Abstract
Introduction
The aim of this study was to describe the safety and anatomical results of a surgical approach with a single‐incision 6‐point fixation vaginal mesh for the treatment of pelvic organ prolapse at perioperatively and at 1‐year follow‐up.
Materials and Methods
This was a prospective observational study of patients who underwent operation receiving an InGYNious anterior transvaginal mesh. All patients with symptomatic stage II prolapse or higher were included in the study. Exclusion criteria were the unwillingness or inability to give written informed consent, neuromuscular disorders, malignant diseases, previous radiation in the pelvis, or chronic pain syndrome. Every patient completed a structured questionnaire and a full physical examination according to the IUGA‐ICS POP‐Q staging system before the operation and at 1‐year follow‐up.
Results
Two hundred fifty‐four patients (91%) were included in the study. The intraoperative complication rate was 7% with hemorrhage being the most common complication. Six patients (2.4%) had undergone reoperation for prolapse (four out of the six patients had reoperation in the posterior compartment) and were excluded from the objective outcome analysis. In the remaining 248 patients all POP‐Q measurements were significantly improved in the anterior and apical compartments. Similarly, urge urinary incontinence and voiding dysfunction improved significantly.
Conclusions
In this series, the objective outcome one year after the InGYNious mesh was good with low numbers of mesh‐related problems or reoperation for prolapse.
Keywords: 1‐year follow‐up, 6‐point fixation, objective outcome, pelvic organ prolapse, vaginal mesh
1. INTRODUCTION
Pelvic organ prolapse (POP) is a major burden for the public health system affecting up to 50% of all women during their life.1 Recurrent prolapse is described to be as high as 30% with native tissue surgery,2 which was the reason for the implementation of synthetic meshes into vaginal surgery. Perioperatively, the incidence of complications is comparable between the native tissue surgery vs transvaginal mesh (TVM) surgery.3 Long‐term objective anatomical results have been reported to be superior in women with TVM compared with native tissue surgery,4 which might be due to the fact that both the anterior and apical compartments are supported. Due to high numbers of side effects including contraction, mesh erosion, and pain with the first generation of vaginal meshes there is heated debate about vaginal mesh surgery with companies withdrawing their kits from the market and whole countries banning vaginal meshes after several food and drug administration (FDA) warnings and law suits.
Problems after transvaginal placement include pain, exposure, extrusion, and dyspareunia.5, 6 The first reports on vaginal mesh surgery included meshes that have been already withdrawn from the market with specific properties that are not preferable any more like heavy weight or transobturator arms. It is known, that lighter meshes are preferable due to lower numbers of complications while heavier meshes cause especially more protrusion or extrusion.7 Quite recently, an ultralightweight mesh kit has been introduced into POP surgery that can be fixated with six arms using a minimal invasive technique. The aim of this study was to describe the safety and anatomical results of a surgical approach with a single‐incision 6‐point fixation vaginal mesh for the treatment of pelvic organ prolapse perioperatively and at 1‐year follow‐up.
2. METHODS
This was a prospective observational study of patients who underwent an operation with an anterior TVM (InGYNious, A.M.I., Feldkirch, Austria) (Figure 1) for POP between November 2014 and June 2016 at six urogynecological centers in Germany. The InGYNious isoelastic mesh with hexagonal structure is ultralightweight made from monofilament polypropylene mesh (21 g/m2) and consists of large micropores of 100 to 150 µm and macropores of 1.9 to 2.8 mm. Ethical approval was granted by the local ethics committees. All patients over the age of 18 presenting with symptomatic stage II prolapse or higher (point Ba or C > −1 according to the international Pelvic Organ Prolapse Quantification System, POP‐Q) were included in the study. Patients with primary and recurrent POP were included in this study. Patients with primary POP were included in case of a lateral or especially large defects. Exclusion criteria were the unwillingness or inability to give written informed consent, neuromuscular disorders, malignant diseases, previous radiation in the pelvis, or chronic pain syndrome. All patients completed a structured questionnaire and examination according to the IUGA‐ICS POP‐Q staging system.8 Preoperative urodynamic was performed routinely but in case of manifest incontinence or if otherwise indicated. The surgery was performed according to the manufacturer's instructions by six different experienced urogynecological surgeons (AB, AK, CF, AN, HL, and MM) proficient in transvaginal surgery as published recently.9 Briefly, the mesh was placed under general or epidural anesthesia with or without concomitant hysterectomy depending on the patient's preference or medical indications.10 Concomitant colporrhaphy and or incontinence surgeries were also performed as indicated. The mesh was placed in the paravesical space and fixated with six polyester sutures using the i‐Stitch instrument (A.M.I.) (Figures 1 and 2). The vaginal incision was closed with braided resorbable sutures. A vaginal pack with estrogen cream and catheter were placed for at least 24 hours.
