Highlights
-
•
Improper activation of the trapezius is associated with abnormal scapular motions.
-
•
This paper reviews the anatomy, kinesiology, and pathokinesiology of the trapezius.
-
•
This paper describes and illustrates exercises that target the trapezius.
Keywords: Physical therapy, Scapular dyskinesis, Scapulothoracic joint, Shoulder rehabilitation, Trapezius exercises
Abstract
Background
The trapezius is an extensive muscle subdivided into upper, middle, and lower parts. This muscle is a dominant stabilizer of the scapula, normally operating synergistically with other scapular muscles, most notably the serratus anterior. Altered activation, poor control, or reduced strength of the different parts of the trapezius have been linked with abnormal scapular movements, often associated with pain. Several exercises have been designed and studied that specifically target the different parts of the trapezius, with the goal of developing exercises that optimize scapular position and scapulohumeral rhythm that reduce pain and increase function.
Methods
This paper describes the anatomy, kinesiology, and pathokinesiology of the trapezius as well as exercises that selectively target the activation of the different parts of this complex muscle.
Conclusions
This review provides the anatomy and kinesiology of the trapezius muscle with the underlying intention of understanding how this muscle contributes to the normal mechanics of the scapula as well as the entire shoulder region. This paper can guide the clinician with planning exercises that specifically target the different parts of the trapezius. It is recommended that this paper be read as a companion to another paper: Kinesiologic considerations for targeting activation of scapulothoracic muscles – part 1: serratus anterior.
Introduction
Scapular position, stability, and control play an important role in the strength and integrity of shoulder movement. These elements are highly dependent on the interplay of several scapulothoracic muscles. The serratus anterior and trapezius constitute the main force couple acting at the scapula. Weakness or improper activation of the scapular stabilizers can alter scapular positioning and mechanics. This paper is part 2 of a companion paper.1 Part 1 reported kinesiologic and therapeutic considerations for targeting the activation of the serratus anterior. This review paper will take a similar approach to describe the therapeutic applications to the trapezius muscle. As a background, this review will also present the anatomy, kinesiology, and pathokinesiology of this complex muscle.
Anatomic considerations
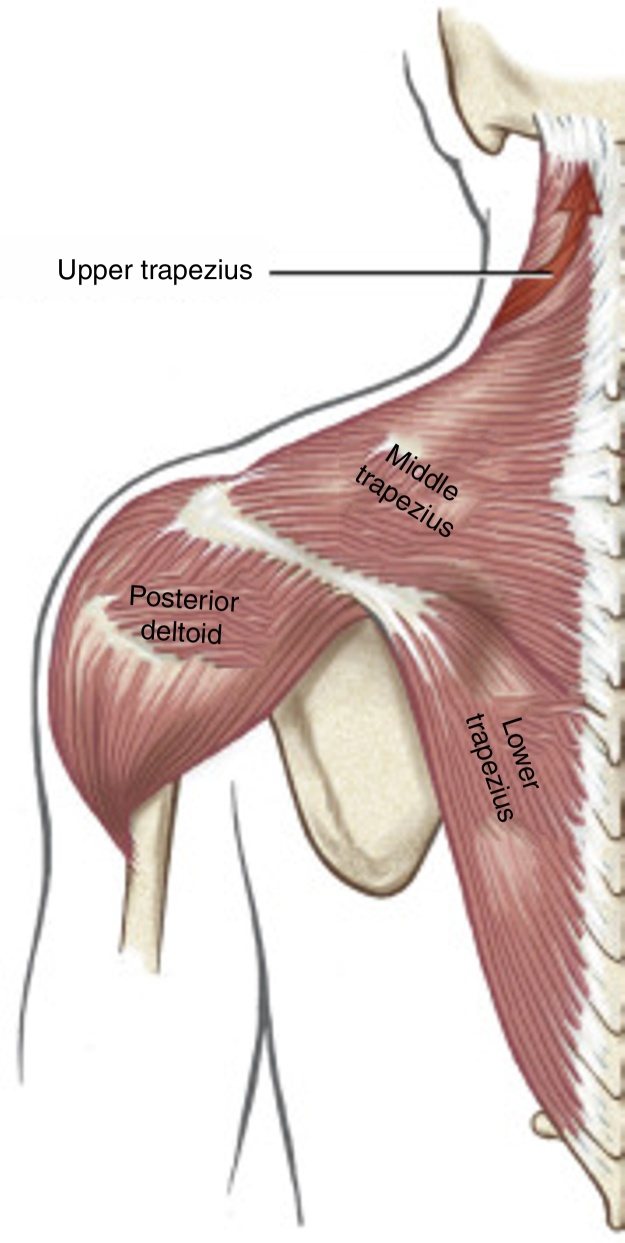
The trapezius is the most visually prominent and superficial of all scapulothoracic muscles (Fig. 1). This extensive muscle is subdivided into upper, middle and lower parts.2 The upper trapezius arises from the occiput, superior nuchal ligament, and spinous processes from vertebra as low as C6, with most fibers descending near vertically to attach to the posterior border of the distal third of the clavicle. The middle and lower trapezius originate from the spinous processes of C7 through T12. The horizontally running middle trapezius attaches to the acromion and spine of the scapula, while the lower trapezius runs obliquely superiorly to attach to the medial base of the scapular spine. As noted in Fig. 1, the different parts of the trapezius have distinctly different fiber directions, hence explaining the muscle's multiple actions.
