Abstract
Background
Coronary CT angiography (CCTA) is utilized in the emergency department (ED) to rule out acute coronary syndrome in low-intermediate risk patients.
Objectives
We evaluated the potential of CCTA to tailor aspirin (ASA) and statin therapy in acute chest pain patients.
Methods
We included all patients in the ROMICAT I trial who underwent CCTA before admission. Results of CCTA were blinded to caretakers. We documented aspirin and statin therapy at admission and discharge and determined change in medications during hospitalization, agreement of discharge medications with contemporaneous guidelines, and agreement with the presence and severity of CAD as determined by CCTA.
Results
We included 368 patients (53±12 years, 61% male). Baseline medical therapy at presentation included 27% on ASA and 24% on statin. The majority of subjects who qualified for secondary prevention were on aspirin and statin therapy at discharge (95% and 80%, respectively), whereas among those qualifying for primary prevention therapy, only 59% of subjects were on aspirin and 33% were on statin at discharge. Excluding secondary prevention subjects, among those with CCTA-detected CAD, only 50% (66/131) were on ASA at discharge and only 40% (53/131) were on statin. Conversely, in those without CCTA-detected CAD, 35% (54/156) were on ASA and 13% (20/151) were on statin at discharge.
Conclusion
There are significant discrepancies between discharge prescription of statin and ASA with the presence and extent of CAD. CCTA presents an efficient opportunity to tailor medical therapy to CAD in patients undergoing CCTA as part of their acute chest pain evaluation.
Keywords: Coronary CT angiography, coronary artery disease, prevention, guidelines, aspirin, statin
Introduction
Coronary CT angiography (CCTA) is an established diagnostic tool for the evaluation of acute chest pain patients. CCTA has excellent negative predictive value for excluding acute coronary syndrome (ACS), (1–4) and is a highly accurate tool for the detection of coronary artery disease (CAD). (5, 6)
A number of studies have demonstrated the excellent prognostic value of CCTA for MACE, supporting a proportional increase of risk for MACE with the presence and extent of non-obstructive and obstructive CAD independent of traditional risk factors. (7–17) Hence, CCTA information may provide an opportunity to effectively align established preventive medical therapies such as aspirin (ASA) and statin with the presence and extent of CAD. Unlike other risk stratification methods such as risk score calculators and functional testing which may indirectly suggest the presence of CAD, CCTA allows for direct anatomic visualization of atherosclerotic plaque in the coronary arteries. Therefore, CCTA findings can allow for physicians to consider preventive medical therapies on the basis of actual presence of CAD in addition to the current guidelines that are primarily based upon risk factor assessment and clinical events.
In this secondary analysis of the Rule Out Myocardial Infarction using Computer Assisted Tomography (ROMICAT I) study, we sought to (i) identify the changes in ASA and statin therapy from admission to discharge with a standard of care evaluation of the acute chest pain patient, (ii) assess agreement between discharge medical therapy and guideline-dictated medical therapy, and (iii) examine how CCTA identification of CAD in this cohort could change the paradigm by which patients are selected for preventive medical therapies.
Methods
Study Population
This is a secondary analysis of the 368 enrolled patients from the ROMICAT I trial. These patients were enrolled from May 2005 to May 2007 at the Massachusetts General Hospital and had an initial chief complaint of acute chest pain lasting > 5 minutes during the 24-hour period before the index hospitalization, as well as a normal initial troponin level and electrocardiographic findings. Details regarding the inclusion and exclusion criteria were previously reported. (1) Briefly, during the index hospitalization, all subjects underwent a standard contrast-enhanced coronary CT study before admission to the hospital. Both caregivers and patients remained blinded to the results of the coronary CT study. Patients were managed according to standard of care, which included stress testing prior to discharge in the majority of patients. The institutional review board approved the study protocol, and all patients provided written informed consent.
Medication Data
Medication information was collected for each patient by systematically reviewing electronic medical records during the index Emergency Department (ED) visit and hospitalization, with a focus on the ED admission and discharge notes, and inpatient admission and discharge notes if the patient underwent admission. Admission and discharge ASA and statin prescription and contraindications to these medications were obtained from these records. We defined contraindication to ASA therapy as a severe ASA allergy (anaphylaxis, angioedema, etc), or documented intolerance due to a history of major GI bleed (requiring transfusion) or intracranial bleed. Contraindication to statin therapy was defined as a history of statin-induced myopathy, rhabdomyolysis, or other documented statin intolerance. Medication data collection was performed blinded to individual patient CCTA results and was performed by an experienced cardiologist. Complete admission and discharge medication status for ASA and statin was available in 358/368 =97% of patients.
Cardiovascular Risk Factors
Risk factors were assessed at the time of subject enrollment, based on self-report as well as review of medical records for the index hospitalization. Hypertension was defined as a systolic blood pressure of at least 140 mm Hg or diastolic blood pressure of at least 90 mm Hg or current anti-hypertensive treatment. Diabetes mellitus was defined as a fasting plasma glucose >=126 or treatment with a hypoglycemic agent. Peripheral vascular disease was defined as having a history transient ischemic attack, cerebrovascular event, or peripheral arterial disease. Family history of CAD was defined as having a first-degree female (<65 years of age) or male (<55 years of age) relative with a documented history of myocardial infarction or sudden cardiac death. Subjects were classified as smokers if they had smoked at least 1 cigarette per day in the year before the study. Lipid profiles were collected as part of the study protocol, and complete lipid data was available in 336/368 (91%) of patients. The 10-year Framingham Risk Score was calculated for each patient, and patients were stratified into the following three groups: <10%, 10–20%, and >20% for 10-year risk of a cardiovascular event.
