Abstract
Impulsivity is associated with smoking, difficulties quitting smoking, and approach tendencies toward cigarette stimuli among adolescents. We examined the effects of impulsivity on (a) the association between approach tendencies and adolescents’ smoking status and (b) the effectiveness of Cognitive Bias Modification (CBM), a smoking cessation intervention focused on changing approach tendencies, among adolescent smokers. We conducted a secondary analysis of evidence from 2 previous published studies: Study 1: a cross-sectional study comparing impulsivity and approach tendencies between adolescent smokers (n = 67) and nonsmokers (n = 58); Study 2: a treatment study that randomized 60 adolescent smokers to receive either CBM or sham training. Impulsivity was measured using the Barratt Impulsiveness Scale (BIS) and the Experiential Discounting Task (EDT). We found higher impulsivity, as determined by the BIS but not the EDT, increased adolescents’ odds of being smokers. We observed that the interaction between EDT and approach tendencies also significantly predicted smoking status, however post hoc comparisons were not significant. Adolescents with higher BIS scores receiving CBM had increased odds of being abstinent at the end of treatment, but we found no association between EDT and treatment outcome. Our findings suggest that approach-bias modification (a form of CBM) may be more effective in impulsive adolescent smokers. Differences in findings for BIS and EDT highlight the complexity of the construct of impulsivity. Future studies with larger samples are needed to further disentangle the effects of different aspects of impulsivity on smoking behaviors and cessation outcomes among youth.
Keywords: adolescent, approach-avoidance bias, cognitive bias modification, impulsivity, smoking
Despite numerous prevention and cessation efforts, cigarette smoking remains one of the leading causes of death worldwide (World Health Organization, 2015). Existing evidence clearly suggests that smoking is typically initiated during adolescence, leading to a greater likelihood of becoming addicted (Centers for Disease Control and Prevention, 2015). Youth smoking is a concern not only in the U.S., but also in other countries. For instance, 9% of U.S. 12th graders (Childstats.gov, 2015) and 12% of Dutch 15-year-olds (De Looze et al., 2013) are daily smokers. Although adolescent smokers want to quit smoking, they are not usually successful (Sussman & Sun, 2009). Thus, there is an urgent need for more effective smoking cessation interventions for adolescent smokers.
Tailoring cessation programs to individual characteristics, especially to high-risk youths, may be the key to the development of effective smoking cessation and prevention intervention for youth smokers. High impulsivity is considered to be a risk factor for adolescent substance use (Elkins, King, McGue, & Iacono, 2006; Stautz & Cooper, 2013). Impulsivity is a complex construct (Dick et al., 2010) which is thought to encompass different aspects such as impulsive motor actions, a lack of planning and impaired attention (Patton, Stanford, & Barratt, 1995). Because of its complexity, impulsivity is often measured using different self-report and behavioral measures, all of which seem to assess slightly different aspects and therefore often correlate poorly (Caswell, Bond, Duka, & Morgan, 2015; J. L. White et al., 1994). There is some evidence to suggest that adolescent substance use, including smoking, increases impulsivity (Treur et al., 2015; H. R. White et al., 2011).
Previous studies have consistently found adolescent smokers to score higher on behavioral and self-report impulsivity measures compared with nonsmokers (Audrain-McGovern et al., 2004; Memetovic, Ratner, Gotay, & Richardson, 2016; O’Loughlin, Dugas, O’Loughlin, Karp, & Sylvestre, 2014; Reynolds et al., 2007). Interestingly, impulsivity might not only be a risk factor for smoking, but it may also influence the success of smoking cessation efforts among adolescents. For instance, Krishnan-Sarin et al. (2007) implemented a 4-week smoking cessation intervention combining contingency management (CM) and cognitive–behavioral therapy (CBT) for adolescent smokers, and observed that adolescents achieving smoking abstinence at end of treatment (EOT) were less impulsive (as measured by a behavioral measure of delay discounting), when compared with those who did not achieve abstinence. Further, a secondary data analysis of a follow-up trial that tested the individual and combined effects of CBT and CM, observed that impulsive smokers who received CM based rewards for abstinence had higher abstinence rates when compared with impulsive smokers who did not receive CM for abstinence (Morean et al., 2015). These findings indicate that impulsive adolescent smokers may respond differently to smoking cessation interventions. Therefore, a better understanding of the role of impulsivity in smoking behaviors is needed to improve cessation interventions for this high-risk group of adolescent smokers.
The role of impulsivity in adolescent smoking can be understood in the context of dual process theories of addiction. According to Wiers et al.’s (2007) dual process theory of adolescent addiction, addictive approach behaviors are the result of an imbalance between two qualitatively different types of processes: impulsive and reflective processes. Impulsive processes are fast and associative and are influenced by affective states, with positive affect eliciting addictive approach behaviors. Reflective processes, in contrast, operate more slowly and render self-control in approach behaviors through consideration of past and possible future consequences of actions (Strack & Deutsch, 2004). In an addicted individual, reflective processing is often diminished, resulting in greater impulsivity and lower self-control, especially when faced with cues associated with drug use. In addition, repeated drug use in the addicted individual also enhances approach tendencies toward the drug and drug cues. Approach tendencies are believed to reflect automatic action tendencies of approach that are triggered by the subjectively positive valence of a stimulus. With continued drug use, approach tendencies toward drug stimuli become stronger, and can only be weakly controlled by the poorly developed reflective system (Robinson & Berridge, 2003; Stacy & Wiers, 2010). This phenomenon is expected to be even more pronounced in adolescents who are developmentally prone to heightened impulsivity (R. W. Wiers et al., 2007). Thus, adolescent smokers, because of their weak reflective system, would be expected to score higher on impulsivity, and also to display stronger approach tendencies toward cigarette stimuli compared to nonsmokers.
Approach tendencies can be assessed using a computerized Approach Avoidance Task (AAT; Rinck & Becker, 2007). In this task, participants are instructed to respond to various pictures with either an approach movement (i.e., pulling a joystick which increases the size of the picture) or an avoidance movement (i.e., pushing a joystick away which makes the picture smaller); this zooming effect creates a sensation of approach or avoidance. Previous studies with adults that used variations of this task found stronger approach biases toward substance-related stimuli, including cigarettes, compared with neutral stimuli. These differences in approach biases were more pronounced in substance users, compared to nonusers (Bradley, Field, Mogg, & De Houwer, 2004; Bradley, Field, Healy, & Mogg, 2008; Mogg, Field, & Bradley, 2005; C. E. Wiers et al., 2013). In contrast, our earlier work (Larsen et al., 2014) examining approach tendencies in adolescents did not detect an approach bias toward cigarette stimuli among adolescent smokers when compared to adolescent nonsmokers.
