Depressive disorders are among the leading causes of disease-related burden worldwide.1 To a large extent, the negative consequences of depression are due to its peak incidence in adolescence and early adulthood, and chronicity throughout life.2 Given the limited efficacy of available interventions to treat depression in adolescence,3 it is compelling to invest in preventive strategies to reduce its burden during this key developmental phase and across the lifespan.
Universal preventive approaches (ie, directed to all individuals, irrespective of a priori risk status) have been developed, most using school-based psychosocial interventions. Despite initial hopes, large trials did not show efficacy of such strategies for the prevention of depression.4 Conversely, targeting individuals at high risk for the disorder has been more successful, but identification of those individuals for whom preventive interventions should be delivered is still a major challenge for the field.
Indicated prevention targets high-risk individuals identified as having minimal but detectable signs or symptoms that foreshadow a disorder, but who do not meet diagnostic criteria for a full-blown diagnosis. Such programmes have been tested and showed efficacy in reducing the incidence of depression;5 however, given the episodic nature of the disorder, uncertainties remain (eg, an adolescent with subsyndromal symptoms might be in partial remission, recovering from a previous episode). Another targeted approach, selective prevention, focuses on subgroups at increased risk on the basis of the presence of biological, psychological, or social factors. Promising results, for example, have been obtained with interventions targeted at youth with a parental history of depression.6 Although family history has been consistently identified as a risk factor for depression, this single factor alone has limited predictive value,7 and thus other risk factors also need to be considered.
Given the complexity of the causes of mental disorders, approaches that reconcile the coexistence of several risk factors simultaneously are needed. This strategy has been recurrent in other fields of medicine; for example, information from multiple risk factors (eg, blood pressure, diabetes, and smoking) is combined to generate composite risk scores to detect individuals at high risk for cardiovascular events.8 Furthermore, such models go beyond a categorical definition of risk (present vs absent), recognising its dimensional nature.
Using multivariate scores to stratify risk constitutes a promising avenue to identify youth at risk for depression early in adolescence, to further understand pathophysiological mechanisms and, ultimately, to selectively target patients for preventive interventions. Considering the gaps in our understanding of causes of adolescent depression, it is possible that many factors presently available for risk stratification will be markers rather than causal agents. Ideally, improving our ability to identify individuals at high risk will allow for the in-depth study of novel, previously unidentified causal factors. Additionally, identifying youth at extremely low risk might also enhance the validity of case-control studies, because comparison groups are typically selected based on lack of depressive symptoms or diagnosis, with little attention to ensure that they represent individuals with the lowest possible risk of subsequently developing depression.
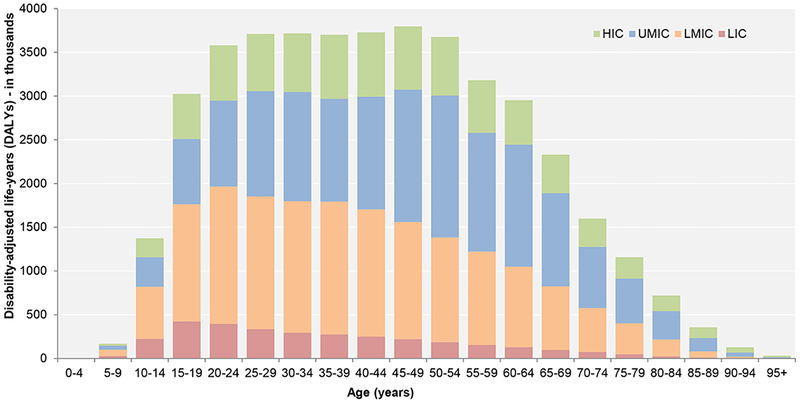
To truly address the worldwide burden of adolescent depression, all these initiatives need a global perspective. Even if it were possible to completely eradicate adolescent depression in high-income countries, this eradication would only represent a limited reduction in the global burden of the disorder, because 9 out of 10 individuals overall under the age of 18 years live in low-income and middle-income countries (Figure 1).1,9 Also, studying depression across multiple settings might provide insights into common or context-specific risk and protective factors. Crucial considerations for such research include exploring the ethical and operational aspects associated with the implementation of risk stratification tools for depression among adolescents, and how preventive strategies might be effectively used across different settings. These strategies will require the involvement of youth, families, health-care providers, teachers, and other stakeholders.
