Summary
Background
The high prevalence of actinic keratosis (AK) requires the optimal use of healthcare resources.
Objectives
To gain insight in to the healthcare utilization of people with AK in a population‐based cohort, and the management of AK in a primary and secondary care setting.
Methods
A retrospective cohort study using three complementary data sources was conducted to describe the use of care, diagnosis, treatment and follow‐up of patients with AK in the Netherlands. Data sources consisted of a population‐based cohort study (Rotterdam Study), routine general practitioner (GP) records (Integrated Primary Care Information) and nationwide claims data (DRG Information System).
Results
In the population‐based cohort (Rotterdam Study), 69% (918 of 1322) of participants diagnosed with AK during a skin‐screening visit had no previous AK‐related visit in their GP record. This proportion was 50% for participants with extensive AK (i.e. ≥ 10 AKs; n = 270). Cryotherapy was the most used AK treatment by both GPs (78%) and dermatologists (41–56%). Topical agents were the second most used treatment by dermatologists (13–21%) but were rarely applied in primary care (2%). During the first AK‐related GP visit, 31% (171 of 554) were referred to a dermatologist, and the likelihood of being referred was comparable between low‐ and high‐risk patients, which is inconsistent with the Dutch general practitioner guidelines for ‘suspicious skin lesions’ from 2017. Annually, 40 000 new claims representing 13% of all dermatology claims were labelled as cutaneous premalignancy. Extensive follow‐up rates (56%) in secondary care were registered, while only 18% received a claim for a subsequent cutaneous malignancy in 5 years.
Conclusions
AK management seems to diverge from guidelines in both primary and secondary care. Underutilization of field treatments, inappropriate treatments and high referral rates without proper risk stratification in primary care, combined with extensive follow‐up in secondary care result in the inefficient use of healthcare resources and overburdening in secondary care. Efforts directed to better risk differentiation and guideline adherence may prove useful in increasing the efficiency in AK management.
What's already known about this topic?
The prevalence of actinic keratosis (AK) is high and, in particular, multiple AKs are a strong skin cancer predictor.
The high prevalence of AK requires optimal use of healthcare resources.
Nevertheless, (population based) AK healthcare utilization and management data are very rare.
What does this study add?
Although AK‐related care already consumes substantial resources, about 70% of the AK population has never received care.
Primary care AK management demonstrated underutilization of topical therapies and high referral rates without proper risk stratification, while in secondary care the extensive follow‐up schedules were applied.
This inefficient use of healthcare resources highlights the need for better harmonization and risk stratification to increase the efficiency of AK care.
Short abstract
Linked Comment: https://doi.org/10.1111/bjd.17862.
https://doi.org/10.1111/bjd.18269 available online
Actinic keratoses (AKs) are erythematous, asymptomatic keratotic lesions that usually develop in the second phase of life, and occur predominately in chronic ultraviolet‐exposed skin of light‐skinned individuals.1, 2 The prevalence of AKs is high: in population‐based data from the Rotterdam Study (RS) and the Australian Skin Cancer Cohort it has been estimated that 24% (the Netherlands) to 60% (Australia) of people older than 50 years have at least one AK.3, 4 The likelihood of an individual lesion to progress to squamous cell carcinoma (SCC) is < 1% per year.5 However, patients often have multiple AKs indicating cutaneous field dysplasia, which substantially increases their risk of developing skin cancer, mostly SCC and basal cell carcinoma (BCC). Although these tumours account for only a few cancer‐related deaths,3, 6 premalignant and malignant skin cancers consume substantial health resources and have an impact on the quality of life.7
Despite the high impact of AK‐related care, there is a lack of empirical evidence on the management of AK. The reasons for this are that patients do not necessarily seek care for asymptomatic AK, AK is often a clinical diagnosis and thus not captured in the pathology and cancer registries, and patients can be managed in both primary and secondary care. A single data source is therefore not sufficient to capture the complete healthcare utilization pathway of this group. A previous study by Kirby et al. showed a variation in costs for the management of AK within and between regions, which could not be fully explained by patient characteristics, and advocated to identify the care pathways of patients with AK.8 The objective of this study was to provide insight in to the management of AKs by describing the healthcare utilization of people with AK in a population‐based cohort and in the primary care and secondary care settings.
Patients and methods
Study design
To study AK management, a retrospective, multiple database, descriptive cohort study of population‐based data and routine data of people with AK was conducted (Fig. 1).
Figure 1.
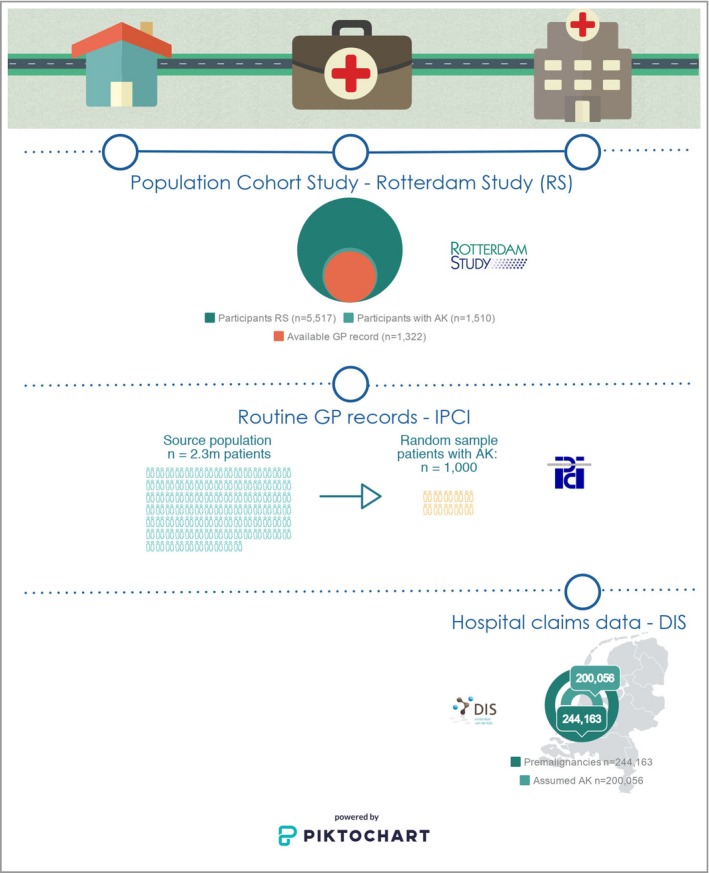
This research was conducted using three complementary databases and shows a visual record of the position in health care of the data collection of each data source for this research. AK, actinic keratosis; DIS, DRG Information System; GP, general practitioner; IPCI, Integrated Primary Care Information.