Figure 1.
The 3 parts of the trapezius muscle. The posterior deltoid is also illustrated. Note that the red arrow shows the line of action of the upper trapezius muscle.
Reproduced with permission from Neumann DA, Kinesiology of the Musculoskeletal System: Foundations for Rehabilitation, 3rd ed, Elsevier, 2017.
The trapezius receives its primary motor innervation from the spinal accessory nerve (cranial nerve XI).2 Sensory innervation is received from branches of nerve roots C2, C3 and C4. The spinal accessory nerve courses obliquely inferiorly between the posterior border of the mid portion of the sternocleidomastoid and anterior border of upper trapezius. Injury to the relatively vulnerable nerve may cause paralysis or marked weakness of both the trapezius and sternocleidomastoid muscles. Isolated trapezius weakness typically results in a “drooping” of the shoulder girdle (i.e., depressed and protracted scapula and clavicle), coupled with excessive downward rotation of the scapula.3, 4 The shoulder girdle loses its essential source of muscular stabilization, potentially leading to subluxation of the glenohumeral and sternoclavicular joints if the condition remains chronic.5
Functional considerations
Ultimately, the specific movements caused by contraction of the trapezius are based on which attachment points of the muscle are held most fixed (rigid). For example, with a relatively fixed craniocervical region, upper trapezius elevates and retracts the clavicle; with a relatively fixed clavicle, upper trapezius contributes to craniocervical extension and lateral flexion. Other similar examples can be applied to middle and lower trapezius. With the scapula held relatively fixed, middle trapezius laterally flexes and contralaterally rotates the thoracic spine; with the thoracic spine held fixed, middle trapezius retracts and externally rotates (within the horizontal plane) the scapula.6 As a final example based on this logic, with the scapula fixed, lower trapezius laterally flexes the lower thoracic spine; with the spine held fixed, lower trapezius externally rotates the scapula and depresses the shoulder girdle, and (with assistance of serratus anterior and upper trapezius) upwardly rotates the scapula.7, 8
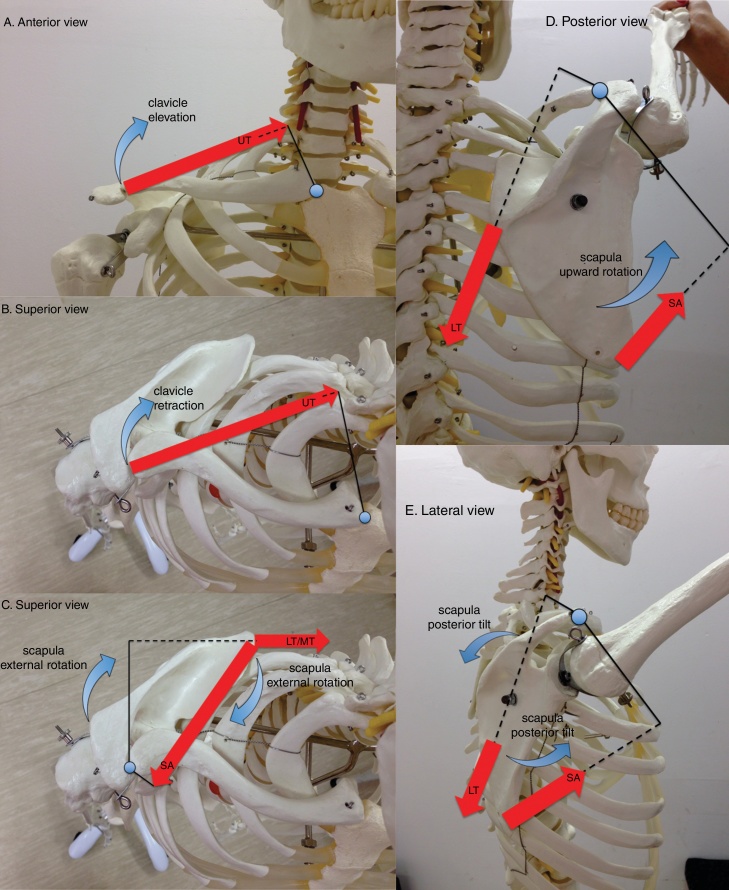
The trapezius and serratus anterior act synergistically to produce many actions of the scapula or clavicle (Fig. 2), typically associated with flexion or abduction of the shoulder. From a broad functional perspective, the trapezius may be considered a dominant stabilizer of the scapula, while the serratus anterior a dominant mover of the scapula, although considerable overlap exists in these generalized functions.
Figure 2.
