Highlights
-
•
Electrical stimulation was tolerable in patients with chronic low back pain.
-
•
Stabilization exercises with NMES did not add clinical benefit for the CLBP.
-
•
Because of the small sample; clinicians should interpreting the results cautiously.
Keywords: Chronic low back pain, Stabilization exercises, Electrical stimulation, Muscle activation, Paraspinal muscles, Motor control exercises
Abstract
Background
One proposed mechanism of chronic low back pain might be paraspinal muscle impairment. Commonly, this impairment is treated with stabilization exercises. However, the effect size of stabilization exercises has been previously reported to be small.
Design
Randomized controlled trial.
Objective
To investigate the clinical benefit of using neuromuscular electrical stimulation as a supplement to stabilization exercises in patients with chronic low back pain.
Methods
Thirty participants with chronic low back pain were randomized into a stabilization exercise only group (n = 15) or a stabilization exercise plus neuromuscular electrical stimulation group (n = 15). The stabilization exercises included abdominal, side support, and quadruped exercises. The neuromuscular electrical stimulation was applied to the lumbar paraspinal muscles for 20 min each session. Both groups received their respective interventions twice a week for 6 weeks. Participant eligibility for inclusion was age between 18 and 60 years, body mass index ≤34, chronic low back pain ≥3 months, Numeric Pain Rating Scale ≥3, Modified Oswestry Disability Questionnaire score ≥20 and ability to understand English. Outcome measurements were self-reported neuromuscular electrical stimulation tolerability scale, Modified Oswestry Disability Questionnaire, Numeric Pain Rating Scale, Fear-Avoidance Beliefs Questionnaire and paraspinal muscle strength.
Results
The neuromuscular electrical stimulation was reported to be tolerable. There were no significant between-group differences on any of the outcome measures (p > 0.05).
Conclusions
The application of neuromuscular electrical stimulation on the paraspinal muscles was reported to be tolerable. Supplementing stabilization exercises with neuromuscular electrical stimulation did not offer any additional clinical benefit for the chronic low back pain patients.
Introduction
Chronic low back pain (CLBP) is a symptom with unknown etiology. Patients with CLBP are commonly prescribed stabilization exercises.1, 2 Prescribing stabilization exercises is based on the rationale that CLBP is associated with motor control impairments3, 4, 5, 6 and atrophy of the paraspinal muscles.7, 8, 9, 10, 11, 12, 13, 14, 15, 16 These impairments presumably render the spinal muscles unable to produce sufficient activation to maintain spinal stability.17, 18, 19 However, stabilization exercises have been reported to have only a small treatment effect in the short-term,20, 21 and their effectiveness has not been shown in the long-term.21
Due to this limited success with stabilization exercises, we postulate that stabilization exercises alone may not suffice to produce the appropriate levels of muscle activation needed to maintain spinal stability during the performance of routine activities of daily-living or more complex functional tasks. One hypothesis is that spinal muscle activation may be enhanced if stabilization exercises are supplemented with neuromuscular electrical stimulation (NMES). This hypothesis is supported by reports in the literature suggesting that NMES can activate the superficial and deep paraspinal muscles,22 and can potentially produce improvement in pain levels in patients with CLBP.23 One randomized controlled trial (RCT) showed that combining NMES with Transcutaneous Electrical Nerve Stimulation (TENS) resulted in significant reduction in pain than TENS or placebo alone.24 A recent RCT showed that combining NMES with volitional exercises for older adults with CLBP may improve their function and walking endurance.25
Therefore, the purpose of this pilot study was to: (1) explore whether patients with CLBP could tolerate the application of NMES on their paraspinal muscles; and (2) investigate whether supplementing a stabilization exercise program with NMES could influence clinical outcomes of function, pain, fear-avoidance behavior, and paraspinal muscle strength.
Methods
This was a randomized controlled trial. All study procedures were performed at the Human Movement Laboratory at University of Pittsburgh. Subjects were recruited from the general public in the Pittsburgh metro region using flyers, the University of Pittsburgh research registry and craigslist.com. The inclusion criteria specified age between 18 and 60 years, body mass index (BMI) less than 34, CLBP duration of 3 months or greater, Numeric Pain Rating Scale (NPRS) of 3 points or greater,26 Modified Oswestry Disability Questionnaire (MODQ) score of 20% or greater,27 and ability to read, write and understand English. The exclusion criteria were positive nerve root tension signs, signs of progressive or persistent neurological deficit, history of spinal surgery, inflammatory joint disease or cardiac disease, contraindications to NMES (e.g. skin allergy to adhesives), history of metastatic cancer in the previous 5 years or present treatment for cancer, pregnancy or plans to become pregnant.
The Institutional Review Board at University of Pittsburgh, Pittsburgh, PA, approved the study (IRB approval # PRO12100651). All participants signed a consent form prior to participation, and the rights of the participants were protected. The trial was registered on clinicaltrials.gov (ID: NCT02864732).
Intervention
Research participants were randomized into one of 2 treatment groups:
-
•
Stabilization exercises program only (stab-only)
-
•
Stabilization exercises program supplemented with NMES (stab + NMES).