Fig. 1.
Burden of depressive disorders in terms of total disability-adjusted life-years (DALYs) across the lifespan. HIC, high-income country; LIC, low-income country; LMIC, lower-middle-income country; UMIC, upper-middle-income country. Data extracted from the Global Burden of Disease Study 2017.
Recognising the need to advance research on the early detection of depression and its precursors in the first decades of life (panel), a multidisciplinary team of investigators has gathered to establish the IDEA (Identifying Depression Early in Adolescence) network.10 Over the next few years, this group will do research using a variety of quantitative and qualitative methods and involving a wide range of stakeholders in distinct contexts (Brazil, Nepal, Nigeria, and UK). Based on data from existing cohorts, we will develop and test a composite score to stratify for the risk of developing major depression among adolescents, and use this score to investigate high-risk and low-risk status profiles using in-depth neurobiological and psychosocial assessments. Our ultimate goal is to improve the early detection and prevention of adolescent depression, no matter where.
Panel: Research priorities for depression in adolescents.
Collaborating with young people, mental health service users, and other stakeholders to develop and implement detection and prevention strategies for depression in adolescents across cultures and contexts
Developing and validating multivariate scores to stratify adolescents at high- and at low-risk for the development of major depression, accounting for contextual heterogeneity
Building capacity for clinical, psychosocial, and biological assessment of depressive disorders and correlates among youth with harmonised measures across cultures and contexts
Assessing how context affects exposure to environmental risk and protective factors to shape trajectories for developing depression among adolescents
Exploring how technology use and globalisation shape risks and protective factors, as well as early detection and prevention strategies, for depression during adolescence
Acknowledgments
VM has received research funding from Johnson & Johnson as part of a research programme on depression and inflammation, outside the submitted work.
The IDEA project is funded by an MQ Brighter Futures grant (MQBF/1 IDEA). Additional support was provided by the UK Medical Research Council (MC_PC_MR/R019460/1) and the Academy of Medical Sciences (GCRFNG\100281) under the Global Challenges Research Fund. CK is a Brazilian National Council for Scientific and Technological Development (CNPq) researcher.
Footnotes
All other authors declare no competing interests.
References
- 1.Institute for Health Metrics and Evaluation. GBD compare—Viz Hub. http://vizhub.healthdata.org/gbd-compare/ (accessed Jan 10, 2019).
- 2.Thapar A, Collishaw S, Pine DS, Thapar AK. Depression in adolescence. Lancet 2012; 379: 1056–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cipriani A, Zhou X, Del Giovane C, et al. Comparative efficacy and tolerability of antidepressants for major depressive disorder in children and adolescents: a network meta-analysis. Lancet 2016; 388: 881–90. [DOI] [PubMed] [Google Scholar]
- 4.Stallard P, Sayal K, Phillips R, et al. Classroom based cognitive behavioural therapy in reducing symptoms of depression in high risk adolescents: pragmatic cluster randomised controlled trial. BMJ 2012; 345: e6058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ormel J, Cuijpers P, Jorm AF, Schoevers R. Prevention of depression will only succeed when it is structurally embedded and targets big determinants. World Psychiatry 2019; 18: 111–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brent DA, Brunwasser SM, Hollon SD, et al. Effect of a cognitive-behavioral prevention program on depression 6 years after implementation among at-risk adolescents: a randomized clinical trial. JAMA Psychiatry 2015; 72: 1110–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Weissman MM, Berry OO, Warner V, et al. A 30-year study of 3 generations at high risk and low risk for depression. JAMA Psychiatry 2016; 73: 970–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.D’Agostino RB Sr, Vasan RS, Pencina MJ, et al. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation 2008; 117: 743–53. [DOI] [PubMed] [Google Scholar]
- 9.Kieling C, Baker-Henningham H, Belfer M, et al. Child and adolescent mental health worldwide: evidence for action. Lancet 2011; 378: 1515–25. [DOI] [PubMed] [Google Scholar]
- 10.MQ: Transforming Mental Health. Identifying depression early in adolescence (IDEA). https://www.mqmentalhealth.org/research/profiles/identifying-depression-early-in-adolescence (accessed Jan 10, 2019).