Abstract
Background
Tublosis (TB) and the approaches to successful management are commonly misunderstood health topics among patients and family members within resource-limited settings. Such public misconceptions often result in delayed diagnoses of afflicted patients, suboptimal compliance with prescribed therapies and a negative community social stigma that hinders effective contact investigations.
Objective
To determine through an observational field pilot study if videography-based TB education program can be implemented in busy resource-limited outpatient TB clinic settings and improve both patient and family understanding of TB and its treatment, as well as, improve the efficiency of TB medical evaluations and corresponding contact investigations.
Methods
We produced and implemented a videography-based health educational pilot strategy in 14 TB clinics within El Salvador to supplement the discussions between health providers, patients and families. Field observations and impressions after the first year of implementation were recorded.
Results
After viewing the video, patient impressions revealed greater understanding of TB including how it's transmitted and successfully treated, as well as, a more optimistic outlook of the diagnosis. Family members viewing the video displayed less fear and greater interest in TB and also exhibited more support for relatives undergoing evaluation or treatment. Salvadorian TB health providers reported improvements in patient compliance with treatment, contact investigations of suspected patients, delivery of sputum samples for testing, clinic time-efficiency spent with patients, and an observed reduction of negative family stigma of TB.
Conclusions
Our findings suggest that videography-based TB education can be successfully implemented in busy and resource-limited outpatient settings, and can provide a potentially efficient and low-cost effective strategy towards optimizing patient understanding, acceptance and compliance with TB treatment recommendations. This feasibility pilot study provides an opportunity within underresourced clinics for further evaluation regarding the favorable educational and sustainable impact of videography-based health education.
Keywords: Tuberculosis, Videography, Education, El Salvador, Communication
1. Introduction
In 2014, approximately 9.6 million people developed active tuberculosis (TB) resulting in 1.5 million deaths [1]. Over 95% of these TB-related deaths occur in low- and middle-income countries where education and public health information are often less accessible [2]. Consequently, many patients diagnosed with active TB or latent infection have minimal or no understanding what tuberculosis is, how it is acquired, transmitted or treated. Patients’ general health beliefs are affected by their own experiences and fundamental understanding of health issues, often referred to as “health literacy”. When health literacy rates are low, patients become more prone towards non-adherence with medical evaluations and treatment recommendations [3]. Patient-driven reluctance in seeking medical attention or resorting to local or ‘traditional’ healers can result in significant delays in TB diagnoses and associated worsening prognoses [4], [5], [6].
For many patients and family members who have some awareness of TB, there often remains an abundance of confusion, social misperceptions and negative social stigma [7], [8]. Such misunderstandings by patients and misinformation circulated within a family or local community about their disease often create a distrust of modernized health care, compromise medication tolerability and reduce treatment compliance [9], [10]. Additionally, family and community misinformation of tuberculosis often lead to patient social isolation or ostracism and pose barriers towards efficient public health contact investigations [9].
Face-to-face discussions with patients and family members are vital towards achieving an adequate fundamental understanding of TB; however, many patients commonly continue to have unresolved questions and confusion. Many factors contributing to persistent patient confusion include underlying health care anxiety; ethnic, cultural and language barriers; and information provided in an uncomprehensive manner to patients with limited educational backgrounds.
Although perhaps more pronounced, these problems are not limited to only low- and middle-income countries, as similar patient misconceptions and barriers between effective patient-health provider communication commonly are encountered within Europe, Canada and the U.S. [11]. Within busy hospital or outpatient clinic practices, health providers often will not have adequate time for more detailed discussions with their patients about TB. This particular problem is notably compounded among many TB clinics within low- and middle-income countries, where the incidence of TB is generally much higher compared to the U.S. According to the World Health Organization (WHO), El Salvador reported an incidence of TB of 33.8 per 100,000 population in 2013 [12], which is over 11 times higher compared to the US (approximatively 3.0 per 100,000 since) [13], [14], [15]. Indeed, many TB clinics within the San Salvador region are typically very busy, and actual provider face-time spent with patients can be quite limited.
We therefore hypothesized that the implementation of a low-cost educational strategy to improve the basic patient and family understanding of TB and the corresponding treatment plan would result in more effective and time-efficient management of TB patients, help reduce negative disease stigma and subsequently improve contact investigations. Such an approach may seem intuitive as health education by videography has been successfully used in other venues, including community-based participatory research and in general medical practice [16], [17], [18], [19]. However, how best to apply such a strategy within an under-resourced and busy international TB health care setting has not been well outlined.
To improve patient and family understanding of tuberculosis, we developed a videography-based educational tool utilizing visual aids and patient testimonials to discuss basic principles of TB, including how it can be successfully treated and cured. This pilot ‘field’ study aims to evaluate the implementation and effectiveness of this low-cost educational intervention in improving patient understanding of TB and compliance with treatment recommendations by gathering impressions of patients, family members and health care providers in TB clinics in San Salvador.
