Abstract
Direct carotid-cavernous fistula is a communication between the internal carotid artery and the cavernous sinus, most of the times established following trauma or rupture of a cavernous aneurysm. The most commonly used treatments (coils, detachable latex balloons, stents, or liquid agents) carry ischemic or hemorrhagic risks, related to hemodynamic diversion of cerebral blood flow or permanent dual antiplatelet therapy. We report a case of coiling of a carotid-cavernous fistula assisted by the Comaneci, a temporary adjustable bridging mesh (Rapid Medical, Israel), to avoid transarterial or -venous migration. In our experience, Comaneci-assisted coiling represents a feasible solution to maintain patency of the distal vessels during coiling and avoid dual antiplatelet medications, even using a transradial approach.
Keywords: Radial access, Comaneci, Direct carotid-cavernous fistula, Embolization, Stent
Background
Direct carotid-cavernous fistula (dCCF) is a communication between the internal carotid artery (ICA) and the cavernous sinus (CS), most of the times established following trauma or rupture of a cavernous aneurysm. Typically, it may manifests itself with acute proptosis, chemosis, headache, orbital bruit, as well as palsy of the VI or other cranial nerves. Once the fistula is mature, the high arterial flow combined with venous steal can rapidly lead to intracerebral venous hypertension and brain infarcts. Therefore, a prompt treatment is often necessary to prevent further cerebrovascular injuries. Herein, we report a case of coiling of a carotid-cavernous fistula assisted by the Comaneci, a temporary adjustable bridging mesh (Rapid Medical, Israel), performed by a transradial access.
Case presentation
Two weeks after a transient ischemic attack and fall to the ground that caused a right-sided parietal calvarial fracture, a 70-year-old male, with a history of hypertension and dyslipidemia, presented to the emergency room with new onset of right frontal headache and ocular chemosis.
Ophthalmologic evaluation also showed low visual acuity, bilateral horizontal diplopia, and proptosis, worse in the right eye. Emergent computed tomography and computed tomography-angiography (Fig. 1) reported a direct high flow carotid-cavernous fistula, localized at the cavernous segment of the right internal carotid artery.
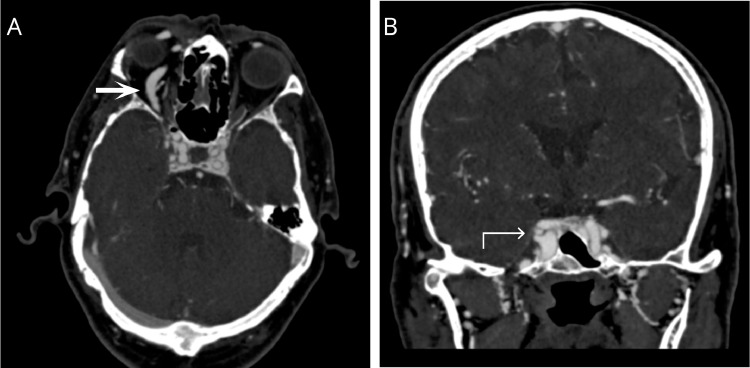
Fig. 1.
Axial (A) and coronal (B) views of contrast-enhanced computed tomography, arterial phase. Arrow: right ophthalmic vein; Curved arrow: right cavernous sinus.
Therefore, a cerebral angiography was obtained, confirming a right CCF with significant reflux to the contralateral CS, pterygoid plexus, ophthalmic and angular veins, inferior petrosal sinus and Galen vein through the basal veins of Rosenthal (Fig. 2). There were no dural contributions and it was considered a type-A fistula, according to Barrow ´s classification [1].
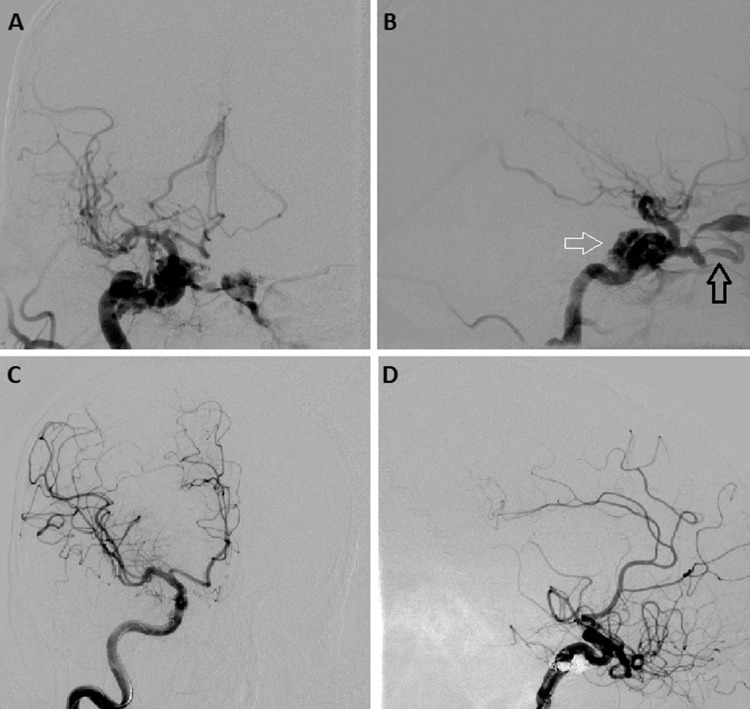
Fig. 2.