Each subject was scheduled for 2 treatment sessions per week over a 6-week period. The sessions lasted 20 min for the stab-only group, and 40 min for the stab + NMES group. The stabilization exercise program that we used has been previously described in the literature.1, 28 The program included abdominal bracing exercises, side support exercises, and quadruped exercises (Appendix 1). The exercises were conducted under the supervision of a licensed physical therapist.
For subjects assigned to the stab + NMES group, the NMES was applied at the start of the session for 20 min, followed by the stabilization exercise program. The NMES was applied to the lumbar paraspinal muscles bilaterally using an Empi 300 portable unit (Empi, 599 Cardigan Rd, St. Paul, MN 55126). A pillow was placed under the abdomen of the prone-lying subject. Two large (12 cm × 6 cm) self-adhesive electrodes were applied to the paraspinal muscles, one electrode on each side. The NMES parameters were set to produce a pulse frequency of 75 pulses per second, a pulse duration of 250 μs, with a 4-s ramp up and ramp down time, and a 6-s stimulation period at the maximum amplitude, followed by a 50 s rest period to minimize fatigue. These parameters were extrapolated from NMES studies applied to the quadriceps femoris muscles.29, 30, 31
All subjects were instructed that the higher the current intensity, the stronger and better the muscle activation. Also, they were instructed to perform active trunk extension as soon as they felt the electrical current ramp up, and to return to the resting prone position when the current ramped down.
Outcome measures
Baseline evaluation included obtaining demographic data and outcome measures (Table 1).
Table 1.
Baseline characteristics and demographics.
| Stab-only (Mean ± SD) |
Stab + NMES (Mean ± SD) |
|
|---|---|---|
| Age | 38.33 ± 11.3 | 33.40 ± 9.0 |
| Height (cm) | 164.98 ± 7.6 | 171.3 ± 10.0 |
| Weight (kg) | 71.11 ± 14.2 | 77.71 ± 13.2 |
| Body mass index (kg/m2) | 25.89 ± 3.8 | 26.47 ± 2.9 |
| MODQ | 30.80 ± 10.2 | 30.52 ± 7.8 |
| NPRS | 4.44 ± 1.8 | 4.20 ± 1.9 |
| FABQ-PA | 12.33 ± 5.5 | 14.27 ± 6.5 |
| FABQ-W | 12.20 ± 10.9 | 11.67 ± 10.5 |
| Paraspinal muscles strength (Nm) | 117.29 ± 57.7 | 154.49 ± 59.1 |
| Gender | n | n |
| Male | 4 | 7 |
| Female | 11 | 8 |
| Ethnicity | ||
| White Caucasian | 9 | 13 |
| African-Americans | 4 | 1 |
| Asians | 1 | 1 |
| Others | 1 | 0 |
NMES, neuromuscular electrical stimulation; SD, standard deviation; MODQ, Modified Oswestry Disability Questionnaire; NPRS, Numeric Pain Rating Scale; FABQ-PA, fear-avoidance behavior questionnaire – physical activity; FABQ-W, fear-avoidance behavior questionnaire – work.
Self-report of NMES tolerability
The assessment of NMES tolerability was performed by asking each subject in the stab + NMES group to describe their subjective perception of both the intensity and discomfort of the NMES current using the verbal descriptors listed in Table 2.
Table 2.
Descriptors of intensity (sensory) and discomfort (affective) aspects of electrical stimulation.
| Descriptors of sensory aspect of the NMES current | Sensory descriptors categories | Descriptors of affective aspect of the NMES current | Affective descriptors categories | ||
|---|---|---|---|---|---|
| Extremely intense | 15 | High intensity descriptors | Excruciating | 15 | High discomfort descriptors |
| Very intense | 14 | Intolerable | 14 | ||
| Very strong | 13 | Unbearable | 13 | ||
| Intense | 12 | Agonizing | 12 | ||
| Strong | 11 | Horrible | 11 | ||
| Slightly intense | 10 | Moderate intensity descriptors | Dreadful | 10 | Moderate discomfort descriptors |
| Barely strong | 9 | Frightful | 9 | ||
| Moderate | 8 | Awful | 8 | ||
| Slightly moderate | 7 | Miserable | 7 | ||
| Very moderate | 6 | Oppressive | 6 | ||
| Mild | 5 | Low intensity descriptors | Distressing | 5 | Low discomfort descriptors |
| Very mild | 4 | Uncomfortable | 4 | ||
| Weak | 3 | Unpleasant | 3 | ||
| Very weak | 2 | Distracting | 2 | ||
| Extremely weak | 1 | Bearable | 1 | ||
The sensory and affective adjectives are numbered from 1 to 15. They are divided into high (11–15), moderate (6–10) and low (1–5). These divisions were not shown to the subjects; the subjects were only shown the two columns of the sensory and affective descriptors. NMES, neuromuscular electrical stimulation.
