Key Points
HLA-DRB1*03:01-DQB1*02:01 haplotype patients develop higher anti–platelet factor 4/heparin (PF4/H) levels following IV heparin exposure.
HLA-restricted antigen presentation may play a role in the formation of anti-PF4/H antibodies.
Introduction
Heparin-induced thrombocytopenia (HIT) is a life-threatening complication of heparin exposure with estimated incidences of 1 in 5000 in general inpatients and 1% to 2% in inpatients following cardiac surgery.1,2 Antibodies against platelet factor 4 (PF4)/heparin (PF4/H) complexes trigger platelet activation, leading to consumptive thrombocytopenia and acquired thrombophilia capable of precipitating severe venous and arterial thrombosis.3 Enzyme-linked immunosorbent assays (ELISAs) are commonly performed to measure anti-PF4/H antibodies in patients with suspected HIT. High optical density (OD) values by ELISA correlate with increased platelet activation in serotonin release assays,4,5 and with the presence of clinical HIT.6-9
The mechanism for developing an anti-PF4/H response is poorly understood, as neither heparin nor PF4 is a foreign antigen in humans. Exogenous heparin may alter intracellular PF4 processing within antigen-presenting cells, causing presentation of aberrant PF4-derived peptides (neoantigens) to T cells.10,11 Although T cells are necessary for the development of anti-PF4/H in murine models,12 proof for aberrant antigen presentation is lacking.
Human PF4 neoantigen presentation may be restricted to specific HLA molecules. We hypothesized that patients having certain class II HLA alleles are predisposed to increased anti-PF4/H antibodies after exposure to heparin. Here, we present a cohort study of 412 heparin-exposed inpatients with paired anti-PF4/H and high-resolution HLA-typing results. We found that high anti-PF4/H antibody levels were associated with a specific class II HLA haplotype widely implicated in autoimmunity.
Methods
Study design
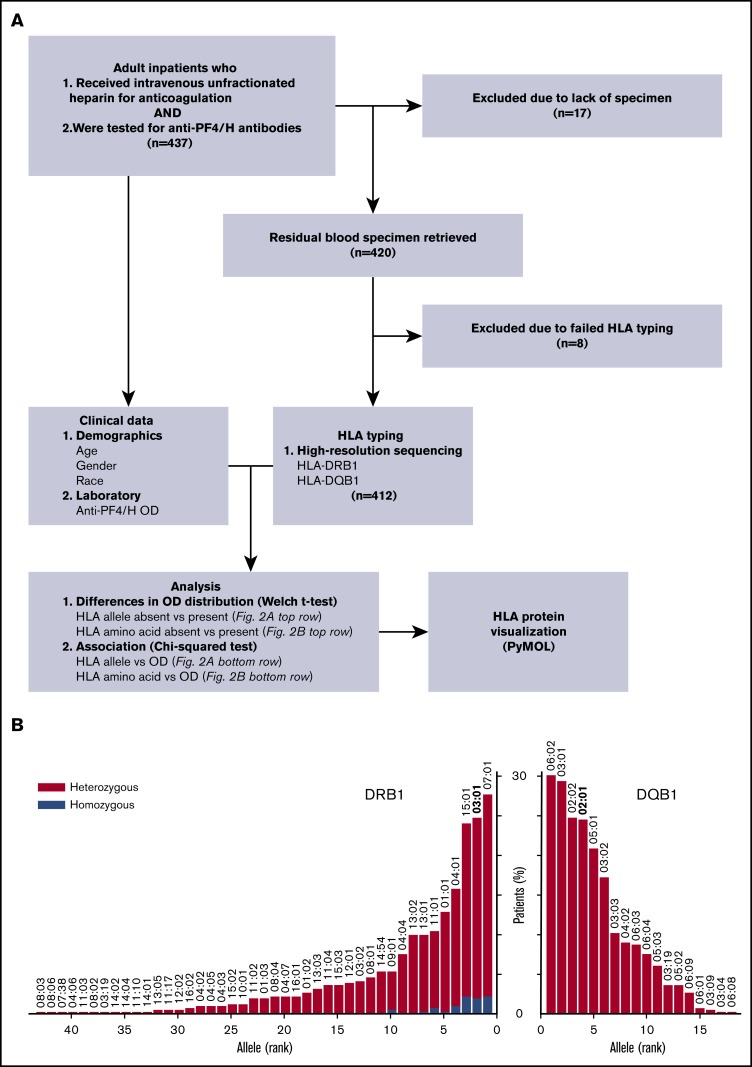
We conducted a single-center cohort study of inpatients who received IV unfractionated heparin for anticoagulation and were subsequently tested for anti-PF4/H due to concerns for HIT (Figure 1). Eligible patients were identified and their demographic information collected from the electronic medical record system. Anti-PF4/H in peripheral blood was measured using a commercial, poly-specific enzyme immunoassay (Asserachrom HPIA-ELISA; Diagnostic Stago). DNA was extracted from residual blood specimens and sequenced (Illumina) for high-resolution 2-field typing of the HLA-DRB1 and -DQB1 loci.13,14 Study approval was obtained from the Human Research Protection Office of Washington University in St. Louis.
