Abstract
Background
Although percutaneous dilatational tracheostomy (PDT) under bronchoscopic guidance is feasible in the intensive care unit (ICU), it requires extensive equipment and specialists. The present study evaluated the feasibility of performing PDT with a light source in the surgical ICU.
Methods
The study involved a retrospective review of the outcomes of patients who underwent PDT with a light source performed by a surgery resident under the supervision of a surgical intensivist in the surgical ICU from October 2015 through September 2016. During the procedure, a light wand was inserted into the endotracheal tube after skin incision. Then, the light wand and the endotracheal tube were pulled out slightly, the passage of light through the airway was confirmed, and the relevant point was punctured.
Results
Fifty patients underwent PDT with a light source. The average procedural duration was 14.0 ± 7.0 minutes. There were no procedure-associated deaths. Intraoperative complications included minor bleeding in three patients (6%) and paratracheal placement of the tracheostomy tube in one patient (2%); these were immediately resolved by the surgical intensivist. Two patients required conversion to surgical tracheostomy because of the difficulty in light wand insertion into the endotracheal tube and a very narrow trachea, respectively.
Conclusions
PDT with a light source can be performed without bronchoscopy and does not require expensive equipment and specialist intervention in the surgical ICU. It can be safely performed by a surgical intensivist with experience in surgical tracheostomy.
Keywords: intensive care units, light wand, percutaneous dilatational tracheostomy
Introduction
Tracheostomy is commonly performed in the intensive care unit (ICU) for patients requiring long-term mechanical ventilation or airway maintenance. Percutaneous dilatational tracheostomy (PDT) was first introduced in 1985 [1] and is based on a modification of the Seldinger principles. The procedure is relatively simple compared with surgical tracheostomy, and several studies have reported similar complication rates for PDT and surgical tracheostomy, concluding that PDT is feasible and safe for ICU patients [2].
With the introduction of bronchoscopy-guided PDT, the procedure is performed more easily at the bedside [3] and can be performed by a medical doctor rather than a surgeon [4]. However, any PDT procedure always requires surgical supervision and intervention for possible complications during the process. Bronchoscopy-guided PDT requires a bronchoscopist and an additional nursing assistant; in addition, large and expensive instruments with several devices must be placed around the ICU patients.
The present study evaluated the safety and feasibility of a novel technique for performing PDT with a light source, without bronchoscopic guidance, in the surgical ICU by reviewing the authors’ experience with this technique over a duration of 1 year.
Materials and Methods
This was a retrospective study. From October 2015 to September 2016, PDT with a light source was performed for all patients who were indicated for tracheostomy, with the exception of liver transplant patients, in the surgical ICU at Asan Medical Center. Liver transplant patients often have coagulopathy and may bleed excessively during or after the procedure. Thus, these patients underwent surgical tracheostomy with meticulous bleeding control measures.
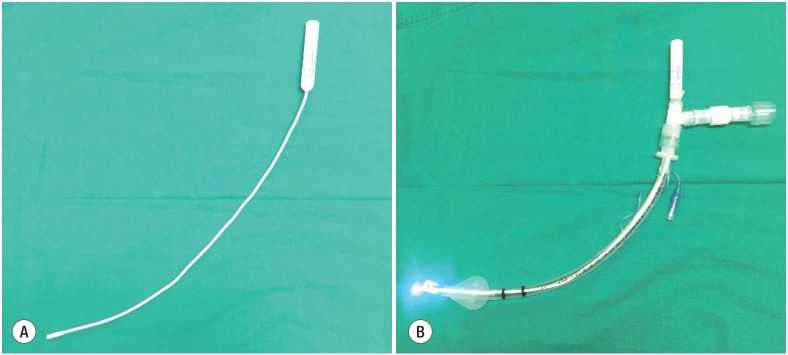
The patient preparation process was as follows. Except for patients with limited neck extension, such as those with cervical spine injuries, all patients were positioned with adequate neck extension using a pillow. Following adequate sedation, surgical draping, and the administration of a local anaesthetic, a skin incision was placed transverse to the midline, approximately 2 cm below the cricothyroid membrane. The pretracheal tissue was minimally dissected, and a light wand was inserted into the endotracheal tube after confirmation of the tracheal ring via palpation. The light wand (Figure 1A) is a device used for intubation in patients with a difficult airway. It was inserted in the swivel connector connected to the endotracheal tube, such that the light source of the wand was located at the end of the tube (Figure 1B). Following insertion, the light wand with the endotracheal tube was pulled out slightly so that the light passed through the incision site (Figure 2). Subsequently, the light source was fixed superior to the incision site; this enabled precise puncture of the trachea compared with identification of the tracheal ring by direct palpation. Following tracheal puncture, the procedure was completed using standard methods, and the light was removed with the endotracheal tube. A chest X-ray was obtained to confirm the location of the cannula and detect complications such as pneumothorax.
