Abstract
Background
Dementia with Lewy bodies (DLB) is a progressive form of dementia, accompanied by a range of behavioural and psychological symptoms. The aim of this study was to identify current clinical practice for the treatment of DLB in Japan.
Methods
We conducted a survey of medical doctors engaged in the management of dementia in Japan. Participants were divided into two groups: psychiatrists (Group P) and neurologists or neurosurgeons (Group NS). Doctors completed a questionnaire and we analysed their responses to compare the two groups with regard to diagnosis and treatment of DLB, and in particular the treatment of behavioural and psychological symptoms of dementia (BPSD).
Results
Responses suggested that Group P conducted biomarker examinations less frequently and decided on their own therapeutic strategies more frequently than did Group NS. Both groups most frequently selected hallucinations/delusions as the symptoms given highest treatment priority. More than 70% of respondents in both groups reported having difficulties in treating BPSD. Atypical antipsychotics were more frequently prescribed by Group P, but were also prescribed in 70% of patients in Group NS. A third of patients received atypical antipsychotics for more than 1 year.
Conclusions
The responses to this survey highlighted the difficulties faced by clinicians managing patients with DLB and identified the need to effectively treat BPSD in such patients.
Keywords: BPSD, dementia with Lewy bodies, diagnosis, survey, treatment
INTRODUCTION
A study in which a sequential series of brain autopsies was conducted indicated that among dementing illnesses, the frequency of dementia with Lewy bodies (DLB) is high, second to that of Alzheimer‐type dementia (ATD).1 In Japan which has an aging population, it is predicted that medical doctors will encounter and be required to manage more patients with DLB in the future. However, the condition may be difficult to diagnose and treat because patients with DLB tend to concurrently present with various symptoms, including behavioural and psychological symptoms of dementia (BPSD), neurological symptoms, and autonomic nervous symptoms, in addition to cognitive impairment. Furthermore, the stage at and order in which each of these symptoms occurs varies from patient to patient. For patients in early stages of DLB in particular, cognitive impairment is mild and it is less likely that dementia will be noticed. Some such patients may be misdiagnosed as having psychiatric disorders, such as major depression and senile mental disorders. Consequently, they may receive treatment for these other conditions, rather than for the underlying cause of their symptoms. Therefore, understanding the current clinical practice for the diagnosis and management of DLB is important when formulating future therapeutic strategies for DLB in Japan.
In the present study, we conducted a survey of medical doctors involved in the management of dementia, via an electronic questionnaire. The aim of the study was to identify current practice for DLB treatment among clinicians in specialised medical care units (psychiatry, neurology and neurosurgery). Furthermore, we specifically probed clinicians on their management of BPSD.
METHODS
Participants
We surveyed 100 psychiatrists, 100 neurologists, and 100 neurosurgeons, with a total sample of 300 doctors. Eligible doctors managed at least 20 patients with dementia and one patient with DLB each month. Included doctors were classified into categories according to the major specialised medical care units. Specialists were separated from non‐specialists in this survey to determine if the presence or absence of specialised expertise would produce any difference in clinical practice for the management of DLB. Each medical care category consisted of 50 non‐specialists and 50 specialists (i.e., doctors qualified as specialists for dementia by at least one academic society from the following: Japanese Psychogeriatric Society, Japan Society for Dementia Research, and Japan Psychiatric Hospitals Association).
Procedures
Between 12 July 2017 and 10 August 2017, a questionnaire was made available to eligible doctors on a website. Participation was anonymous, with each participant accessing the website and responding to the questionnaire online (refer to Supporting Information, Appendix S1).
Before completing the online survey, respondents were informed that the survey results would be analysed, disclosed, and provided to medical institutions and companies, as well as published at scientific conferences, in scientific papers, and on any other relevant occasions. The questionnaire was made available only to those who consented to the data being disseminated in this manner. It was not necessary to apply to the ethics review committee, because this study was an investigation of physicians and that personal information was protected.
The results of the survey were compiled according to the following groups: psychiatrists (Group P) and neurologists or neurosurgeons (Group NS); or specialists and non‐specialists. Subsequently, we conducted between‐group comparisons to identify similarities and differences in clinical practice. Based on the questionnaire, two groups consisting of Group P or Group NS were compiled and compared. SPSS Version 24 (IBM Corp., Tokyo, Japan) was used for statistical analyses and population rates were tested. The purpose of the survey was to explore the actual status of current DLB diagnosis and treatment, and not to test a specific hypothesis. Accordingly, our statistical analyses indicate exploratory results.