The subjects were asked to increase the NMES current to 20 mA. Each subject was informed that 20 mA corresponded to the “extremely weak” descriptor in terms of the sensory aspect of the current, and the “bearable” descriptor in terms of the affective aspect of the NMES current. Each subject was then asked to increase the intensity to their highest level of tolerance. Once the highest tolerance was reached, the subject was asked to provide new descriptions of their perception of the current tolerability in relation to the 20 mA reference current. This approach to measuring NMES current tolerability has been described in the literature.32
Functional outcome measure
The MODQ is a self-reported measure of functional disability consisting of 10 questions about various activities related to back pain. Each question has 6 possible responses ranging from 0 to 5, with a total possible maximum score of 50. The total MODQ score is multiplied by 2 to get a percentage score, with higher percentages indicating greater levels of self-reported disability. The MODQ has excellent reliability and good construct validity.27
Pain outcome measure
The NPRS measures pain intensity on an 11-point scale from 0 (no pain) to 10 (maximum pain). We used the “triple NPRS” in which the subject is asked to respond to three questions: (1) the intensity of current pain; (2) the best pain intensity in the past 24 h; and (3) the worst pain intensity in the past 24 h. The mean of these sub-scores was reported as the subject's NPRS score. The triple NPRS has excellent reliability and good validity.26
Fear-avoidance outcome measure
The Fear Avoidance-Behavior Questionnaire (FABQ) is a self-reported questionnaire consisting of a total of 16 items, divided into two subscales: physical activity (5 items) and work (11 items). Not all items are calculated toward the final score (i.e. item 1 in the physical activity scale, and items 8, 12, 14 and 16 in the work scale do not count). The total possible maximum FABQ score is 66, with higher scores indicating greater levels of fear avoidance. The FABQ has acceptable levels of reliability and validity.33
Muscle strength outcome measure
Paraspinal muscle strength was assessed using the Biodex 3 Pro dynamometer (20 Ramsey Rd, Shirley, NY 11967). Active extension of the trunk was performed with the subject in a semi-standing position; the subject's hips were flexed at 60 degrees with the feet resting on an adjustable footrest. The thighs were secured to the seat with two Velcro straps. The scapulae rested against a bar. The trunk was secured with two Velcro straps that crossed the front trunk forming the shape of an “X”. Using the same verbal instructions, each subject was asked to extend the trunk by exerting maximal isometric contraction for 5 s against the scapular bar. The average of three 5-s trials was recorded in Nm.
All of the outcome measures were collected at baseline and post-treatment at week 6 during the final session. The MODQ and NPRS were also collected at week 10; 4 weeks after the final treatment session.
Sample size
The total sample size (n = 30) was based upon the resources available to conduct this study. As such, we did not conduct a formal power analysis.
Randomization and blinding
We used a randomization website (www.graphpad.com) to randomize subjects into the 2 treatment arms (1:1 ratio). The website generated a list of group allocation at random. The list was kept in a locked cabinet, and each consecutive patient was assigned a group based on that list. Due to the nature of the intervention, there was no blinding in this study.
Statistical analysis
Descriptive statistics were used to report the baseline demographics and characteristics of each treatment group (Table 1). Independent-sample t tests or Mann–Whitney U tests were used to assess if there were any significant differences between the groups at baseline (Table 1). Descriptive statistics were also used to summarize tolerability data by reporting the percentages of subjects who rated the sensory and affective aspects of NMES intensity.
For the clinical outcomes of MODQ, NPRS, FABQ and paraspinal muscle strength, we used a separate 2 × 2 (group × time) mixed analysis of variance (ANOVA) to test for between-group significance from baseline to the 6-week assessment point for each outcome measure. Assumptions of normality and homoscedasticity were checked. The level of significance was set at p < 0.05 for all comparisons.
Missing data were managed by multiple imputation technique, which creates 5 sets of imputed data beside the original data set. We replaced each missing value by a value that was pooled from the 5 sets.
Results
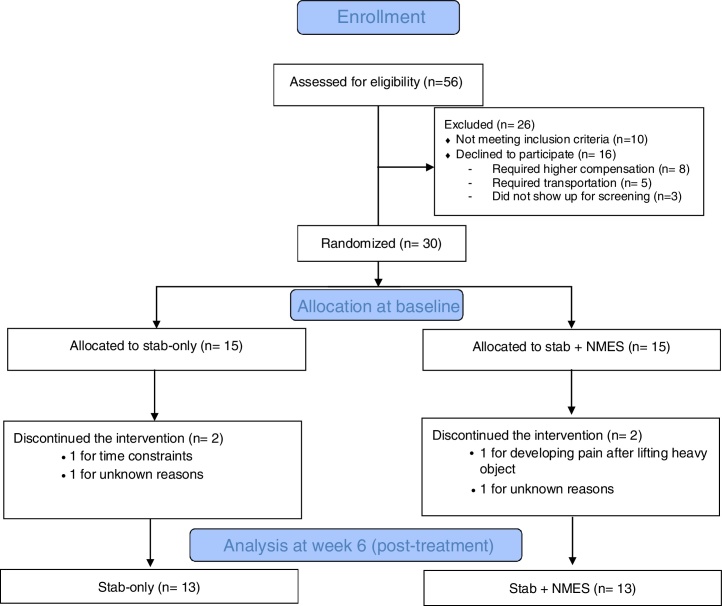
The study was conducted from January 2014 to January 2015. We performed baseline screening examinations on 56 subjects with CLBP; 16 declined to participate, and 10 were ineligible. The remaining 30 participants were randomized to one of the two treatment groups (Fig. 1). The dropout rate was 13%.