Lines of action of selected scapulothoracic muscles are depicted by red large straight arrows (UT: upper trapezius, MT: middle trapezius, LT: lower trapezius, SA: serratus anterior). The muscles are shown contributing to clavicular elevation (A), clavicular retraction (B), scapular external rotation (C), scapular upward rotation (D), and scapular posterior tilt (E) during shoulder flexion. Internal moment arms for muscles are shown as a solid line from the axis of rotation to the line of action of each muscle. Dashed lines indicate a right-angle intersection between muscle's line of action and its moment arm. Note two axes of rotation: the sternoclavicular axis, located near the manubrium, and the acromioclavicular axis, located near the acromion.
As the arm is elevated during abduction or flexion, the scapula upwardly rotates, internally/externally rotates, and posteriorly tilts.9, 10, 11, 12, 13 By far, upward rotation is the most obvious and extensive motion, which can be verified by palpating the path of movement of the inferior angle of the scapula. Other more subtle accessory motions refine the position of the scapula as it upwardly rotates. Simultaneous with the upward rotation, for example, the scapula internally or externally rotates, depending of the plane of arm elevation and portion of the range of motion.11 Internal and external rotations of the scapula are also commonly referred as to protraction and retraction, respectively. Although variable, the scapula tends to internally rotate slightly during flexion to project the glenoid fossa more anteriorly; slight external rotation typically occurs at the end range of flexion. Abduction closer to the frontal plane, however, is typically associated with slight external rotation of the scapula, which projects the glenoid fossa closer toward the frontal plane for better congruency with the abducting humerus. The position of the upwardly rotating scapula is further refined by a posterior tilting motion. This relatively consistent motion takes the acromion posteriorly, away from the advancing humeral head. This is likely a mechanical strategy that favors an increase in the subacromial space, thereby reducing likelihood of excessive contact between humeral head and acromion or other soft tissues.
Acting in concert with the serratus anterior, forces produced by each of the three parts of the trapezius are essential to the fluid motion of the scapulothoracic joint and therefore the entire shoulder complex. Scapulothoracic motion and/or stability serves as the basis for all shoulder motions, not just abduction and flexion which are emphasized throughout this paper.
Upper trapezius
Because the upper trapezius attaches distally only to clavicle, most of its influence on scapulothoracic mobility is due to forces applied directly to this bone. Contraction of the upper trapezius creates a strong elevation and a retraction pull on the clavicle at the sternoclavicular joint7, 8, 14 (Fig. 2A and B). The moment arm of the upper trapezius for these actions relative to the sternoclavicular joint is large, conducive for effective torque production and support of the entire upper limb.
Partially because the upper trapezius attaches distally to the clavicle (and not the scapula), its ability to directly control the upward rotation of the scapula is relatively minimal and thus dependent on other muscles.7 Nevertheless, by attaching to the clavicle, the upper trapezius exerts a significant influence on other kinematics across the shoulder girdle. Specifically, the forces exerted by the upper trapezius on the clavicle are strongly linked to the natural kinematic coupling that exists between the sternoclavicular and scapulothoracic joints: elevation of the clavicle contributes about 75% of scapular anterior tilt and only 25% of upward rotation of the scapula.15 Clavicular retraction contributes to 100% of scapular external rotation.15 As such, isolated contraction of the upper trapezius contributes modestly to upward rotation, but significantly to external rotation of the scapula.14 Although Neumann has described the upper trapezius has part of a classic force-couple for upward rotation of the scapula,5 this function is secondary and indirect, and only possible with simultaneous activation of the lower trapezius and serratus anterior.
Understanding the effects of a paralysis of a given muscle can help explain a muscle's natural role in movement. Although isolated paralysis of the upper trapezius is rare, such a condition results in a loss of support of the shoulder girdle, along with excessive scapular internal rotation or protraction. Upward rotation of the scapula is typically only minimally impaired, compensated primary by an innervated serratus anterior.
Middle and lower trapezius
The middle and lower trapezius produce scapular retraction by a direct translational pull on the bone. These muscles also externally rotate the scapula via a torque produced across the acromioclavicular joint. The external rotation force produced by the middle and lower trapezius is particularly important during shoulder abduction or flexion, as these muscles must offset the strong lateral translation (protraction) and internal rotation force produced by simultaneous activation of the serratus anterior7 (Fig. 2C). The lower trapezius along with the serratus anterior are the primary upward rotators of the scapula (Fig. 2D), especially during the early and middle range of shoulder abduction.14 The lower trapezius is most aligned to upwardly rotate the scapula during abduction more than during flexion. Although the middle and lower trapezius may partially assist with posterior tilting of the scapula, the primary muscle for this action by far is the serratus anterior8, 14 (Fig. 2E).
Classic manual muscle test of the strength of the trapezius
Manual muscle testing is utilized extensively in the clinic to determine the strength and control of the trapezius. These tests help clinicians determine the most appropriate therapeutic approach to improve muscle performance during the rehabilitation program. The following tests are based primarily on the classic manual muscles tests originally described by Kendall et al.6
One common way to test the strength of the upper trapezius is depicted in Fig. 3A. From a starting position of slight craniocervical ipsilateral lateral flexion, manual resistance is simultaneously applied against craniocervical extension-and-lateral flexion and elevation of the scapula. A weakened trapezius typically results in the lack of ability to bring the acromion of the scapula toward the head.