Figure 1.
Data analysis
HLA genotypes were examined at both the allele and the amino acid residue levels. Alleles exceeding 5% frequency in our study population were analyzed. Significance for differences in OD values between groups was evaluated using the Welch 2-sided unequal variances Student t test. Significance for associations between OD values (categorized as either high or low based on a moving OD cutoff) and either allele or amino acid residue (categorized as present or absent) was evaluated using the χ2 test of independence. The false discovery rate was controlled at 5% using the Benjamini-Hochberg procedure.
Results and discussion
Patients
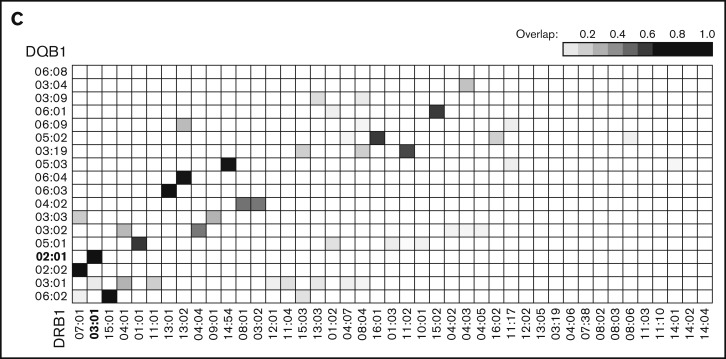
Between September 2016 and November 2017, 437 patients were evaluated, of whom 420 with blood specimens available were enrolled. The final analysis included 412 patients (176 females [42.7%]) who were successfully typed at both HLA loci (Figure 1A). Our study population contained 337 white, 73 black, and 2 Asian patients. Ages ranged from 21 to 87 years (median, 62 years; interquartile range, 50-69 years). Antibody OD values ranged from 0.01 to 3.00 (median, 0.20; interquartile range, 0.09-0.53). There was no significant difference in OD values between patients based on sex, race, or age. Altogether, 43 DRB1 and 18 DQB1 alleles exceeded 5% frequency in our study population (Figure 1B). Genetic linkage was evident between several DRB1-DQB1 allele pairs (Figure 1C).