(A, B) Digital Subtraction Angiography before Comaneci-assisted coiling of a right direct carotid-cavernous fistula. Early contrast-enhancement of the cavernous sinus (white arrow) and ophthalmic vein (black arrow). Anteroposterior (C) and lateral (D) views with Digital Subtraction Angiography after Comaneci-assisted coiling of a right direct carotid-cavernous fistula.
Treatment
After discussing endovascular options, the patient agreed to be treated through a transarterial access to prevent potential retroperitoneal hematoma, femoral artery pseudoaneurysm, or iatrogenic fistula formation [2], [3], [4]. A preprocedural Allen test was performed, confirming a valid collateral circulation. Therefore, a 6F short introducer was placed in the right radial artery (Terumo Glidesheath Slender) and heparin (i.e., 4000 IU) and antispasmodic medications (i.e., 4 mg Verapamil + 200 mcg of Nitroglycerin) were administered via the sheath.
The tip of a Simmons-2 Envoy DA Neuro-catheter (Codman, Raynham, MA) was preformed to be advanced with a .035” guidewire through the innominate and the right common carotid artery up to the right ICA. Once in the cavernous segment of the ICA, a 0.021” microcatheter (Prowler select; Codman Neurovascular, MA) was inserted through a Y-adapter connected to the lateral port of the Y-adapter of the Envoy and finally located in the ICA distally to the fistula. The Comaneci was loaded into the microcatheter and navigated until an optimal coverage of the arterial side of the dCCF was obtained.
Then, an Excelsior SL10 microcatheter (Stryker Neurovascular, CA) was inserted through the other port of the Y-adapter, parallel to the Comaneci's one, and finally advanced in the fistula. At that time, the Comaneci was gently released by pulling back its microcatheter. The correct diameter was obtained adjusting with the slider on the control handle, since fluoroscopy confirmed that the parent ICA was completely covered by the bridging mesh. Finally, a Comaneci-assisted coiling of the artery–CS communication was performed via the Excelsior SL10 microcatheter deploying 10 coils (ie, 84 cm; Axium, Medtronic and Hydrocoils, Microvention). During coiling, the Comaneci was opened and closed to be sure that coils were not going through the mesh (Fig. 3). Finally, the device was deflated, recaptured with its microcatheter and removed.
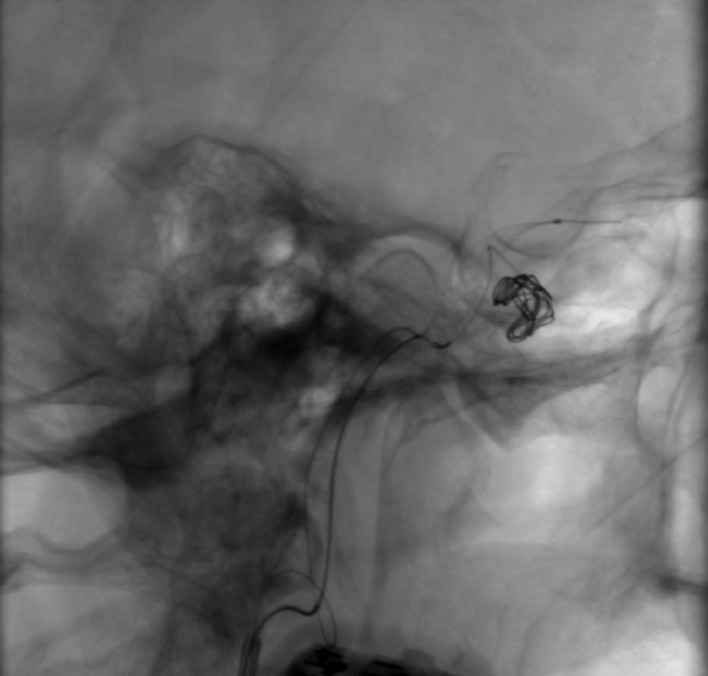
Fig. 3.
Comaneci-assisted coiling a right direct carotid-cavernous fistula.
Postprocedural cerebral angiography demonstrated a complete occlusion of the fistula without intracranial complications. A total of 7000 UI of heparin were administered during the procedure.
Outcome and follow-up
Patient had a complete resolution of the chemosis after the procedure. At 7 month follow-up, there was no recurrence of symptoms, despite the patient still present some weak diplopia.