Guideline-Dictated Medical Therapy
Guideline-dictated medical therapy for ASA and statin was defined as compliance with the respective, authoritative, and contemporaneous guidelines for primary prevention or secondary prevention. Secondary prevention guidelines pertained to those patients who were diagnosed with ACS during the index hospitalization (defined as unstable angina or myocardial infarction), or had a history of a CAD equivalent including peripheral arterial disease, transient ischemic attack, or cerebrovascular accident. We utilized the 2006 American Heart Association/American College of Cardiology joint secondary prevention guidelines, which dictated the use of ASA therapy for all these individuals, and statin therapy for those with LDL> 70 mg/dl. (18–21)
If a patient did not meet secondary prevention guideline criteria, the primary prevention guidelines applied. Specifically, for ASA therapy, this meant adherence to the 2002 American Heart Association/American College of Cardiology primary prevention guidelines which recommended ASA for individuals with a 10-year FRS > 10%. (22) The 2004 Updated Third Report of the Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (ATP III) dictated the use of primary prevention statin therapy. (23, 24) We based guideline-dictated prescription of ASA therapy in diabetic patients on the 2002 US Preventive Services Task Force guidelines, which recommended ASA for patients with a diagnosis of diabetes mellitus and age over 40 years and at least one additional risk factor. (25–27)
To assess agreement of prescribed medical therapy with guideline-dictated medical therapy, we utilized discharge medication data.
CCTA was performed using a 64-slice CT scanner (Sensation 64, Siemens Medical Solutions, Forchheim, Germany) as previously described. (1) For coronary atherosclerotic plaque and stenosis assessment, the presence of coronary atherosclerotic plaque per segment, either calcified or non-calcified, was determined as described previously, using a modified 17-segment model of the coronary artery tree. Patients were stratified based on the presence and severity of CAD into the following strata: no CAD, non-obstructive CAD, and obstructive CAD. Obstructive CAD was defined either as coronary artery stenosis with >50% luminal diameter obstruction or if coronary stenosis could not be confidently excluded. Non-obstructive CAD was defined as the presence of a coronary artery stenosis <50%.
Statistical Analysis
Continuous data are presented as mean ± SD and categorical variables are expressed as frequencies and percentages. To test for differences in frequency of ASA and statin prescription between guideline recommended and not guideline recommended medical therapy, we used Fisher’s exact test. A two-sided P value of less than 0.05 was considered statistically significant. All analyses were performed using SAS (Version 9.2, SAS Institute Inc, Cary, NC).
Results
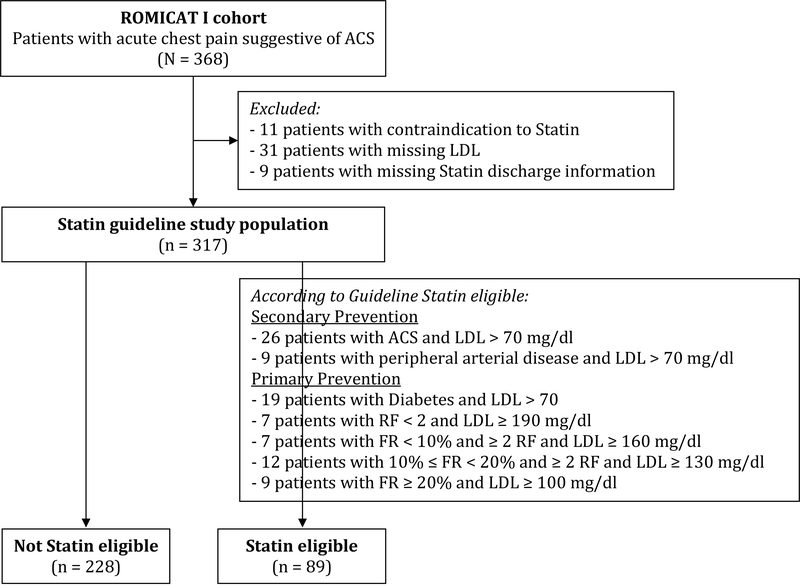
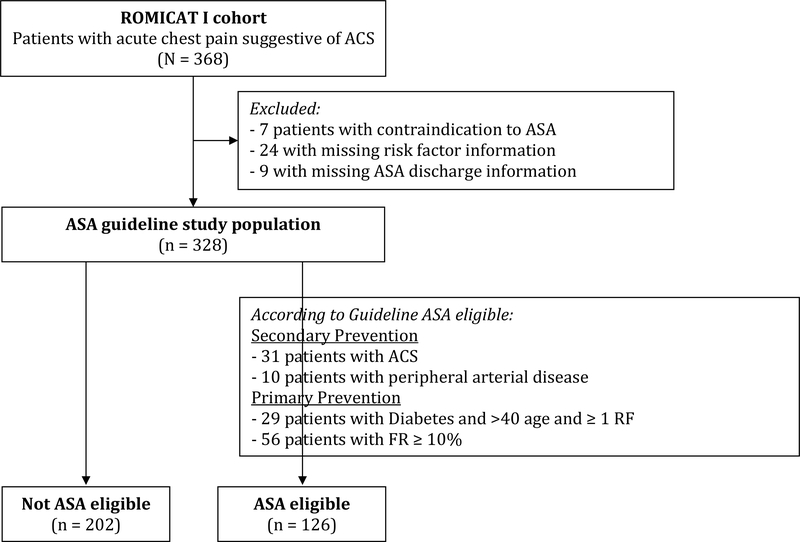
Determination of guideline-based eligibility for statin or ASA is depicted in Figure 1a and Figure 1b, respectively. The baseline characteristics and risk profile of patients are as shown below in Table 1. Of note, in the overall cohort, 11% of patients had diabetes, 4% had a history of vascular disease, and 8% of patients developed an acute coronary syndrome during the index hospitalization. The majority of patients however had a 10-year Framingham risk of less than 10%. Patients who developed ACS or had a history of vascular disease were considered candidates for secondary prevention (n=41 in ASA cohort and n=35 in Statin cohort), whereas those without were considered primary prevention with guideline (ASA: n=85; Statin: n=54) or without guideline (ASA: n= 202; Statin: n=228) indication for medical therapy. Of note, there were 3 patients with ACS and one patient with established PVD who did not qualify for secondary prevention statin therapy because they had an LDL<70 mg/dl. As expected, patients who had a guideline indication for therapy (either secondary or primary prevention) had more risk factors than those without a guideline indication.