Figure 3.
Manual muscle test of strength of the upper trapezius (A), middle trapezius (B) and lower trapezius (C).
The strength of the middle trapezius may be tested with subject prone and shoulder externally rotated and abducted near 90°. Resistance is applied on the arm against the motion of shoulder horizontal abduction6 (Fig. 3B). If the medial border of scapula flares and becomes prominent, i.e. excessively internally rotated, the test suggests weakness of the middle trapezius.
Finally, the strength of the lower trapezius may be tested with the subject prone and the shoulder abducted to where the arm is parallel with the fibers of the lower trapezius (about 120°). The subject is asked to hold the arm off the supporting surface as downward resistance is applied against the arm6 (Fig. 3C). The inferior angle of the scapula pulls away from the thorax when the muscle is weak.
The aforementioned testing positions have been shown to produce the greatest electromyographic activity of each portion of the trapezius as compared to other positions.16 In addition to muscle strength, neuromuscular control should also be assessed during movement of the arm. Inadequate neuromuscular control may be evident by abnormal scapula movements, often referred to as “scapular dyskinesis”. Scapular dyskinesis may be detected by having the patient perform bilateral, active, non-weighted and weighted elevation of the arm in the sagittal and frontal planes.17, 18 Although many forms of scapular dyskinesis are possible, the following are typical patterns: (1) the medial border and/or inferior angle of the scapula become prominent, (2) the shoulder excessively shrugs at the beginning of arm elevation, or (3) rapid downward rotation occurs during elevation of the arm.19 Presence of scapular dyskinesis may indicate lack of neuromuscular control (muscle activation or timing) or strength of the scapulothoracic muscles. A simple method to measure scapular upward rotation in a clinical setting with the aid of a goniometer has been previously described.1, 5
Scapular pathomechanics related to altered activation of the trapezius
Appropriate activation of the trapezius and serratus anterior muscles is essential for optimal movement and stabilization of the scapula. This muscular interaction has been studied primarily during the active motions of flexion and abduction of the shoulder. Studies have identified that individuals with shoulder pain during elevation of the arm often present with abnormal or labored scapula movements in conjunction with (1) excessive activation of the upper trapezius and (2) decreased and/or delayed activation of the lower and middle trapezius and the serratus anterior.9, 20 Specifically, excessive activation of the upper trapezius is likely associated with increased elevation of the clavicle coupled with undesired anterior tilt of the scapula.8, 21 Furthermore, studies suggest that decreased activation of the lower trapezius is likely accompanied with reduced scapular upward rotation.8, 20 Delayed activation of the middle trapezius during elevation of the arm has also been measured in individuals with shoulder pain22 and this may be related to undesired increased internal rotation of the scapula and lack of medial stabilization of the scapula on the thorax.
All the aforementioned abnormal scapular movements are typically associated with some underlying shoulder pathology. However, it is unclear if “scapular dyskinesis” is the cause or the result of shoulder pathology. Different mechanisms may contribute to abnormal scapular movements, including pain, soft tissue tightness,23, 24 imbalance in muscle strength or activation,20 muscle fatigue25 and abnormal thoracic posture.26 Although speculation, these alterations in scapular motion during elevation of the arm may alter the effective line of force of the rotator cuff muscles, thereby reducing the active arthrokinematics of the glenohumeral joint. Furthermore, abnormal scapular kinematics may reduce subacromial space, thereby reducing clearance for the rotator cuff tendons and other subacromial structures during elevation of the arm.27
Exercises that selectively target the activation of the trapezius
After a careful clinical examination, the clinician may decide to focus on increasing muscular strength and endurance of specific shoulder muscles or muscle groups. In addition, it may be equally important to focus training on improving neuromuscular control over shoulder movements. Many individuals with shoulder pain do not present with “weakness” (i.e., reduced peak torque upon maximal effort) of the trapezius and serratus anterior. Instead they present with a lack of endurance, control, or timing of specific muscle activation. Because the primary therapeutic goal may not be to induce muscle hypertrophy, it may be useful to incorporate repetitive low-to-moderate level resistive exercises to optimize the most appropriate muscle activation.28 Careful cueing and feedback from the therapist may be helpful. The key to improvement may lie in thoughtful and careful practice of movements, with a focus on building endurance and enhancing quality of the movement. If muscle weakness is observed, then high-load exercises may be necessary to restore strength of specific muscles.
Based on the pathomechanics described earlier in this paper, exercises may need to focus on shoulder movements that are naturally associated with minimal activation of the upper trapezius, while still demanding substantial activation of the lower and middle trapezius and serratus anterior. Exercises that appropriately target activation of the serratus anterior are described in a paper by Neumann and Camargo.1 Additional data are available in the research literature that can help the clinician design exercises that either selectively target or inhibit the activation of various parts of the trapezius muscle during shoulder movements.29, 30, 31, 32, 33 Table 1 shows a sample of these evidence-based exercises intended to serve as a foundation to encourage the clinician to develop even more complex trapezius-based exercises, based on the need and response from the patients.
Table 1.