Data sources and study population
Population‐based cohort: Rotterdam Study
The RS is an ongoing population‐based cohort study of nearly 15 000 participants aged 45 years and older from a suburb in Rotterdam in the Netherlands.9 Between August 2010 and November 2015, 5517 participants received a full‐body skin examination (FBSE) by dermatologically trained physicians. Standardized forms were used to document the most common skin diseases, including AK and categorizing the total body count into 0, 1–3, 4–9 and ≥ 10 lesions. General practitioner (GP) records before the RS screening visit of participants with AK were manually screened for the presence of previous AK diagnoses (clinical diagnosis by GP or dermatologist, or histologically confirmed), treatments and AK‐related follow‐up visits. As participants with extensive AK were advised to consult their GP, which may have changed their healthcare consumption, only records before the screening visit were evaluated (Fig. 2). To assess the total health impact, RS was used to evaluate the management during all AK‐related visits, instead of differentiating between initial and follow‐up visit. Subsequent keratinocyte cancer (KC) development was obtained by linkage of all RS participants with the Dutch Pathology Registry (PALGA), the nationwide registry of histo‐ and cytopathology in the Netherlands (Data S1; see Supporting Information).10, 11
Figure 2.
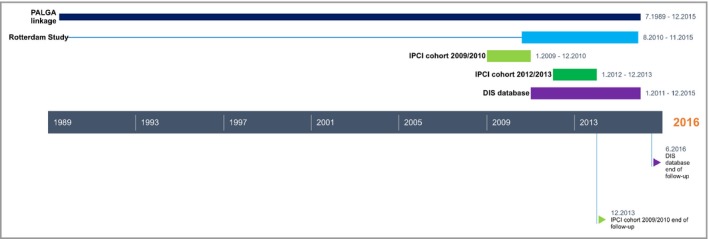
Each data source had a slightly different period of data collection. The figure shows the data‐collection timeline of each data source. DIS, DRG Information System; FBSE, full‐body skin examination; GP, general practitioner; IPCI, Integrated Primary Care Information; PALGA, the Dutch Pathology Registry.
Routine general practitioner records: Integrated Primary Care Information database
Integrated Primary Care Information (IPCI) is a central research database with a collection of 2·3 million electronic routine patients records from 265 GP practices in the Netherlands since 1989.12 To capture both long‐term follow‐up and recent common practice, a random sample of 1000 patients diagnosed with AK was selected based on a free text algorithm equally divided over 2009/2010 and 2012/2013 (Data S1; see Supporting Information). Patients were eligible if the GP mentioned AK in the differential diagnosis, AK was confirmed in a histopathological report or AK diagnosis was confirmed by a medical specialist. For eligible patients, the treatment at first GP encounter was extracted, and for those with non‐AK‐specific treatments, such as antibiotics, treatment during the second consultation was included. For the cohort 2009/2010, the frequency of documented BCC and SCC during the remaining follow‐up period was assessed.
Nationwide hospital claims: DRG Information System database
Outpatient care for patients with AK was further evaluated using the national healthcare insurance data from the DRG Information System (DIS). To obtain a perspective on the scope of the problem, data were extracted from opendisdata.nl, which is an openly accessible source on healthcare insurance data.13 Health insurance is compulsory for all Dutch residents, and all activities related to diagnosing or treating patients are recorded into a DRG package, which results in a healthcare claim.14 The nationwide DIS database receives and manages information on healthcare claims but does not contain personal data. Patients with a dermatologist‐based healthcare claim for a cutaneous premalignancy (code 017) between 2011 and 2015 without previous cutaneous malignancies (code 014) were included. Data were obtained on registered treatments, follow‐up visits and potential subsequent claims for cutaneous malignancies. As a claim for a ‘cutaneous premalignancy’ can also include other cutaneous premalignancies, an algorithm was developed to identify patients with AK based on healthcare procedures. This algorithm was validated with local (i.e. Erasmus University Medical Center, Rotterdam) patient records resulting in a positive predictive value of 93% (Data S1; see Supporting Information).
Statistical analysis
The primary objective was to describe current clinical practice and healthcare utilization. No hypothesis testing and sample‐size calculations were therefore performed. All available data from the RS and DIS were used. For the IPCI data, we considered that 1000 patients with AK was sufficient to describe current clinical practice and was feasible with regard to the time‐consuming manual review of medical records.
Complementing the descriptive analyses, we calculated the relative risk and the 95% confidence interval (CI) for subsequent KC risk among RS participants. The χ2‐test was used to evaluate the significance level (P = 0·05) between proportions for several values among different AK severity categories.