RESULTS
Participant characteristics
We first compared the psychiatrists who primarily manage psychiatric symptoms of DLB with the neurologists and neurosurgeons who primarily manage neurological symptoms of DLB to determine if there is any difference in terms of diagnosis and treatment between these two groups. Group P had a mean age of 47.5 years and Group NS had a mean age of 50.3 years. In both groups, approximately 80.0% of respondents were working in hospitals or clinics. Regarding the place of work, compared with Group NS, there was a higher proportion of respondents working in clinics in Group P (Group P: 21.0% vs. Group NS: 13.5%), and a lower proportion working in university hospitals in Group P (Group P: 7.0% vs. Group NS: 20.0%). Group P also had a greater number of clinicians belonging to medical centres for dementia than did Group NS (Group P: 27.0% vs. Group NS: 14.5%). The medical centre for dementia is a dedicated medical institution in which dementia is diagnosed, BPSD and physical complications are managed, and medical consultation with specialised doctors is arranged. Moreover, through collaboration with primary care doctors, nursing homes/welfare facilities for the elderly, and local governments, the medical centre for dementia provides adequate specialised medical care for patients with dementia and their family members in local communities.2
In Group P, 27.0% of respondents were specialists for dementia qualified by the Japanese Psychogeriatric Society, 17.0% by the Japan Society for Dementia Research, and 19.0% by the Japan Psychiatric Hospital Association (some were qualified by more than one academic society). In Group NS, 4.0% of respondents were specialists for dementia qualified by the Japanese Psychogeriatric Society, 48.5% by the Japan Society for Dementia Research, and 0.5% by the Japan Psychiatric Hospital Association. Moreover, 31.0% and 34.0% of respondents in Groups P and NS, respectively, were qualified as dementia support physicians. The dementia support physician functions as an adviser to primary care doctors regarding diagnosis of dementia and any other relevant matters, and it plays a central role in promoting collaboration with local communities.
The mean number of dementia patients examined by respondents in the past month was 54.7 (median: 35.0) for Group P and 57.7 (median: 35.0) for Group NS. The difference between the average and the median number of patients indicates that the number of patients in many clinicians is biased toward less than average. Among these, patients with ATD accounted for 58.5% in Group P and 59.3% in Group NS, vascular dementia accounted for 19.3% in Group P and 18.6% in Group NS, DLB patients accounted for 15.0% in Group P and 14.1% in Group NS, and other types of dementia accounted for 7.2% in Group P and 8.0% in Group NS. There was no significant difference in types of dementia between the groups. The proportion of patients with ATD with parkinsonism was 9.0% for Group P and 9.6% for Group NS, indicating no difference between the two groups. The proportion of patients with DLB with parkinsonism was higher in Group NS (71.8%) than in Group P (59.9%).
In terms of decision‐making about therapeutic strategies for patients with DLB, 91.0% and 81.0% of Groups P and NS, respectively, reported that they decided on their own diagnosis and therapeutic strategies, indicating a significantly higher proportion in Group P. The proportion of respondents suggesting that they either make decisions on diagnosis and therapeutic strategies or conduct treatment themselves was also significantly higher in Group P (Group P: 99.0% vs. Group NS: 94.0%).
Figure 1 shows the drugs prescribed by respondents for patients with dementia in the past 6 months. The two groups did not significantly differ from each other in the proportions of cholinesterase inhibitors prescribed, whereas memantine was prescribed significantly more often by Group P than by Group NS. All antipsychotic agents were prescribed significantly more often by Group P than by Group NS. In addition, yokukansan, trazodone, benzodiazepine antianxiety drugs, and mood stabilizers were all more frequently prescribed by Group P than by Group NS.
Figure 1.
