, TSH, FSH, LH, T4 and T3 levels but elevated levels of alkaline phoshatase [2, 3].
Treatment of cherubism ranges from radical surgical reconstruction to wait and see. The cherubic appearance in a young patient may be highly traumatic to the psychosocial element of one’s personality, so surgical reconturing is required. Radiotherapy is contraindicated. Pharmacological intervention in form of calcitonin has been suggested but clinical evidence to endorse its application is still lacking [2, 6, 7].
Conclusion
In general, cherubism has a good prognosis. Cherubism does not progress after puberty, and as the patient grows to adulthood, the entire jawbone lesion tends to develop a more normal configuration. Surgery is not a treatment of choice. But in case of expansion of tissue resulting in difficulty with airway or chewing capacity, biopsy and surgical intervention can be done. Medical attention for aesthetic and functional concern is required.
Funding
This case report has not been financially supported by any person or institute.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
For this type of study, formal consent is not required.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Sunaina Singla, Email: dr.singla2013@gmail.com.
Ravi Narula, Email: ravinarula10@yahoo.com.
Ajay Mittal, Email: ajaymittal1189@yahoo.com.
Hirdepal Singh Brar, Email: hirdenote85@gmail.com.
References
- 1.Srichinthu KK, Yoithapprabhunath TR, Chitturi RT, Yamunadevi A, Potsangbam AD, Sningh DN. Fibro osseous lesions-classifications, pathophysiology and importance of radiology: a short review. Int Biol Biomed J Winter. 2016;2(1):11–20. [Google Scholar]
- 2.Kaur M, Shah S, Babaji P, Singh J, Nair D, Kamble SS. Cherubism: a rare case report. J Nat Sci Biol Med. 2014;5:488–491. doi: 10.4103/0976-9668.127330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Prajapati VK. Non-familial Cherubism. Contemp Clin Dent. 2013;4:88–89. doi: 10.4103/0976-237X.111609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Degala S, Mahesh KP, Monalisha Cherubism: a case report. J Maxillofac Oral Surg. 2015;14(1):S258–S262. doi: 10.1007/s12663-013-0474-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Seward GR, Hankey GT. Cherubism. Oral Surg Oral Med Oral Pathol. 1957;10(10):952–974. doi: 10.1016/S0030-4220(57)80047-4. [DOI] [PubMed] [Google Scholar]
- 6.Jain V, Gamanagatti SR, Gadodia A, Kataria P, Bhatti SS. Non-familial cherubism. Singap Med J. 2007;48:e253. [PubMed] [Google Scholar]
- 7.Mehrotra D, Kesarwani A, Nandlal Cherubism: case report with review of literature. J Maxillofac Oral Surg. 2011;10(1):64–70. doi: 10.1007/s12663-010-0164-y. [DOI] [PMC free article] [PubMed] [Google Scholar]