The analyses were performed using SPSS 21·0 statistical software (IBM Corp., Armonk, NY, U.S.A.) and SAS 9·3 statistical software (SAS Institute Inc., Cary, NC, U.S.A.). The STROBE and RECORD statements were used for reporting the descriptive analyses.15, 16
Results
Population‐based cohort: Rotterdam Study
Of the 5517 individuals from the RS who underwent an FBSE, 1510 (27%) were diagnosed with AK. The primary care record was available in 1322 of 1510 participants (87·6%); 55% were male and the mean ± SD age was 61 ± 5 years (Table 1).
Table 1.
Characteristics of the skin screened sample from the population‐based cohort (RS) and a random sample of patients with AK from the GPs database (IPCI)
| Routine GP records (IPCI) | RS | ||
|---|---|---|---|
| N | 1000 | 1322 | |
| Male, n (%) | 471 (47) | 723 (55) | |
| Age, mean ± SD | 69 ± 12 | 61 ± 5 | |
| Number of AK, n (%) | Described by GPa,b | Counted during FBSE | Described by GP during 455 visitsa |
| 1–3 | 528 (53) | 724 (55) | 117 (26) |
| 4–9 | 27 (3) | 328 (25) | 5 (1) |
| > 10 | 2 (0·2) | 270 (20) | 0 (0) |
| Present, without absolute numbers | 412 (41) | 0 (0) | 333 (73) |
| History of cutaneous keratinocyte carcinoma, n (%) | 325 (25) | ||
| Basal cell carcinoma | 53 (5) | 271 (20) | |
| Squamous cell carcinoma | 23 (2) | 69 (5) | |
Basic characteristics of patients included in hospital claims data are not available as patient characteristics are not recorded in claims data on a nationwide level. AK, actinic keratosis; FBSE, full‐body skin examination; GP, general practitioner; IPCI, Integrated Primary Care Information; RS, Rotterdam Study. aBased on routine GP care, where FBSE is usually not conducted and the number of AK is usually not explicitly stated in GP records. bTotal number does not add up to 1000 as 31 patients ultimately did not have AK.
Diagnosis
Of the 1322 participants with AK and a primary care record, 55% had one to three AKs, 25% had four to nine AKs and 20% had ≥ 10 AKs (Table 1). The retrospective GP record review of this population‐based AK cohort, showed that 918 (69%) participants had never visited a healthcare provider for their AK before the FBSE (Table 2). Although this decreased slightly with the number of AKs, 50% of those with ≥ 10 AKs had never consulted a physician for AK. No substantial differences in likelihood of having consulted a physician for AKs were observed across age categories and gender (Data S1 tables; see Supporting Information).
Table 2.
Likelihood of actinic keratosis (AK) diagnosis in routine care among participants with AK detected by skin screening in a population‐based cohort study (Rotterdam Study, RS)
| Number of AK diagnosed during RS FBSE | Total | |||
|---|---|---|---|---|
| 1–3 AK | 4–9 AK | ≥ 10 AK | ||
| AK detection in skin screening, n | 724 | 328 | 270 | 1322 |
| No routine care based prior AK diagnosis, n (%) | 556 (77) | 226 (69) | 136 (50) | 918 (69) |
| Previous routine care based AK diagnosis, n (%) | 168 (23) | 102 (31) | 134 (50) | 404 (31) |
| Diagnosis by GP, n (%) | 68 (40) | 45 (44) | 40 (30) | 153 (38) |
| Diagnosis by dermatologist,a n (%) | 60 (36) | 30 (29) | 48 (36) | 138 (34) |
| Diagnosis by both GP and dermatologist, n (%) | 40 (24) | 27 (26) | 46 (34) | 113 (28) |
FBSE, full‐body skin examination; GP, general practitioner. aAs derived from GP records. If dermatologist correspondence does not state AK, diagnosis is classified as AK according to the differential diagnosis of the GP.
Treatment
Of the 1322 participants, 266 (20%) had a previous AK‐related GP consultation, with 455 visits. No active AK‐focused treatment was described in the GP record in 19% of AK‐related visits (85 of 455), and in 16% (n = 74) of all first and subsequent visits the patients were referred to secondary care (Table 3). Among those with ≥ 10 AKs, the odds of being referred to a specialist during the first AK‐related GP visit were not significantly different from those with one to three AKs (19 of 86 vs. 20 of 108; odds ratio 1·2, 95% CI 0·62–2·52, P = 0·54).
Table 3.
Distribution of treatment modalities for actinic keratosis (AK) by general practitioners (GPs) and dermatologists using three different datasets
| Treatment by GP | Treatment by dermatologist | |||
|---|---|---|---|---|
| Routine GP records (IPCI) | RS | RS | Hospital claims data (DIS) | |
| GP records, first AK visit | GP records, all AK‐related visits | Dermatologist correspondence, all AK‐related visits | Claims for cutaneous premalignancies, first AK‐related visit | |
| Patients, n | 554a | 266b | 251b | 200 056 |
| Visits, n | 554 | 455 | 422 | 200 056 |
| No treatment (incl. no referral), n (%) | 42 (8) | 85 (19) | 52 (12) | 44 262 (22) |
| Referral, n (%) | 171 (31) | 67 (15) | N/A | N/A |
| Treatment by GP, n (%) | 341 (62) | 297 (65) | N/A | N/A |
| Treatment and subsequent referral | 41 (7) | 7 (2) | – | – |
| Treatment by GP only | 300 (54) | 290 (64) | – | – |
| Missing, n (%) | 0 (0) | 6 (1) | 6 (1) | 0 (0) |
| Type of treatment, n (%) | 341 (62) | 297 (65)c | 364 (86)c | 155 794 (78)d |
| Cryotherapy | 251 (74) | 239 (78) | 203 (56) | 64 047 (41) |
| Topical treatment of AKe | 23 (7) | 7 (2) | 76 (21) | 20 908 (13) |
| Photodynamic therapy | – | – | 19 (5) | 3150 (2) |
| Surgical | 28 (8) | 12 (4) | 43 (12) | 26 324 (17) |
| Other medical treatment of AKf | 38 (11) | 42 (14) | 22 (6) | 981 (1) |
| Otherg | 1 (0·3) | 5 (2) | 1 (0·3) | 40 384 (26) |
Different datasets are not comparable. When methyl aminolaevulinate cream is mentioned, this is not scored since the only indication for this treatment is as a primer for photodynamic therapy. DIS, DRG Information System; IPCI, Integrated Primary Care Information; N/A, not applicable; RS, Rotterdam Study.