Figure 1.
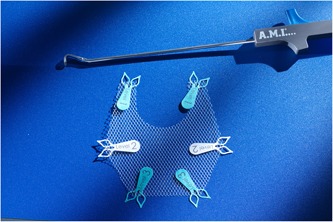
InGYNious mesh and i‐Stitch instrument
Figure 2.
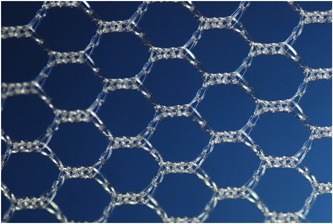
Microscopic view of InGYNious mesh
At 1‐year anatomical success was defined as any point of the POP‐Q System less than 1 cm relative to the hymen for both anterior and apical compartments.11 The examination was performed by a gynecologist other than the surgeon. Patients who were unavailable for the 12 months follow‐up were excluded from the analysis. All definitions are in line recommendations from IUGA/ICS.6, 11 Postoperative pain was assessed using the validated visual analogue scale (VAS) on the day of discharge. Perioperative and postoperative complications within the last 12 months were recorded in the CRFs.
The manufacturer of the mesh kit was a cosponsor of the trial and reviewed the presubmission draft of the manuscript. The company did not provide the products used in the study and was not involved in data collection, analysis or in the decision to submit the results for publication. The senior author (DU) collated the results but did not participate in the surgical part of the study.
2.1. Statistical analysis
Descriptive statistics are presented as mean and standard deviation for numerical variables and as counts and percentages for categorical variables. Differences between preoperation and 1‐year follow‐up are analyzed by means of the Wilcoxon signed‐rank test for matched pairs for numerical variables and the McNemar test for categorical variables. The level of significance is set to 5%.
3. RESULTS
Two hundred seventy‐eight patients were included in the study and operated with the InGYNious mesh. Twenty‐four were lost to follow‐up, hence 254 (91%) were available for data analysis. The demographic data of the study group are presented in Table 1. Concomitant operations are listed in Table 2 with colporrhaphy posterior being the most common procedure.
Table 1.
Demographic data of patients (n = 254) at time of InGYNious operation
| Age, y, mean ± SD | 70.62 ± 9.56 |
| BMI, kg/m2, mean ± SD | 26.54 ± 3.98 |
| Smoking, n (%) | 10 (3.9) |
| Parity, median (range) | 2 (0‐8) |
| Mode of delivery, mean ± SD | |
| Vaginal delivery | 2.10 ± 1.24 |
| Cesarean section | 0.06 ± 0.26 |
| Vaginal‐operative delivery | 0.07 ± 0.27 |
| Previous surgery, n (%) | |
| Hysterectomy | 76 (29.9) |
| POP surgery | 44 (17.3) |
| Anti‐incontinence procedures | 10 (3.9) |
| Comorbidities, n (%) | |
| Diabetes | 13 (5.1) |
| Lung disease | 5 (2.0) |
| Length of hospital stay, mean ± SD | 6.04 ± 2.45 |
Abbreviations: BMI, body mass index; POP, pelvic organ prolapse.
Data are given as mean ± standard deviation or number (%).
Table 2.
Concomitant operations performed at the time of the InGYNious procedure (n = 254)
| n (%) | |
|---|---|
| Colporrhaphy posterior | 23 (9) |
| Posterior mesh reinforcement (InGYNious posterior) | 4 (1.6) |
| vaginal hysterectomy | 11 (4) |
| Concomitant suburethral sling for symptomatic or occult SUI | 8 (3.1) |
Abbreviation: SUI, stress urinary incontinence.
Seventeen patients (7%) had intraoperative complications including bladder lesions in two patients (0.8%), ureteral lesion in one patient (0.4%), and fourteen (5.5%) with heavy bleeding causing a hematoma. The two patients with bladder lesion received a temporary suprapubic catheter. Only a few postoperative complications occurred and were transient; one patient had a wound infection (0.4%), and two had hydronephrosis (0.8%). These two patients received a permanent catheter until the voiding dysfunction resolved (44 and 48 days after operation).