Figure 1.
(A) The light wand. (B) Light source located at the tip of endotracheal tube.
Figure 2.

Visualization of the trachea. During the procedure, transillumination of the light source helps visualize and puncture the trachea more accurately than tactile sense alone.
All procedures were performed by a senior surgery resident under the supervision of a surgical intensivist experienced in surgical tracheostomy. The tracheostomy nurse participated in all tracheostomy procedures, including control of the light wand and endotracheal tube during the procedure and preparation of a tracheostomy template that recorded the patient’s information, indications, procedural duration, and complications during and immediately after the procedure. All study results were based on this tracheostomy template.
The procedural duration was defined as the time from skin incision to cannula insertion. Minor bleeding was defined by the need for additional hemostatic procedures during the tracheostomy procedure and the need for a dressing because of continuous oozing after the procedure. Major bleeding was defined by the need for surgical conversion due to persistent bleeding despite conservative treatment.
The protocol of this study was reviewed and approved by the Institutional Review Board of Asan Medical Center (IRB No. 2016-1134).
Results
A total of 50 patients underwent PDT with a light source during the study period. More than half the patients who underwent PDT were admitted to the ICU with severe sepsis or septic shock (52%). Other reasons for ICU admission were severe multiple trauma (14%) and hypovolemic shock (12%) (Table 1). All patients required long-term mechanical ventilation or airway maintenance. There was no emergency case. The mean duration of mechanical ventilation before tracheostomy was 9.1 ± 3.8 days. The mean procedural duration was 14.0 ± 7.0 minutes, including the cases of surgical conversion.
Table 1.
Baseline characteristics of patients who underwent percutaneous dilatational tracheostomy with a light source in the surgical ICU
| Variable | Patient (n = 50) |
|---|---|
| Demographic profile | |
| Age (yr) | 66.34 ± 13.68 |
| Male sex | 42 (84) |
| Body mass index (kg/m2) | 22.72 ± 4.23 |
| Reason for ICU admission | |
| Severe sepsis or septic shock | 26 (52) |
| Multiple trauma | 7 (14) |
| Hypovolemic shock | 6 (12) |
| Postoperative closed monitoring | 4 (8) |
| Others | 7 (14) |
Values are presented as mean ± standard deviation or number (%).
ICU: intensive care unit.
There were no procedure-related deaths. Intraoperative complications included minor bleeding in three patients (6%) and paratracheal placement of the tracheostomy tube in one patient (2%) (Table 2). There was no case of major bleeding requiring surgical conversion, and the three patients with minor bleeding required additional hemostatic procedures. Paratracheal placement of the tracheostomy tube occurred in one patient. This was detected before removal of the endotracheal tube during the procedure, and the procedure was successfully performed again without other sequelae.
Table 2.
Complications during percutaneous dilatational tracheostomy with a light source
| Complication | Patient (n = 50) |
|---|---|
| Total | 4 (8) |
| Minor bleeding | 3 (6) |
| Paratracheal placement of the tracheostomy tube | 1 (2) |
Values are presented as number (%).
Two patients required conversion to surgical tracheostomy. In one patient, insertion of the light wand into the endotracheal tube was not smooth. It was later confirmed that the endotracheal tube lumen was covered with thick sputum and was narrowed, which complicated light wand insertion. The other patient had a very narrow trachea for cannula insertion and safely underwent surgical tracheostomy.