Given that impulsivity is known to be heightened during adolescence (Steinberg & Chein, 2015) and adolescent smokers are known to be more impulsive than nonsmokers (Lewis, Harris, Slone, Shelton, & Reynolds, 2015; Reynolds et al., 2007), heightened impulsivity in adolescent smokers may enhance approach tendencies to cigarette cues. In the present study, we first conducted a secondary data analysis of the evidence collected in Larsen et al. (2014) to examine whether impulsivity has a moderating effect on the association between approach tendencies and smoking status. We hypothesized that a co-occurrence of high impulsivity and strong approach tendencies would increase the odds of being a smoker relative to being a nonsmoker.
Because approach tendencies play a role in addiction, they have also been a target for interventions. Cognitive Bias Modification (CBM) is a computerized intervention aimed at changing approach tendencies through the use of a modified AAT that trains individuals to push away the smoking-related stimuli (Eberl et al., 2013; C.E. Wiers et al., 2014; Kong et al., 2015). CBM is thought to work by decreasing approach tendencies toward smoking stimuli, thereby weakening the impulsive system and allowing for an improved reflective control of smoking behavior in the presence of smoking stimuli.
CBM has shown promising results when used in the treatment of adults with alcohol addiction (Eberl et al., 2013; C. E. Wiers et al., 2014), online gaming addiction (Rabinovitz & Nagar, 2015), and smoking (Macy, Chassin, Presson, & Sherman, 2015). However, only a limited number of studies have used CBM to treat adolescent addictions. Our previous work (Kong et al., 2015) tested the efficacy of CBM, when provided with Cognitive Behavioral Therapy (CBT), in a 4-week long randomized controlled trial (RCT) with adolescent smokers in the U.S. and in the Netherlands. Although we did not find a change in approach tendencies over the course of treatment, we observed a trend toward higher EOT abstinence in the CBM group compared to the control group. Given the close connection between impulsivity and approach tendencies, it is possible that CBM might be more effective for impulsive adolescents. Thus, in the present study, we also conducted a secondary data analysis of the evidence collected in Kong et al.’s (2015) study to examine the role of impulsivity on the efficacy of the CBM intervention. We hypothesized that more impulsive smokers would benefit more from the CBM intervention than less impulsive smokers.
Method
We briefly review key aspects of the Larsen et al. (2014) and Kong et al. (2015) study designs below.
Participants
Hypothesis 1.
To address the first hypothesis (i.e., Impulsivity moderates the association between approach tendencies and smoking status), we analyzed the data from both Study 1 and 2; Study 1 (Larsen et al., 2014): smokers: n = 66 (American: n = 26; Dutch: n = 40); nonsmokers: n = 58 (American: n = 20; Dutch: n = 38); Study 2 (Kong et al., 2015): smokers: N = 75 (American: n = 26; Dutch: n = 49). For this study, we examined baseline evidence prior to initiating treatment (Kong et al., 2015). The total combined sample included 141 adolescent smokers (Dutch [n = 89]; American [n = 52]) and 58 nonsmokers (Dutch [n = 38]; American [n = 20]). Participants were 13–18 years old (M = 16.27; SD = 1.31). The smokers (defined as self-reported smoking at least 5 cigarettes daily for at least 6 months) from Study 1 and 2 did not differ significantly on any of the baseline measures (see Table 1).
Table 1.
Sample Characteristics for Hypothesis 1 and 2
| Variable | Hypothesis 1: Study 1 and 2 combined (N = 199) | Hypothesis 2: Study 2 eligible participants only (N = 60) | |||||
|---|---|---|---|---|---|---|---|
| Nonsmokers (n = 58) | Smokers (n = 141) | CBM (n = 29) | Sham (n = 31) | Abstinent (n = 16) | Nonabstinent (n = 44) | ||
| Age | 15.88 (1.33)a | 16.44 (1.27)a | 16.24 (1.35)b | 16.87 (1.06)b | 16.56 (.81) | 16.57 (1.37) | |
| Sex (Female n/Male n) | 23/35a | 56/84a | 13/16 | 8/23 | 3/13 | 18/26 | |
| Cigarettes per day | — | 11.56 (6.43) | 13.10 (6.30) | 13.06 (7.89) | 10.81 (5.68) | 13.91 (7.44) | |
| Age at first cigarette | — | 12.92 (1.75) | 13.14 (2.01) | 12.32 (2.07) | 12.59 (2.60) | 12.76 (1.85) | |
| mFTQ | — | 2.71 (1.40) | 2.75 (1.34) | 2.96 (1.36) | 2.25 (1.31)c | 3.08 (1.30)c | |
| Bias mean | 21.12 (86.46) | 6.76 (120.43) | −7.25 (179.56) | −24.96 (1.36) | 47.41 (107.83) | −25.73 (148.59) | |
| BIS | 66.02 (6.64) | 68.43 (10.68) | 73.09 (12.81) | 70.08 (10.60) | 69.73 (15.70) | 72.26 (9.55) | |
| EDT | .15 (.25) | .14 (.20) | .12 (.13) | .19 (.25) | .16 (.19) | .16 (.24) | |
Note. Standard deviations appear in parentheses next to means; mFTQ = modified Fagerström Tolerance Questionnaire; BIS = Barratt Impulsiveness Scale 11 – total score; EDT = Experiential Discounting Task - area under the curve.
Smokers are significantly older and more likely to be male (p < .01).
Participants in the sham condition were significantly older (p = .05).
Participants who did not stay abstinent scored significantly higher (p = .03).
Hypothesis 2.
To address the second hypothesis (i.e., CBM + CBT treatment will be more effective for impulsive adolescents), we used evidence from Study 2 (Kong et al., 2015). A total of 60 adolescent smokers (Dutch [n = 42] and American [n = 18]) were randomized to four weeks of CBM + CBT (n = 29) or sham + CBT (n = 31) treatment.
Procedures
Recruitment procedures.
For both studies, participants were recruited in local public high schools in the United States (New Haven area, Connecticut) and The Netherlands (Amsterdam and Haarlem area). Prior to recruitment, information letters were sent out to inform parents about the details of the study and giving them the opportunity to contact the research team if they did not want their child to participate. Interested adolescents signed up at recruitment tables during lunch period. Assent was obtained from adolescents 14–17 years old and consent was obtained from 18 years and older. In both studies, participants had to be between ages 14 and 18, and exclusion criteria were meeting the current criteria for dependence on another psychoactive substances, diagnosis of psychosis, major depression or panic disorder as evaluated by a trained clinician, and the use of psychotropic medication less than 2 months prior to the assessment. No participants were excluded based on these criteria (Larsen et al., 2014). For Study 2, an additional inclusion criterion was willingness to participate in a smoking cessation program (Kong et al., 2015).
Ethics.
Both studies were approved by the Ethical Committee of the Faculty of Social Sciences, University of Amsterdam, the Institutional Review Board at Yale University School of Medicine, and participating schools.
Study procedures.
Study 1.
Smokers and nonsmokers were recruited into this study. Research assistants administered the assessments to each participant within a single session. Participants were reimbursed for their participation with €5 (NL) or $25 (U.S.).