At 1‐year follow‐up patients were invited for a standardized interview and urogynecologic examination. At this time, six patients (2.4%) had undergone reoperation for prolapse and were excluded from the objective outcome analysis. Four out of the six patients had reoperation in the posterior compartment and all had satisfactory anatomical results at the time of follow up. Two out of the six patients received a bilateral sacrospinous colposuspension (BSC) mesh for apical recurrence. In the remaining 248 patients, POP‐Q measurements improved significantly 1 year after the operation in the anterior and apical compartments (Table 3). Anatomical success was achieved in 79% of cases in the anterior, in 83% in the apical compartment, and in 73% in both the anterior and apical compartments. If we had set success to any point less than 0 (POPQ) success would have been achieved in 93% for both the anterior and apical compartments. TVL also improved and was not shortened by the operation.
Table 3.
POP‐Q measurements preoperatively and at 1‐year follow‐up
| N = 248 | N = 6 | |||||
|---|---|---|---|---|---|---|
| Variables | Preop. | At 1‐y follow‐up | P value* | Preop. excluded | 1‐y excluded | P value* |
| Aa | 1.17 ± 1.07 | −2.04 ± 0.96 | <0.001 | 1.00 ± 1.67 | −2.33 ± 0.82 | 0.027 |
| Ba | 1.67 ± 1.56 | −2.16 ± 0.88 | <0.001 | 1.83 ± 1.47 | −2.33 ± 0.82 | 0.026 |
| C | −0.99 ± 3.59 | −5.36 ± 3.18 | <0.001 | 0.00 ± 2.28 | −5.00 ± 4.15 | 0.026 |
| Ap | −1.48 ± 1.27 | −1.65 ± 1.15 | 0.144 | −1.50 ± 0.55 | −2.17 ± 0.75 | 0.157 |
| Bp | −1.47 ± 1.50 | −1.69 ± 1.19 | 0.205 | −1.67 ± 0.52 | −2.17 ± 0.75 | 0.180 |
| TVL | 8.81 ± 1.46 | 9.18 ± 1.69 | <0.001 | 8.83 ± 1.72 | 9.67 ± 1.03 | 0.102 |
| GH | 4.51 ± 1.18 | 4.16 ± 1.26 | <0.001 | 5.00 ± 0.89 | 4.67 ± 1.03 | 0.157 |
Abbreviations: POP‐Q, Pelvic Organ Prolapse Quantification System; Preop, preoperatively.
Data are shown as mean ± SD. POP‐Q measurements as defined by IUGA‐ICS prolapse staging.
The Wilcoxon signed‐rank test for matched pairs.
Urinary and anal symptoms are listed in Table 4. Thirty‐four percent (83 of 254) of the patients were stress urinary incontinent (SUI) at the time of the operation. Eight received a concomitant suburethral tape; 21 received a tape within 12 months after the InGYNious mesh. At the time of follow‐up 29 out of the 72 women with previous SUI (40%) had persistent SUI; 37 of 153 (24%) had de novo SUI out of those who were not reoperated for SUI and/or POP and no primary SUI. Eighty‐one patients (33%) had urge urinary incontinence (UUI) preoperatively; however, only 19 (8%) had this issue at the time of follow‐up. Similarly, voiding dysfunction and residual urine improved significantly postoperatively. Bowel symptoms remained stable with a slight decrease of obstructed defecation.
Table 4.
Urinary and anal incontinence symptoms preoperatively and postoperatively excluding patients with reoperation for POP#
| Variables | Preop. | At 1‐y follow‐up | P value | Preop. excluding# | 1‐y excluding# | P value a |
|---|---|---|---|---|---|---|
| Bladder symptoms, n (%) | ||||||
| SUI | 83 (33.5) | 68 (27.6) b | 0.246 | 3 (50.0) | 1 (16.7) | 0.500 |
| UUI | 81 (32.7) | 19 (7.7) | <0.001 | 1 (16.7) | 0 (0) | n.a. |
| Voiding dysfunction | 100 (40.3) | 3 (1.2) | <0.001 | 2 (33.3) | 0 (0) | n.a. |
| Residual urine, mL, mean ± SD | 61.62 ± 82.19 | 21.57 ± 33.26 | <0.001 | 44.00 ± 62.24 | 18.83 ± 18.61 | 0.686 |
| Bowel symptoms, n (%) | ||||||
| Obstructed defecation | 20 (8.1) | 15 (6.0) | 0.442 | 0 (0) | 1 (16.7) | n.a. |
| Fecal incontinence | 4 (1.6) | 4 (1.6) | 1.000 | 0 (0) | 0 (0) | n.a. |
Abbreviations: na, not applicable; Preop, preoperatively; SUI, stress urinary incontinence; UUI, urge urinary incontinence.
Data are shown as n (%) except for residual urine.
McNemar test, except for residual urine for which the Wilcoxon signed‐rank test for matched pairs was used.