Figure 1a:
Determination of Statin Guideline Eligibility
Figure 1b:
Determination of Aspirin Guideline Eligibility
Table 1:
Baseline Patient Characteristics
| Aspirin Therapy |
Statin Therapy |
||||||
|---|---|---|---|---|---|---|---|
| Total | Secondary Prevention | Primary Prevention w/o Guideline Indication | Primary Prevention with Guideline Indication | Secondary Prevention | Primary Prevention w/o Guideline Indication | Primary Prevention with Guideline Indication | |
| Characteristic | N= 368 | N = 41 | N = 202 | N = 85 | N = 35 | N = 228 | N = 54 |
| Mean Age (years) | 52.8 ± 11.8 | 60.1 ± 12.7 | 48.6 ± 9.8 | 58.9 ± 11.6 | 60.3 ± 10.9 | 51.2 ± 11.4 | 55.0 ± 12.3 |
| Male sex – n (%) | 226 (61) | 26 (63) | 111 (55) | 69 (81) | 22 (63) | 138 (61) | 38 (70) |
| Hypertension – n (%) | 145 (39) | 25 (61) | 57 (28) | 50 (59) | 21 (61) | 78 (34) | 25 (46) |
| Smoking – n (%) | 180 (49) | 23 (56) | 83 (41) | 58 (68) | 19 (54) | 108 (47) | 30 (56) |
| Diabetes Mellitus – n (%) | 40 (11) | 6 (15) | 1 (1) | 30 (35) | 6 (17) | 9 (4) | 19 (35) |
| Vascular Disease (TIA/CVA/PAD) – n (%) | 13 (4) | 11 (27) | 0 (0) | 0 (0) | 10 (29) | 1 (0.5) | 0 (0) |
| Acute Coronary Syndrome - n (%) | 31 (8) | 31 (76) | 0 (0) | 0 (0) | 26 (74) | 3 (1) | 0 (0) |
| FRS category, n (%) | |||||||
| <10% | 251 (68) | 22 (54) | 202 (100) | 16 (19) | 20 (57) | 190 (83) | 24 (44) |
| 10% – 20% | 62 (17) | 11 (27) | 0 (0) | 49 (58) | 9 (26) | 31 (14) | 17 (31) |
| >20% | 26 (7) | 7 (17) | 0 (0) | 17 (20) | 6 (17) | 5 (2) | 13 (24) |
| Dyslipidemia – n (%) | 135 (37) | 24 (59) | 61 (30) | 40 (47) | 21 (60) | 76 (33) | 21 (39) |
| Total Cholesterol (mg/dl) | 195 ± 42 | 189 ± 42 | 196 ± 40 | 195 ± 48 | 195 ± 41 | 186 ± 37 | 231 ± 47 |
| LDL Cholesterol (mg/dl) | 114 ± 37 | 111 ± 38 | 116 ± 40 | 112 ± 37 | 117 ± 35 | 106 ± 32 | 146 ± 42 |
| HDL Cholesterol (mg/dl) | 51 ± 15 | 45 ± 12 | 54 ± 16 | 46 ± 12 | 46 ± 12 | 53 ± 16 | 48 ± 12 |
Plus-minus values are means ± SD.
TIA: Transient Ischemic Attack, CVA: Cerebrovascular Accident, PAD: Peripheral Arterial Disease, FRS: 10-year Framingham Risk Score
Admission and discharge ASA and statin therapy stratified by guideline indication is shown in Table 2. As shown, among secondary prevention patients, the vast majority were discharged on aspirin and statin (95% and 80%, respectively). Primary prevention patients with guideline indication were more likely than those without guideline indication to be discharged on aspirin (59% versus 35%; p<0.001) but not on statins (33% versus 24%; p=0.170).