Anti-PF4/H vs HLA allele
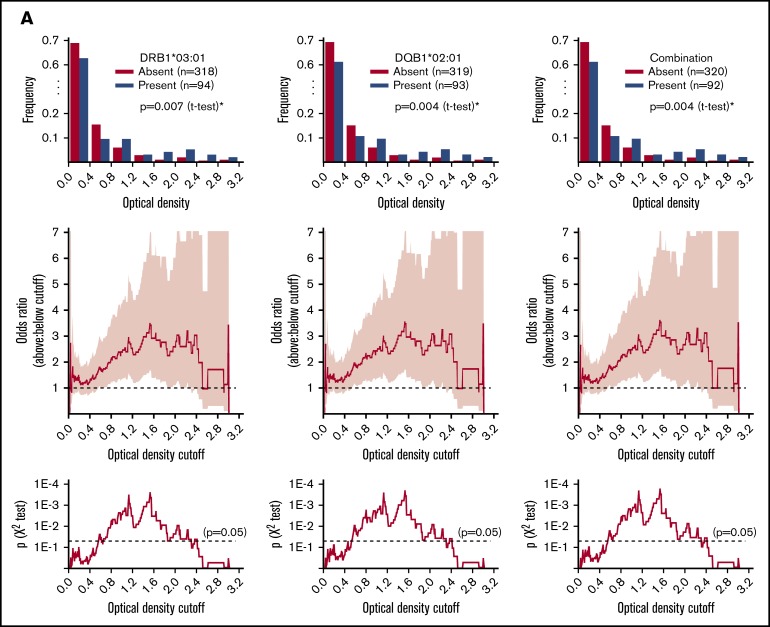
Patients with the DRB1*03:01 and/or DQB1*02:01 allele(s) had higher OD values than those without (P = .004-.007; Figure 2A top row), even after controlling for sex, race, and age. Using a moving OD cutoff to classify anti-PF4/H levels as either high or low, the presence of these alleles was associated with high anti-PF4/H over a broad range of OD value cutoffs (Figure 2A middle and bottom rows). Notably, patients possessing both DRB1*03:01 and DQB1*02:01 had 4 times the odds of other patients of having an OD value exceeding 1.5. Patients having both alleles constituted 44.7% of all patients whose OD values exceeded 1.5 (17 of 38); the baseline frequency for having both alleles was 22.3% (92 of 412).
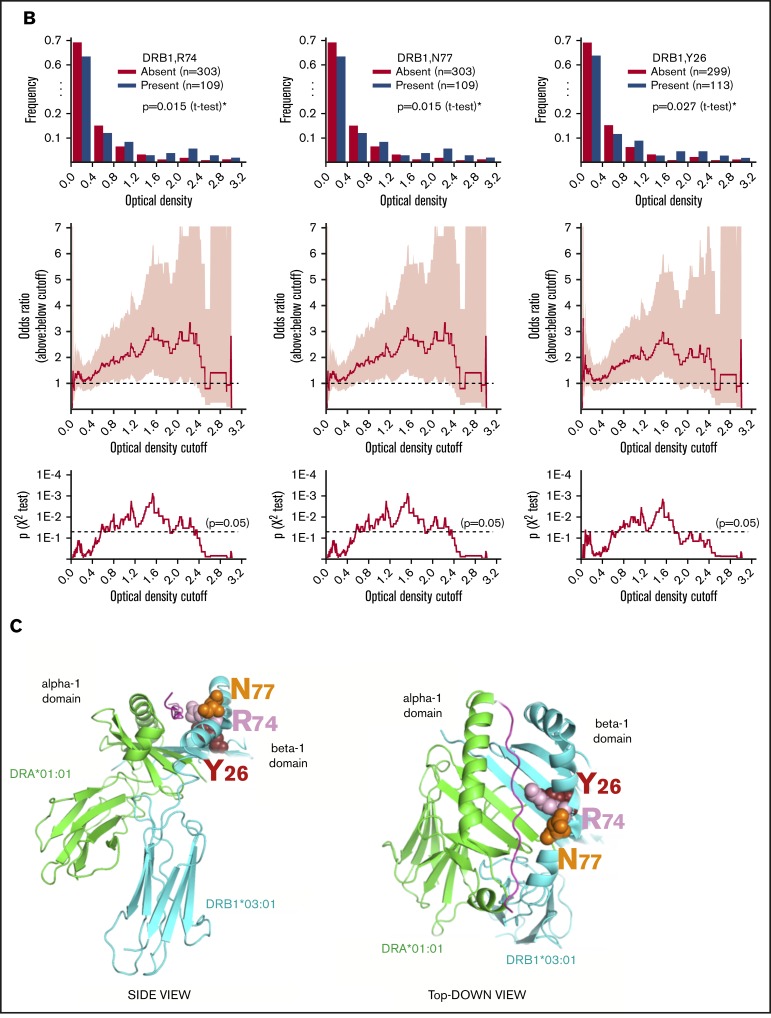
Figure 2.