aIn 554 of the 1000 patients included from the IPCI GP database, AK was in the differential diagnosis of the GP. bOf the 1322 participants screened in the RS, 266 had an AK‐related visit at the GP and 251 at the dermatologist. cTotal numbers add up to > 100% as patients may have received multiple treatments for their AK(s). dFor each AK‐related visit only the most invasive treatment was scored. eRelevant treatment of AK: 5‐fluorouracil, imiquimod and ingenol mebutate gel. For the hospital claims data this was only registered if patient picked up their prescribed treatment within 7 days after the outpatient clinic visit. fIncluded in other medical treatment of AK: nontopical treatment, tretinoin, salicylic acid, ureum, lanette, fucidine, cetomacrogol, diclofenac, antimycotic, antibacterial. gOther treatments are: laser, coagulation, unknown.
Patients were treated by a GP in 297 of the 455 AK‐related visits (65%), at which cryotherapy was mostly applied (78%, 239 of 297). Among patients only seen by the GP, the proportion of visits during which cryotherapy was applied increased significantly with the number of AKs (52% in one to three AKs to 68% in ≥ 10 AKs, P = 0·04; Data S1 tables; see Supporting Information). In 2% of the 297 AK visits during which a treatment was given by the GP, a topical AK therapy was prescribed, while other treatments unrelated to AK (e.g. antibacterial ointments) were prescribed in 14% of visits.
Of the 1322 patients with AK, 251 had at least one previous dermatology visit with 422 visits (Table 3). No treatment was given during 52 (12%) visits and in 364 of 422 (86%) of all visits the patient was treated by the dermatologist; in the remaining six visits information was missing. Cryotherapy was the most used treatment (56%, 203 of 364), followed by field treatment (26%), of which photodynamic therapy was used during 19 visits. For patients treated by the dermatologist the proportion of visits during which the field treatment was selected increased significantly with the number of AKs (20% in one to three AKs to 32% in ≥ 10 AKs, P = 0·02; Data S1 tables; see Supporting Information).
Follow‐up
Of the 266 individuals with AK seen by the GP, 166 patients (62%) had no second visit for AK recorded over a median follow‐up time of 2·8 years (Table 4); although this group also contains patients referred to the dermatologist. The remaining 100 patients had 189 subsequent visits for AK, 24% of follow‐up visits were within 3 months after the initial treatment and 22% in the year following the first GP visit. Among 1322 RS cohort participants with AK, a BCC was recorded in PALGA among 7% (n = 88) and an SCC in 4% (n = 50) of participants during a median follow‐up period of 2·8 years (interquartile range 1·3–4·4). The risk of any KC (i.e. not AK‐lesion specific) increased from 9% (65 of 724) for individuals with one to three AKs to 16% (43 of 270) for those with ≥ 10 AKs. The relative risk of developing a histologically confirmed KC was 3·0 (95% CI 2·4–3·9) for the group with AK compared with those without AK in the RS (111 of 1322 vs. 116 of 4193).
Table 4.
Actinic keratosis (AK)‐related healthcare visits and subsequent (pre)malignancies among patients with AK
| Database | GP records | Dermatologist records | |
|---|---|---|---|
| Routine GP records (IPCI) | Rotterdam Study | Claims data (DIS) | |
| Patients, n | 486d | 266 | 200 056 |
| Follow‐up time (years) | Median 5·6, IQR 5·1–6·2 | Median 2·8, IQR 1·3–4·4 | Up to 5 yearse |
| Follow‐up | |||
| Number of AK‐related follow‐up visits | |||
| 0 | 149 (31) | 166 (62) | 87 302 (44) |
| ≥ 1 | 337 (69)a | 100 (38) | 112 754 (56) |
| Visits per period, n (%) | N/A | 189 visits in 100 patients | 317 642 visits in 112 754 patients |
| <3 months | – | 46 (24) | 101 382 (32) |
| 3–12 months | – | 42 (22) | 86 766 (27) |
| > 12 months | – | 94 (50) | 129 494 (41) |
| Unknown | – | 7 (4) | 0 (0) |
| Cutaneous lesions | |||
| Subsequent cutaneous malignancy, n (%) | 138 (10) of 1322b | 19 178 (11)c | |
| Basal cell carcinoma | 72 (15) | 88 (7) | N/A |
| Squamous cell carcinoma | 36 (7) | 50 (4) | N/A |
DIS, DRG Information System; GP, general practitioner; IPCI, Integrated Primary Care Information; IQR, interquartile range; N/A, not applicable. a486 patients with confirmed AK in the cohort 2009/2010. bAll patients were followed up to mid‐2016, independent of the year of initial treatment. cTotal of patients with one or more skin cancer related GP visits (not AK specific). dCases were identified using linkage with the Dutch Pathology Registry (PALGA) in the period from the date of skin screening based AK diagnosis until the end of 2015. Median follow‐up period for this group is 3·7 (IQR 1·3–4·6). eIncludes patients with a subsequent claim for diagnostic code 0017 for cutaneous malignancy, including basal cell carcinoma, squamous cell carcinoma, (lentigo maligna) melanoma, lymphoma, cutaneous metastatic disease and other cutaneous malignancies; no further differentiation available. Only the first claim for cutaneous malignancy could be extracted.
