Abstract
Invasive fungal rhinosinusitis is a rare infection that occurs primarily in immunocompromised patients. The fungal pathogen Alternaria alternata is rarely associated with rhinosinusitis. We report a case of A. alternata rhinosinusitis in an immunocompetent patient.
Keywords: Cerebral parenchyma, fungus, mycelian filaments, sinus
Introduction
Alternaria is an ubiquitous fungus that is considered to be a nonpathogenic contaminant of the clinical specimen unless isolated by repeated culture and correlated with clinical findings. However, it is a rare cause of human infection, especially in immunocompromised patients but even more rarely in healthy hosts [1].
We report a case of Alternaria alternata in a healthy patient. Cutaneous infections are the most frequent diseases caused by Alternaria. However, infections in other organs, such as facial osteomyelitis [2], sinusitis [3] and keratomycosis [4], have also been reported. Initially patients may report nonspecific symptoms similar to chronic rhinosinusitis. Complications related to the orbital extension include preseptal cellulitis and orbital cellulitis. The lesion grows contiguously, possibly invading the central nervous system [5].
Case report
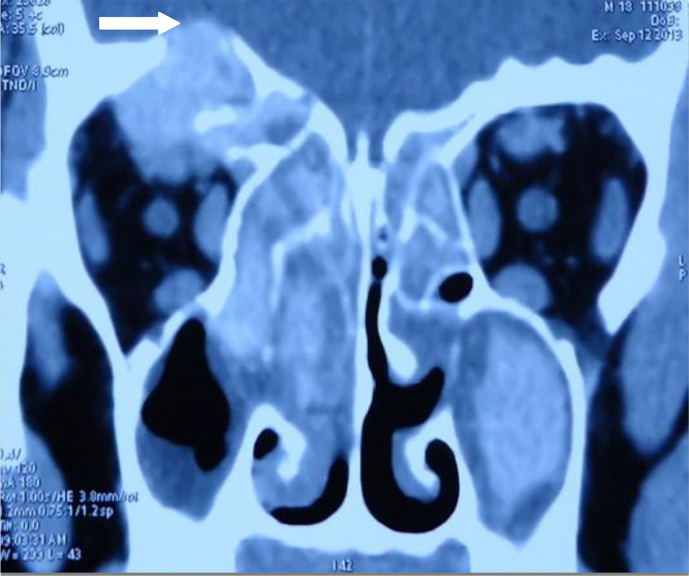
A 19-year-old man with allergic rhinitis, with no history of corticoid therapy or nasal drug use, sought care for haemicranial headache with purulent rhinorrhea, anosmia, right exophthalmia, and vision impairment without fever, which had evolved for 9 months. His neurologic examination revealed nothing abnormal. Ocular motility was normal. Examination of the fundus found a papillary edema. Computed tomographic scan revealed obliteration of the maxillary and frontal sinuses with destruction of the orbital wall and intraorbital extension (Fig. 1). Histologic examination of sinus biopsy material showed an inflammatory process of the nasal mucosa chorion with periodic acid–Schiff mycelian filaments in the mucus and fibrin leucocyte material.
Fig. 1.
Coronal-view preoperative computed tomographic scan revealing intracranial and intraocular extension.
Culture of the biopsy sample identified A. alternata. Antifungal sensitivity could not be assessed. The bronchial tree at fibroscopy was normal; the mycelian filaments were not found in alveolar lavage fluid. The patient underwent debridement, septoplasty and sphenoidotomy and was treated with amphotericin B 37 mg/kg per day for 15 days, followed by oral itraconazole 200 mg per day for 2 months. HIV serology was negative. Immunoglobulin assay revealed no deficit. The patient underwent septoplasty, sphenoidectomy, polypectomy and meatotomy. There were no complications at 1 year.
Conclusion
Our patient presented rhinosinusitis due to Alternaria involving the cerebral parenchyma and had no apparent predisposing factor outside of a history of allergic rhinosinusitis, which is considered to be a risk factor for fungal sinusitis [6].
The confirmation of diagnosis is based on histopathologic examination of a sample with periodic acid–Schiff staining. The histologic appearance of Alternaria is characterized by a dense accumulation of hyphae, infiltration of surrounding tissue, and occasional branching and chains of conidia. The treatment of Alternaria and appropriate antifungal therapy doses are not standardized in the literature. The optimal treatment should consist of broad surgical debridement of involved tissues with prolonged systemic antifungal medication. Alternaria is sensitive to amphotericin B and miconazole [7]. Therefore, itraconazole was cited in the literature as the treatment of choice in Alternaria infections based on its minimum inhibitory concentration values.
Alternaria is a cause of chronic fungal sinusitis. Histopathologic examination and microbiologic identification can help in diagnosis.
Conflict of interest
None declared.
References
- 1.Loveless M.O., Winn R.E., Campbell M., Jones S.R. Mixed invasive infection with Alternaria species and Curvularia species. Am J Clin Pathol. 1981;76:491–493. doi: 10.1093/ajcp/76.4.491. [DOI] [PubMed] [Google Scholar]
- 2.Chhabra V., Rastogi S., Barua M., Kumar S. Alternaria alternata infection associated osteomyelitis of maxilla: a rare disease entity. Indian J Dent Res. 2013;24:639–641. doi: 10.4103/0970-9290.123420. [DOI] [PubMed] [Google Scholar]
- 3.Shugar M.A., Montgomery W.W., Hyslop N.E., Jr. Alternaria sinusitis. Ann Otol Rhinol Laryngol. 1981;90:251–254. doi: 10.1177/000348948109000311. [DOI] [PubMed] [Google Scholar]
- 4.Zahra L.V., Mallia D., Hardie J.G., Bezzina A., Fenech T. Keratomycosis due to Alternaria alternata in a diabetic patient [case report] Mycoses. 2002;45:512–514. doi: 10.1046/j.1439-0507.2002.00806.x. [DOI] [PubMed] [Google Scholar]
- 5.Ingley A.P., Parikh S.L., DelGaudio J.M. Orbital and cranial nerve presentations and sequelae are hallmarks of invasive fungal sinusitis caused by Mucor in contrast to Aspergillus. Am J Rhinol. 2008;22:155–158. doi: 10.2500/ajr.2008.22.3141. [DOI] [PubMed] [Google Scholar]
- 6.Klimek L., Bardenhewer C., Spielhaupter M., Harai C., Becker K., Pfaar O. [Local allergic rhinitis to Alternaria alternata: evidence for local IgE production exclusively in the nasal mucosa] HNO. 2015;63:364–372. doi: 10.1007/s00106-015-0005-x. [DOI] [PubMed] [Google Scholar]
- 7.Valera F.C.P., de Lago T., Tamashiro E., Yassuda C.C., Silveira F., Anselmo-Lima W.T. Prognosis of acute invasive fungal rhinosinusitis related to underlying disease. Int J Infect Dis. 2011;15:e841–e844. doi: 10.1016/j.ijid.2011.08.005. [DOI] [PubMed] [Google Scholar]