Figure 1.
Flowchart outlining subjects flow throughout the trial.
Table 1 presents the baseline characteristics and demographics of the two treatment groups. The stab + NMES group had younger participants, more males, and higher baseline scores of paraspinal muscle strength compared to the stab only group.
Subjects in the stab + NMES group were able to increase the current intensity from baseline to post-intervention at week 6 (Table 3). Despite this increase in current intensity, 100% of the subjects reported low discomfort with the current.
Table 3.
Electrical stimulation ratings of sensory (intensity) and affective (discomfort) aspects at baseline and final session.
| Sensory descriptors categories | Baseline | Final session (6 weeks) | Affective descriptors categories | Baseline | Final session (6 weeks) |
|---|---|---|---|---|---|
| High | 60% | 76% | High | 0% | 0% |
| Medium | 40% | 24% | Medium | 0% | 0% |
| Low | 0% | 0 | Low | 100% | 100% |
See Table 1 for a list of descriptors.
All self-reported clinical outcome measures (i.e. MODQ, NPRS, FABQ-PA and FABQ-W) showed no interaction of group with time (p > 0.05). Also, there were no significant differences between the groups on any of these outcome measures (p > 0.05) (Table 4).
Table 4.
Outcome measures scores for each group over time.
| Baseline | 6 weeks | Δ within group | Δ between group (95% CI) |
|
|---|---|---|---|---|
| Outcome, mean ± SD | ||||
| MODQ (0–100 scale) | ||||
| Stab-only | 30.80 ± 10.2 | 12.81 ± 5.2 | 17.99* | −1.68 (−7.88–4.19) |
| Stab + NMES | 30.52 ± 7.8 | 14.49 ± 10.2 | 16.03* | |
| NPRS (0–10 scale) | ||||
| Stab-only | 4.44 ± 1.8 | 2.07 ± 1.1 | 2.37* | −0.27 (−1.24–.70) |
| Stab + NMES | 4.20 ± 1.9 | 2.34 ± 1.5 | 1.86* | |
| FABQ-PA (0–24 scale) | ||||
| Stab-only | 12.33 ± 5.5 | 8.41 ± 6.0 | 3.92* | −2.33 (−6.38–1.71) |
| Stab + NMES | 14.27 ± 6.5 | 10.75 ± 4.7 | 3.52* | |
| FABQ-W (0–42 scale) | ||||
| Stab-only | 12.20 ± 10.9 | 8.87 ± 9.6 | 3.33 | 1.12 (−5.37–7.61) |
| Stab + NMES | 11.67 ± 10.5 | 7.75 ± 7.6 | 3.92 | |
| Paraspinal muscle strength (Biodex 3 Pro dynamometer)*,‡ | ||||
| Stab-only | 117.29 ± 57.7 Nm | 162.30 ± 55.2 Nm | 45.01* | −13.51 (−56.00–28.98) |
| Stab + NMES | 154.49 ± 59.1 Nm | 175.80 ± 58.4 Nm | 21.31* | |
SD, standard deviation; MODQ, Modified Oswestry Disability Questionnaire; NMES, neuromuscular electrical stimulation; NPRS, Numeric Pain Rating Scale; FABQ-PA, fear-avoidance behavior questionnaire – physical activity; FABQ-W, fear-avoidance behavior questionnaire – work; 95% CI, 95% confidence interval.
Indicates significant within group difference (p < 0.05).
Controlling for age, gender, ethnicity, and baseline paraspinal muscle strength difference.
For paraspinal muscle strength testing, we ran a mixed ANOVA controlling for age, gender, ethnicity and baseline paraspinal muscle strength. There was no interaction of group with time (p = 0.12), and no significant difference between the groups (p = 0.12).
Discussion
Tolerability of NMES
Supplementing a stabilization exercise program with NMES had no negative effect on retention or rate of adherence to treatment. The NMES was tolerable on the lumbar paraspinal muscles without any adverse events reported. All of the subjects were able to increase the current intensity from baseline to 6 weeks, suggesting that subjects were able to adapt to the intensity of NMES current over time. The NMES intensities that can be applied to the lumbar paraspinal muscles are similar to the intensities that have been applied to the quadriceps femoris muscle.30, 31, 34, 35 For example, in a study by Snyder-Mackler et al.,31, 34 a number of subjects were able to use the full available amperage of the NMES devices, which was 100 mA. In our study, we had similar findings.
Subjects were able to successfully distinguish between the sensory and affective aspects of the NMES current, which is relevant to day-to-day physical therapy practice. Physical therapists can continuously encourage patients to increase the NMES intensity to achieve high levels of contraction; and at the same time assure the patients that higher intensity is safe and will become more comfortable from one session to the next.
Since there were no universally accepted NMES parameters, we chose the parameters suggested by clinical practice guidelines.29 These parameters consist of high frequency (>50 Hz) and long pulse duration (150–300 ms), the combination of which can create a strong quadriceps femoris muscle contraction.29, 36 We recognize the quadriceps muscle is different from the paraspinal muscles. However, since the quadriceps femoris is such a large muscle that can achieve faster recovery with electrical stimulation of 10% of maximum voluntary contraction,31 we expect that a smaller muscle like the paraspinals would achieve appropriate muscle activation using the same parameters.