Study 2.
Research assistants administered the assessments to each participant at baseline prior to treatment. Eligible participants (see below for smoking criteria) were randomized into the 4-week smoking cessation intervention where adolescent smokers received weekly CBT for smoking cessation with either CBM or sham training. Participants could receive up to €50 (NL) or $180 (U.S.) for their participation.
Measures
All measures indicated below were obtained in both Study 1 and 2.
Smoking status at baseline was assessed with an open-ended question inquiring about the number of cigarettes smoked per day over the last 6 months. Smokers had to report having smoked at least five cigarettes per day over the last 6 months. Nonsmokers had to report never smoking a cigarette in their lifetime. We also assessed the number of cigarettes and days smoked using Time Line Follow Back (TLFB; Sobell, Toneatto, Sobell, Leo, & Johnson, 1992; Lewis-Esquerre et al., 2005) on a weekly basis during the treatment period in Study 2. Self-report of not smoking any cigarettes in the last 7 days prior to end of treatment (EOT) was considered abstinence.
Nicotine dependence was assessed among smokers using the modified Fagerström Tolerance Questionnaire (mFTQ; Prokhorov, Pallonen, Fava, Ding, & Niaura, 1996). The mFTQ summed score ranges from 0 to 9 (0–2 = no nicotine dependence, 3–5 = moderate dependence, 6–9 = high dependence; Farber & Sachs, 2010).
Approach-avoidance bias was assessed using the computerized Smoking Approach Avoidance Task (S-AAT; Larsen et al., 2014; Watson, Cousijn, Hommel, & Wiers, 2013). In brief, participants were presented with neutral or cigarette images that were rotated 3° to the left or to the right. Participants were instructed to push the stimuli away or pull the stimuli toward themselves using a joystick depending on the orientation of the image, and not on the image content. To increase the perception of pulling or pushing, the image decreased in size if pushed, and increased in size if pulled. A total of 40 images were used (20 smoking-related, 20 neutral) and each image was presented four times, twice rotated in each direction (total number of trials N = 160). Reaction times (RT) were measured for each trial. To correct for outliers, RTs below 200 ms, and more than 3 SD above and below the individual mean were removed for each participant. Approach and avoidance biases were calculated for cigarette- and neutral images separately, by subtracting the mean RT for each image type in the pull condition from the mean RT for the same image type in the push condition. Based on these values, a mean bias value (bias mean) was calculated by subtracting the bias for cigarette images from the bias for neutral images. Positive bias mean values indicate that approach tendencies are stronger than avoidance tendencies.
Impulsivity was assessed with the Barratt Impulsiveness Scale (BIS-11; Patton et al., 1995) and the Experiential Discounting Task (EDT; Reynolds & Schiffbauer, 2004).
The BIS-11 is a 30-item self-report measure of trait impulsivity. Cronbach’s alpha of the present sample was acceptable at .75. We used the BIS total score in our analysis (Du et al., 2016).
The EDT measures participants’ ability to delay gratification. It is a computerized behavioral measure assessing the rate at which a monetary reward loses its subjective value depending on the delay and probability with which it is received. In the EDT version used (Reynolds & Schiffbauer, 2004), participants received the reward at the end of the session. Monetary rewards were converted into Euros for the Dutch sample. The area under the discounting curve (AUC) was used to quantify discounting (Myerson et al., 2001). Smaller AUC values reflect faster discounting and therefore higher impulsivity.
These impulsivity measures were chosen based on our earlier work showing that both measures were related to smoking cessation outcomes among adolescent smokers (Krishnan-Sarin et al., 2007; Morean et al., 2015).
Treatment Conditions for Study 2
Cognitive–behavioral therapy (CBT) for smoking cessation was delivered by experienced therapists with at least a master’s level of education. Therapists followed a manual-guided protocol (Cavallo et al., 2007; Krishnan-Sarin et al., 2006, 2013). The manual was translated into Dutch for participating therapists in The Netherlands. All therapists were supervised by licensed clinical psychologists, and cases were discussed with supervisors on a monthly basis. Participants received a “preparation to quit” CBT session one week prior to quitting, and a “pre-quit” session on the day before quitting. Following the “pre-quit” session, participants had their first CBM or sham training session. CBT therapists were blind to whether participants received CBM or sham training.
Cognitive bias modification (CBM) training was conducted with a modified version of the S-AAT described above (Kong et al., 2015). Unlike the S-AAT, 90% of cigarette images were presented in the push, and only 10% in the pull condition. The opposite was the case for neutral images. As in the S-AAT, 40 different images were used (20 cigarette, 20 neutral). Each CBM session consisted of 260 training trials, during which each image was shown 6.5 times on average. Preceding these training trials, participants completed 15 practice trials, followed by 25 trials during which only 20 of the images were used (10 cigarette, 10 neutral) and each image was presented 50% in the pull and 50% in the push condition. In total, participants completed 300 trials during each session.
Sham training was identical to the S-AAT. Participants receiving sham treatment also completed a total of 300 trials during each session.
Treatment Outcome Measure for Study 2
As mentioned earlier, smoking status during the treatment period was assessed using TLFB procedures (Sobell et al., 1992; Lewis-Esquerre et al., 2005). Abstinence was defined as self-reports of 7-day point prevalence abstinence (7-day PP) at EOT (Hughes, Carpenter, & Naud, 2010); specifically, participants had to report not having smoked in the last 7 days prior to the EOT assessment in order to be coded as abstinent.
Data analysis
All data analysis was conducted using IBM SPSS Statistics version 21 (SPSS Inc., Chicago, IL). All variables were checked for outliers. Scores of both impulsivity measures (EDT, BIS) and bias mean scores were centered prior to the analyses.
Hypothesis 1.
To examine the first hypothesis, whether impulsivity moderated the association between approach tendencies and smoking status, we first used t tests and chi-square tests to evaluate differences in baseline measures between smoking status (smokers vs. nonsmokers) and site (U.S. vs. Netherlands). Then we conducted separate binary logistic regressions for both of the impulsivity measures (BIS and EDT). We assessed the influence of BIS and EDT on smoking status using separate models due to the large number of predictors relative to sample size. Conducting a single binary logistic regression containing all variables would have increased the risk of missing predictive variables due to overfitting the model.
The first logistic regression model tested the effect of BIS and approach tendencies (bias mean) on smoking status. Smoking status was entered as the dependent variable. Predictor variables were BIS, bias mean, and the interaction between BIS and bias mean.
The second logistic regression model tested the effect of EDT and bias mean on smoking status. In this model, smoking status was entered as the dependent variable. Predictor variables were EDT, bias mean, and the interaction between EDT and bias mean.
