To the Editor:
Granulomatous rosacea is a variant of rosacea characterised by discrete erythematous papules most commonly affecting the central face. It is a rare condition reported primarily in middle‐aged women, and tends to have a chronic course often recalcitrant to therapy. We report a case of granulomatous rosacea treated with chromophore gel‐assisted phototherapy (CGAP).
A 50‐year‐old woman of Lebanese background presented with a 3‐month history of a papulopustular eruption. She described paroxysms of papules affecting the glabellar, malar and mental regions. She denied any flushing or ophthalmological symptoms. Examination demonstrated tumid papules and pustules affecting the glabella with malar erythema composed of fine telangiectasia. There was no appreciable phymatous change (Figure 1A). Biopsy demonstrated ectatic dermal blood vessels and pandermal granulomatous inflammation with lymphocytes and neutrophils (Figure 2A,B). Microbial studies including special stains, as well as bacteria, Mycobacteria and deep fungal culture & PCR were negative. The clinical and pathological findings were consistent with granulomatous rosacea.
Figure 1.
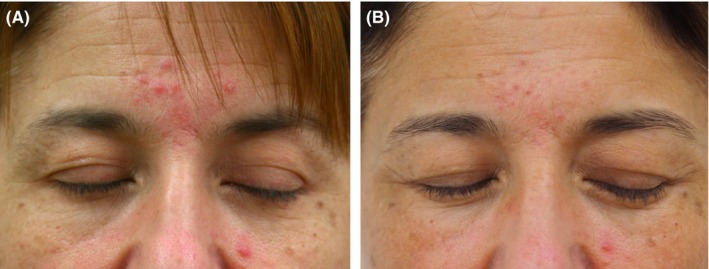
A, Baseline photographs of a patient with a papular eruption affecting the glabellar and malar regions. B, Following twelve treatments with CGAP, significant improvement is observed [Colour figure can be viewed at wileyonlinelibrary.com]
Figure 2.
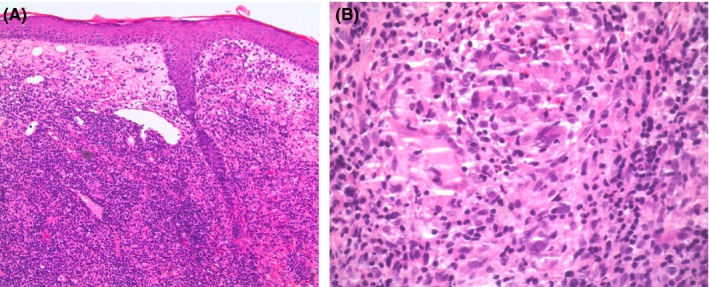
Biopsy demonstrated ectatic dermal blood vessels, and pandermal granulomatous inflammation composed of epithelioid histiocytes, multinuclear giant cells, lymphocytes and neutrophils. A, Haematoxylin and eosin, original magnification × 10. B, Haematoxylin and eosin, original magnification × 40 [Colour figure can be viewed at wileyonlinelibrary.com]
Modest improvement was observed with topical metronidazole, ivermectin and brimonidine and systemic minocycline 50 mg BD led to the development of headache. The patient was reticent to pursue alternate systemic treatments and accordingly a trial of CGAP was pursued. The patient received twelve treatment sessions over 6 weeks involving application of a 2 mm layer of the photoconverter chromophore gel (Kleresca®) followed by irradiation with a multi‐LED lamp (415 nm and 447 nm) (Kleresca®, Balerup, Denmark). Significant improvement was observed in both the papulopustular and erythematotelangiectatic components of her rosacea (Figure 1B). To date, there has been no relapse in her rosacea off all active treatment, at a time‐point 6 months after cessation of CGAP.
Granulomatous rosacea is notoriously difficult to treat, and there is no current consensus regarding the best approach to management. Small‐volume case reports and series have advocated therapeutic options including dapsone, tetracyclines and isotretinoin.1 However, systemic treatment is not always accepted or tolerated, as in the case of our patient.
Chromophore gel‐assisted phototherapy is a new therapeutic modality that has been shown to be effective in papulopustular rosacea,2 as well other conditions such as acne3, 4 and erlotinib induced acneiform eruptions.5 CGAP involves irradiation of a chromophore gel (Kleresca®) with light at the wavelengths 415 and 447 nm to generate a fluorescent spectrum from approximately 510‐630 nm. CGAP is non‐invasive, in‐office intervention with no known systemic side effects. While the pathophysiology of rosacea is unclear, there appears to be an overgrowth of commensal organisms paired with alterations in innate immune response.1 Further studies with greater methodological rigor should be employed to determine the role of CGAP in this setting. However, it is biologically plausible that CGAP may have be effective in the management of rosacea due to its proposed anti‐inflammatory and antibacterial effects.6 Additionally, light based modalities such as phototherapy and photodynamic therapy have been shown to be helpful in other granulomatous diseases, such sarcoidosis, by decreasing interleukin 1 and tumour necrosis factor alpha locally which are necessary for granuloma formation and maintenance.7
This case suggests that there is promise in CGAP as management of granulomatous rosacea. However, a single case report cannot discount the impact of a placebo effect, or the possibility of spontaneous remission. Nonetheless, the noteworthy response of our patient to treatment suggests that CGAP may be of therapeutic value, and warrants further research with more rigorous studies.
CONFLICT OF INTEREST
None declared.
ACKNOWLEDGEMENTS
Dr Deshan Sebaratnam has received a travel grant from FB Dermatology to present at the 27th European Academy of Dermatology and Venereology Congress, Paris.
REFERENCES
- 1. Lee GL, Zirwas MJ. Granulomatous rosacea and periorficial dermatitis: controversies and review of manageent and treatment. Dermatol Clin. 2015;33(3):447‐455. [DOI] [PubMed] [Google Scholar]
- 2. Braun SA, Gerber PA. A photoconverter gel‐assisted blue light therapy for the treatment of rosacea. Int J Dermatol. 2017;56(12):1489‐1490. [DOI] [PubMed] [Google Scholar]
- 3. Nikolis A, Fauverghe S, Scapagnini G, et al. An extension of a multicenter, randomized, split‐face clinical trial evaluating the efficacy and safety of chromophore gel‐assisted blue light phototherapy for the treatment of acne. Int J Dermatol. 2018;57(1):94‐103. [DOI] [PubMed] [Google Scholar]
- 4. Antoniou C, Dessinioti C, Sotiriadis D, et al. A multicenter, randomized, split‐face clinical trial evaluating the efficacy and safety of chromophore gel‐assisted blue light phototherapy for the treatment of acne. Int J Dermatol. 2016;55(12):1321‐1328. [DOI] [PubMed] [Google Scholar]
- 5. Mahendran A, Wong XL, Kao S, et al. Treatment of erlotinib induced acneiform eruption with chromophore‐gel activated phototherapy. Photodermatol Photoimmunol Photomed. 2018. [Epub ahead of print]. 10.1111/phpp.12446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ghate VS, Ng KS, Zhou W, et al. Antibacterial effect of light emitting diodes of visible wavelengths on selected foodborne pathogens at different illumination temperatures. Int J Food Microbiol. 2013;16(166):399‐406. [DOI] [PubMed] [Google Scholar]
- 7. Penrose C, Mercer SE, Shim‐Chang H. Photodynamic therapy for the treatment of cutaneous sarcoidosis. JAAD. 2011;65(1):e12‐e14. [DOI] [PubMed] [Google Scholar]