Exercises that specifically target the trapezius muscle.
| Exercise | Targeted muscle |
|---|---|
| Shrug exercises and retraction (Fig. 4) | Upper trapezius |
| Overhead shrug (Fig. 5) | Upper trapezius |
| Prone horizontal abduction (Fig. 6) | Middle trapezius |
| Retraction overhead (Fig. 7) | Middle trapezius |
| Prone scapular setting (Fig. 8) | Lower trapezius |
| Elevation with external rotation (Fig. 9) | Lower and middle trapezius |
| Prone extension (Fig. 10) | Lower and middle trapezius |
| Side-lying external rotation (Fig. 11) | Lower and middle trapezius |
| Side-lying forward flexion (Fig. 12) | Lower and middle trapezius |
| Prone I, T, Y (Fig. 13) | Lower and middle trapezius |
As a general guide to selecting certain exercises associated with trapezius activation, the clinician should consider the following guiding principles. Exercises that increase the strength or relative activation of the upper trapezius may be counterproductive in many patients with shoulder pain, especially those with symptoms of impingement. The upper trapezius naturally causes an increased anterior tilt of the scapula, which may compromise the volume within the subacromial space. The exception may be those patients that present with obvious weakness of the upper trapezius and subsequently show a depressed or protracted posture of their shoulder girdle. Shoulder-shrug type exercises may be appropriate in these cases. Patients presenting either with excess scapular internal rotation with prominence of the medial scapular border may benefit from incorporation of middle trapezius enhanced exercises into their rehabilitation protocol. Patients presenting either with excessive scapular internal rotation/anterior tilt, or reduced scapular upward rotation, may benefit from lower trapezius enhanced exercises into their rehabilitation program.
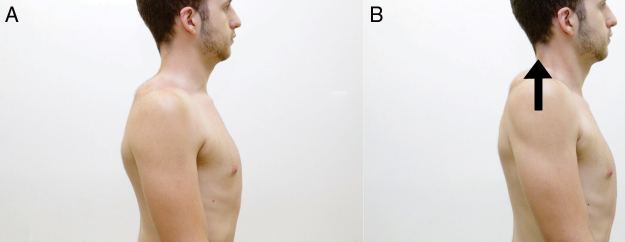
Figure 4.
Shrug exercises and retraction. Exercise starts with the individual with the arms at the side of the trunk and shoulders in retraction (A). Perform the shrug movement (B) and return to the starting position.
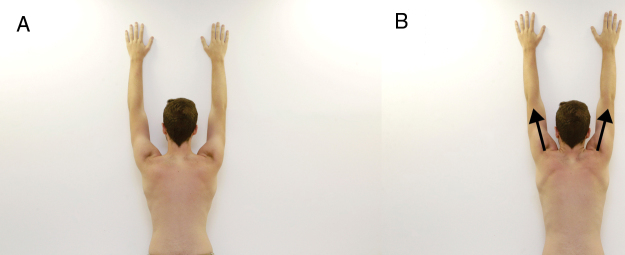
Figure 5.
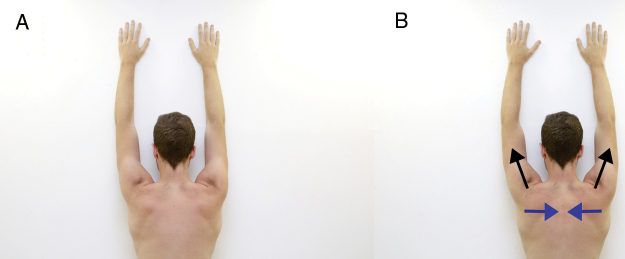
Overhead shrug. Exercise starts with the individual standing, placing the arms in overhead position against the wall (A) and performing a shrug movement (B) and returning to the starting position.
Figure 6.

Prone horizontal abduction. Exercise starts with the individual in prone and arm abducted to 90° with external rotation. Perform horizontal abduction.
Figure 7.
Retraction overhead. Exercise starts with the individual standing, placing the arms in overhead position against the wall (A) and lifting both arms (black arrows) while performing retraction (blue arrows) of the shoulders (B), then return to the starting position.
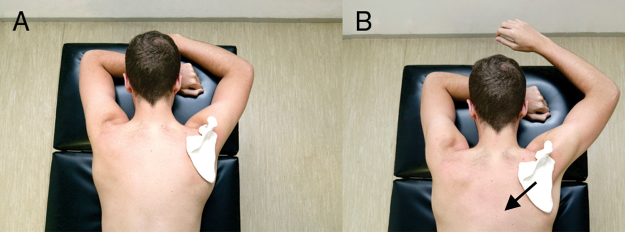
Figure 8.
Prone scapular setting. Exercise starts with the individual lying in prone with the arm in overhead position resting on the treatment table (A). Position the scapula in relative retraction and depression (black arrow). While maintaining this scapular position, lift the arm slightly off the treatment table (B). Avoid shrugging the shoulder and activity of the upper trapezius.