Discussion
There are 2 main treatment options for carotid-cavernous fistulas: the first approach is to sacrifice the artery above and below the fistula, while the alternative one is to close the fistulus rent preserving the artery. Both are feasible solutions by using coils, detachable latex balloons, stents, or liquid agents.
Among risks that each treatment carry on, there is some uncertainty in releasing devices while avoiding transarterial or -venous migration, with unpredictable consequences. Indeed, standard coiling or liquid agents are related with thromboembolic complications or vessel occlusions caused by a potential dislocation into the parent vessels [5].
To address this issue, the transarterial placement of a temporary balloon or a permanent bare metal stent [6], [7] is often considered. However, even these solutions introduce an ischemic or hemorrhagic risk. Indeed, balloon angioplasty determine a temporary undesiderable hemodynamic diversion of cerebral blood flow while permanent dual antiplatelet therapy is needed to prevent in-stent complications. Instead, the Comaneci represents a solution to maintain patency of the distal vessels during coiling and avoid dual antiplatelet medications since the device is removed once a good coil packing is obtained.
In our experience, during coiling the device provides a temporary bridging mesh, similar to balloon-assisted embolization but without any hemodynamic diversion of brain circulation.
Moreover, our case report demonstrates that coil occlusion of dCCF assisted by the Comaneci is feasible even when using a transradial approach.
Learning points/take home messages
-
1.
Direct carotid-cavernous fistula is a communication between the internal carotid artery and the cavernous sinus, most of the times established following trauma or rupture of a cavernous aneurysm.
-
2.
The most commonly used treatments carry ischemic or hemorrhagic risks, related to hemodynamic diversion of cerebral blood flow or permanent dual antiplatelet therapy.
-
3.
The Comaneci-assisted coiling represents a feasible solution to maintain patency of the distal vessels during coiling and avoid dual antiplatelet medications, even using a transradial approach.
Compliance with ethical standards
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Institutional Review Board (IRB) approval: Informed consent was obtained from all individual participants included in the study.
Consent for publication: Consent for publication was obtained for every individual person's data included in the study.
Footnotes
Funding: This study was not supported by any funding.
Declaration of Competing Interests: The authors declare that they have no conflict of interest.
References
- 1.Barrow D.L., Spector R.H., Braun I.F., Landman J.A., Tindall S.C., Tindall G.T. Classification and treatment of spontaneous carotid-cavernous sinus fistulas. J Neurosurg. 1985;62(2):248–256. doi: 10.3171/jns.1985.62.2.0248. [DOI] [PubMed] [Google Scholar]
- 2.Jolly S.S., Yusuf S., Cairns J., Niemelä K., Xavier D., Widimsky P. Radial versus femoral access for coronary angiography and intervention in patients with acute coronary syndromes (RIVAL): a randomised, parallel group, multicentre trial. Lancet. 2011;377(9775):1409–1420. doi: 10.1016/S0140-6736(11)60404-2. [DOI] [PubMed] [Google Scholar]
- 3.Rao S.V., Ou F-S, Wang T.Y., Roe M.T., Brindis R., Rumsfeld J.S. Trends in the prevalence and outcomes of radial and femoral approaches to percutaneous coronary intervention: a report from the National Cardiovascular Data Registry. JACC Cardiovasc Interv. 2008;1(4):379–386. doi: 10.1016/j.jcin.2008.05.007. [DOI] [PubMed] [Google Scholar]
- 4.Goyal M., Demchuk A.M., Menon B.K., Eesa M., Rempel J.L., Thornton J. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015;372(11):1019–1030. doi: 10.1056/NEJMoa1414905. [DOI] [PubMed] [Google Scholar]
- 5.Kim D.J., Kim D.I., Suh S.H., Kim J., Lee S.K., Kim E.Y. Results of transvenous embolization of cavernous dural arteriovenous fistula: a single-center experience with emphasis on complications and management. AJNR Am J Neuroradiol. 2006;27(10):2078–2082. [PMC free article] [PubMed] [Google Scholar]
- 6.Morón F.E., Klucznik R.P., Mawad M.E., Strother C.M. Endovascular treatment of high-flow carotid cavernous fistulas by stent-assisted coil placement. AJNR Am J Neuroradiol. 2005;26(6):1399–1404. [PMC free article] [PubMed] [Google Scholar]
- 7.Lee C-Y, Yim M-B, Kim I-M, Son E-I, Kim D-W. Traumatic aneurysm of the supraclinoid internal carotid artery and an associated carotid-cavernous fistula: vascular reconstruction performed using intravascular implantation of stents and coils. Case report. J Neurosurg. 2004;100(1):115–119. doi: 10.3171/jns.2004.100.1.0115. [DOI] [PubMed] [Google Scholar]