Association between HLA and anti-PF4/H antibody levels. (A) HLA allele associations: top row, distribution of OD values; middle row, odds ratio for having an OD value above vs below a given cutoff; and bottom row, significance of association across all possible cutoffs (95% confidence intervals in pink). (B) HLA amino acid residue associations: top row, distribution of OD values; middle row, odds ratio for having an OD value above vs below a given cutoff; and bottom row, significance of association across all possible cutoffs (95% confidence intervals in pink). (C) Two views of candidate amino acid residues within DRB1 driving risk for anti-PF4/H antibody development (Protein Data Bank code: 1A6A). *Significance within a 5% false discovery rate.
Anti-PF4/H vs HLA amino acid residue
The top amino acid residue candidates for driving increased anti-PF4/H were R74, N77, and Y26, all within the peptide-binding groove of DRB1 (Figure 2B-C). Patients having these residues had higher OD values than those who did not (P = .015-.027; Figure 2B top row). These patients had 3 times the odds of other patients of having an OD value exceeding 1.5 (Figure 2B middle and bottom rows). Patients having all 3 residues constituted 47.4% of all patients whose OD values exceeded 1.5 (18 of 38); the baseline frequency was 26.4% (109 of 412).
Discussion
We investigated immunogenetic risk for elevated anti-PF4/H, which ultimately causes clinical HIT in a subset of patients, by the hypothesis that HLA-restricted aberrant antigen presentation precedes production of anti-PF4/H. Our end point was ELISA anti-PF4/H level. Other end points such as serotonin release assay or clinical HIT with thrombosis, despite their importance, require additional elements (eg, platelet-related factors) to manifest. Due to a lack of uniformly accepted OD value cutoff for positivity,15 we characterized the complete OD value distribution and examined all possible cutoffs. We found that DRB1*03:01 and DQB1*02:01 were significant risk factors for increased anti-PF4/H antibodies following heparin exposure among inpatients.
Earlier studies generated inconsistent findings of association between HLA and anti-PF4/H.16-18 These studies were limited by the typing methodology at the time, providing low-resolution16,17 or inferred18 typing only. One study also used healthy individuals without known heparin exposure as controls.16 Our results corroborate the finding of DR3-HIT antibody association from Paparella et al,17 extending their conclusions from cardiovascular surgical patients to general inpatients. Notably, our study used high-resolution HLA typing to enable prediction of risk-carrying residues within the peptide-binding groove of DRB1, providing a basis for future investigations into which peptides may cause disease.
The DRB1*03:01-DQB1*02:01 haplotype has been associated with multiple autoimmune disorders, including celiac disease,19 type 1 diabetes,20 and systemic lupus erythematosus.21 HIT may share similar pathogenesis with these disorders via aberrant antigen presentation by DRB1*03:01 and/or DQB1*02:01. One of the DRB1 amino acid residues associated with increased anti-PF4/H (Y26) has been implicated in type 1 diabetes and autoimmune thyroid disease.22 In patients with celiac disease, altered gut microbiota23 or defective intestinal barriers may also prime an anti-PF4/H response given the observed connection between bacteria and HIT antibodies.24 Presence of a shared susceptibility to these autoimmune disorders and elevated anti-PF4/H antibodies could signal an increased pretest probability for HIT in thrombocytopenic heparin-exposed patients having a known history of autoimmunity.