Table 2:
Admission and Discharge Medical Therapy Stratified by Applicable Guideline
| Total | Secondary Prevention | Primary Prevention w/o Guideline Indication | Primary Prevention with Guideline Indication | |
|---|---|---|---|---|
| Aspirin Therapy | N = 368 | N = 41 | N = 202 | N = 85 |
| Admission Medication – n (%) | 95/353 (27) | 21/41 (51) | 39/202 (19) | 31/84 (37) |
| Discharge Medication – n (%) | 166/352 (47) | 39/41 (95) | 70/202 (35) | 50/85 (59) |
| Change in Medication – n (%) | 74/351 (21) | 18/41 (44) | 33/202 (16) | 18/84 (21) |
| Upgrade in Therapy | 73/351 (21) | 18/41 (44) | 32/202 (16) | 18/84 (21) |
| Downgrade in Therapy | 1/351 (0) | 0/41 (0) | 1/202 (0.5) | 0/84 (0) |
| Contraindication to Aspirin – n (%) | 7/368 (2) | --- | --- | --- |
| Statin Therapy | N = 368 | N = 35 | N = 228 | N = 54 |
| Admission Medication– n (%) | 85/349 (24) | 17/35 (49) | 49/227 (22) | 14/54 (26) |
| Discharge Medication– n (%) | 108/348 (31) | 28/35 (80) | 55/228 (24) | 18/54 (33) |
| Change in Medication – n (%) | 27/347 (8) | 13/35 (37) | 6/227 (3) | 6/54 (11) |
| Upgrade in Therapy | 25/347 (7) | 12/35 (34) | 6/227 (3) | 5/54 (9) |
| Downgrade in Therapy | 2/347 (1) | 1/35 (3) | 0/227 (0) | 1/54 (2) |
| Contraindication to Statin – n (%) | 11/368 (3) | --- | --- | --- |
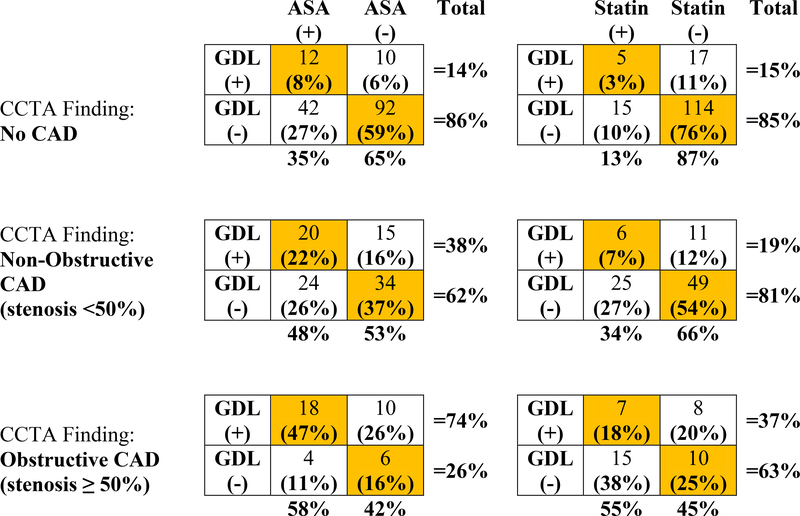
CCTA results, which were blinded to providers, were stratified into categories of no CAD, non-obstructive CAD, and obstructive CAD. Figure 2 summarizes the overall agreement between actual discharge medical therapy and guideline-dictated medical therapy among those patients returning to primary prevention after a negative chest pain workup, stratified by the presence and severity of coronary artery disease on coronary CTA: (i) For patients with no CAD detected by CCTA, the guidelines would dictate medical therapy in 14% of patients for ASA, and 15% for statin. Of note, 35% and 13% of these patients actually received ASA and statins as discharge medical therapy, respectively. (ii) For patients with non-obstructive CAD detected by CCTA, there was relatively modest agreement between actual discharge medical therapy and guideline-dictated medical therapy (59% agreement for ASA and 61% agreement for statin therapy). In addition, the guidelines (based on risk factors and results of standard of care evaluation) would have advised that only 38% of these patients be on ASA, and only 19% on statin therapy. (iii) For patients with obstructive CAD detected by CCTA, 74% of patients should have been discharged on ASA and only 37% on statin according to the guidelines. However, 58% of patients in this strata were actually discharged on ASA, and 55% were actually discharged on statin therapy.
Figure 2: Discharge Medical Therapy and Guideline-Dictated Therapy By CCTA for Primary Prevention Group (Excluding Secondary Prevention Patients).
Detected CAD Strata: Patients are stratified according to CAD strata (no CAD, non-obstructive CAD, and obstructive CAD) based on CCTA results, which were blinded to caretakers. Guideline recommended therapy is as described in the Methods section.
Key: Gdl (+) Recommended by Guidelines;
Gdl (−) No Recommendation by Guidelines;
ASA (+) or Statin (+) Patient actually discharged on ASA or statin, respectively; ASA (−) or Statin (−) Patient NOT discharged on ASA or statin, respectively.
Orange shaded cells represent agreement between guideline-dictated medical therapy and actual discharge medical therapy.
In Table 3 we depict patient characteristics for those subjects who were found to have CCTA-detected CAD (either obstructive or non-obstructive) stratified by whether aspirin or statin are recommended per respective guidelines. In general, the subjects that are not recommended for statin therapy are “lower risk” by traditional risk factor algorithms, and we note that all of the subjects for whom aspirin is not recommended and the majority of subjects for whom statin is not recommended have an FRS<10%.
Table 3:
Patient Characteristics for all Patients with CCTA-detected CAD According to Guideline Recommendation
| Characteristic | Aspirin not recommended | Aspirin recommended | Statins not recommended | Statins recommended |
|---|---|---|---|---|
| N=68 | N=99 | N = 99 | N = 63 | |
| Mean Age (years) | 53.5 ± 9.0 | 60.9 ± 12.1 | 57.7 ± 10.8 | 59.0 ± 12.4 |
| Male sex – n (%) | 36 (53) | 78 (79) | 64 (65) | 45 (71) |
| Hypertension – n (%) | 30 (44) | 60 (63) | 51 (52) | 36 (57) |
| Smoking – n (%) | 32 (47) | 66 (67) | 58 (59) | 37 (59) |
| Diabetes Mellitus – n (%) | 1 (1) | 25 (25) | 7 (7) | 18 (29) |
| Vascular Disease (TIA/CVA/PAD) – n (%) | 0 (0) | 6 (6) | 0 (0) | 6 (10) |
| Acute Coronary Syndrome - n (%) | 0 (0) | 31 (31) | 3 (3) | 26 (41) |
| FRS category, n (%) | ||||
| <10% | 68 (100) | 28 (28) | 67 (68) | 27 (43) |
| 10% –20 % | 0 (0) | 49 (49) | 26 (26) | 20 (32) |
| >20% | 0 (0) | 21 (21) | 5 (5) | 16 (25) |
| Dyslipidemia – n (%) | 36 (53) | 51 (52) | 53 (54) | 31 (49) |
| Total Cholesterol (mg/dl) | 196 ± 42 | 190 ± 47 | 182 ± 42 | 208 ± 46 |
| LDL Cholesterol (mg/dl) | 116 ± 36 | 109 ± 36 | 103 ± 32 | 125 ± 38 |
| HDL Cholesterol (mg/dl) | 53 ± 16 | 45 ± 12 | 50 ± 15 | 47 ± 12 |
Plus-minus values are means ± SD.