Discussion
The present study evaluated the safety and feasibility of a novel technique for performing PDT with a light source, without bronchoscopic guidance, in the surgical ICU by reviewing our experience with this technique over a period of 1 year. Since PDT was first described in 1985 [1], many ICU patients have undergone this procedure. PDT has several advantages. First, it can be performed at the bedside, thus avoiding the inconvenience and risk associated with the transportation of a critically ill patient to the operating suite as well as the additional expense of these resources [5]. Second, the technique is relatively easy compared with the surgical method; therefore, it can be performed by a medical doctor, not a surgeon, in the ICU. Third, there is no difference in complications and outcomes when compared with procedures performed with the surgical method. One study also reported a low infection rate, probably due to the minimally invasive nature of PDT [6,7].
The use of additional modalities such as bronchoscopy and ultrasonography has made PDT easier and safer since its introduction. Several studies have reported the benefits of using these modalities [8,9]. However, there is no specific PDT method that is recommended as a standard method [10]. In addition, these modalities require expensive equipment and a specialist, which adds to the overall cost.
In the present study, we confirmed the feasibility and safety of PDT with a light source performed for 50 patients in the surgical ICU. The light wand is used for intubation in patients with a difficult airway and is mainly used in the anaesthesiology department. Transillumination of the soft tissues at the anterior neck of the patient confirms that the light source at the tip of the light wand is in the tracheal lumen, thus facilitating precise intubation. Although PDT has been performed with this light wand, it is used only for a few patients and is not routinely used for all patients requiring tracheostomy [11].
A light wand is inexpensive and simple to use, thus precluding the requirement for additional professional personnel. While bronchoscopy requires preoperative equipment preparation, the light wand requires no such preparation. Also, use of the light wand does not require much additional time during the procedure; the process of inserting the light wand into the endotracheal tube can be completed within a few seconds. In the present study, the mean duration of the procedure was 14 ± 7 minutes, which was not significantly different from that for conventional PDT [12]. Tracheal visualization is clearer than that achieved with an ultrasound device, and the light wand can be fitted at the entrance of the swivel connector when it is inserted. Finally, the procedure can be performed more comfortably because events such as desaturation do not occur during the procedure.
As a basic principle, the trachea is punctured on the sole basis of tactile perception during PDT, without the aid of other instruments. The use of a light wand increases the ease and safety of the procedure because it enables visualization of the tip of the endotracheal tube, which lowers the risk of unexpected endotracheal tube depletion and balloon rupture. In the present study, complications such as cuff perforation and accidental decannulation of the endotracheal tube did not occur.
However, PDT with a light source has some limitations. Insertion of the light wand through the endotracheal tube may not be possible if the endotracheal tube lumen is too narrow. Although the light wand is a flexible device, its use will be limited if the endotracheal tube is deformed. In addition, perforation of the posterior wall of the trachea, although not observed in this study, cannot be confirmed during the procedure. Furthermore, because this method involves transillumination through the soft tissues in the neck, additional dissection of pretracheal soft tissues may be necessary for very obese patients with a very thick neck.
All PDT procedures in the present study were performed by a surgeon. Although PDT can be easily performed by individuals without surgical training, there should be provisions for the management of any complications that may occur during the procedure. The advantage of a PDT procedure performed by a surgeon is that intraoperative complications, including surgical conversion, can be quickly addressed. The procedurerelated complication rate in the present study was 8% (n = 4), which was similar to the rates reported for other PDT techniques [13]. Minor bleeding in three patients required additional hemostatic procedures and was easily controlled by the surgical intensivist who participated in the procedure, with no other sequelae. Other severe complications reported in other studies such as pneumothorax, subcutaneous emphysema, and wound infection did not occur.