Clinical effectiveness of NMES
There was no significant difference between the groups on any of the outcome measures; however, both groups improved from baseline to 6 weeks post treatment. This lack of significant difference has 2 possible explanations. One possibility is that NMES truly does not add any clinical benefit when combined with stabilization exercises. However, this study was not adequately powered and therefore should not be used to draw any definitive conclusions about the effectiveness of NMES as a supplement to stabilization exercises. Type II error is quite possible.
The second possible explanation is that the NMES dosage was not optimal for creating an effective treatment response. The number of NMES sessions used in our study may not have been sufficient to make significant changes between the groups. The number of sessions per subject was only 12, without home sessions. In other studies, however, the number of NMES sessions was much higher. For example, in a study by Snyder-Mackler et al.,31 NMES was delivered to the quadriceps muscle for 15 min, four times per day, for 5 days a week for 4 weeks. Also, in a study by Piva et al.,30 NMES was delivered for 60 sessions divided into 12 supervised sessions and 48 at-home sessions. With such higher dosages the NMES was shown to improve the clinical outcome of pain, function and quadriceps femoris strength for patients post knee surgery. However, it should be noted that increasing the number of sessions is associated with additional cost that could be incurred by patients for additional units of treatment.
Limitations
A major limitation of this study was the small sample size (n = 30). Also, our study did not include a control group that received no treatment, which limited our ability to refute the argument that the observed improvement from pre to post intervention occurred naturally. Additionally, there was no blinding in this study.
This study suggests that using NMES in combination with stabilization exercises is tolerable on patients with CLBP. However, this study also suggests that combining NMES with stabilization exercises adds no additional effect to the clinical outcome. Larger trials are strongly needed.
Funding
This work was supported by a grant from King Fahad Specialist Hospital, Dammam, Saudi Arabia.
Conflicts of interest
The authors declare no conflicts of interest.
Acknowledgement
King Fahad Specialist Hospital – Dammam for funding the study.
Footnotes
Trial registered: NCT02864732 (https://clinicaltrials.gov/ct2/show/NCT02864732).
Appendix 1.
Stabilization program
This packet contains descriptions of all exercises included in the stabilization exercise program. These exercises are performed as the therapist has indicated. The exercises are performed at least once a day. Before beginning any of the stabilization exercises, 5–6 cycles of the cat/camel exercise should be performed. This exercise is performed by arching the back upwards (camel), then slowly lowering the back toward the floor (cat).
Abdominal bracing exercises (non-weight bearing)
| Exercise |
|---|
| 1. Abdominal bracing (supine) |
| Lie on your back with your knees bent. Tighten your stomach muscles without pressing your back flat to the floor. Hold for 8 s, counting aloud to avoid holding your breath. Relax and repeat. |
| 2. Abdominal bracing (supine) with heel slide |
| Lie on your back with knees bent. While tightening your stomach muscles (abdominal brace), slide the heel of one foot away from you until your knee is straight (3 s count). |
| Then, slide your heel back toward you until your knee is in its original bent position (3 s count). Relax and repeat on opposite leg. |
| 3. Abdominal bracing (supine) with leg lifts |
| Lie on your back with knees bent. While tightening your stomach muscles (abdominal brace), lift one foot about 6 inches off the floor for a 3 s count. Then, return it to the floor at a 3 s count. Relax and repeat with opposite leg. |
| 4. Abdominal bracing (supine) with bridging |
| Lie on your back with knees bent. While tightening your stomach muscles (abdominal brace), tighten your buttocks and slowly lift them off the floor. Do not allow your back to arch. Hold for 8 seconds. Relax and repeat. |
| 5. Bracing with single leg bridging |
| Lie on your back with knees bent. While tightening your stomach muscles (abdominal brace), tighten your buttocks and slowly straighten one knee so that only one foot is on the floor. Then, slowly lift your buttocks off the floor. Hold for 8 seconds. Relax and repeat. |
Abdominal bracing exercises (weight bearing)
| Exercise |
|---|
| 1. Abdominal bracing in standing |
| While standing, tighten your stomach muscles without changing the curve of your back. Hold for 8 s. Relax and repeat. |
| 2. Isometric Torsion |
| Stand in a slightly forward-bent position with one hand used as support on a table. Perform the abdominal brace and lift a light weight (2–3# dumbbell, can of soup, etc.) |