In both logistic regression models, age and sex were entered as covariates, as they differed significantly between smokers and nonsmokers (see Table 1). Additionally, site (U.S. vs. Netherlands) was entered as covariate, because we found differences in approach and avoidance tendencies between the two sites in previous analyses (Kong et al., 2015; Larsen et al., 2014). We also conducted the two logistic regression models described above by including the smoking bias scores while controlling for neutral bias scores instead of the bias mean. We obtained comparable results so we presented the models using the bias mean.
Hypothesis 2.
Similar to the data analysis for Hypothesis 1, for Hypothesis 2, we examined whether CBM + CBT treatment was more effective for impulsive adolescents by conducting two binary logistic regressions to examine the predictive value of impulsivity (BIS and EDT) and treatment condition (CBM vs. sham) on abstinence.
The first logistic regression model tested the effect of BIS and treatment condition on abstinence. The dependent variable was 7-day PP abstinence. Predictor variables were treatment condition, BIS, and the interaction between BIS and treatment condition.
The second logistic regression model tested the effect of EDT and treatment condition on treatment outcome. Again 7-day PP abstinence was entered as the dependent variable. Predictor variables were treatment condition, EDT, and the interaction between EDT and treatment condition.
As for Hypothesis 1, site (U.S. vs. Netherlands) was entered as covariate in both logistic regression models. Additionally, in both logistic regression models, mFTQ was entered as a covariate, as abstinent and nonabstinent participants differed significantly on this measure (see Table 1). Because age and sex did not differ significantly between abstinent and nonabstinent participants (see Table 1), they were not entered as covariates.
Results
Hypothesis 1
Does impulsivity moderate the association between approach tendencies and smoking status?
See Table 1 for baseline variables. Smokers were significantly older than nonsmokers, t(196) = −2.77, p = .006 and more likely to be male χ2[1, N = 198] = 6.83, p = .009). Smokers and nonsmokers did not differ significantly in baseline BIS total score, bias mean, or EDT.
The logistic regression model showed that the interaction between BIS and bias mean was not significant, but that BIS was associated with smoking status (p = .05, OR = 1.04; Table 2). There was a 27% increase in odds of being a smoker with a one standard deviation increase in the BIS score. Although EDT by itself was not predictive of smoking status, the interaction between EDT and bias mean was significant (p = .03, OR = 0.97; Table 2).
Table 2.
Results of the Logistic Regression Models With Smoking Status as Dependent Variable
| Predictor | β | SE β | Wald’s χ2 | df | p | eβ (Odds ratio) |
|---|---|---|---|---|---|---|
| Dependent variable: Smoking status | ||||||
| BIS | ||||||
| Constant | −3.54 | 2.45 | 2.07 | 1 | .15 | NA |
| Bias mean | −.001 | .002 | .27 | 1 | .60 | 1.00 |
| BIS total score | .04 | .02 | 3.95 | 1 | .05 | 1.04 |
| Bias Mean × BIS | .000 | .000 | .23 | 1 | .64 | 1.00 |
| Overall model evaluation | ||||||
| Omnibus Test of Model Coefficients | 19.15 | 6 | .004 | |||
| Hosmer & Lemshow | 6.34 | 8 | .61 | |||
| EDT | ||||||
| Constant | −5.23 | 2.19 | 5.69 | 1 | .02 | NA |
| Bias mean | −.003 | .002 | 1.89 | 1 | .17 | 1.00 |
| EDT | −.11 | .92 | .01 | 1 | .91 | .90 |
| Bias Mean × EDT | −.03 | .01 | 5.02 | 1 | .03 | .97 |
| Overall model evaluation | ||||||
| Omnibus Test of Model Coefficients | 23.69 | 6 | .001 | |||
| Hosmer & Lemshow | 6.81 | 8 | .56 | |||
| Dependent variable: Smoking abstinence at EOT | ||||||
| BIS | ||||||
| Constant | −1.31 | 1.27 | 1.06 | 1 | .30 | .27 |
| Condition | 2.02 | 1.31 | 2.37 | 1 | .12 | 7.56 |
| BIS | −.37 | .17 | 4.75 | 1 | .03 | .69 |
| Condition × BIS | .42 | .17 | 5.76 | 1 | .02 | 1.51 |
| Overall model evaluation | ||||||
| Omnibus Test of Model Coefficients | 22.30 | 5 | .000 | |||
| Hosmer & Lemshow | 6.30 | 8 | .61 | |||
| EDT | ||||||
| Constant | .31 | .82 | .15 | 1 | .70 | 1.37 |
| Condition | −.02 | .68 | .001 | 1 | .98 | .98 |
| EDT | −.91 | 1.86 | .24 | 1 | .63 | .40 |
| Condition × EDT | 2.94 | 4.28 | .47 | 1 | .49 | 18.96 |
| Overall model evaluation | ||||||
| Omnibus Test of Model Coefficients | 7.03 | 5 | .22 | |||
| Hosmer & Lemshow | 11.18 | 8 | .19 |
Note. BIS = Barratt Impulsiveness Scale 11 – total score; EDT = Experiential Discounting Task (Area under the curve); EOT = end of treatment; mFTQ = modified Fagerström Tolerance Questionnaire; Results for the covariates for the BIS model with smoking status as dependent variable were: Site: β= −.06; SE β= .37; df = 1; p = .87; eβ = .94. Sex: β= −1.09; SE β= .37; df = 1; p = .003; eβ = .34. Age: β= .38; SE β= .14; df = 1; p = .009; eβ = 1.46. Results for the covariate for the EDT model with smoking status as dependent variable were: Site: β= .17; SE β= .36; df = 1; p = .63; eβ = 1.19. Sex: β= 1.08; SE β= .36; df = 1; p = .002; eβ = 2.94. Age: β= .34; SE β= .13; df = 1; p = .01; eβ = 1.40. Results for the covariates for the BIS model with smoking abstinence at EOT as dependent variable were: Site: β= .22; SE β= .85; df = 1; p = .80; eβ = 1.25. mFTQ: β= −.61; SE β= .31; df = 1; p = .05; eβ = .54. Results for the covariates for the EDT model with smoking abstinence at EOT as dependent variable were: Site: β= .70; SE β= .73; df = 1; p = .33; eβ = 2.02. mFTQ: β= −.53; SE β= .26; df = 1; p = .04; eβ = .59.