In conclusion, PDT with a light source can be performed safely, precisely and comfortably without much cost and additional medical personnel. Thus, it is feasible to perform this procedure in the ICU. When PDT is performed by a surgeon, there is an advantage for additional management of any complications that may occur during the procedure.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Ciaglia P, Firsching R, Syniec C. Elective percutaneous dilatational tracheostomy. A new simple bedside procedure: preliminary report. Chest. 1985;87:715–9. doi: 10.1378/chest.87.6.715. [DOI] [PubMed] [Google Scholar]
- 2.Johnson-Obaseki S, Veljkovic A, Javidnia H. Complication rates of open surgical versus percutaneous tracheostomy in critically ill patients. Laryngoscope. 2016;126:2459–67. doi: 10.1002/lary.26019. [DOI] [PubMed] [Google Scholar]
- 3.Hinerman R, Alvarez F, Keller CA. Outcome of bedside percutaneous tracheostomy with bronchoscopic guidance. Intensive Care Med. 2000;26:1850–6. doi: 10.1007/s001340000718. [DOI] [PubMed] [Google Scholar]
- 4.Beiderlinden M, Karl Walz M, Sander A, Groeben H, Peters J. Complications of bronchoscopically guided percutaneous dilational tracheostomy: beyond the learning curve. Intensive Care Med. 2002;28:59–62. doi: 10.1007/s00134-001-1151-z. [DOI] [PubMed] [Google Scholar]
- 5.Freeman BD, Isabella K, Cobb JP, Boyle WA, 3rd, Schmieg RE, Jr, Kolleff MH, et al. A prospective, randomized study comparing percutaneous with surgical tracheostomy in critically ill patients. Crit Care Med. 2001;29:926–30. doi: 10.1097/00003246-200105000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Putensen C, Theuerkauf N, Guenther U, Vargas M, Pelosi P. Percutaneous and surgical tracheostomy in critically ill adult patients: a meta-analysis. Crit Care. 2014;18:544. doi: 10.1186/s13054-014-0544-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Delaney A, Bagshaw SM, Nalos M. Percutaneous dilatational tracheostomy versus surgical tracheostomy in critically ill patients: a systematic review and meta-analysis. Crit Care. 2006;10:R55. doi: 10.1186/cc4887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Guinot PG, Zogheib E, Petiot S, Marienne JP, Guerin AM, Monet P, et al. Ultrasound-guided percutaneous tracheostomy in critically ill obese patients. Crit Care. 2012;16:R40. doi: 10.1186/cc11233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rudas M, Seppelt I, Herkes R, Hislop R, Rajbhandari D, Weisbrodt L. Traditional landmark versus ultrasound guided tracheal puncture during percutaneous dilatational tracheostomy in adult intensive care patients: a randomised controlled trial. Crit Care. 2014;18:514. doi: 10.1186/s13054-014-0514-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Raimondi N, Vial MR, Calleja J, Quintero A, Cortés A, Celis E, et al. Evidence-based guidelines for the use of tracheostomy in critically ill patients. J Crit Care. 2017;38:304–18. doi: 10.1016/j.jcrc.2016.10.009. [DOI] [PubMed] [Google Scholar]
- 11.Addas BM, Howes WJ, Hung OR. Light-guided tracheal puncture for percutaneous tracheostomy. Can J Anaesth. 2000;47:919–22. doi: 10.1007/BF03019677. [DOI] [PubMed] [Google Scholar]
- 12.Gobatto AL, Besen BA, Tierno PF, Mendes PV, Cadamuro F, Joelsons D, et al. Comparison between ultrasound- and bronchoscopy-guided percutaneous dilational tracheostomy in critically ill patients: a retrospective cohort study. J Crit Care. 2015;30:220. doi: 10.1016/j.jcrc.2014.09.011. e13-7. [DOI] [PubMed] [Google Scholar]
- 13.Gobatto AL, Besen BA, Tierno PF, Mendes PV, Cadamuro F, Joelsons D, et al. Ultrasound-guided percutaneous dilational tracheostomy versus bronchoscopy-guided percutaneous dilational tracheostomy in critically ill patients (TRACHUS): a randomized noninferiority controlled trial. Intensive Care Med. 2016;42:342–51. doi: 10.1007/s00134-016-4218-6. [DOI] [PubMed] [Google Scholar]