Excluding eight patients with concomitant suburethral tape at time of InGYNious operation.
No serious adverse events were reported for any of the patients within 12 months after the InGYNious insertion. Complications were rare with one patient suffering from recurrent UTI (0.4%), three had voiding dysfunction, and four patients had mesh protrusion (1.6%) but were asymptomatic and only treated with local estrogen. Pain in the pelvis was also rare; only 10 patients (3.9%) described pain with a median pain score of 2.5 on the VAS. Similarly, pain during intercourse was rare; only five patients (1.9%) had dyspareunia at 1‐year follow‐up.
4. DISCUSSION
In this prospective study, the objective anatomical outcome after a vaginal mesh kit operation was high with a low complication rate. The reoperation rates for prolapse or mesh specific problems were also rare in contrast to previous results.4
Our anatomical success rates are similar to previously reported TVM studies where success rates between 75% to 88% have been reported.12 Especially with laparoscopic surgery, cystocele recurrence has been reported to be as high as 24% or any prolapse of at least stage 2 to be as high as 79% which is higher than in our study.13 In this study, both the anterior and apical compartments were equally well treated which might be related to the 6‐point mesh fixation both at the sacrospinous ligament and at the arcus tendineous fascia medially and anteriorly. The InGYNious mesh spreads across the whole vesicovaginal space both treating central and lateral defects. If we had set success of the POP‐Q to stage less than or equal to 1, the success rates would have been higher (93%) which is in line with previously published results with a 2‐point fixated mesh with 94% success rate.14 Hence, apical support seems to be the most important factor for restoring anatomical stability.
After mesh surgery it has been shown that the development of de novo POP can be as high as 47% in the untreated compartments15; however, this high number could not be observed in our study at 12 months follow‐up with only four women needing reoperation in the posterior compartment.
It has also been postulated that TVM could overcorrect the anterior vaginal wall resulting in a high de novo SUI rate. In this study, the de novo SUI rate was 24%; however, none of these women had reoperation for SUI so far and all other aspects of lower urinary tract symptoms improved significantly including voiding function and overactive bladder (OAB).
Serious complications were rare which is in line with previously reported results.16 The erosion rate was below 2% and none of those women needed reoperation but local estrogen therapy was sufficient. Pain and dyspareunia were also lower than previously reported.4, 17 This might be due to the fact that the InGYNious mesh is isoelastic, or that the mesh is only fixated with sutures that are not fixed to the mesh with the sutures also being fixated without any anchors. Another reason for our low number of mesh‐related problems might be the combination of new meshes with skilled surgeons in the field of urogynecology. We have not analyzed the learning curve of our surgeons, but all surgeons had done at least 300 meshes before the start of the study. In Germany, urogynecologic centers have a high volume of patients and TVM surgery still plays a role in POP surgery if indicated.
The complication rate in this study is comparable to native tissue surgery18 or to first generation vaginal meshes.19 There are specific mesh related risks, and they need to be discussed with the patient properly before the operation.
A strength of this study is the prospective design and the standardized way of mesh insertion. A limitation is the single arm design; however, we would have needed too many patients in a randomized setting. That would have taken too long to complete randomization in a timely manner. Another limitation is the fact that subjective outcome data is not reported with a validated outcome tool.
In conclusion, the 6‐point fixation surgery using a lightweight mesh could be an alternative for women with POP, especially in recurrent POP, with a good anatomical outcome and a low rate of mesh‐related complications. Longer follow‐up is needed to draw more specific conclusions especially in terms of reoperation for POP and those data are to be awaited soon.
ACKNOWLEDGMENT
We thank Dr. Fedor Daghofer for statistical analysis.
Brandt A, Kuszka A, Niesel A, et al. 1‐year outcome after treatment of uterovaginal prolapse with a 6‐point fixation mesh. Neurourology and Urodynamics. 2019;38:1129‐1134. 10.1002/nau.23968
The copyright line for this article was changed on 14 May 2019 after original online publication.