TIA: Transient Ischemic Attack, CVA: Cerebrovascular Accident, PAD: Peripheral Arterial Disease, FRS: 10-year Framingham Risk Score
Discussion
The observational, blinded cohort study design of the ROMICAT I trial allows for this secondary analysis to provide several unique insights into the medical management of acute chest patients, and the potential role for CCTA beyond current preventive therapy guidelines.
Specifically, our study characterizes some key discrepancies, including (1) the gap between actual discharge medical therapy and guideline-dictated medical therapy, and (2) the gap between discharge medical therapy based on standard care evaluation of acute chest pain in the ED and actual CCTA-detected presence and extent of coronary artery disease. The former discrepancy may be resolved by understanding that the majority of patients were evaluated in the emergency department and did not require hospital admission and were not evaluated by an internist or cardiologist who may have greater familiarity with the primary and secondary prevention guidelines. Moreover, the ED is typically considered a place for triage of acute chest pain and identification of the highest risk patients, and not necessarily initiation of longer-term preventive medical therapies such as ASA and statin. However, it is important to note that this cohort had an 8% event rate for acute coronary syndrome, with most events occurring within a few days of presentation. Therefore, deferring decision-making to the outpatient clinician in this relatively high-risk population may not be ideal, particularly if the patient is not able to follow-up with an internist or cardiologist in a reasonable timeframe.
The latter discrepancy can be evaluated given the blinded nature of CCTA examination in the ROMICAT I trial. The gap between discharge medical therapy and CCTA findings offers a potentially valuable role for a CCTA-based diagnostic strategy beyond current preventive medical therapy guidelines. Current primary prevention guidelines for initiation of ASA and statin therapy are based on algorithms incorporating cardiac risk factors and secondary prevention guidelines rely on the presence of established coronary artery disease, peripheral vascular disease or development of cardiovascular events. This conventional framework of primary prevention guidelines being applied to asymptomatic patients, and secondary prevention guidelines being applied to those who have ACS or peripheral vascular disease has its limitations. Specifically, the “symptomatic” patients in our cohort who are “ruled out” for ACS do not quite fit into either of these conventional frameworks (a limitation of current guidelines), though we would argue that they deserve at least primary prevention consideration.
Given the increased risk of future cardiovascular events with the severity and extent of CAD on CCTA, patients with any degree of coronary artery disease (which represents about half of patients presenting with acute chest pain in the ED) should arguably be given a statin given its excellent safety profile. It has been suggested that aspirin be given for those with CAC score >100 based on favorable risk/benefit analysis in a large primary prevention population, regardless of traditional risk factors. (28) Given that our patient cohort is not truly asymptomatic, it is conceivable that the threshold of coronary atherosclerosis for which to recommend aspirin based on a benefit and harm analysis may be lower. However, further outcome data would be necessary to evaluate this.
Our data reveals that over half of patients with non-obstructive CAD detected by CCTA were not prescribed statin therapy at the time of discharge, suggesting a limitation of a standard-of-care evaluation to identify these patients who may potentially benefit from medical therapy. Conversely, the absence of CAD on coronary CTA denotes an excellent prognosis in acute chest pain patients, and therefore arguably these patients may not receive the same benefit to risk ratio of medical treatment as those with CCTA-detected CAD. (8)
A few studies have examined the effect of CCTA on prescription of preventive medical therapies, building upon work evaluating the impact of coronary calcium on intensification of medical therapy. However, these were not in the ED setting of acute chest pain. For example, Taylor et al showed that the presence of coronary calcification is associated with increased initiation and persistence of statin and ASA therapy in a community cohort of asymptomatic patients.(29) Treatment of patients with elevated coronary artery calcium was even associated with a trend towards reduction in outcomes in the St. Francis Heart Study.(30) In contrast, McEvoy et al found that although CCTA screening in asymptomatic patients resulted in increased outpatient aspirin and statin prescription, they found that screening CCTA was not justifiable based on equivalent event rates after 18-month follow-up compared to a matched control group that did not undergo CCTA. (31)
In symptomatic patients, a study of patients by LaBounty and colleagues showed increased use of medical therapies including ASA, statins, and anti-hypertensive medication after CCTA, however this was a relatively small, single-center, retrospective study of a heterogeneous patient population.(32) More recently, two recent studies showed similar findings in a larger cohort of consecutive patients undergoing CCTA.(33, 34) However, all of these studies in symptomatic patients lacked a clear control group (e.g. functional testing) as an alternative to CCTA evaluation, and require substantial adjustment for traditional risk factors. In contrast, the SPARC registry did have a functional testing arm and showed that after adjustment of risk factors, patients undergoing coronary CCTA were more likely to have medication adjustments, but also were more likely to have subsequent invasive testing. (35)
It should be emphasized that in contrast to these studies, our analysis does not actually evaluate prescription behavior in response to CCTA, but rather assesses the limitations of current standard care strategies in efficiently aligning preventive medical therapies with those who would benefit the most. We outline some of the potential limitations of current guidelines for ASA and statin prescription, which would “miss” a substantial number of patients who have CCTA-detected CAD. Therefore, our insights should be taken in concert with the above studies, and provide impetus for future research, ideally within the construct of a randomized controlled trial, examining how CCTA truly impacts prescription behavior of preventive medical therapy and downstream outcomes.