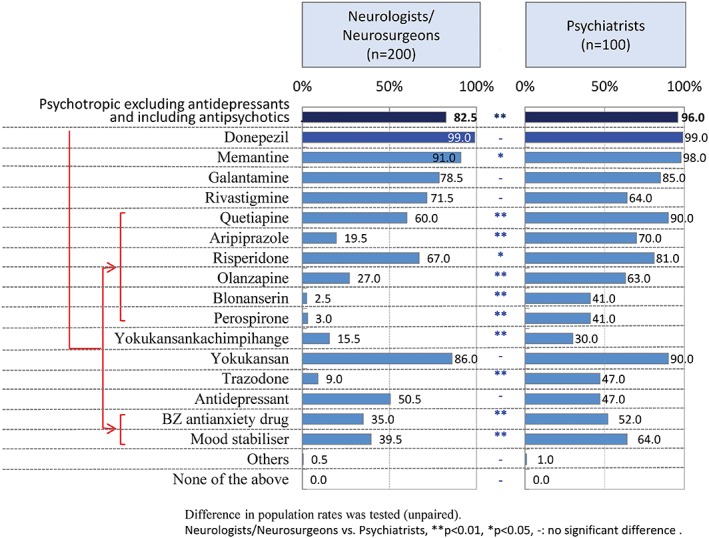
Drugs prescribed by respondents for patients with dementia in the past 6 months. Answers in response to: ‘SC5‐1. Among the anti‐dementia drugs and psychotropic drugs listed below, please select those you have prescribed for patients with dementia in the past 6 months (multiple answers allowed).’ The difference in population rates between the two groups, i.e., the group of neurologists/neurosurgeons and the group of psychiatrists was tested (unpaired).
Diagnosis and treatment of DLB
Among the biomarkers and examinations reported to always be conducted when diagnosing DLB, computed tomography/magnetic resonance imaging of the head (Group P: 62.0% vs. Group NS: 89.0%), neurological examinations (Group P: 38.0% vs. Group NS: 76.0%), and dopamine transporter single‐photon emission computed tomography imaging (Group P: 2.0% vs. Group NS: 13.5%) were performed significantly more frequently by Group NS. However, electroencephalography (Group P: 16.0% vs. Group NS: 8.0%) was performed significantly more frequently by Group P. When combining answers for ‘always conducted’ and ‘conducted as appropriate’, in addition to the examinations stated above, positron emission tomography/single‐photon emission computed tomography imaging and meta‐iodobenzylguanidine myocardial scintigraphy were also performed significantly more frequently by Group NS, whereas no difference was observed in rates of electroencephalography. The rate of REM sleep behavioural disorder (RBD) screening, olfactometry, and overnight polysomnography were not different between both group.
When questioned about the length of time from suspicion of DLB to a definite diagnosis, respondents most frequently reported a period of < 3 months (Group P: 49.0% and Group NS: 48.0%), followed by ≥ 3 months to < 6 months (Group P: 40.0% and Group NS: 36.0%). Several diagnoses were identified as most frequently made prior to the diagnosis of DLB. In Group P, respondents reported that ATD (45.0%), delirium (18%), Parkinson's disease (PD) (15.0%), major depression (12.0%), and delusional disorders (6%) were often diagnosed. In Group NS, respondents reported that ATD (41.0%), PD (34.0%), delirium (9.5%), major depression (6.0%), and delusional disorders (4.0%) were often diagnosed. In both groups, the most frequent challenging issues when diagnosing DLB identified by respondents were ‘symptoms are not stable’, followed by ‘differentiation from the other illnesses’.
In Japan, no drugs have yet been given official approval for the management of BPSD. When asked which symptoms are observed in patients with DLB, the results suggest that there were significantly greater proportions of patients with DLB presenting with cognitive impairment, parkinsonism, hallucinations/delusions, autonomic failure, RBD, and depression/apathy in Group NS than in Group P.
When asked which symptoms are currently prioritised for treatment (Fig. 2), hallucinations/delusions were most frequently selected by both groups (Group P: 54.0% and Group NS: 46.5%). The second and third most prioritised symptoms for treatment were irascibility/irritability and cognitive impairment in Group P, and cognitive impairment and parkinsonism in Group NS. There was a significantly greater proportion of clinicians prioritising parkinsonism in Group NS than in Group P. There was a significantly greater proportion of clinicians prioritising parkinsonism and cognitive impairment in Group NS, whereas the proportion prioritising depression/apathy was significantly greater in Group P. The top three symptoms in patients with DLB that respondents expressed a desire to prioritise in future were cognitive impairment, parkinsonism, and depression/apathy in this order for Group P, and hallucinations/delusions, cognitive impairment, and depression/apathy in this order for Group NS (Fig. 3).
Figure 2.