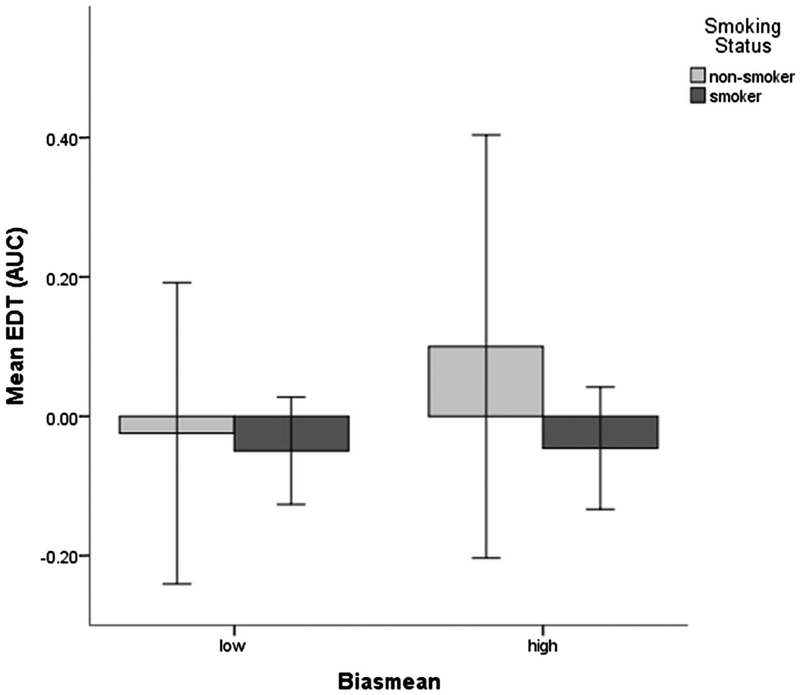
Figure 1 illustrates the direction of the interaction between EDT and bias mean. For post hoc comparison, we assessed the correlation between EDT and bias mean for nonsmokers and for smokers, separately. We did not find any significant associations (smokers: r =C215.04; p = .63; nonsmokers: r = .22; p = .09). We also categorized bias mean into low and high based on SD (Bias mean high [H11350] Mean + 1 SD; Bias mean low ≤ Mean – 1 SD) and conducted t tests to examine the difference between EDT and low/high bias mean separated by smoking status (see Figure 1). There were no differences in EDT scores between participants with high bias mean scores and participants with low bias mean scores (smokers, t(24) = −.07, p = .95, and nonsmokers, t(9) = .84, p = .42).
Figure 1.
This figure illustrates the direction of the interaction effect between bias mean and EDT. Error bars = 95% Confidence interval; EDT = Experiential Discounting Task (area under the curve; higher scores indicate lower impulsivity); Bias mean high ≥ Mean + 1 Standard Deviation; Bias mean low ≤ Mean + 1 Standard Deviation.
Hypothesis 2
Is CBM + CBT treatment more effective for impulsive adolescents?
See Table 1 for baseline variables. Participants in the sham condition were significantly older than participants in the CBM condition, t(58) =−2.016, p = .05. Participants in the two conditions did not differ significantly in other variables.
Differences Between Abstinent and Nonabstinent Participants
Participants who were abstinent at EOT had lower mFTQ scores at baseline (abstinent (n = 16): M = 2.25 (SD = 1.31); nonabstinent (n = 44): M = 3.08 (SD = 1.30); t(58) = 2.19, p = .03). Abstinent and nonabstinent participants did not differ in other variables (see Table 1).
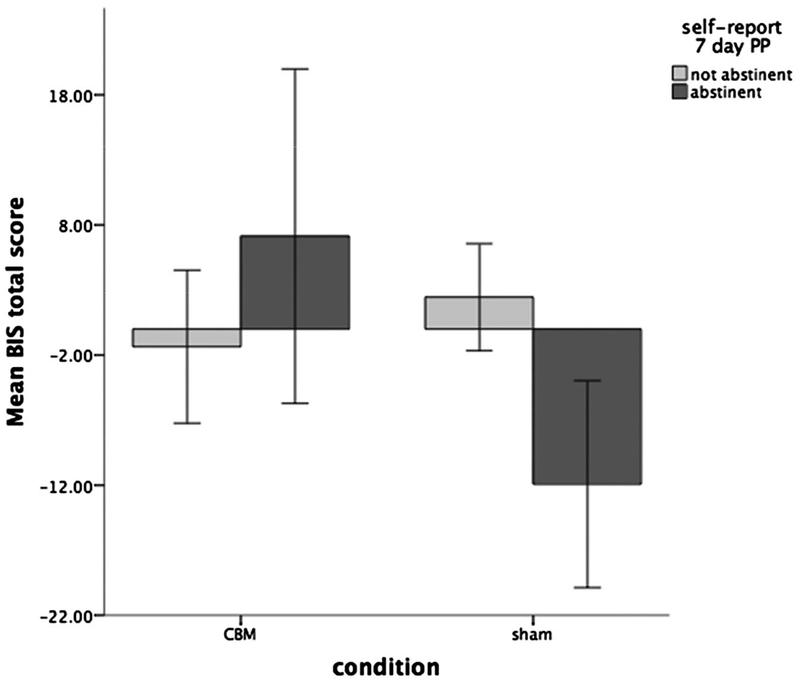
The interaction between BIS and treatment condition was significantly related to treatment outcome (see Table 2). Neither EDT, nor its interaction with condition, were predictive of treatment outcome (see Table 2).
Figure 2 illustrates the interaction between treatment condition and BIS, separated by treatment outcome. We further explored the interaction between BIS and treatment condition using two separate independent sample t tests for abstinent and nonabstinent participants. For abstinent participants, BIS scores differed significantly between the CBM condition and the sham condition, with participants in the CBM condition scoring higher, t(13) = 2.90, p = .01, indicating more impulsivity. For nonabstinent participants there was no difference in BIS scores between the CBM and sham condition, t(32) =−1.16, p = .25.
Figure 2.
This figure illustrates the direction of the interaction effect between treatment condition and BIS Error bars = 95% Confidence interval; BIS = Barratt Impulsiveness Scale 11 – total score; 7-day PP = self-report 7-day point prevalence abstinence.
Discussion
The goals of this study were to (a) investigate whether the co-occurrence of higher impulsivity and stronger approach tendencies toward cigarette-stimuli would increase adolescents’ odds of being a smoker, and (b) to examine whether impulsive smokers would benefit more from a smoking cessation treatment that was focused on retraining these approach tendencies.
Regarding the first hypothesis, we detected a significant interaction between EDT and approach tendencies, which shows evidence that low impulsivity (as indicated by higher EDT scores) in the presence of strong approach tendencies is associated with being a nonsmoker. However, our post hoc analysis did not support this hypothesis. This could be attributable to our small sample size. Future studies with larger sample sizes should further explore the possibility of a moderating effect of impulsivity, as measured with the EDT, on the association between approach tendencies and smoking status.
We further found that more impulsive adolescents, as measured with the BIS, had higher odds of being smokers independent of their approach tendencies toward cigarette stimuli. Previous studies also found adolescent smokers to be more impulsive than nonsmokers (Lewis et al., 2015; Reynolds et al., 2007; Schepis, McFetridge, Chaplin, Sinha, & Krishnan-Sarin, 2011). However, in the current study, impulsivity as assessed using the EDT, was not related to differences in smoking status. This could be attributable to the two measures assessing different aspects of impulsivity. Earlier studies have shown that impulsivity is a multidimensional construct with multiple domains, and that behavioral and self-report measures of this construct do not always measure the same domain (e.g., Meda et al., 2009). Previous research has also shown that the results of self-report and behavioral impulsivity measures do not correlate well (Caswell et al., 2015; J. L. White et al., 1994). Similar to our previous work (Krishnan-Sarin et al., 2007), we did not find a significant correlation between EDT and BIS (r = .02; p = .84) in the current study. Our findings are further evidence for the heterogeneous nature of impulsivity and highlight the importance of considering different impulsivity measures when exploring the effects of impulsivity.