| 3. Abdominal Bracing with walking |
| While walking, perform the abdominal brace. Hold 8 s. Relax for 10 s and repeat. Continue this cycle as you walk. Progress up to 10 min of walking. |
Side support exercises
| Exercise |
|---|
| 1. Side support with knees flexed |
| Lie on your side with knees bent and upper body supported on the lower elbow. Then, lift your body from the table with all weight borne on the lower knee and elbow. Hold for 8 s. Relax and repeat. |
| 2. Side support with knees flexed and bracing |
| Perform the abdominal brace (tighten your stomach muscles) then do the side support as above. Hold for 8 s. Relax and repeat. |
| 3. Side support with knees extended |
| Lie on your side with knees straight and upper body supported on the lower elbow. Then, lift your body from the table with all weight borne on the lower foot and elbow. Hold for 8 s. Relax and repeat. |
| 4. Side support with knees extended and bracing |
| Perform the abdominal brace (tighten your stomach muscles) then do the side support as above with knees straight. Hold for 8 s. Relax and repeat. |
| 5. Advanced Side Bridge |
| Perform the side support as described above. Roll from one elbow to the other while abdominally bracing to attain a side support position on the opposite elbow. Then, lower yourself from side support position on the opposite elbow down to the floor. |
Quadruped exercises
| Exercise |
|---|
| No exercise begun in this group until able to complete Abdominal Bracing in supine (10 reps × 8 s hold) |
| 1. Quadruped Arm Lifts with bracing |
| Start on your hands and knees. Tighten your stomach muscles. Then lift your right arm from the table. Hold for 8 s. Return to start position and repeat with left arm. |
| 2. Quadruped Leg Lifts with bracing |
| Start on your hands and knees. Tighten your stomach muscles. Then extend your right leg so that your knee is lifted from the table. Keep your hips level with the table as you do this. Hold for 8 s. Return to start position and repeat with left leg. |
| 3. Quadruped Opposite Arm and Leg Lift with bracing |
| Start on your hands and knees. Tighten your stomach muscles. Then extend your right leg so that your knee is lifted from the table and lift your left arm from the table at the same time. Keep your hips level with the table as you do this. Hold for 8 s. Return to start position and repeat with left leg. |
Criterion-based stabilization program
For each group of exercises listed below, the patient must be able to achieve specific exercise goals before he or she can move on to the next exercise within that group. For example, the patient must complete 30 repetitions (8 s hold time) of the abdominal brace in supine before progressing to abdominal brace with heel slide. Once the patient reaches the final exercise in a progression group, he or she should continue to perform the final exercise and even progress repetitions if possible.
Abdominal bracing exercises (non-weight bearing)
| Exercise | Criterion for progression |
|---|---|
| Abdominal bracing (supine) | Able to complete 30 reps × 8 s hold |
| Abdominal bracing (supine) with heel slides | Able to complete 20 reps per leg (4 s count) |
| Abdominal bracing (supine) with leg lifts | Able to complete 20 reps per leg (4 s count) |
| Abdominal bracing (supine) with bridging | For progression to single leg bridging, able to complete 30 reps × 8 s hold. Continue with increased repetitions of bridging until able to perform single leg bridging |
| Bracing with single leg bridging | Goal is 30 reps × 8 s hold |
Abdominal bracing exercises (weight bearing)
| Exercise | Criterion for progression |
|---|---|
| For progression to abdominal bracing in weight-bearing positions, the individual should be able to complete 20 reps × 8 s hold of abdominal bracing with bridging | |
| Abdominal bracing in standing | Able to complete 30 reps × 8 s hold |
| Isometric Torsion (standing row in slight trunk flexion with one hand used as support on a table) |
Able to complete 20 reps on each side (6 s count) |
| Abdominal Bracing with walking | Goal is to walk for 10 min with abdominal bracing (8 s hold and 10 s rest) |
Side support exercises
| Exercise | Criterion for progression |
|---|---|
| Side support with knees flexed | Able to complete 30 reps × 8 s hold on each side. Able to complete Abdominal Bracing in supine (10 reps × 8 s hold) |
| Side support with knees flexed and bracing | Able to complete 30 reps × 8 s hold on each side |
| Side support with knees extended | Able to complete 30 reps × 8 s hold on each side |
| Side support with knees extended and bracing | Able to complete 30 reps × 8 s hold on each side |
| Advanced Side Bridge (roll from one elbow to the other while abdominally bracing) | Continue to add reps until able to complete 30 reps × 8 s |
Quadruped exercises