Routine general practitioner records: Integrated Primary Care Information database
Diagnosis
Among the 1000 randomly selected eligible patients who mentioned AK for the first time in the patient record, 47% (n = 471) were men and the mean ± SD age was 69 ± 12 years (Table 1). Among these 1000 patients, 400 were included based on correspondence from dermatologists in the GP record and were not seen by the GP for AK during the preceding year. The remaining 600 patients had a GP visit including an AK diagnosis, of which AK Was in the differential diagnosis by GPs in 554 cases. In 97%, AKs were clinically diagnosed and 3% were confirmed by histology.
Treatment
Over 60% (n = 341) of the 554 patients with AK in the differential diagnosis were treated by their GP, predominantly with cryotherapy (251 of 341, 74%; Table 3), followed by surgery (8%) and topical treatment (7%). Other medical treatments (e.g. antibacterial ointments) were prescribed by GPs in 11% (n = 38) of patients with the first mention of AK in their record. In 8% (42 of 554) the GP recorded an AK and did not describe any further treatment or referral suggesting a wait‐and‐see policy. One‐third (171 of 554) of patients with AK were referred to the dermatologist at the time of the first clinical diagnosis.
Follow‐up
During a median follow‐up of 5·6 years of 486 patients with a confirmed AK in the 2009/2010 cohort, 69% had a second GP visit related to cutaneous (pre)malignancies (not AK specific; Table 4). Subsequent BCCs were recorded among 72 patients (15%) and SCCs among 36 of the 486 patients (7%).
Among the 38 patients who initially received treatments not indicated for AK, four subsequently received cryotherapy, four again received treatments not indicated for AK and 30 received no further treatment during follow‐up.
Nationwide hospital claims: DRG Information System
Using open source data, 98 435 (13%) of the 768 770 dermatology‐related claims in 2015 were due to cutaneous premalignancies, including AK. Between 2011 and 2015, 200 056 claims of incidental patients with AK without a previous cutaneous malignancy were identified (Data S1; see Supporting Information).
Treatment
In 22% (44 262 of 200 056) of the first AK‐related visits, no treatment was registered. Of the 155 794 claims that included a treatment, 41% involved cryotherapy, 13% topical AK treatment, 2% photodynamic therapy, 17% a surgical procedure (i.e. biopsy or excision) and 26% coagulation or laser therapy (Table 3).
Follow‐up
All 200 056 patients with AK were followed until 31 December 2015, with 517 698 dermatology outpatient clinic visits. Fifty‐six per cent of the 200 056 patients had at least one dermatology follow‐up visit, with a total of 317 642 visits (Table 4). Almost two‐thirds of the follow‐up visits were in the first year after initial treatment, with an average of 1·8 visits per patient. Thirteen per cent of the 317 642 follow‐up visits included a surgical procedure and 17% cryotherapy.
In the cohort with an initial claim for AK in 2011 (n = 46 415), and thus with the most extended follow‐up time of 5 years, 18% (n = 8390) of the patients had a subsequent claim for a cutaneous malignancy.
Discussion
Although AK is a common skin condition that accounts for at least 10% of all dermatological visits, a substantial proportion of the general population seems unaware of having AK. In both primary and secondary care, cryotherapy was most commonly used. Field therapy was the second option for dermatologists, while GPs only rarely applied these topical therapies. The number of AKs only modestly increased the likelihood of having an AK‐related GP consultation, while it did not affect the risk of being referred to secondary care. Follow‐up schedules seem to be extensive in secondary care.
This study shows that half of the people with ≥ 10 AKs in the population‐based cohort had no previous consultation. As GP consultations are mostly patient driven, it is most likely the result of patients being unaware of having AKs and the potential increased risk to develop KC. Limited awareness in the general population implies the potential of underdiagnosis and undertreatment of AK. Although not all AKs warrant treatment, this does raise concerns with extensive AK (i.e. multiple AKs or field change).2 As a clinical biomarker of extensive ultraviolet exposure, we have demonstrated that the number of AKs correlates with an increased risk of KC, which may contribute to the growing burden of KC.2, 3, 17, 18 Therefore, appropriate awareness about AK and its treatment, particularly for patients with ≥ 10 AKs, is important for both the general population and GPs, which is also advocated by the US Preventative Services Task Force.5, 19, 20, 21 As AKs are often located on visible skin sites such as the face and scalp, GPs may have an important role in increasing the awareness of AKs.3, 19, 22 Unfortunately, from our data we were unable to estimate the extent to which the AKs have been noted by GPs. However, it may be questioned if GPs being proactive about AKs is feasible, as patients are already bringing multiple problems to the brief consultations with the GP; therefore, a low‐risk condition such as AK may not be of the highest priority for either the patient or the GP.23, 24, 25
Relatively recently (June 2017) the first Dutch GP guidelines for ‘suspicious skin lesions’ were published, while secondary care AK‐specific guidelines have been available since 2010.19, 26, 27 This might have affected different (awareness and) management of AK between primary and secondary care. Cryotherapy was the main treatment modality used by GPs, and interestingly the number of cryotherapy treatments significantly increased with more extensive AK. The recently introduced GP guidelines recommend cryotherapy for five or fewer AKs, which is comparable with international guidelines.2, 19, 28, 29, 30 The limited treatment modalities used by GPs may be a reflection of limited familiarity of GPs with different treatment modalities for AK, possibly because of the undersupply of dermatology training in both GP specialist training and continuing medical education programmes in many countries.31, 32, 33, 34, 35, 36, 37, 38, 39, 40 Effective and successful implementation of the primary care guidelines has the potential to fill this educational gap in the short term, and may result in the decreased use of nonindicated treatments (such as antibiotics) and structuring the use of suitable treatments by GPs. However, without proper dermatology training for GPs, clinical guidelines are not sufficient to improve patient care.41 Sufficient education, time and resources are pivotal for the successful management of AK in primary care.