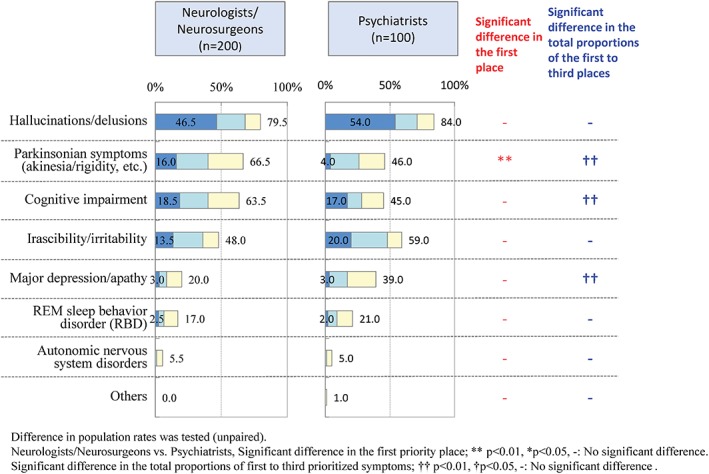
Current status of prioritisation of symptoms to be treated in patients with dementia with Lewy bodies. Answers in response to: ‘Q2. When you treat patients with dementia with Lewy bodies, please indicate your priority from first to third of symptoms to be treated from those listed below.’ The difference in population rates between the two groups, i.e., the group of neurologists/neurosurgeons and the group of psychiatrists was tested (unpaired). ( ) First, (
) First, ( ) second, and (
) second, and ( ) third.
) third.
Figure 3.
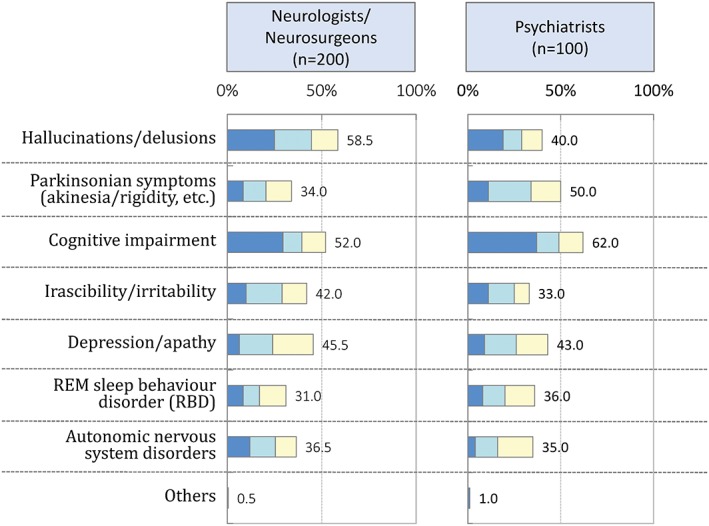
Symptoms in patients with dementia with Lewy bodies that respondents want to focus on treating in the future. Answers in response to: ‘Q2. When you treat patients with dementia with Lewy bodies, please indicate your priority from first to third of symptoms to be treated from those listed below. Regarding symptoms you want to treat but do not feel you treat adequately, please indicate the first to third prioritized symptoms you would like to treat, if possible, from now on.’ ( ) First, (
) First, ( ) second, and (
) second, and ( ) third.
) third.
Treatment of BPSD in patients with DLB
The proportion of patients presenting with BPSD was comparable between the groups (65.7% for Group P and 65.2% for Group NS). The BPSD that were given priority in terms of treatment were hallucinations/delusions in both groups (Group P: 58.0% and Group NS: 56.5%), followed by agitation/aggression (Group P: 18.0% and Group NS: 25.0%).
Respondents also reported that the BPSD with which patients themselves appear to have the greatest burdens are hallucinations/delusions in both groups (Group P: 29.0% and Group NS: 41.0%), followed by depression/apathy (Group P: 23.0% and Group NS: 18.0%), anxiety (Group P: 23.0% and Group NS: 15.0%), agitation/aggression (Group P: 9.0% and Group NS: 12.0%), irritability/lability (Group P: 8.0% and Group NS: 7.5%), and aberrant motor behaviour (Group P: 5.0% and Group NS: 4.5%). The proportion of patients having greatest burdens with hallucinations/delusions was significantly greater in Group NS than in Group P.