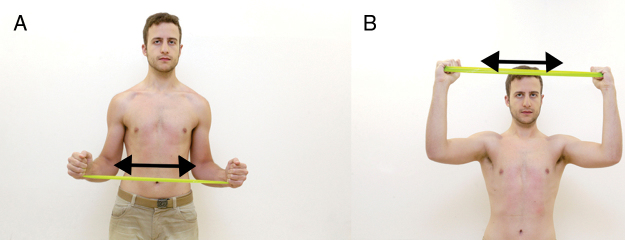
Figure 9.
Elevation with external rotation. Exercise starts with the individual standing, elbows flexed to 90° and an elastic band held in hands. The elastic band is brought to tension with 30° of arms external rotation (A). Elevate both arms to 90° in the scapular plane while holding/maintaining the tension in the band (B).
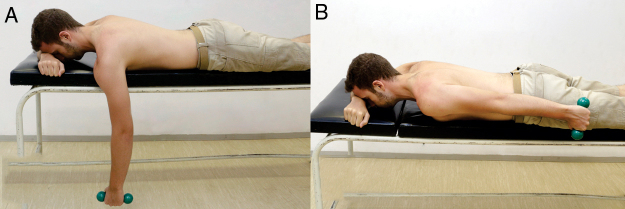
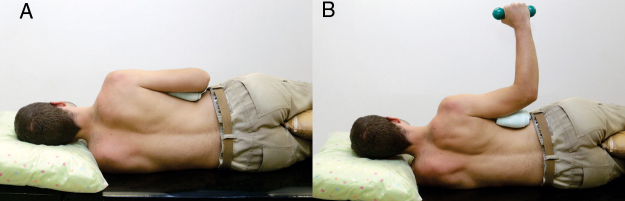
Figure 10.
Prone extension. Exercise starts with the individual in prone with the arm at 90° of forward flexion (A). Perform extension to neutral position with the shoulder in neutral rotation (B).
Figure 11.
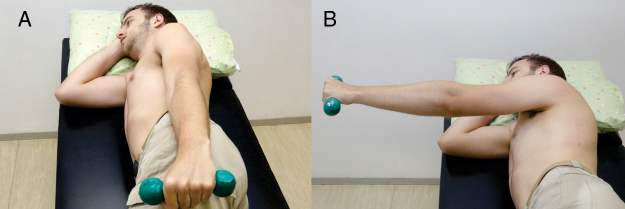
Side-lying external rotation. Exercise starts with the individual in the side-lying position with the shoulder in neutral position and elbow flexed to 90° (A). Perform external rotation of the shoulder with a towel between the elbow and trunk (B). Avoid compensatory movements.
Figure 12.
Side-lying forward flexion. Exercise starts with the individual in the side-lying position and the arm parallel with the body (A). Perform forward flexion (B).
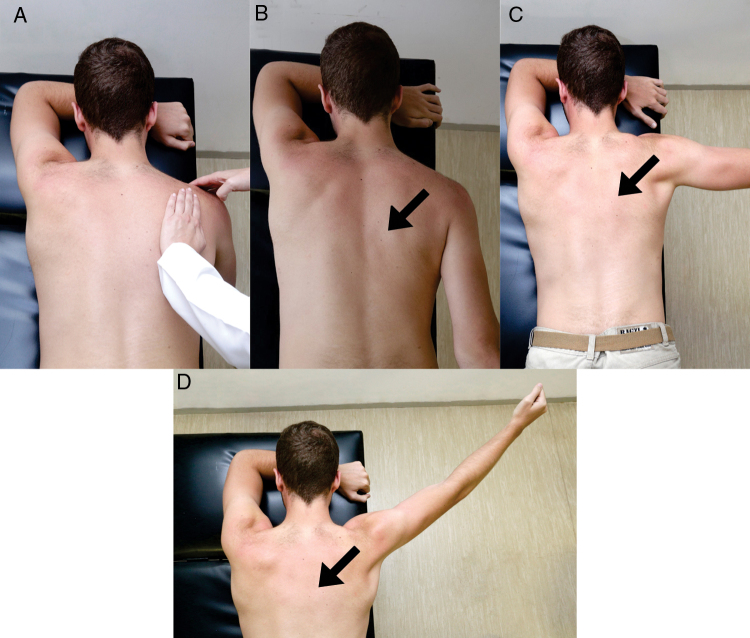
Figure 13.
Prone: Making I, T, Y letters. Exercise starts with the individual lying in prone with arm hanging off the edge of the treatment table (A). Position the scapula in retraction and depression. The therapist can provide feedback with hands. Maintain this position while extending the arm posteriorly in line with the trunk (letter “I”, B), horizontally abducting the arm (letter “T”, C) or elevating the arm to about 120° (letter “Y”, D). Avoid activity of the upper trapezius. The black arrows indicate the importance of maintaining relative scapular retraction and depression during the exercise.
Closing comments
There is still much to be learned about the coordinated activity of the scapulothoracic muscles. Exercises targeting the trapezius and serratus anterior muscles are commonly incorporated into rehabilitation programs with the aim of optimizing scapular position and motion in individuals with shoulder pain. As clinicians, it is important to identify the primary movement impairment contributing to the painful conditions and to determine the potential contributors to the movement impairment.34, 35
Conflicts of interest
The authors declare no conflicts of interest.