A substantial proportion of patients with AK were referred to the dermatologists (38% at the first encounter in primary care), which was unrelated to the extent of AK. The group of patients solely referred for AK is already significant with 40 000 new patients being referred to the dermatologists per year within a population of 17 million inhabitants. However, this is still a substantial underestimation of the total AK load in secondary care as this excludes patients who also have cutaneous malignancies. Given these large numbers of patients with AK, AK being managed rather than cured, and overburdening in secondary care, both national and international guidelines support the concept that the majority of patients with AK could and should be managed in primary care.2, 19, 28, 29 Many countries including the Netherlands, have some level of gatekeeping in access to specialists, although the extent varies widely between countries.42, 43, 44, 45 However, with skin cancer GP education being side‐lined in both a national and an international perspective, successful AK management (and thus efficient gatekeeping) is compromised.32, 33, 34, 37, 38, 39, 46, 47 Increasing the familiarity of GPs with AK management by extending dermatology training for GPs may increase the likelihood of treating the condition themselves, reducing the use of nonindicated treatments (e.g. antibiotics) and limiting patients entering secondary care.19, 37, 40, 48, 49 Examples of the effect of additional training can be seen with dedicated and specialized GPs in Australia and the U.K., where they have a greater role in skin cancer management.50, 51, 52 In addition, further structuring of AK management, including explicit criteria for referral (e.g. AK not responding to treatment, AK in immunosuppressed patients, AK with the potential of SCC), may provide a substantive potential to lower the burden in secondary care.19, 53
In addition to efforts directed towards the general population and primary care, this study also identified potential areas for improvement in secondary care. Firstly, in the case of extensive AKs (i.e. n ≥ 10), field treatment is recommended in national and international guidelines.2, 27 However, these guidelines seem to be followed inconsistently, with only 32% of patients with extensive AK receiving field treatment (although significantly higher than in the group with mild AK). Secondly, the majority of patients with AK seen by the dermatologists had at least one follow‐up visit, whereas the guidelines recommend follow‐up in secondary care only for high‐risk patients (e.g. those with immunosuppression).2, 27 Comparable high follow‐up rates among patients with AK were observed in the U.K.52 These extensive follow‐up rates by dermatologists for what may be considered low‐risk care have the potential for overtreatment, and motives for this need to be explored.
A strength of this study is that multiple databases were analysed to obtain a comprehensive overview of AK‐related care, which has not been described before. The combination of a population‐based cohort and routine GP records is a unique way to identify patients with AK who never visited a GP or were not previously diagnosed in routine care, and to study the occurrence of KCs related to AK extensiveness. Furthermore, by combining primary care and secondary care databases, it provides a more comprehensive overview of the management of patients with AK throughout the care process.
A limitation of routinely collected healthcare data is related to what and how clinical data are recorded. An issue in GP databases was, for example, that clinical AK severity or explicit follow‐up recommendations are usually not recorded. Furthermore, it is possible that a patient visits the GP for a different (main) reason besides AK, which may result in lack of AK registration in the GP record. However, by using these different databases, the findings become more detailed and complementary. In healthcare claims data, it remains uncertain that the claimed care was actually administered. Diagnoses in claims data are less specific. Therefore, we may have included patients with other more rare cutaneous premalignancies (e.g. Bowen disease). This could have resulted in a greater amount of treatments less specific to AK, or higher follow‐up visit rates. However, an algorithm to identify these patients with AK showed a positive predictive value of up to 93%. Finally, some aspects may be specific to the Dutch healthcare system, and this may raise some concerns about the generalizability of our results. However, in many Western countries, primary care is the point of entry in the healthcare system for patients, and in many countries, some level of a gatekeeping system is applied.45, 52 Therefore, we believe that our observations could be applied to other countries as well. Regardless of the type of healthcare system, AK is a high‐volume condition and therefore comparable issues should be evaluated in other countries to improve the efficiency of care.
In conclusion, AKs are a high‐volume condition, with a significant healthcare impact, but with a seemingly limited familiarity with AK in the general population and possibly among GPs this may lead to the suboptimal use of healthcare resources. We identified areas in AK management that deviate from (both national and international) primary care and secondary care guideline recommendations. Adequate risk differentiation and improved guideline adherence in both primary and secondary care seem warranted to strengthen the vital role of GPs in AK management and to optimize the utilization of healthcare resources. To tailor the efforts needed, motives for AK management diverging from current guidelines among GPs and dermatologists need to be explored.
Supporting information
Data S1 Methods.
Acknowledgments
The participants of the Rotterdam Study are gratefully acknowledged, and the authors thank the research physicians for the data collection. We further thank the staff of PALGA, the Dutch Pathology Registry and Joris Verkouteren for his help with the record linkage. This research project was initiated and supported as part of the Project Sensible Care (in Dutch: Zinnige Zorg) by the Dutch National Health Care Institute.
Funding sources This study was funded by the National Health Care Institute for the Project Sensible Care (in Dutch: Zinnige Zorg) for patients with nonmelanoma skin cancer and actinic keratosis.