In both groups, the BPSD with which patients’ family members and caregivers have the greatest burdens were reported to be agitation/aggression (Group P: 42.0% and Group NS: 50.5%). In Group P, this was followed by aberrant motor behaviour (24.0%) and hallucinations/delusions (19.0%). In Group NS, it was followed by hallucinations/delusions (25.0%) and aberrant motor behaviour (12.0%). The proportion of family members/carers having the greatest burdens with aberrant motor behaviour was significantly greater in Group P than in Group NS (Fig. 4).
Figure 4.
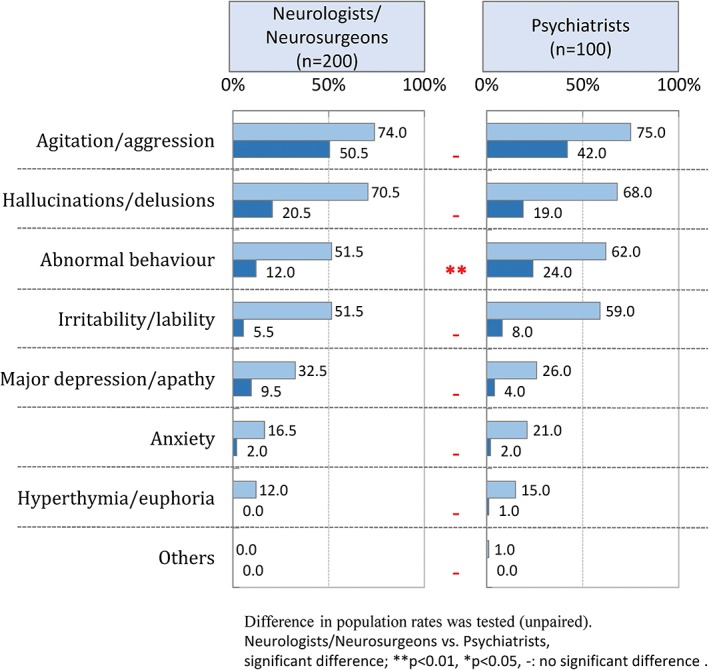
Behavioural and psychological symptoms of dementia that cause caregivers of patients with dementia with Lewy bodies the greatest burdens. Answers in response to: ‘Q24SQ2. Regarding behavioural and psychological symptoms of dementia in patients with dementia with Lewy bodies, please indicate symptoms with which patients’ caregivers have burdens. Among these, please indicate the symptom that is the most troublesome.’ Regarding symptoms with which caregivers have the greatest burdens, the difference in population rates between the two groups, i.e., the group of neurologists/neurosurgeons and the group of psychiatrists was tested (unpaired). ( ) Difficult symptom and (
) Difficult symptom and ( ) most difficult symptom.
) most difficult symptom.
Among the BPSD that respondents reported having most difficulties in treating (combining answers for ‘slight difficulties’ and ‘extreme difficulties’), the greatest proportion selected aberrant motor behaviour in both groups (Group P: 83.0% and Group NS: 79.5%). Approximately 70.0% of respondents reported difficulties treating even the following symptoms: agitation/aggression (Group P: 73.0% and Group NS; 78.5%), irritability/lability (Group P: 74.0% and Group NS: 76.5%), hallucinations/delusions (Group P: 68.0% and Group NS: 79.0%), and depression/apathy (Group P: 70.0% and Group NS: 69.0%). The proportion of respondents who reported treating BPSD themselves was 84.0% for Group P and 49.0% for Group NS. However, half of the respondents in Group NS had a choice to refer patients to psychiatry.
When asked about pharmacotherapies for BPSD, respondents in Group P reported the highest use of atypical antipsychotics (89.0%), followed by anti‐dementia drugs including N‐methyl‐d‐aspartate receptor antagonist (86.0%), and herbal medicines (76.5%). Respondents in Group NS reported the highest use of anti‐dementia drugs (81.5%), followed by herbal medicines (76.5%), and atypical antipsychotics (72.5%) (Fig. 5). The proportion of atypical antipsychotics prescribed was significantly higher in Group P than in Group NS. Comparisons between dementia‐qualified specialists and non‐specialists irrespective of their specialised medical fields provided no significant differences in the proportion of each drug prescribed.
Figure 5.