References
REFERENCES
- 1. Løwenstein E, Ottesen B, Gimbel H. Incidence and lifetime risk of pelvic organ prolapse surgery in Denmark from 1977 to 2009. Int Urogynecol J. 2015;26(1):49‐55. [DOI] [PubMed] [Google Scholar]
- 2. Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL. Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol. 1997;89(4):501‐506. [DOI] [PubMed] [Google Scholar]
- 3. Besser L, Schwarzman P, Mastrolia SA, et al. Comparative analysis of early adverse events of pelvic organ prolapse repair with or without transvaginal mesh using Clavien‐Dindo classification. Int J Gynaecol Obstet. 2018;142(1):108‐113. [DOI] [PubMed] [Google Scholar]
- 4. Maher C, Feiner B, Baessler K, Christmann‐Schmid C, Haya N, Marjoribanks J. Transvaginal mesh or grafts compared with native tissue repair for vaginal prolapse. Cochrane Database Syst Rev. 2016;2:Cd012079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Miklos JR, Chinthakanan O, Moore RD, et al. The IUGA/ICS classification of synthetic mesh complications in female pelvic floor reconstructive surgery: a multicenter study. Int Urogynecol J. 2016;27(6):933‐938. [DOI] [PubMed] [Google Scholar]
- 6. Haylen BT, Freeman RM, Swift SE, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint terminology and classification of the complications related directly to the insertion of prostheses (meshes, implants, tapes) and grafts in female pelvic floor surgery. Neurourol Urodyn. 2011;30(1):2‐12. [DOI] [PubMed] [Google Scholar]
- 7. Moore RD, Lukban JC. Comparison of vaginal mesh extrusion rates between a lightweight type I polypropylene mesh versus heavier mesh in the treatment of pelvic organ prolapse. Int Urogynecol J. 2012;23(10):1379‐1386. [DOI] [PubMed] [Google Scholar]
- 8. Bump RC, Mattiasson A, Bo K, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996;175(1):10‐17. [DOI] [PubMed] [Google Scholar]
- 9. Brandt A, Ulrich D, Kruska A, et al. Treatment of pelvic organ prolapse using a lightweight modified HexaPro mesh. Pelviperineology. 2018;37:39‐41. [Google Scholar]
- 10. Rivaux G, Fatton B, Letouzey V, Cayrac M, Boileau L, de Tayrac R. Utero‐vaginal suspension using a bilateral vaginal anterior sacrospinous fixation with mesh. Preliminary results. Prog Urol. 2012;22(17):1077‐1083. [DOI] [PubMed] [Google Scholar]
- 11. Haylen BT, Maher CF, Barber MD, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic organ prolapse (POP). Int Urogynecol J. 2016;27(2):165‐194. [DOI] [PubMed] [Google Scholar]
- 12. Maher C, Feiner B, Baessler K, Christmann‐Schmid C, Haya N, Brown J. Surgery for women with anterior compartment prolapse. Cochrane Database Syst Rev. 2016;11:Cd004014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bedford ND, Seman EI, O'Shea RT, Keirse MJ. Long‐term outcomes of laparoscopic repair of cystocoele. Aust N Z J Obstet Gynaecol. 2015;55(6):588‐592. [DOI] [PubMed] [Google Scholar]
- 14. Altman D, Mikkola TS, Bek KM, et al. Pelvic organ prolapse repair using the uphold vaginal support system: a 1‐year multicenter study. Int Urogynecol J. 2016;27(9):1337‐1345. [DOI] [PubMed] [Google Scholar]
- 15. Withagen MI, Milani AL, de Leeuw JW, Vierhout ME. Development of de novo prolapse in untreated vaginal compartments after prolapse repair with and without mesh: a secondary analysis of a randomised controlled trial. BJOG. 2012;119(3):354‐360. [DOI] [PubMed] [Google Scholar]
- 16. Altman D, Vayrynen T, Engh ME, Axelsen S, Falconer C, Nordic Transvaginal Mesh G. Anterior colporrhaphy versus transvaginal mesh for pelvic‐organ prolapse. N Engl J Med. 2011;364(19):1826‐1836. [DOI] [PubMed] [Google Scholar]
- 17. Letouzey V, Ulrich D, Balenbois E, Cornille A, de Tayrac R, Fatton B. Utero‐vaginal suspension using bilateral vaginal anterior sacrospinous fixation with mesh: intermediate results of a cohort study. Int Urogynecol J. 2015;26(12):1803‐1807. [DOI] [PubMed] [Google Scholar]
- 18. Vollebregt A, Fischer K, Gietelink D, van der Vaart CH. Primary surgical repair of anterior vaginal prolapse: a randomised trial comparing anatomical and functional outcome between anterior colporrhaphy and trocar‐guided transobturator anterior mesh. BJOG. 2011;118(12):1518‐1527. [DOI] [PubMed] [Google Scholar]
- 19. Bjelic‐Radisic V, Aigmueller T, Preyer O, et al. Vaginal prolapse surgery with transvaginal mesh: results of the Austrian registry. Int Urogynecol J. 2014;25(8):1047‐1052. [DOI] [PubMed] [Google Scholar]