Regarding our second hypothesis, adolescents who were more impulsive on the BIS-11 and received CBM treatment were more likely to report being abstinent than impulsive adolescents who received sham treatment. We found no difference in treatment outcome regarding treatment condition for nonimpulsive adolescents. These findings suggest that smoking cessation among impulsive adolescents may be supported by training approach tendencies through CBM.
The finding that CBM differs in efficacy for impulsive and nonimpulsive adolescents corresponds with findings from previous studies that likewise found differences in treatment efficacy depending on participants’ impulsivity. Although cognitive–behavioral therapy (CBT), by itself, appears to be generally less effective for smoking cessation among impulsive adolescents (Krishnan-Sarin et al., 2007; Wegmann, Bühler, Strunk, Lang, & Nowak, 2012), contingency management (CM) was found to be more effective at achieving smoking abstinence among impulsive adolescents (Morean et al., 2015). CM targets difficulties in delaying rewards by offering money or vouchers as a more immediate reward for smoking abstinence (Higgins & Petry, 1999). Instead of offering alternative rewards, CBM is directed at decreasing approach tendencies toward cigarette-stimuli. Decreasing approach tendencies toward cigarette-stimuli is thought to indirectly decrease the incentive value associated with cigarettes (Deutsch, Gawronski, & Strack, 2006).
In sum, both CM and CBM target impulsive processes, whereas CBT targets mainly the reflective processes. Our collective evidence suggests that treatments targeting impulsive processes appear to be beneficial for smoking cessation among impulsive adolescents.
Surprisingly, we did not find a difference in treatment outcome when EDT was used as an impulsivity measure. As discussed above, this could be a result of EDT and BIS assessing different aspects of impulsivity. Future studies that examine the role of impulsivity in adolescent smoking should continue to use both self-report as well as behavioral measures. The use of multiple impulsivity measures might not only help to cover all aspects of impulsivity, but in the long term, further identify these different aspects and their roles in the development of addictive behaviors.
Although results of the present study are promising, there are several limitations that should be acknowledged. First, in the present study, the BIS total scale was used instead of the three subscales suggested by Patton et al. (1995) separately assessing motor, attentional, and nonplanning impulsivity. This was done to decrease the total number of predictors in the logistic regression models to accommodate our limited sample size. It is possible that subscales of the BIS correlate better with the EDT. This possibility is supported by our previous work where we found the BIS subscale to be differently predictive of the outcome of a smoking cessation treatment (Morean et al., 2015).
A further limitation of the present study is that other forms of tobacco use besides conventional cigarettes, particularly e-cigarette use, were not assessed. However, data collection took place between June and September 2012 and e-cigarettes, although currently the most popular tobacco product among adolescents in the U.S., only began to surpass conventional cigarettes in this age group in 2014 (Singh et al., 2016). Moreover, the adolescent smokers who participated in these studies were light smokers. While other research has observed that current adolescent smokers tend to be lighter smokers who smoke fewer than 5 cigarettes per day (ConstanceWiener, Trickett Shockey, & Morgan, 2016), future studies with heavier smokers, as well as those who use other forms of combustible and noncombustible tobacco, are needed. Finally, future larger RCTs are needed to assess the main and interaction effects of CBM and impulsivity on biochemically confirmed smoking cessation outcomes.
In summary, to our knowledge, this study is the first to investigate the effect of impulsivity on (a) the association between approach tendencies toward smoking stimuli and smoking status and on (b) the efficacy of a novel smoking cessation treatment employing CBM. Our results suggest that impulsive adolescents appear to be at a heightened risk for cigarette smoking, and may benefit from the use of CBM for smoking cessation. Larger scale studies, potentially also addressing the influence of peer presence on adolescents’ impulsivity, are needed to further explore the clinical utility of CBM in adolescent smoking cessation treatments.
Public Health Significance.
This study suggests that approach bias modification, a form of cognitive bias modification, may be a more effective treatment for impulsive adolescent smokers compared with nonimpulsive adolescent smokers. This finding supports the importance of considering the effects of impulsivity on adolescent smoking behavior in the research of smoking cessation treatments.
Acknowledgments
This research was supported in part by a supplemental grant to Suchitra Krishnan-Sarin (R01DA01596 and P50DA009241) and a ZONMW grant to Reinout W. Wiers (60-60600-97-305). These sponsors had no role in the study design; collection, analysis or interpretation of the data; writing the manuscript; or the decision to submit the paper for publication.