| Exercise | Criterion for progression |
|---|---|
| No exercise begun in this group until the following criterion is met | Able to complete Abdominal Bracing in supine (10 reps × 8 s hold) |
| Quadruped Arm Lifts with bracing | Able to complete 30 reps × 8 s hold on each side |
| Quadruped Leg Lifts with bracing | Able to complete 30 reps × 8 s hold on each side |
| Quadruped Opposite Arm and Leg Lift with bracing | Continue to add reps until able to complete 40 reps × 8 s |
References
- 1.McGill S. 2nd ed. Human Kinetics; Champaign, IL: 2007. Low Back Disorders: Evidence-Based Prevention and Rehabilitation. [Google Scholar]
- 2.Richaedson C., Hodges P., Hides J. Churchill Livingstone; Edinburgh: 2004. Therapeutic Exercise for Lumbopelvic Stabilization. [Google Scholar]
- 3.Cholewicki J., Greene H.S., Polzhofer G.K., Galloway M.T., Shah R.A., Radebold A. Neuromuscular function in athletes following recovery from a recent acute low back injury. J Orthop Sports Phys Ther. 2002;32(11):568–575. doi: 10.2519/jospt.2002.32.11.568. [DOI] [PubMed] [Google Scholar]
- 4.Cholewicki J., Silfies S.P., Shah R.A. Delayed trunk muscle reflex responses increase the risk of low back injuries. Spine (Phila Pa 1976) 2005;30(23):2614–2620. doi: 10.1097/01.brs.0000188273.27463.bc. [DOI] [PubMed] [Google Scholar]
- 5.Radebold A., Cholewicki J., Panjabi M.M., Patel T.C. Muscle response pattern to sudden trunk loading in healthy individuals and in patients with chronic low back pain. Spine (Phila Pa 1976) 2000;25(8):947–954. doi: 10.1097/00007632-200004150-00009. [DOI] [PubMed] [Google Scholar]
- 6.Radebold A., Cholewicki J., Polzhofer G.K., Greene H.S. Impaired postural control of the lumbar spine is associated with delayed muscle response times in patients with chronic idiopathic low back pain. Spine (Phila Pa 1976) 2001;26(7):724–730. doi: 10.1097/00007632-200104010-00004. [DOI] [PubMed] [Google Scholar]
- 7.Hides J.A., Richardson C.A., Jull G.A. Multifidus muscle recovery is not automatic after resolution of acute, first-episode low back pain. Spine (Phila Pa 1976) 1996;21(23):2763–2769. doi: 10.1097/00007632-199612010-00011. [DOI] [PubMed] [Google Scholar]
- 8.Hides J.A., Stokes M.J., Saide M., Jull G.A., Cooper D.H. Evidence of lumbar multifidus muscle wasting ipsilateral to symptoms in patients with acute/subacute low back pain. Spine (Phila Pa 1976) 1994;19(2):165–172. doi: 10.1097/00007632-199401001-00009. [DOI] [PubMed] [Google Scholar]
- 9.Kjaer P., Bendix T., Sorensen J.S., Korsholm L., Leboeuf-Yde C. Are MRI-defined fat infiltrations in the multifidus muscles associated with low back pain? BMC Med. 2007;5:2. doi: 10.1186/1741-7015-5-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Danneels L.A., Vanderstraeten G.G., Cambier D.C., Witvrouw E.E., De Cuyper H.J. CT imaging of trunk muscles in chronic low back pain patients and healthy control subjects. Eur Spine J. 2000;9(4):266–272. doi: 10.1007/s005860000190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kent-Braun J.A., Le Blanc R. Quantitation of central activation failure during maximal voluntary contractions in humans. Muscle Nerve. 1996;19(7):861–869. doi: 10.1002/(SICI)1097-4598(199607)19:7<861::AID-MUS8>3.0.CO;2-7. [DOI] [PubMed] [Google Scholar]
- 12.De Serres S.J., Enoka R.M. Older adults can maximally activate the biceps brachii muscle by voluntary command. J Appl Physiol. 1998;84(1):284–291. doi: 10.1152/jappl.1998.84.1.284. [DOI] [PubMed] [Google Scholar]
- 13.Stackhouse S.K., Dean J.C., Lee S.C., Binder-MacLeod S.A. Measurement of central activation failure of the quadriceps femoris in healthy adults. Muscle Nerve. 2000;23(11):1706–1712. doi: 10.1002/1097-4598(200011)23:11<1706::aid-mus6>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 14.Yue G.H., Ranganathan V.K., Siemionow V., Liu J.Z., Sahgal V. Older adults exhibit a reduced ability to fully activate their biceps brachii muscle. J Gerontol A: Biol Sci Med Sci. 1999;54(5):M249–M253. doi: 10.1093/gerona/54.5.m249. [DOI] [PubMed] [Google Scholar]
- 15.Mizner R.L., Stevens J.E., Snyder-Mackler L. Voluntary activation and decreased force production of the quadriceps femoris muscle after total knee arthroplasty. Phys Ther. 2003;83(4):359–365. [PubMed] [Google Scholar]
- 16.O’Reilly S.C., Jones A., Muir K.R., Doherty M. Quadriceps weakness in knee osteoarthritis: the effect on pain and disability. Ann Rheum Dis. 1998;57(10):588–594. doi: 10.1136/ard.57.10.588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McGill S.M., Cholewicki J. Biomechanical basis for stability: an explanation to enhance clinical utility. J Orthop Sports Phys Ther. 2001;31(2):96–100. doi: 10.2519/jospt.2001.31.2.96. [DOI] [PubMed] [Google Scholar]
- 18.McGill S.M., Grenier S., Kavcic N., Cholewicki J. Coordination of muscle activity to assure stability of the lumbar spine. J Electromyogr Kinesiol. 2003;13(4):353–359. doi: 10.1016/s1050-6411(03)00043-9. [DOI] [PubMed] [Google Scholar]
