Cohort studies and randomized trials among hospitalized patients with acute and serious illnesses commonly use mortality as the primary or key secondary outcome measure. Death is a patient-centered outcome because nearly everyone wishes to avoid it. Despite this general preference, however, studies among healthy outpatients and those with serious illnesses show that a significant minority, and sometimes a majority, rate states such as severe dementia as worse than death.1–3
To our knowledge, there is no evidence as to whether patients with acute illnesses requiring hospitalization also consider certain states of debility as worse than death. This distinction is important because some evidence suggests that as death nears, people may choose more aggressive treatment options in an attempt to prevent it.4 We therefore sought to understand how hospitalized patients with serious illnesses would evaluate states of cognitive or functional debility relative to death.
Methods |
We conducted a prospective cohort study nested within a randomized trial of different approaches to decision making among 180 patients with serious illnesses who were hospitalized between July 1, 2015, and March 7, 2016, at an academic medical center in Philadelphia, Pennsylvania. The cohort study consisted of structured interviews with inpatients 60 years or older with advanced solid malignant neoplasms, hematologic malignant conditions, class III or IV congestive heart failure, or severe obstructive or restrictive lung disease. None of these patients had limitations on any life-sustaining treatment documented in their electronic medical records.
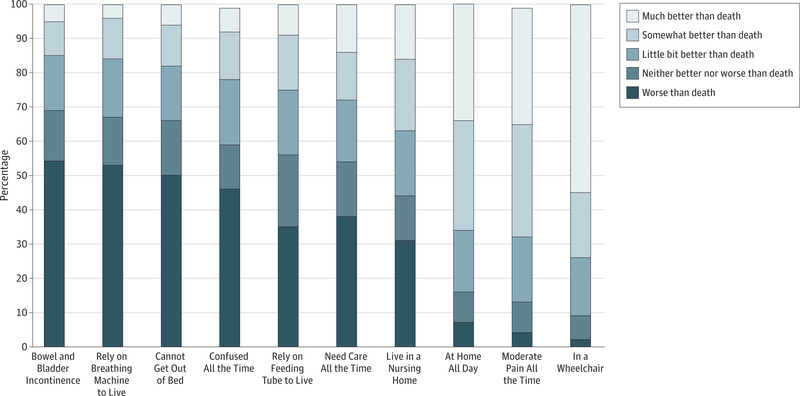
All patients were asked to evaluate health states with specific physical and cognitive debilities, dependencies on forms of life support, and dependencies on others to perform various activities (Figure). Patients rated each state on a 5-point Likert scale indicating whether they considered the state to be worse than death, neither better nor worse than death, a little better than death, somewhat better than death, or much better than death. Combinations of states were not evaluated. The University of Pennsylvania institutional review board approved the protocol and patients provided written informed consent.
Figure. Ratings of States of Functional Debility Relative to Death by Hospitalized Patients With Serious Illnesses.
Distribution of patient ratings of each queried health state on a 5-point Likert scale.
Results |
Patients displayed considerable heterogeneity in their ratings of health states relative to death (Figure), but significant percentages of patients rated each evaluated state of serious functional debility as equal to or worse than death. For example, a majority of respondents considered bowel and bladder incontinence (124 [68.9%]), requiring a breathing tube to live (121 [67.2%]), relying on a feeding tube to live (100 [55.6%]) and needing care from others all the time (97 [53.9%]) as health states the same or worse than death.
Discussion |
Hospitalized patients with serious and potentially life-limiting illnesses are at high risk for experiencing outcomes that many would consider to be worse than death. Nonetheless, studies of interventions in the hospital and specifically the intensive care unit, as well as hospital quality measures, commonly ignore such preferences, assuming implicitly or explicitly that death is an outcome to be avoided no matter what the alternatives are.5 This assumption may create untoward incentives for clinicians or health care systems to provide care that results in states of severe functional debility that patients prefer to avoid, even if the alternative is death.
There are many reasons why hospitalized patients with serious illnesses may receive care aimed at prolonging life when they are living in states they have deemed to be the same as or worse than death. Such reasons include changing preferences as death nears, belief that better health will be restored, willingness to endure undesirable states for the sake of family, surrogates’ or clinicians’ unawareness of the patient’s values, and clinicians’ failures to offer and implement alternatives that are more consistent with the patient’s priorities.
It is also possible that patients may underestimate their abilities to adapt to certain health states, such that once-feared states become more tolerable once they are experienced.6 Limitations of this study include the recruitment of patients from a single health care system and the solicitation of preferences for one-dimensional health states. Nonetheless, the fact that hospitalized patients with a broad range of serious illnesses so often viewed commonly encountered health states as worse than death should challenge researchers of patient-centered outcomes and those who develop quality measures to formulate and use new metrics such as the avoidance of states worse than death.
Acknowledgments
Funding/Support: This study was supported in part by grant T32HL098054 from the National Heart, Lung, and Blood Institute (Dr Rubin) and a grant from the Center for Health Incentives and Behavioral Economics at the University of Pennsylvania (Dr Rubin).
Role of the Funder/Sponsor: The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Conflict of Interest Disclosures: None reported.
Contributor Information
Emily B. Rubin, Pulmonary, Allergy and Critical Care Division, University of Pennsylvania, Philadelphia; Fostering Improvement in End-of-Life Decision Science Program, University of Pennsylvania, Philadelphia.
Anna E. Buehler, Fostering Improvement in End-of-Life Decision Science Program, University of Pennsylvania, Philadelphia.
Scott D. Halpern, Pulmonary, Allergy and Critical Care Division, University of Pennsylvania, Philadelphia; Fostering Improvement in End-of-Life Decision Science Program, University of Pennsylvania, Philadelphia; Center for Clinical Epidemiology and Biostatistics, University of Pennsylvania, Philadelphia; Department of Medical Ethics and Health Policy, Perelman School of Medicine, University of Pennsylvania, Philadelphia.
References
- 1.Patrick DL, Pearlman RA, Starks HE, Cain KC, Cole WG, Uhlmann RF.Validation of preferences for life-sustaining treatment: implications for advance care planning. Ann intern Med. 1997;127(7):509–51. [DOI] [PubMed] [Google Scholar]
- 2.Ditto PH, Druley JA, Moore KA, Danks JH, Smucker WD. Fates worse than death: the role of valued life activities in health-state evaluations. Health Psychol.1996;15(5):332–343. [DOI] [PubMed] [Google Scholar]
- 3.Fried TR, Van Ness PH, Byers AL, Towle VR, O’Leary JR, Dubin JA. Changes in preferences for life-sustaining treatment among older persons with advanced illness. J Gen intern Med. 2007;22(4):495–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bryce CL, Loewenstein G, Arnold RM, Schooler J, Wax RS, Angus DC. Quality of death: assessing the importance placed on end-of-life treatment in the intensive-care unit. Med Care. 2004;42(5):423–431. [DOI] [PubMed] [Google Scholar]
- 5.Harhay MO, Wagner J, Ratcliff SJ, et al. Outcomes and statistical power in adult critical care randomized trials. Am J Respir Crit Care Med. 2014;189(12): 1469–1478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ubel PA, Loewenstein G, Schwarz N, Smith D. Misimagining the unimaginable: the disability paradox and health care decision making. Health Psychol. 2005;24(4)(suppl):S57–S62. [DOI] [PubMed] [Google Scholar]