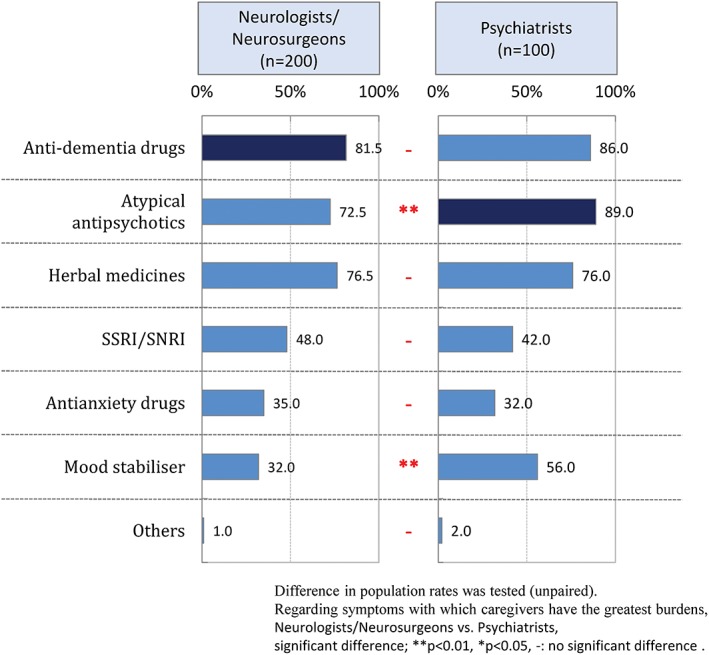
Drugs prescribed to treat behavioural and psychological symptoms of dementia in patients with dementia with Lewy bodies. Answers in response to: ‘Q27. Please indicate the drugs you have prescribed for the management of behavioural and psychological symptoms of dementia in patients with dementia with Lewy bodies (multiple answers allowed).’ The difference in population rates between the two groups, i.e., the group of neurologists/neurosurgeons and the group of psychiatrists was tested (unpaired). SSRI/SNRI: Selective serotonin reuptake inhibitor/Serotonin noradrenalin reuptake inhibitor.
When focusing on pharmacotherapy for hallucinations/delusions, Group P reported the use of quetiapine most often (78.0%), followed by yokukansan (67.0%). In Group NS, yokukansan was most frequently prescribed (67.0%), followed by memantine (62.0%). In this survey, all atypical antipsychotics and trazodone were prescribed significantly more frequently in Group P than in Group NS. There were no significant differences observed in the use of anti‐dementia drugs, yokukansan, or mood stabilisers. Comparisons between qualified specialists and non‐specialists irrespective of their specialised medical fields revealed that the largest proportion prescribed yokukansan in both groups, with no significant differences in the proportions of other drugs prescribed.
We also asked respondents about their prioritisation of treating hallucinations/delusions or parkinsonism. In Group P, there was a similar proportion of respondents suggesting that they treated hallucinations/delusions in parallel with parkinsonism to the proportion reporting that they prioritised hallucinations/delusions (47.0% vs. 46.0%, respectively). In Group NS, the proportion reporting that they treated these symptoms in parallel was higher than that reporting that they gave treatment priority to hallucinations/delusions (53.5% vs. 38.0%, respectively). The proportion of respondents reporting that they prioritised the treatment of parkinsonism was low in both groups (Group P: 5.0% and Group NS: 8.0%). Comparisons between dementia‐qualified specialists and non‐specialists revealed that in both groups the greatest proportion of respondents reported treating these two symptoms in parallel (qualified specialists: 52.7% and non‐specialists: 50.0%).
DISCUSSION
In this study, we conducted an online survey of doctors who are routinely engaged in the management of dementia, to determine current clinical practice for the management of DLB in Japan. We focused on specialised medical care units so as to understand the actual status of diagnosis and treatment of DLB, as well as treatment of BPSD.
A greater proportion of psychiatrists than those of neurologists or neurosurgeons reported that they decided on the diagnosis and therapeutic strategies and/or administer treatment to their patients. Psychiatrists reported prescribing a wide range of psychotropic drugs to patients with dementia in the past 6 months with more prescriptions than neurologists/neurosurgeons of memantine, antipsychotics, yokukansan, trazodone, benzodiazepines, and mood stabilisers.
Our results suggest that when diagnosing and treating DLB, neurologists and neurosurgeons more frequently conduct biomarker‐aided and neurological examinations than do psychiatrists. This finding may be related to how easily they can access these examinations in their workplaces and their specialty. The latest DLB diagnostic criteria place particular importance on biomarker findings. Nonetheless, despite differences in diagnostic assessments, we did not observe any difference between the groups in terms of the length of time to a definite diagnosis of DLB.