- 19.McGill S.M. Low back stability: from formal description to issues for performance and rehabilitation. Exerc Sport Sci Rev. 2001;29(1):26–31. doi: 10.1097/00003677-200101000-00006. [DOI] [PubMed] [Google Scholar]
- 20.van Tulder M., Malmivaara A., Hayden J., Koes B. Statistical significance versus clinical importance: trials on exercise therapy for chronic low back pain as example. Spine (Phila Pa 1976) 2007;32(16):1785–1790. doi: 10.1097/BRS.0b013e3180b9ef49. [DOI] [PubMed] [Google Scholar]
- 21.Hayden J.A., van Tulder M.W., Malmivaara A.V., Koes B.W. Meta-analysis: exercise therapy for nonspecific low back pain. Ann Intern Med. 2005;142(9):765–775. doi: 10.7326/0003-4819-142-9-200505030-00013. [DOI] [PubMed] [Google Scholar]
- 22.Baek S.O., Ahn S.H., Jones R. Activations of deep lumbar stabilizing muscles by transcutaneous neuromuscular electrical stimulation of lumbar paraspinal regions. Ann Rehabil Med. 2014;38(4):506–513. doi: 10.5535/arm.2014.38.4.506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Coghlan S., Crowe L., McCarthypersson U., Minogue C., Caulfield B. Neuromuscular electrical stimulation training results in enhanced activation of spinal stabilizing muscles during spinal loading and improvements in pain ratings. Conf Proc IEEE Eng Med Biol Soc. 2011;2011:7622–7625. doi: 10.1109/IEMBS.2011.6091878. [DOI] [PubMed] [Google Scholar]
- 24.Moore S.R., Shurman J. Combined neuromuscular electrical stimulation and transcutaneous electrical nerve stimulation for treatment of chronic back pain: a double-blind, repeated measures comparison. Arch Phys Med Rehabil. 1997;78(1):55–60. doi: 10.1016/s0003-9993(97)90010-1. [DOI] [PubMed] [Google Scholar]
- 25.Hicks G.E., Sions J.M., Velasco T.O., Manal T.J. Trunk muscle training augmented with neuromuscular electrical stimulation appears to improve function in older adults with chronic low back pain: a randomized preliminary trial. Clin J Pain. 2016;32(10):898–906. doi: 10.1097/AJP.0000000000000348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Childs J.D., Piva S.R., Fritz J.M. Responsiveness of the numeric pain rating scale in patients with low back pain. Spine (Phila Pa 1976) 2005;30(11):1331–1334. doi: 10.1097/01.brs.0000164099.92112.29. [DOI] [PubMed] [Google Scholar]
- 27.Fritz J.M., Irrgang J.J. A comparison of a modified Oswestry Low Back Pain Disability Questionnaire and the Quebec Back Pain Disability Scale. Phys Ther. 2001;81(2):776–788. doi: 10.1093/ptj/81.2.776. [DOI] [PubMed] [Google Scholar]
- 28.Hicks G.E., Fritz J.M., Delitto A., McGill S.M. Preliminary development of a clinical prediction rule for determining which patients with low back pain will respond to a stabilization exercise program. Arch Phys Med Rehabil. 2005;86(9):1753–1762. doi: 10.1016/j.apmr.2005.03.033. [DOI] [PubMed] [Google Scholar]
- 29.Logerstedt D.S., Snyder-Mackler L., Ritter R.C., Axe M.J., Godges J.J. Knee stability and movement coordination impairments: knee ligament sprain. J Orthop Sports Phys Ther. 2010;40(4):A1–A37. doi: 10.2519/jospt.2010.0303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Piva S.R., Goodnite E.A., Azuma K. Neuromuscular electrical stimulation and volitional exercise for individuals with rheumatoid arthritis: a multiple-patient case report. Phys Ther. 2007;87(8):1064–1077. doi: 10.2522/ptj.20060123. [DOI] [PubMed] [Google Scholar]
- 31.Snyder-Mackler L., Delitto A., Stralka S.W., Bailey S.L. Use of electrical stimulation to enhance recovery of quadriceps femoris muscle force production in patients following anterior cruciate ligament reconstruction. Phys Ther. 1994;74(10):901–907. doi: 10.1093/ptj/74.10.901. [DOI] [PubMed] [Google Scholar]
- 32.Delitto A., Strube M.J., Shulman A.D., Minor S.D. A study of discomfort with electrical stimulation. Phys Ther. 1992;72(6):410–421. doi: 10.1093/ptj/72.6.410. discussion on 421–414. [DOI] [PubMed] [Google Scholar]
- 33.Waddell G., Newton M., Henderson I., Somerville D., Main C.J. A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain. 1993;52(2):157–168. doi: 10.1016/0304-3959(93)90127-B. [DOI] [PubMed] [Google Scholar]
- 34.Snyder-Mackler L., Delitto A., Bailey S.L., Stralka S.W. Strength of the quadriceps femoris muscle and functional recovery after reconstruction of the anterior cruciate ligament. A prospective, randomized clinical trial of electrical stimulation. J Bone Jt Surg Am. 1995;77(8):1166–1173. doi: 10.2106/00004623-199508000-00004. [DOI] [PubMed] [Google Scholar]
- 35.Laufer Y., Ries J.D., Leininger P.M., Alon G. Quadriceps femoris muscle torques and fatigue generated by neuromuscular electrical stimulation with three different waveforms. Phys Ther. 2001;81(7):1307–1316. [PubMed] [Google Scholar]
- 36.Cameron M.H. Elsevier Health Sciences; 2012. Physical Agents in Rehabilitation: From Research to Practice. [Google Scholar]