References
- 1.Neumann D.A., Camargo P.R. Kinesiologic considerations for targeting activation of scapulothoracic muscles: part 1: serratus anterior. Braz J Phys Ther. 2019;23(6):459–466. doi: 10.1016/j.bjpt.2019.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.De Vita A., Kibler W.B., Pouliart N., Sciascia A. Scapulothoracic joint. In: Di Giacomo G., Pouliart N., Constantini A., DeVita A., editors. Atlas of Functional Shoulder Anatomy. 1st ed. Springer; Milan: 2008. [Google Scholar]
- 3.Wiater J.M., Bigliani L.U. Spinal accessory nerve injury. Clin Orthop Relat Res. 1999;(368):5–16. [PubMed] [Google Scholar]
- 4.Chan P.K., Hems T.E. Clinical signs of accessory nerve palsy. J Trauma. 2006;60(5):1142–1144. doi: 10.1097/01.ta.0000174718.83440.75. [DOI] [PubMed] [Google Scholar]
- 5.Neumann D.A. 3rd ed. Elsevier; St Louis: 2017. Kinesiology of the Musculoskeletal System: Foundations for Rehabilitation. [Google Scholar]
- 6.Kendall F.P., McCreary E.K., Provance P.G., Rodgers M.M., Romani W.A. 5th ed. Lippincott Williams & Wilkins; Baltimore: 2005. Muscles: Testing and Function, with Posture and Pain. [Google Scholar]
- 7.Johnson G., Bogduk N., Nowitzke A., House D. Anatomy and actions of the trapezius muscle. Clin Biomech. 1994;9(1):44–50. doi: 10.1016/0268-0033(94)90057-4. [DOI] [PubMed] [Google Scholar]
- 8.Ludewig P.M., Braman J.P. Shoulder impingement: biomechanical considerations in rehabilitation. Man Ther. 2011;16(1):33–39. doi: 10.1016/j.math.2010.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ludewig P.M., Cook T.M. Alterations in shoulder kinematics and associated muscle activity in people with symptoms of shoulder impingement. Phys Ther. 2000;80(3):276–291. [PubMed] [Google Scholar]
- 10.McClure P.W., Michener L.A., Sennett B.J., Karduna A.R. Direct 3-dimensional measurement of scapular kinematics during dynamic movements in vivo. J Shoulder Elbow Surg. 2001;10(3):269–277. doi: 10.1067/mse.2001.112954. [DOI] [PubMed] [Google Scholar]
- 11.Ludewig P.M., Phadke V., Braman J.P., Hassett D.R., Cieminski C.J., LaPrade R.F. Motion of the shoulder complex during multiplanar humeral elevation. J Bone Joint Surg. 2009;91(2):378–389. doi: 10.2106/JBJS.G.01483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Timmons M.K., Thigpen C.A., Seitz A.L., Karduna A.R., Arnold B.L., Michener L.A. Scapular kinematics and subacromial-impingement syndrome: a meta-analysis. J Sport Rehabil. 2012;21(4):354–370. doi: 10.1123/jsr.21.4.354. [DOI] [PubMed] [Google Scholar]
- 13.Lawrence R.L., Braman J.P., Laprade R.F., Ludewig P.M. Comparison of 3-dimensional shoulder complex kinematics in individuals with and without shoulder pain, part 1: sternoclavicular, acromioclavicular, and scapulothoracic joints. J Orthop Sports Phys Ther. 2014;44(9):636–645. doi: 10.2519/jospt.2014.5339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fey A.J., Dorn C.S., Busch B.P., Laux L.A., Hassett D.R., Ludewig P.M. Potential torque capabilities of the trapezius. J Orthop Sports Phys Ther. 2007;37(1):A44–A45. [abstract] [Google Scholar]
- 15.Teece R.M., Lunden J.B., Lloyd A.S., Kaiser A.P., Cieminski C.J., Ludewig P.M. Three-dimensional acromioclavicular joint motion during elevation of the arm. J Orthop Sports Phys Ther. 2008;38(4):181–190. doi: 10.2519/jospt.2008.2386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ekstrom R.A., Soderberg G.L., Donatelli R.A. Normalization procedures using maximum voluntary isometric contractions for the serratus anterior and trapezius muscles during surface EMG analysis. J Electromyogr Kinesiol. 2005;15(4):418–428. doi: 10.1016/j.jelekin.2004.09.006. [DOI] [PubMed] [Google Scholar]
- 17.McClure P., Tate A.R., Kareha S., Irwin D., Zlupko E. A clinical method for identifying scapular dyskinesis, part 1: reliability. J Athl Train. 2009;44:160–164. doi: 10.4085/1062-6050-44.2.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Uhl T.L., Kibler W.B., Gecewich B., Tripp B.L. Evaluation of clinical assessment methods for scapular dyskinesis. Arthroscopy. 2009;25:1240–1248. doi: 10.1016/j.arthro.2009.06.007. [DOI] [PubMed] [Google Scholar]