Conflicts of interest The authors received an institutional grant from the National Health Care Institute throughout the study.
https://doi.org/10.1111/bjd.18269 available online
References
- 1. Siegel JA, Korgavkar K, Weinstock MA. Current perspective on actinic keratosis: a review. Br J Dermatol 2017; 177:350–8. [DOI] [PubMed] [Google Scholar]
- 2. de Berker D, McGregor JM, Mohd Mustapa MF et al British Association of Dermatologists’ guidelines for the care of patients with actinic keratosis 2017. Br J Dermatol 2017; 176:20–43. [DOI] [PubMed] [Google Scholar]
- 3. Flohil SC, van der Leest RJ, Dowlatshahi EA et al Prevalence of actinic keratosis and its risk factors in the general population: the Rotterdam Study. J Invest Dermatol 2013; 133:1971–8. [DOI] [PubMed] [Google Scholar]
- 4. Frost CA, Green AC. Epidemiology of solar keratoses. Br J Dermatol 1994; 131:455–64. [DOI] [PubMed] [Google Scholar]
- 5. Werner RN, Sammain A, Erdmann R et al The natural history of actinic keratosis: a systematic review. Br J Dermatol 2013; 169:502–18. [DOI] [PubMed] [Google Scholar]
- 6. Hollestein LM, de Vries E, Nijsten T. Trends of cutaneous squamous cell carcinoma in the Netherlands: increased incidence rates, but stable relative survival and mortality 1989‐2008. Eur J Cancer 2012; 48:2046–53. [DOI] [PubMed] [Google Scholar]
- 7. Hollestein LM, de Vries E, Aarts MJ et al Burden of disease caused by keratinocyte cancer has increased in The Netherlands since 1989. J Am Acad Dermatol 2014; 71:896–903. [DOI] [PubMed] [Google Scholar]
- 8. Kirby JS, Gregory T, Liu G et al Variation in the cost of managing actinic keratosis. JAMA Dermatol 2017; 153:264–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ikram MA, Brusselle GGO, Murad SD et al The Rotterdam Study: 2018 update on objectives, design and main results. Eur J Epidemiol 2017; 32:807–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Casparie M, Tiebosch AT, Burger G et al Pathology databanking and biobanking in The Netherlands, a central role for PALGA, the nationwide histopathology and cytopathology data network and archive. Cell Oncol 2007; 29:19–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Verkouteren JA, Smedinga H, Steyerberg EW et al Predicting the risk of a second basal cell carcinoma. J Invest Dermatol 2015; 135:2649–56. [DOI] [PubMed] [Google Scholar]
- 12. Vlug AE, van der Lei J, Mosseveld BM et al Postmarketing surveillance based on electronic patient records: the IPCI project. Methods Inf Med 1999; 38:339–44. [PubMed] [Google Scholar]
- 13. Nederlandse Zorgautoriteit . TDHAN. DIS Open data: The Dutch Healthcare Authority (Nederlandse Zorgautoriteit). Available at: http://www.opendisdata.nl/ (last accessed 4 March 2019).
- 14. Dinmohamed AG, van Norden Y, Visser O et al The use of medical claims to assess incidence, diagnostic procedures and initial treatment of myelodysplastic syndromes and chronic myelomonocytic leukemia in the Netherlands. Leuk Res 2015; 39:177–82. [DOI] [PubMed] [Google Scholar]
- 15. Benchimol EI, Smeeth L, Guttmann A et al The REporting of studies Conducted using Observational Routinely‐collected health Data (RECORD) statement. PLOS Med 2015; 12:e1001885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. von Elm E, Altman DG, Egger M et al Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Br Med J 2007; 335:806–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Torezan LA, Festa‐Neto C. Cutaneous field cancerization: clinical, histopathological and therapeutic aspects. An Bras Dermatol 2013; 88:775–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Rosen T, Lebwohl MG. Prevalence and awareness of actinic keratosis: barriers and opportunities. J Am Acad Dermatol 2013; 68 (Suppl. 1):S2–9. [DOI] [PubMed] [Google Scholar]
- 19. Baaten GGG, Buis PAJ, Damen Z et al NHG‐Standaard Verdachte Huidafwijkingen 2017. Available at: https://www.nhg.org/standaarden/volledig/nhg-standaard-verdachte-huidafwijkingen (last accessed 11 April 2019).
- 20. U.S. Preventive Services Task Force . Screening for skin cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med 2009; 150:188–93. [DOI] [PubMed] [Google Scholar]
- 21. U.S. Preventive Services Task Force . Behavioral counseling to prevent skin cancer: recommendation statement. Am Fam Physician 2012; 86:1–3. [PubMed] [Google Scholar]
- 22. Youl PH, Janda M, Aitken JF et al Body‐site distribution of skin cancer, pre‐malignant and common benign pigmented lesions excised in general practice. Br J Dermatol 2011; 165:35–43. [DOI] [PubMed] [Google Scholar]
- 23. Bjørland E, Brekke M. What do patients bring up in consultations? An observational study in general practice. Scand J Prim Health Care 2015; 33:206–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Beasley JW, Hankey TH, Erickson R et al How many problems do family physicians manage at each encounter? A WReN study. Ann Fam Med 2004; 2:405–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Sandelowsky H, Hylander I, Krakau I et al Time pressured deprioritization of COPD in primary care: a qualitative study. Scand J Prim Health Care 2016; 34:55–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Venereologie NVvDe . Richtlijn Actinische keratose (Versie 15‐10‐2010) 2010. Available at: http://www.nvdv.nl/wp-content/uploads/2014/07/Richtlijn-Actinische-Keratose-2010-15-10.pdf (last accessed 11 April 2019).