Our analysis does have some limitations. We did not look at changes in medical therapy beyond the time of discharge to evaluate for outpatient adjustment of medications, as many of these patients did not follow-up at our institution. However, our aim was to evaluate how many patients are treated optimally at the time of ED discharge to establish the gap between CCTA findings and standard of care of management at this time point. Also, although we have found a potentially valuable role of CCTA to address some of the limitations of current standard-of-care guided medical optimization, one cannot assume that CCTA will indeed optimize treatment patterns, as other variables such as the treating physician response to CCTA findings and patient adherence must be taken into account. For example, in the NCDR cardiac catheterization registry, a relatively small percentage of patients with moderate non-obstructive coronary artery disease actually received ASA (76%) and statin (65%) therapy at hospital discharge. (36) Lastly, we limited our analysis of preventive medical therapy to ASA and statin, as evaluation of other medical therapies such as beta-blocker and ace inhibitor are more complex given varied indications for these medications beyond prevention and treatment of coronary artery disease.
Conclusions
There are significant discrepancies between actual discharge prescription of statin and ASA with the presence and extent of CAD. CCTA presents an efficient opportunity to tailor medical therapy to CAD in patients undergoing CCTA as part of their ED evaluation for acute chest pain.
Highlights.
Many patients who are “ruled out” for acute chest pain have CCTA-detected CAD.
Discrepancies exist between discharge prescription of statin and ASA with the presence and extent of CAD.
CCTA presents an efficient opportunity to tailor medical therapy to CAD in patients undergoing CCTA as part of their acute chest pain evaluation.
Acknowledgments
Financial Disclosures:
This work was supported by grants from the National Heart, Lung, and Blood Institute (R01 HL080053 and 5K24HL113128). Dr. Pursnani received funding from NIHT32 HL076136.
Abbreviations
- ACS
Acute Coronary Syndrome
- ASA
Aspirin
- CAD
Coronary Artery Disease
- CCTA
Coronary Computed Tomography Angiography
- ED
Emergency Department
- FRS
Framingham Risk Score
- MACE
Major Adverse Cardiovascular Events
- ROMICAT
Rule Out Myocardial Infarction with Computer Assisted Tomography
Footnotes
The authors disclose no relevant relationship with industry.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Hoffmann U, Bamberg F, Chae CU, Nichols JH, Rogers IS, Seneviratne SK, Truong QA, Cury RC, Abbara S, Shapiro MD, Moloo J, Butler J, Ferencik M, Lee H, Jang IK, Parry BA, Brown DF, Udelson JE, Achenbach S, Brady TJ, Nagurney JT. Coronary computed tomography angiography for early triage of patients with acute chest pain: the ROMICAT (Rule Out Myocardial Infarction using Computer Assisted Tomography) trial. J Am Coll Cardiol 2009. May 5;53(18):1642–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hoffmann U, Truong QA, Schoenfeld DA, Chou ET, Woodard PK, Nagurney JT, Pope JH, Hauser TH, White CS, Weiner SG, Kalanjian S, Mullins ME, Mikati I, Peacock WF, Zakroysky P, Hayden D, Goehler A, Lee H, Gazelle GS, Wiviott SD, Fleg JL, Udelson JE. Coronary CT angiography versus standard evaluation in acute chest pain. N Engl J Med 2012. July 26;367(4):299–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goldstein JA, Chinnaiyan KM, Abidov A, Achenbach S, Berman DS, Hayes SW, Hoffmann U, Lesser JR, Mikati IA, O’Neil BJ, Shaw LJ, Shen MY, Valeti US, Raff GL. The CT-STAT (Coronary Computed Tomographic Angiography for Systematic Triage of Acute Chest Pain Patients to Treatment) trial. J Am Coll Cardiol 2011. September 27;58(14):1414–22. [DOI] [PubMed] [Google Scholar]
- 4.Bamberg F, Marcus RP, Schlett CL, Schoepf UJ, Johnson TR, Nance JW Jr., Hoffmann U, Reiser MF, Nikolaou K. Imaging evaluation of acute chest pain: systematic review of evidence base and cost-effectiveness. J Thorac Imaging 2012. September;27(5):289–95. [DOI] [PubMed] [Google Scholar]
- 5.Budoff MJ, Dowe D, Jollis JG, Gitter M, Sutherland J, Halamert E, Scherer M, Bellinger R, Martin A, Benton R, Delago A, Min JK. Diagnostic performance of 64-multidetector row coronary computed tomographic angiography for evaluation of coronary artery stenosis in individuals without known coronary artery disease: results from the prospective multicenter ACCURACY (Assessment by Coronary Computed Tomographic Angiography of Individuals Undergoing Invasive Coronary Angiography) trial. J Am Coll Cardiol 2008. November 18;52(21):1724–32. [DOI] [PubMed] [Google Scholar]
- 6.Miller JM, Rochitte CE, Dewey M, Arbab-Zadeh A, Niinuma H, Gottlieb I, Paul N, Clouse ME, Shapiro EP, Hoe J, Lardo AC, Bush DE, de Roos A, Cox C, Brinker J, Lima JA. Diagnostic performance of coronary angiography by 64-row CT. N Engl J Med 2008. November 27;359(22):2324–36. [DOI] [PubMed] [Google Scholar]