- 19.Kibler W.B., Uhl T.L., Maddux J.W., Brooks P.V., Zeller B., McMullen J. Qualitative clinical evaluation of scapular dysfunction: a reliability study. J Shoulder Elbow Surg. 2002;11(6):550–556. doi: 10.1067/mse.2002.126766. [DOI] [PubMed] [Google Scholar]
- 20.Phadke V., Camargo P.R., Ludewig P.M. Scapular and rotator cuff function during arm elevation: a review of normal function and alterations with shoulder impingement. Rev Bras Fisioter. 2009;13(1):1–9. doi: 10.1590/S1413-35552009005000012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ludewig P.M., Reynolds J. The association of scapular kinematics and glenohumeral joint pathologies. J Orthop Sports Phys Ther. 2009;39:90–104. doi: 10.2519/jospt.2009.2808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cools A.M., Witvrouw E.E., Declercq G.A., Danneels L.A., Cambier D.C. Scapular muscle recruitment patterns: trapezius muscle latency with and without impingement symptoms. Am J Sports Med. 2003;31(4):542–549. doi: 10.1177/03635465030310041101. [DOI] [PubMed] [Google Scholar]
- 23.Tyler T.F., Nicholas S.J., Roy T., Gleim G.W. Quantification of posterior capsule tightness and motion loss in patients with shoulder impingement. Am J Sports Med. 2000;28(5):668–673. doi: 10.1177/03635465000280050801. [DOI] [PubMed] [Google Scholar]
- 24.Borstad J.D., Ludewig P.M. The effect of long versus short pectoralis minor resting length on scapular kinematics in healthy individuals. J Orthop Sports Phys Ther. 2005;35:227–238. doi: 10.2519/jospt.2005.35.4.227. [DOI] [PubMed] [Google Scholar]
- 25.Michener L.A., McClure P.W., Karduna A.R. Anatomical and biomechanical mechanisms of subcromial impingement syndrome. Clin Biomech. 2003;18(5):369–379. doi: 10.1016/s0268-0033(03)00047-0. [DOI] [PubMed] [Google Scholar]
- 26.Lee S.T., Moon J., Lee S.H. Changes in activation of serratus anterior, trapezius and latissimus dorsi with slouched posture. Ann Rehabil Med. 2016;40(2):318–325. doi: 10.5535/arm.2016.40.2.318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Graichen H., Bonel H., Stammberger T. Three-dimensional analysis of the width of the subacromial space in healthy subjects and patients with impingement syndrome. Am J Roentgenol. 1999;172(4):1081–1086. doi: 10.2214/ajr.172.4.10587151. [DOI] [PubMed] [Google Scholar]
- 28.Reinold M.M., Escamilla R.F., Wilk K.E. Current concepts in the scientific and clinical rationale behind exercises for glenohumeral and scapulothoracic musculature. J Orthop Sports Phys Ther. 2009;39(2):105–117. doi: 10.2519/jospt.2009.2835. [DOI] [PubMed] [Google Scholar]
- 29.Ekstrom R.A., Donatelli R.A., Soderberg G.L. Surface electromyographic analysis of exercises for the trapezius and serratus anterior muscles. J Orthop Sports Phys Ther. 2003;33:247–258. doi: 10.2519/jospt.2003.33.5.247. [DOI] [PubMed] [Google Scholar]
- 30.Cools A.M., Dewitte V., Lanszweert F. Rehabilitation of scapular muscle balance: which exercises to prescribe? Am J Sport Med. 2007;35:1744–1751. doi: 10.1177/0363546507303560. [DOI] [PubMed] [Google Scholar]
- 31.Castelein B., Cools A., Parlevliet T., Cagnie B., Castelein B.C. Modifying the shoulder joint position during shrugging and retraction exercises alters the activation of the medial scapular muscles. Man Ther. 2016;21:250–255. doi: 10.1016/j.math.2015.09.005. [DOI] [PubMed] [Google Scholar]
- 32.Castelein B., Cagnie B., Parlevliet T., Cools A. Superficial and deep scapulothoracic muscles electromyographic activity during elevation exercises in the scapular plane. J Orthop Sports Phys Ther. 2016;46:2184–2193. doi: 10.2519/jospt.2016.5927. [DOI] [PubMed] [Google Scholar]
- 33.Castelein B., Cagnie B., Cools A. Scapular muscle dysfunction associated with subacromial pain syndrome. J Hand Ther. 2017;30(2):136–146. doi: 10.1016/j.jht.2017.03.006. [DOI] [PubMed] [Google Scholar]
- 34.Ludewig P.M., Kamonseki D.H., Staker J.L., Lawrence R.L., Camargo P.R., Braman J.P. Changing our diagnostic paradigm: movement system diagnostic classification. Int J Sports Phys Ther. 2017;12(6):884–893. [PMC free article] [PubMed] [Google Scholar]
- 35.Sahrmann S., Azevedo D.C., Dillen Van L. Diagnosis and treatment of movement system impairment syndromes. Braz J Phys Ther. 2017;21(6):391–399. doi: 10.1016/j.bjpt.2017.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]