References
- Audrain-McGovern J, Rodriguez D, Tercyak KP, Epstein LH, Goldman P, & Wileyto EP (2004). Applying a behavioral economic framework to understanding adolescent smoking. Psychology of Addictive Behaviors, 18, 64–73. 10.1037/0893-164X.18.1.64 [DOI] [PubMed] [Google Scholar]
- Bradley BP, Field M, Healy H, & Mogg K (2008). Do the affective properties of smoking-related cues influence attentional and approach biases in cigarette smokers? Journal of Psychopharmacology, 22, 737–745. 10.1177/0269881107083844 [DOI] [PubMed] [Google Scholar]
- Bradley B, Field M, Mogg K, & De Houwer J (2004). Attentional and evaluative biases for smoking cues in nicotine dependence: Component processes of biases in visual orienting. Behavioural Pharmacology, 15, 29–36. 10.1097/00008877-200402000-00004 [DOI] [PubMed] [Google Scholar]
- Caswell AJ, Bond R, Duka T, & Morgan MJ (2015). Further evidence of the heterogeneous nature of impulsivity. Personality and Individual Differences, 76, 68–74. 10.1016/j.paid.2014.11.059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavallo DA, Cooney JL, Duhig AM, Smith AE, Liss TB, McFetridge AK, … Krishnan-Sarin S (2007). Combining cognitive behavioral therapy with contingency management for smoking cessation in adolescent smokers: A preliminary comparison of two different CBT formats. The American Journal on Addictions, 16, 468–474. 10.1080/10550490701641173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2015). Youth and tobacco use. Retrieved December 6, 2015, from http://www.cdc.gov/tobacco/data_statistics/fact_sheets/youth_data/tobacco_use/
- Childstats.gov. (2015). Regular cigarette smoking. Retrieved December 7, 2015, from http://www.childstats.gov/americaschildren/beh1.asp
- ConstanceWiener R, Trickett Shockey AK, & Morgan SK (2016). Adolescent light cigarette smoking patterns and adult cigarette smoking. Advanced Epidemiology, 2016, 1–7. 10.1155/2016/9587340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Looze M, ter Bogt T, Hublet A, Kuntsche E, Richter M, Zsiros E, … Vollebergh W (2013). Trends in educational differences in adolescent daily smoking across Europe, 2002–10. European Journal of Public Health, 23, 846–852. 10.1093/eurpub/ckt022 [DOI] [PubMed] [Google Scholar]
- Deutsch R, Gawronski B, & Strack F (2006). At the boundaries of automaticity: Negation as reflective operation. Journal of Personality and Social Psychology, 91, 385–405. 10.1037/0022-3514.91.3.385 [DOI] [PubMed] [Google Scholar]
- Dick DM, Smith G, Olausson P, Mitchell SH, Leeman RF, O’Malley SS, & Sher K (2010). Understanding the construct of impulsivity and its relationship to alcohol use disorders. Addiction Biology, 15, 217–226. 10.1111/j.1369-1600.2009.00190.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Du X, Qi X, Yang Y, Du G, Gao P, Zhang Y, … Zhang Q (2016). Altered structural correlates of impulsivity in adolescents with internet gaming disorder. Frontiers in Human Neuroscience, 10, 4 10.3389/fnhum.2016.00004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eberl C, Wiers RW, Pawelczack S, Rinck M, Becker ES, & Lindenmeyer J (2013). Approach bias modification in alcohol dependence: Do clinical effects replicate and for whom does it work best? Developmental Cognitive Neuroscience, 4, 38–51. 10.1016/j.dcn.2012.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elkins IJ, King SM, McGue M, & Iacono WG (2006). Personality traits and the development of nicotine, alcohol, and illicit drug disorders: Prospective links from adolescence to young adulthood. Journal of Abnormal Psychology, 115, 26–39. 10.1037/0021-843X.115.1.26 [DOI] [PubMed] [Google Scholar]
- Farber HJ, & Sachs DPL (2010). The Modified Fagerström Tolerance Questionnaire (mFTQ) for Adolescents (Scoring Information) Tobacco-Dependence Treatment ToolKit (3rd ed.). Glenview, IL: American College of Chest Physicians. [Google Scholar]
- Higgins ST, & Petry NM (1999). Contingency management. Incentives for sobriety. Alcohol Research & Health, 23, 122–127. [PMC free article] [PubMed] [Google Scholar]
- Hughes JR, Carpenter MJ, & Naud S (2010). Do point prevalence and prolonged abstinence measures produce similar results in smoking cessation studies? A systematic review. Nicotine & Tobacco Research, 12, 756–762. 10.1093/ntr/ntq078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kong G, Larsen H, Cavallo DA, Becker D, Cousijn J, Salemink E, … Krishnan-Sarin S (2015). Re-training automatic action tendencies to approach cigarettes among adolescent smokers: A pilot study. The American Journal of Drug and Alcohol Abuse, 41, 425–432. 10.3109/00952990.2015.1049492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krishnan-Sarin S, Cavallo DA, Cooney JL, Schepis TS, Kong G, Liss TB, … Carroll KM (2013). An exploratory randomized controlled trial of a novel high-school-based smoking cessation intervention for adolescent smokers using abstinence-contingent incentives and cognitive behavioral therapy. Drug and Alcohol Dependence, 132(1–2), 346–351. 10.1016/j.drugalcdep.2013.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krishnan-Sarin S, Duhig AM, McKee SA, McMahon TJ, Liss T, McFetridge A, & Cavallo DA (2006). Contingency management for smoking cessation in adolescent smokers. Experimental and Clinical Psychopharmacology, 14, 306–310. 10.1037/1064-1297.14.3.306 [DOI] [PubMed] [Google Scholar]
- Krishnan-Sarin S, Reynolds B, Duhig AM, Smith A, Liss T, McFetridge A, … Potenza MN (2007). Behavioral impulsivity predicts treatment outcome in a smoking cessation program for adolescent smokers. Drug and Alcohol Dependence, 88, 79–82. 10.1016/j.drugalcdep.2006.09.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larsen H, Kong G, Becker D, Cousijn J, Boendermaker W, Cavallo D, … Wiers R (2014). Implicit motivational processes underlying smoking in American and Dutch adolescents. Frontiers in Psychiatry, 5, 51 10.3389/fpsyt.2014.00051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis R, Harris M, Slone SA, Shelton BJ, & Reynolds B (2015). Delay discounting and self-reported impulsivity in adolescent smokers and nonsmokers living in rural Appalachia. The American Journal on Addictions/American Academy of Psychiatrists in Alcoholism and Addictions, 24, 492–494. 10.1111/ajad.12253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis-Esquerre JM, Colby SM, Tevyaw TOL, Eaton CA, Kahler CW, & Monti PM (2005). Validation of the timeline follow-back in the assessment of adolescent smoking. Drug and Alcohol Dependence, 79, 33–43. 10.1016/j.drugalcdep.2004.12.007 [DOI] [PubMed] [Google Scholar]
- Macy JT, Chassin L, Presson CC, & Sherman JW (2015). Changing implicit attitudes toward smoking: Results from a web-based approach-avoidance practice intervention. Journal of Behavioral Medicine, 38, 143–152. 10.1007/s10865-014-9585-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meda SA, Stevens MC, Potenza MN, Pittman B, Gueorguieva R, Andrews MM, … Pearlson GD (2009). Investigating the behavioral and self-report constructs of impulsivity domains using principal component analysis. Behavioural Pharmacology, 20(5–6), 390–399. 10.1097/FBP.0b013e32833113a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Memetovic J, Ratner PA, Gotay C, & Richardson CG (2016). Examining the relationship between personality and affect-related attributes and adolescents’ intentions to try smoking using the Substance Use Risk Profile Scale. Addictive Behaviors, 56, 36–40. 10.1016/j.addbeh.2016.01.002 [DOI] [PubMed] [Google Scholar]