- 7.Ostrom MP, Gopal A, Ahmadi N, Nasir K, Yang E, Kakadiaris I, Flores F, Mao SS, Budoff MJ. Mortality incidence and the severity of coronary atherosclerosis assessed by computed tomography angiography. J Am Coll Cardiol 2008. October 14;52(16):1335–43. [DOI] [PubMed] [Google Scholar]
- 8.Min JK, Shaw LJ, Devereux RB, Okin PM, Weinsaft JW, Russo DJ, Lippolis NJ, Berman DS, Callister TQ. Prognostic value of multidetector coronary computed tomographic angiography for prediction of all-cause mortality. J Am Coll Cardiol 2007. September 18;50(12):1161–70. [DOI] [PubMed] [Google Scholar]
- 9.Chow BJ, Small G, Yam Y, Chen L, Achenbach S, Al-Mallah M, Berman DS, Budoff MJ, Cademartiri F, Callister TQ, Chang HJ, Cheng V, Chinnaiyan KM, Delago A, Dunning A, Hadamitzky M, Hausleiter J, Kaufmann P, Lin F, Maffei E, Raff GL, Shaw LJ, Villines TC, Min JK. Incremental prognostic value of cardiac computed tomography in coronary artery disease using CONFIRM: COroNary computed tomography angiography evaluation for clinical outcomes: an InteRnational Multicenter registry. Circ Cardiovasc Imaging 2011. September;4(5):463–72. [DOI] [PubMed] [Google Scholar]
- 10.Mortality incidence of patients with non-obstructive coronary artery disease diagnosed by computed tomography angiography., (2011). [DOI] [PubMed]
- 11.Prognostic value of coronary computed tomographic angiography in comparison with calcium scoring and clinical risk scores., (2011). [DOI] [PubMed]
- 12.Prognostic value of multidetector coronary computed tomographic angiography for prediction of all-cause mortality., (2007). [DOI] [PubMed]
- 13.Prognostic value of multislice computed tomography coronary angiography in patients with known or suspected coronary artery disease., (2007). [DOI] [PubMed]
- 14.Prognostic value of CT angiography for major adverse cardiac events in patients with acute chest pain from the emergency department: 2-year outcomes of the ROMICAT trial., (2011). [DOI] [PMC free article] [PubMed]
- 15.Prognostic Value of Multislice Computed Tomography and Gated Single-Photon Emission Computed Tomography in Patients With Suspected Coronary Artery Disease, (2009). [DOI] [PubMed]
- 16.Meta-analysis and systematic review of the long-term predictive value of assessment of coronary atherosclerosis by contrast-enhanced coronary computed tomography angiography., (2011). [DOI] [PubMed]
- 17.Prognostic value of cardiac computed tomography angiography: a systematic review and meta-analysis., (2011). [DOI] [PubMed]
- 18.Smith SC Jr., Allen J, Blair SN, Bonow RO, Brass LM, Fonarow GC, Grundy SM, Hiratzka L, Jones D, Krumholz HM, Mosca L, Pasternak RC, Pearson T, Pfeffer MA, Taubert KA. AHA/ACC guidelines for secondary prevention for patients with coronary and other atherosclerotic vascular disease: 2006 update: endorsed by the National Heart, Lung, and Blood Institute. Circulation 2006. May 16;113(19):2363–72. [DOI] [PubMed] [Google Scholar]
- 19.Antman EM, Hand M, Armstrong PW, Bates ER, Green LA, Halasyamani LK, Hochman JS, Krumholz HM, Lamas GA, Mullany CJ, Pearle DL, Sloan MA, Smith SC Jr., Anbe DT, Kushner FG, Ornato JP, Jacobs AK, Adams CD, Anderson JL, Buller CE, Creager MA, Ettinger SM, Halperin JL, Hunt SA, Lytle BW, Nishimura R, Page RL, Riegel B, Tarkington LG, Yancy CW. 2007 Focused Update of the ACC/AHA 2004 Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines: developed in collaboration With the Canadian Cardiovascular Society endorsed by the American Academy of Family Physicians: 2007 Writing Group to Review New Evidence and Update the ACC/AHA 2004 Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction, Writing on Behalf of the 2004 Writing Committee. Circulation 2008. January 15;117(2):296–329. [DOI] [PubMed] [Google Scholar]
- 20.Smith SC Jr., Benjamin EJ, Bonow RO, Braun LT, Creager MA, Franklin BA, Gibbons RJ, Grundy SM, Hiratzka LF, Jones DW, Lloyd-Jones DM, Minissian M, Mosca L, Peterson ED, Sacco RL, Spertus J, Stein JH, Taubert KA. AHA/ACCF Secondary Prevention and Risk Reduction Therapy for Patients with Coronary and other Atherosclerotic Vascular Disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation. Circulation 2011. November 29;124(22):2458–73. [DOI] [PubMed] [Google Scholar]
- 21.Anderson JL, Adams CD, Antman EM, Bridges CR, Califf RM, Casey DE Jr., Chavey WE 2nd, Fesmire FM, Hochman JS, Levin TN, Lincoff AM, Peterson ED, Theroux P, Wenger NK, Wright RS, Smith SC Jr., Jacobs AK, Halperin JL, Hunt SA, Krumholz HM, Kushner FG, Lytle BW, Nishimura R, Ornato JP, Page RL, Riegel B. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non ST-Elevation Myocardial Infarction): developed in collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons: endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine. Circulation 2007. August 14;116(7):e148–304. [DOI] [PubMed] [Google Scholar]