- 27. Beljaards RC, van der Sande A. Update richtlijn actinische keratosen 2017. Ned Tijdschr Dermatol Venereol 2017; 27:190–2. [Google Scholar]
- 28. Primary Care Dermatology Society (PCDS) . Actinic keratosis (syn. solar keratosis). 2017. (updated 17 November 2017). Available at: http://www.pcds.org.uk/clinical-guidance/actinic-keratosis-syn.-solar-keratosis/ (last accessed 11 April 2019).
- 29. de Berker D, McGregor JM, Hughes BR. Guidelines for the management of actinic keratoses. Br J Dermatol 2007; 156:222–30. [DOI] [PubMed] [Google Scholar]
- 30. Fleming P, Zhou S, Bobotsis R, Lynde C. Comparison of the treatment guidelines for actinic keratosis: a critical appraisal and review. J Cutan Med Surg 2017; 21:408–17. [DOI] [PubMed] [Google Scholar]
- 31. Koelink CJ, Kollen BJ, Groenhof F et al Skin lesions suspected of malignancy: an increasing burden on general practice. BMC Fam Pract 2014; 15:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Hayes SF. Early detection of melanoma is key, so let's teach it. Br Med J 2009; 338:a3138. [DOI] [PubMed] [Google Scholar]
- 33. de Vries E. Huidaandoeningen bij huisarts en dermatoloog. 2013. Available at: https://www.ntvg.nl/academie/infographics/huidaandoeningen-bij-huisarts-en-dermatoloog (last accessed 4 March 2019).
- 34. Yaakub A, Cohen SN, Singh M, Goulding JMR. Dermatological content of U.K. undergraduate curricula: where are we now? Br J Dermatol 2017; 176:836. [DOI] [PubMed] [Google Scholar]
- 35. Fleischer AB Jr, Herbert CR, Feldman SR, O'Brien F. Diagnosis of skin disease by nondermatologists. Am J Manag Care 2000; 6:1149–56. [PubMed] [Google Scholar]
- 36. Hansra NK, O'Sullivan P, Chen CL, Berger TG. Medical school dermatology curriculum: are we adequately preparing primary care physicians? J Am Acad Dermatol 2009; 61:23–9e1. [DOI] [PubMed] [Google Scholar]
- 37. Murase JE. Understanding the importance of dermatology training in undergraduate medical education. Dermatol Pract Concept 2015; 5:95–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Farrimond H, Dornan TL, Cockcroft A, Rhodes LE. Development and evaluation of an e‐learning package for teaching skin examination. Action research. Br J Dermatol 2006; 155:592–9. [DOI] [PubMed] [Google Scholar]
- 39. Kirshen C, Shoimer I, Wismer J et al Teaching dermatology to Canadian undergraduate medical students. J Cutan Med Surg 2011; 15:150–4. [DOI] [PubMed] [Google Scholar]
- 40. Schofield JK, Fleming D, Grindlay D, Williams H. Skin conditions are the commonest new reason people present to general practitioners in England and Wales. Br J Dermatol 2011; 165:1044–50. [DOI] [PubMed] [Google Scholar]
- 41. Fischer F, Lange K, Klose K et al Barriers and strategies in guideline implementation—a scoping review. Healthcare (Basel) 2016; 4:E36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Greenfield G, Foley K, Majeed A. Rethinking primary care's gatekeeper role. Br Med J 2016; 354:i4803. [DOI] [PubMed] [Google Scholar]
- 43. Wammes JJ, Jeurissen PP, Verhoef LM et al Is the role as gatekeeper still feasible? A survey among Dutch general practitioners. Fam Pract 2014; 31:538–44. [DOI] [PubMed] [Google Scholar]
- 44. Barnett ML, Song Z, Bitton A, Rose S, Landon BE. Gatekeeping and patterns of outpatient care post healthcare reform. Am J Manag Care 2018; 24:e312–18. [PubMed] [Google Scholar]
- 45. Rotar AM, Van Den Berg MJ, Schafer W et al Shared decision making between patient and GP about referrals from primary care: does gatekeeping make a difference? PLOS ONE 2018; 13:e0198729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. de Vries E, Nijsten T, Louwman MW, Coebergh JW. [Skin cancer epidemic in the Netherlands]. Ned Tijdschr Geneeskd 2009; 153:A768 (in Dutch). [PubMed] [Google Scholar]
- 47. Cipriano SD, Dybbro E, Boscardin CK et al Online learning in a dermatology clerkship: piloting the new American Academy of Dermatology Medical Student Core Curriculum. J Am Acad Dermatol 2013; 69:267–72. [DOI] [PubMed] [Google Scholar]
- 48. Halpern AC, Hanson LJ. Awareness of, knowledge of and attitudes to nonmelanoma skin cancer (NMSC) and actinic keratosis (AK) among physicians. Int J Dermatol 2004; 43:638–42. [DOI] [PubMed] [Google Scholar]
- 49. Lam TP, Yeung CK, Lam KF. What are the learning outcomes of a short postgraduate training course in dermatology for primary care doctors? BMC Med Educ 2011; 11:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Taneja A, Singh PP, Tan JPL et al Efficacy of general practitioners with specialty interests for surgical procedures. ANZ J Surg 2015; 85:344–8. [DOI] [PubMed] [Google Scholar]
- 51. Spurling G, Jackson C. GPs with special interests—benefits to patients, GPs and the community. Aust Fam Physician 2009; 38:337–9. [PubMed] [Google Scholar]
- 52. Schofield J, Grindlay D, Williams H. Skin Conditions in the U.K.: A Health Care Needs Assessment. Nottingham: Centre of Evidence Based Dermatology, University of Nottingham; 2009. [Google Scholar]
- 53. Chetty P, Choi F, Mitchell T. Primary care review of actinic keratosis and its therapeutic options: a global perspective. Dermatol Ther (Heidelb) 2015; 5:19–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1 Methods.