Our study is limited by sampling from a single institution without a replication cohort. Dosages, durations, and indications for heparin, as well as patient histories including the presence of autoimmune disease, could not be reliably ascertained for the study. We also examined only DRB1 and DQB1 in order to balance investigating the most functionally relevant class II loci with minimizing redundant or multiple testing (for example, DRB3/4/5 were omitted due to well-established tight genetic linkage with DRB1-DQB1), and therefore cannot rule out the contribution of other HLA loci or other genetically linked genes in the HLA region that may affect anti-PF4/H production. Finally, an immunoglobulin G–specific ELISA may have been better suited for this study compared with the poly-specific assay available at our institution, although high values from either assay correlate well with HIT. Future multidisciplinary studies are warranted to further understand the functional relationship between HLA and anti-PF4/H antibodies.
Acknowledgments
The authors thank DKMS Life Science Laboratory GmbH for performing Illumina-based HLA typing, and Rhonda Porche-Sorbet for technical assistance.
This work was partly supported by the Washington University in St. Louis Hematology Scholars K12 award (K12-HL087107-07 from the National Institutes of Health, National Heart, Lung, and Blood Institute) (C.L.).
Authorship
Contribution: R.Z. analyzed data and composed the manuscript; B.F.D. handled specimens and extracted DNA; V.L. performed HLA typing; C.S.E. designed the study and composed the manuscript; and C.L. designed the study, procured specimens, analyzed data, and composed the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Charles S. Eby, Division of Laboratory and Genomic Medicine, Department of Pathology and Immunology, and Division of Hematology, Department of Medicine, School of Medicine, Washington University in St. Louis, 660 South Euclid Ave, Campus Box 8118, St. Louis, MO 63110; e-mail: eby@wustl.edu; and Chang Liu, Division of Laboratory and Genomic Medicine, Department of Pathology and Immunology, School of Medicine, Washington University in St. Louis, 660 South Euclid Ave, Campus Box 8118, St. Louis, MO 63110; e-mail: cliu32@wustl.edu.
References
- 1.Pishko AM, Cuker A. Heparin-induced thrombocytopenia in cardiac surgery patients. Semin Thromb Hemost. 2017;43(7):691-698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Greinacher A. Heparin-induced thrombocytopenia. N Engl J Med. 2015;373(19):1883-1884. [DOI] [PubMed] [Google Scholar]
- 3.Warkentin TE, Levine MN, Hirsh J, et al. . Heparin-induced thrombocytopenia in patients treated with low-molecular-weight heparin or unfractionated heparin. N Engl J Med. 1995;332(20):1330-1335. [DOI] [PubMed] [Google Scholar]
- 4.Raschke RA, Curry SC, Warkentin TE, Gerkin RD. Improving clinical interpretation of the anti-platelet factor 4/heparin enzyme-linked immunosorbent assay for the diagnosis of heparin-induced thrombocytopenia through the use of receiver operating characteristic analysis, stratum-specific likelihood ratios, and Bayes theorem. Chest. 2013;144(4):1269-1275. [DOI] [PubMed] [Google Scholar]
- 5.Chan CM, Woods CJ, Warkentin TE, Sheppard JI, Shorr AF. The role for optical density in heparin-induced thrombocytopenia: a cohort study. Chest. 2015;148(1):55-61. [DOI] [PubMed] [Google Scholar]
- 6.Warkentin TE, Greinacher A, Gruel Y, Aster RH, Chong BH; Scientific and Standardization Committee of the International Society on Thrombosis and Haemostasis . Laboratory testing for heparin-induced thrombocytopenia: a conceptual framework and implications for diagnosis. J Thromb Haemost. 2011;9(12):2498-2500. [DOI] [PubMed] [Google Scholar]
- 7.Baroletti S, Hurwitz S, Conti NA, Fanikos J, Piazza G, Goldhaber SZ. Thrombosis in suspected heparin-induced thrombocytopenia occurs more often with high antibody levels. Am J Med. 2012;125(1):44-49. [DOI] [PubMed] [Google Scholar]