- 22.Pearson TA, Blair SN, Daniels SR, Eckel RH, Fair JM, Fortmann SP, Franklin BA, Goldstein LB, Greenland P, Grundy SM, Hong Y, Miller NH, Lauer RM, Ockene IS, Sacco RL, Sallis JF Jr., Smith SC Jr., Stone NJ, Taubert KA. AHA Guidelines for Primary Prevention of Cardiovascular Disease and Stroke: 2002 Update: Consensus Panel Guide to Comprehensive Risk Reduction for Adult Patients Without Coronary or Other Atherosclerotic Vascular Diseases. American Heart Association Science Advisory and Coordinating Committee. Circulation 2002. July 16;106(3):388–91. [DOI] [PubMed] [Google Scholar]
- 23.Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 2002. December 17;106(25):3143–421. [PubMed] [Google Scholar]
- 24.Grundy SM, Cleeman JI, Merz CN, Brewer HB Jr., Clark LT, Hunninghake DB, Pasternak RC, Smith SC Jr., Stone NJ. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III Guidelines. J Am Coll Cardiol 2004. August 4;44(3):720–32. [DOI] [PubMed] [Google Scholar]
- 25.Colwell JA. Aspirin therapy in diabetes. Diabetes Care 2004. January;27 Suppl 1:S72–3. [DOI] [PubMed] [Google Scholar]
- 26.Hayden M, Pignone M, Phillips C, Mulrow C. Aspirin for the primary prevention of cardiovascular events: a summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med 2002. January 15;136(2):161–72. [DOI] [PubMed] [Google Scholar]
- 27.Aspirin for the primary prevention of cardiovascular events: recommendation and rationale. Ann Intern Med 2002. January 15;136(2):157–60. [DOI] [PubMed] [Google Scholar]
- 28.Miedema MD, Duprez DA, Misialek JR, Blaha MJ, Nasir K, Silverman MG, Blankstein R, Budoff MJ, Greenland P, Folsom AR. Use of coronary artery calcium testing to guide aspirin utilization for primary prevention: estimates from the multi-ethnic study of atherosclerosis. Circ Cardiovasc Qual Outcomes 2014. May;7(3):453–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Taylor AJ, Bindeman J, Feuerstein I, Le T, Bauer K, Byrd C, Wu H, O’Malley PG. Community-based provision of statin and aspirin after the detection of coronary artery calcium within a community-based screening cohort. J Am Coll Cardiol 2008. April 8;51(14):1337–41. [DOI] [PubMed] [Google Scholar]
- 30.Arad Y, Spadaro LA, Roth M, Newstein D, Guerci AD. Treatment of asymptomatic adults with elevated coronary calcium scores with atorvastatin, vitamin C, and vitamin E: the St. Francis Heart Study randomized clinical trial. J Am Coll Cardiol 2005. July 5;46(1):166–72. [DOI] [PubMed] [Google Scholar]
- 31.McEvoy JW, Blaha MJ, Nasir K, Yoon YE, Choi EK, Cho IS, Chun EJ, Choi SI, Rivera JJ, Blumenthal RS, Chang HJ. Impact of coronary computed tomographic angiography results on patient and physician behavior in a low-risk population. Arch Intern Med 2011. July 25;171(14):1260–8. [DOI] [PubMed] [Google Scholar]
- 32.LaBounty TM, Devereux RB, Lin FY, Weinsaft JW, Min JK. Impact of coronary computed tomographic angiography findings on the medical treatment and control of coronary artery disease and its risk factors. Am J Cardiol 2009. October 1;104(7):873–7. [DOI] [PubMed] [Google Scholar]
- 33.Cheezum MK, Hulten EA, Smith RM, Taylor AJ, Kircher J, Surry L, York M, Villines TC. Changes in Preventive Medical Therapies and CV Risk Factors After CT Angiography. JACC Cardiovasc Imaging 2013. April 5. [DOI] [PubMed] [Google Scholar]
- 34.Hulten E, Bittencourt MS, Singh A, O’Leary D, Christman MP, Osmani W, Abbara S, Steigner ML, Truong QA, Nasir K, Rybicki FF, Klein J, Hainer J, Brady TJ, Hoffmann U, Ghoshhajra BB, Hachamovitch R, Di Carli MF, Blankstein R. Coronary artery disease detected by coronary computed tomographic angiography is associated with intensification of preventive medical therapy and lower low-density lipoprotein cholesterol. Circ Cardiovasc Imaging 2014. July;7(4):629–38. [DOI] [PubMed] [Google Scholar]
- 35.Hachamovitch R, Nutter B, Hlatky MA, Shaw LJ, Ridner ML, Dorbala S, Beanlands RS, Chow BJ, Branscomb E, Chareonthaitawee P, Weigold WG, Voros S, Abbara S, Yasuda T, Jacobs JE, Lesser J, Berman DS, Thomson LE, Raman S, Heller GV, Schussheim A, Brunken R, Williams KA, Farkas S, Delbeke D, Schoepf UJ, Reichek N, Rabinowitz S, Sigman SR, Patterson R, Corn CR, White R, Kazerooni E, Corbett J, Bokhari S, Machac J, Guarneri E, Borges-Neto S, Millstine JW, Caldwell J, Arrighi J, Hoffmann U, Budoff M, Lima J, Johnson JR, Johnson B, Gaber M, Williams JA, Foster C, Hainer J, Di Carli MF. Patient management after noninvasive cardiac imaging results from SPARC (Study of myocardial perfusion and coronary anatomy imaging roles in coronary artery disease). J Am Coll Cardiol 2012. January 31;59(5):462–74. [DOI] [PubMed] [Google Scholar]
- 36.Maddox TM, Ho PM, Roe M, Dai D, Tsai TT, Rumsfeld JS. Utilization of secondary prevention therapies in patients with nonobstructive coronary artery disease identified during cardiac catheterization: insights from the National Cardiovascular Data Registry Cath-PCI Registry. Circ Cardiovasc Qual Outcomes 2010. November;3(6):632–41. [DOI] [PubMed] [Google Scholar]