We investigated the differential diagnoses most frequently made prior to a diagnosis of DLB, with ATD the most frequent such diagnosis in both groups. This was followed by delirium, PD, and major depression in psychiatrists, and by PD, delirium, and major depression in neurologists and neurosurgeons. It has been reported that delirium occurs more frequently in DLB than does ATD.3 Moreover, even experts in delirium are reported to have difficulties in differentiating DLB from deliruim.4 This may be explained by difficult differentiation between cognitive fluctuations and delirium when the former are aggravated. However, because a different therapeutic approach is required for cognitive fluctuations and delirium, differential diagnosis is a particularly important challenge in the diagnosis and management of DLB. The higher rate of diagnosis of PD made prior to DLB in Group NS may be related to the fact that many patients presenting chiefly with neurological symptoms visit specialised medical care units. Characteristically, many patients with DLB are diagnosed with major depression or other psychiatric disorders. In the field of psychiatric care for the elderly, it is also particularly important that DLB is differentiated from major depression.5
Respondents reported on the priority given to treatment of different symptoms in DLB, with the greatest proportion of physicians in both groups reporting that hallucinations/delusions are given the highest priority. This was followed by psychiatric symptoms, including irascibility/irritability and cognitive impairment in psychiatrists, but with parkinsonism and cognitive impairment in neurologists and neurosurgeons. Such prioritisation of symptoms to be treated likely reflects the specialty of the respondents. When questioned about symptoms that the respondents want to treat in the future, psychiatrists included cognitive impairment, parkinsonism, and depressive symptoms. This suggests that psychiatrists are interested in treatment of not only psychiatric symptoms but also neurological symptoms.
We also investigated the treatment of BPSD in DLB. Respondents in both groups reported giving the highest treatment priority to hallucinations/delusions first and then agitation/aggression. Respondents reported differences between the patients and their caregivers in symptoms with which they have burdens. Similarly, both groups reported that the BPSD with which patients subjectively consider that they have the greatest burdens are hallucinations/delusions, followed by depression/apathy, and anxiety. In contrast, patients’ family members and caregivers most frequently reported having the greatest burdens with agitation/aggression in both groups, while the proportion reporting handling aberrant motor behaviour was significantly higher in Group P than in Group NS. In this survey, how the patients and their caregivers felt burdens was not investigated and this is one of the limitation of the survey. Nonetheless, the above‐stated findings are interesting because they can provide insight to inform the formulation of therapeutic strategies. Among BPSD, the greatest number of respondents reported having difficulties in treating aberrant motor behaviour, and approximately 70.0% of respondents reported having difficulties in treating the following symptoms: agitation/aggression, irritability/lability, hallucinations/delusions, and depression/apathy. This finding confirms that attending physicians often face difficulties treating BPSD in DLB. Moreover, 80.0% of psychiatrists reported that they themselves treat BPSD, whereas half of neurologists/neurosurgeons consult psychiatry when treating BPSD.
For the treatment of BPSD, non‐pharmacological therapy is prioritised, although there is no evidence indicating the usefulness of this strategy. In this survey, the purpose was to investigate differences among drug regimens used for the treatment of BPSD, and therefore, questions about non‐pharmacological therapy were not asked. When treating BPSD in DLB with pharmacotherapy, psychiatrists more frequently prescribe atypical antipsychotics, although atypical antipsychotics are also prescribed in more than 70% of patients by neurologists and neurosurgeons. Our survey demonstrates that atypical antipsychotics have been continuously prescribed for as long as more than a year in one‐third of patients. Previously, it has been reported that prescription of antipsychotics in DLB shortens the length of time until admission to the nursing home.6 In Japan, as in European and North American countries, risk of mortality is increased among patients with ATD receiving antipsychotics for the treatment of BPSD.7 Indeed, some antipsychotics aggravate extrapyramidal symptoms or autonomic failure.8 In future, when treating patients with DLB, it is important to explore strategies by which administration of antipsychotics can be avoided.
In both groups, around half of the respondents reported that they tend to treat hallucinations/delusions and parkinsonism in parallel, although a greater number of psychiatrists than neurologists/neurosurgeons reported prioritising hallucinations/delusions alone. In contrast, the proportion of respondents who reported prioritising parkinsonism alone was low in both groups.