- Mogg K, Field M, & Bradley BP (2005). Attentional and approach biases for smoking cues in smokers: An investigation of competing theoretical views of addiction. Psychopharmacology, 180, 333–341. 10.1007/s00213-005-2158-x [DOI] [PubMed] [Google Scholar]
- Morean ME, Kong G, Camenga DR, Cavallo DA, Carroll KM, Pittman B, & Krishnan-Sarin S (2015). Contingency management improves smoking cessation treatment outcomes among highly impulsive adolescent smokers relative to cognitive behavioral therapy. Addictive Behaviors, 42, 86–90. 10.1016/j.addbeh.2014.11.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myerson J, Green L, & Warusawitharana M (2001). Area under the curve as a measure of discounting. Journal of the Experimental Analysis of Behavior, 76, 235–243. 10.1901/jeab.2001.76-235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Loughlin JL, Dugas EN, O’Loughlin EK, Karp I, & Sylvestre MP (2014). Incidence and determinants of cigarette smoking initiation in young adults. Journal of Adolescent Health, 54, 26–32.e4. 10.1016/j.jadohealth.2013.07.009 [DOI] [PubMed] [Google Scholar]
- Patton JH, Stanford MS, & Barratt ES (1995). Factor structure of the Barratt impulsiveness scale. Journal of Clinical Psychology, 51, 768–774. 10.1002/1097-4679(199511)51:6[H11021]768 [DOI] [PubMed] [Google Scholar]
- Prokhorov AV, Pallonen UE, Fava JL, Ding L, & Niaura R (1996). Measuring nicotine dependence among high-risk adolescent smokers. Addictive Behaviors, 21, 117–127. 10.1016/0306-4603(96)00048-2 [DOI] [PubMed] [Google Scholar]
- Rabinovitz S, & Nagar M (2015). Possible end to an endless quest? Cognitive bias modification for excessive multiplayer online gamers. Cyberpsychology, Behavior, and Social Networking, 18, 581–587. 10.1089/cyber.2015.0173 [DOI] [PubMed] [Google Scholar]
- Reynolds B, Patak M, Shroff P, Penfold RB, Melanko S, & Duhig AM (2007). Laboratory and self-report assessments of impulsive behavior in adolescent daily smokers and nonsmokers. Experimental and Clinical Psychopharmacology, 15, 264–271. 10.1037/1064-1297.15.3.264 [DOI] [PubMed] [Google Scholar]
- Reynolds B, & Schiffbauer R (2004). Measuring state changes in human delay discounting: An experiential discounting task. Behavioural Processes, 67, 343–356. 10.1016/S0376-6357(04)00140-8 [DOI] [PubMed] [Google Scholar]
- Rinck M, & Becker ES (2007). Approach and avoidance in fear of spiders. Journal of Behavior Therapy and Experimental Psychiatry, 38, 105–120. 10.1016/j.jbtep.2006.10.001 [DOI] [PubMed] [Google Scholar]
- Robinson TE, & Berridge KC (2003). Addiction. Annual Review of Psychology, 54, 25–53. 10.1146/annurev.psych.54.101601.145237 [DOI] [PubMed] [Google Scholar]
- Schepis TS, McFetridge A, Chaplin TM, Sinha R, & Krishnan-Sarin S (2011). A pilot examination of stress-related changes in impulsivity and risk taking as related to smoking status and cessation outcome in adolescents. Nicotine & Tobacco Research, 13, 611–615. 10.1093/ntr/ntr022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh T, Arrazola RA, Corey CG, Husten CG, Neff LJ, Homa DM, & King BA (2016). Tobacco use among middle and high school students—United States, 2011–2015. Morbidity and Mortality Weekly Report, 65, 361–367. 10.15585/mmwr.mm6514a1 [DOI] [PubMed] [Google Scholar]
- Sobell LC, Toneatto T, Sobell MB, Leo GI, & Johnson L (1992). Alcohol abusers’ perceptions of the accuracy of their self-reports of drinking: Implications for treatment. Addictive Behaviors, 17, 507–511. 10.1016/0306-4603(92)90011-J [DOI] [PubMed] [Google Scholar]
- Stacy AW, & Wiers RW (2010). Implicit cognition and addiction: A tool for explaining paradoxical behavior. Annual Review of Clinical Psychology, 6, 551–575. 10.1146/annurev.clinpsy.121208.131444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stautz K, & Cooper A (2013). Impulsivity-related personality traits and adolescent alcohol use: A meta-analytic review. Clinical Psychology Review, 33, 574–592. 10.1016/j.cpr.2013.03.003 [DOI] [PubMed] [Google Scholar]
- Steinberg L, & Chein JM (2015). Multiple accounts of adolescent impulsivity. Proceedings of the National Academy of Sciences of the United States of America, 112, 8807–8808. 10.1073/pnas.1509732112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strack F, & Deutsch R (2004). Reflective and impulsive determinants of social behavior. Personality and Social Psychology Review, 8, 220–247. 10.1207/s15327957pspr0803_1 [DOI] [PubMed] [Google Scholar]
- Sussman S, & Sun P (2009). Youth tobacco use cessation: 2008 update. Tobacco Induced Diseases, 5, 3 10.1186/1617-9625-5-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Treur JL, Willemsen G, Bartels M, Geels LM, van Beek JHDA, Huppertz C, … Vink JM (2015). Smoking during adolescence as a risk factor for attention problems. Biological Psychiatry, 78, 656–663. 10.1016/j.biopsych.2014.06.019 [DOI] [PubMed] [Google Scholar]
- Watson P, Cousijn J, Hommel B, & Wiers RW (2013). Motivational Mechanisms Underlying the Approach Bias to Cigarettes. Journal of Experimental Psychopathology, 4, 250–262. 10.5127/jep.030512 [DOI] [Google Scholar]
- Wegmann L, Bühler A, Strunk M, Lang P, & Nowak D (2012). Smoking cessation with teenagers: The relationship between impulsivity, emotional problems, program retention and effectiveness. Addictive Behaviors, 37, 463–468. 10.1016/j.addbeh.2011.12.008 [DOI] [PubMed] [Google Scholar]
- White HR, Marmorstein NR, Crews FT, Bates ME, Mun E-Y, & Loeber R (2011). Associations between heavy drinking and changes in impulsive behavior among adolescent boys. Alcoholism: Clinical and Experimental Research, 35, 295–303. 10.1111/j.1530-0277.2010.01345.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- White JL, Moffitt TE, Caspi A, Bartusch DJ, Needles DJ, & Stouthamer-Loeber M (1994). Measuring impulsivity and examining its relationship to delinquency. Journal of Abnormal Psychology, 103, 192–205. 10.1037/0021-843X.103.2.192 [DOI] [PubMed] [Google Scholar]
- Wiers CE, Kühn S, Javadi AH, Korucuoglu O, Wiers RW, Walter H, … Bermpohl F (2013). Automatic approach bias towards smoking cues is present in smokers but not in ex-smokers. Psychopharmacology, 229, 187–197. 10.1007/s00213-013-3098-5 [DOI] [PubMed] [Google Scholar]
- Wiers CE, Stelzel C, Gladwin TE, Park SQ, Pawelczack S, Gawron CK, … Bermpohl F (2014). Effects of cognitive bias modification training on neural alcohol cue reactivity in alcohol dependence. The American Journal of Psychiatry, 172, 335–343. 10.1176/appi.ajp.2014.13111495 [DOI] [PubMed] [Google Scholar]
- Wiers RW, Bartholow BD, van den Wildenberg E, Thush C, Engels RCME, Sher KJ, … Stacy AW (2007). Automatic and controlled processes and the development of addictive behaviors in adolescents: A review and a model. Pharmacology, Biochemistry, and Behavior, 86, 263–283. 10.1016/j.pbb.2006.09.021 [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2015). Tobacco-Fact sheets. Retrieved December 6, 2015, from http://www.who.int/mediacentre/factsheets/fs339/en/