- 8.Paul AK, Fricke W, Kouides PA. A threshold optical density value in immunoassay predicts thrombosis in patients with heparin induced thrombocytopenia [abstract]. Blood. 2013;122(21). Abstract 4755. [Google Scholar]
- 9.Pearson MA, Nadeau C, Blais N. Correlation of ELISA optical density with clinical diagnosis of heparin-induced thrombocytopenia: a retrospective study of 104 patients with positive anti-PF4/heparin ELISA. Clin Appl Thromb Hemost. 2014;20(4):349-354. [DOI] [PubMed] [Google Scholar]
- 10.Warkentin T, Greinacher A. Heparin-Induced Thrombocytopenia. 4th ed. Boca Raton, FL: Taylor & Francis; 2007160. [Google Scholar]
- 11.Bacsi S, Geoffrey R, Visentin G, De Palma R, Aster R, Gorski J. Identification of T cells responding to a self-protein modified by an external agent. Hum Immunol. 2001;62(2):113-124. [DOI] [PubMed] [Google Scholar]
- 12.Zheng Y, Yu M, Padmanabhan A, et al. . Critical role of CD4 T cells in PF4/heparin antibody production in mice. Blood. 2015;125(11):1826-1829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lange V, Böhme I, Hofmann J, et al. . Cost-efficient high-throughput HLA typing by MiSeq amplicon sequencing. BMC Genomics. 2014;15(1):63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schöfl G, Lang K, Quenzel P, et al. . 2.7 million samples genotyped for HLA by next generation sequencing: lessons learned. BMC Genomics. 2017;18(1):161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rice L. There is no such thing as a “positive” antibody test: diagnosing heparin-induced thrombocytopenia in 2015. Chest. 2015;148(1):1-3. [DOI] [PubMed] [Google Scholar]
- 16.Greinacher A, Mueller-Eckhardt G. Heparin-associated thrombocytopenia: no association of immune response with HLA. Vox Sang. 1993;65(2):151-153. [DOI] [PubMed] [Google Scholar]
- 17.Paparella D, Micelli M, Favoino B, D’Alò M, Fiore T, de Luca Tupputi Schinosa L. Anti-heparin-platelet factor 4 antibodies after cardiopulmonary bypass: role of HLA expression. Haematologica. 2001;86(3):326-327. [PubMed] [Google Scholar]
- 18.Karnes JH, Cronin RM, Rollin J, et al. . A genome-wide association study of heparin-induced thrombocytopenia using an electronic medical record. Thromb Haemost. 2015;113(4):772-781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rubio-Tapia A, Abdulkarim AS, Wiesner RH, Moore SB, Krause PK, Murray JA. Celiac disease autoantibodies in severe autoimmune liver disease and the effect of liver transplantation. Liver Int. 2008;28(4):467-476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cheong KY, Allcock RJ, Eerligh P, et al. . Localization of central MHC genes influencing type I diabetes. Hum Immunol. 2001;62(12):1363-1370. [DOI] [PubMed] [Google Scholar]
- 21.Parks CG, Pandey JP, Dooley MA, et al. . Genetic polymorphisms in tumor necrosis factor (TNF)-α and TNF-β in a population-based study of systemic lupus erythematosus: associations and interaction with the interleukin-1α-889 C/T polymorphism [published correction appears in Hum Immunol. 2005;66(3):331]. Hum Immunol. 2004;65(6):622-631. [DOI] [PubMed] [Google Scholar]
- 22.Menconi F, Osman R, Monti MC, Greenberg DA, Concepcion ES, Tomer Y. Shared molecular amino acid signature in the HLA-DR peptide binding pocket predisposes to both autoimmune diabetes and thyroiditis. Proc Natl Acad Sci USA. 2010;107(39):16899-16903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wacklin P, Laurikka P, Lindfors K, et al. . Altered duodenal microbiota composition in celiac disease patients suffering from persistent symptoms on a long-term gluten-free diet. Am J Gastroenterol. 2014;109(12):1933-1941. [DOI] [PubMed] [Google Scholar]
- 24.Krauel K, Pötschke C, Weber C, et al. . Platelet factor 4 binds to bacteria, [corrected] inducing antibodies cross-reacting with the major antigen in heparin-induced thrombocytopenia [published correction appears in Blood. 2011;117(21):5783]. Blood. 2011;117(4):1370-1378. [DOI] [PubMed] [Google Scholar]