It has been reported that DLB is difficult to treat because of the coexistence of cognitive impairment, movement disorders, BPSD, and autonomic failure, and it leads to higher mortality rates than does ATD.9 Our survey has demonstrated that, irrespective of specialty, physicians treat DLB patients while taking into account BPSD, movement disorders, and other symptoms involving more than one medical field. Moreover, the proportion of psychotropics prescribed was high for the treatment of BPSD, indicating that respondents have difficulties in managing these symptoms. Psychiatrists reported that they decide on their own therapeutic strategies for BPSD. Psychiatrists also treat parkinsonism but give lower priority to this symptom than do neurologists/neurosurgeons. However, psychiatrists ranked parkinsonism high when asked about symptoms that they want to focus on treating in the future. Extreme caution should be exercised when simultaneously treating parkinsonism and BPSD with pharmacology in patients with DLB. In particular, it is important to pay attention to quality of life and activities of daily living when prioritising symptoms for treatment.
Our survey was conducted with a small number of doctors who are registered at a survey company and therefore has limitations. However, no previous surveys have been conducted in which psychiatrists and neurologists/neurosurgeons have been compared regarding the management of DLB and the status of treatment of BPSD in actual clinical practice. Therefore, the results from this survey are significant in increasing our understanding of the differences and commonalities in diagnosis and treatment among different medical care fields.
Supporting information
Appendix S1 Questionnaires for survey (SC1.–SC5.) and Questionnaire completed by respondents (Q1–Q33).
ACKNOWLEDGMENTS
This survey was conducted as part of a joint research with Medical Affairs, Sumitomo Dainippon Pharma Co., Ltd. with funds from Sumitomo Dainippon Pharma Co., Ltd. The authors extend our cordial gratitude to all concerned for their kind cooperation and assistance.
Disclosure: Co‐author (Osamu Konishi) is employed by Sumitomo Dainippon Pharma Co., Ltd.
Dainippon Sumitomo Pharma
REFERENCES
- 1. Perry RH, Irving D, Blessed G, Fairbairn A, Perry EK. Senile dementia of Lewy body type. A clinically and neuropathologically distinct form of Lewy body dementia in the elderly. J Neurol Sci 1990; 95: 119–139. [DOI] [PubMed] [Google Scholar]
- 2. Awata S. New national health program against dementia in Japan: the medical center for dementia. Psychogeriatrics 2010; 10: 102–106. [DOI] [PubMed] [Google Scholar]
- 3. Vardy E, Holt R, Gerhard A, Richardson A, Snowden J, Neary D. History of a suspected delirium is more common in dementia with Lewy bodies than Alzheimer's disease: a retrospective study. Int J Geriatr Psychiatry 2014; 29: 178–181. [DOI] [PubMed] [Google Scholar]
- 4. Richardson S, Teodorczuk A, Bellelli G et al Delirium superimposed on dementia: a survey of delirium specialists shows a lack of consensus in clinical practice and research studies. Int Psychogeriatr 2016; 28: 853–861. [DOI] [PubMed] [Google Scholar]
- 5. Takahashi S, Mizukami K, Yasuno F, Asada T. Depression associated with dementia with Lewy bodies (DLB) and the effect of somatotherapy. Psychogeriatrics 2009; 9: 56–61. [DOI] [PubMed] [Google Scholar]
- 6. Rongve A, Vossius C, Nore S, Testad I, Aarsland D. Time until nursing home admission in people with mild dementia: comparison of dementia with Lewy bodies and Alzheimer's dementia. Int J Geriatr Psychiatry 2014; 29: 392–398. [DOI] [PubMed] [Google Scholar]
- 7. Arai H, Nakamura Y, Taguchi M et al Mortality risk in current and new antipsychotic Alzheimer's disease users: large scale Japanese study. Alzheimers Dement 2016; 12: 823–830. [DOI] [PubMed] [Google Scholar]
- 8. Tampi RR, Tampi DJ, Balachandran S, Srinivasan S. Antipsychotic use in dementia: a systematic review of benefits and risks from meta‐analyses. Ther Adv Chronic Dis 2016; 7: 229–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Price A, Farooq R, Yuan JM, Menon VB, Cardinal RN, O'Brien JT. Mortality in dementia with Lewy bodies compared with Alzheimer's dementia: a retrospective naturalistic cohort study. BMJ Open 2017; 7: e017504. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1 Questionnaires for survey (SC1.–SC5.) and Questionnaire completed by respondents (Q1–Q33).