2. Methods
2.1. Partnership and review process
Working with the El Salvador Ministry of Health (MOH) and corresponding National Tuberculosis program (Programa Nacional de TB y Enfermedades Respiratorias; Ministerio de Salud, El Salvador/MINSAL), we first performed an on-site educational needs-assessment of the MOH TB clinics within El Salvador. Supplemental TB educational strategies for patient and their family members were identified as a priority need. We therefore developed an educational video specifically designed for patients, family members and local communities. The script and visual content for the video was composed in partnership with Salvadoran TB clinic physician-leaders and nurses and was formally approved by the El Salvador MOH TB program health directors. The medical content was additionally examined to ensure consistency with current published TB management guidelines by the Pan American Health Organization (PAHO) [20] and WHO [21] as well as with local established clinical practice TB protocols within El Salvador. The filming was performed entirely on location in El Salvador (San Salvador and surrounding municipalities). All personnel filmed in the video including health providers and former patients are from El Salvador.
2.2. Settings
The 14 participating MOH TB clinics, including locations, are listed in Table 1. Given the diverging educational and literacy backgrounds of the regional patient populations, the video includes as much visual imagery for select teaching points as possible. Spanish is the primary language of El Salvador; therefore, the script was composed in Spanish using verbal dialogue that was both readily understandable and appropriate for the general population (as determined by the Salvadorian health providers).
Table 1.
Participating TB clinics in El Salvador.
| Name | State/region | Setting/region |
|---|---|---|
| 1. UCSF Mejicanos | Central San Salvador | Metropolitan |
| 2. UCSF Zacamil | Central San Salvador | Metropolitan |
| 3. UCSF Apopa | North San Salvador | Metropolitan |
| 4. UCSF Popotlán | North San Salvador | Metropolitan |
| 5. UCSF Unicentro | East San Salvador | Metropolitan |
| 6. UCSF Quezaltepeque | La Libertad | Central-west |
| 7. UCSF Ciudad Arce | La Libertad | Central-west |
| 8. UCSF Díaz del Pinal | La Libertad | Central-west |
| 9. UCSF Puerto de la Libertad | La Libertad | Central-west |
| 10. UCSF Periférica Chalatenango | Chalatenango | Central-west |
| 11. UCSF Periférica de Zacatecoluca | La Paz | South-central |
| 12. UCSF Periférica Cojutepeque | Cuscatlán | Central |
| 13. UCSF Periférica San Vicente | San Vicente | Central-east |
| 14. UCSF Periférica de San Miguel | San Miguel | Eastern |
UCSF = La Unidad Comunitaria de Salud Familiar (Community family health unit).
2.3. Educational video content
The educational composition of the video is listed in Table 2. The video content is divided into 4 short sections: (1) basic information on what TB is and how it is acquired, (2) fundamental points how TB is detected and successfully treated, (3) common public misconceptions and misunderstandings of TB and (4) patient testimonials regarding their experiences with TB and its treatment.
Table 2.
TB video educational content.
| Section I: What is tuberculosis – general information: |
|
| Section II: Detection and treatment of TB |
|
| Section III: addressing misconceptions / misunderstandings of TB |
|
| Section IV: patient testimonials (successful completion of TB therapy) |
|
The video opens with former patients discussing their initial perceptions and misperceptions of TB and what they subsequently learned about TB after seeing their health provider. The content of the video is delivered verbally by Salvadorian health providers and former TB patients superimposed with informational graphics and imagery along with select narrated text added to reinforce specific points. The video portrays real patients speaking with or being examined by their health providers, patients interacting with family members at home, and images of the general public and notable local landmarks. The video concludes with patient testimonials regarding their favorable TB treatment outcomes and returning to their work or other daily activities.
2.4. Flow process model for video viewing
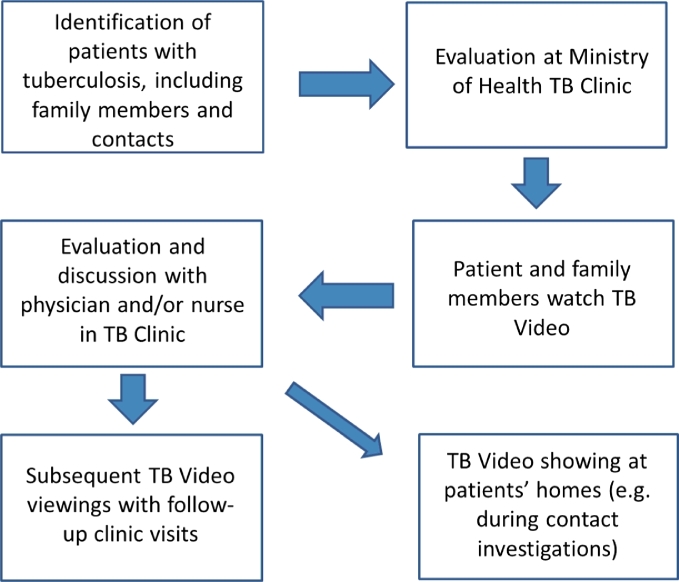
The time period for observational data collection and initial program evaluation was from January 2013 through January 2014. Supplemental patient questionnaire responses and additional TB clinic nursing comparative observations were collected in 2015. Each participating TB clinic received multiple DVDs containing the TB educational video and DVD players (Fig. 1). Portable lightweight, battery operated DVD players were used to allow for viewings in both the TB clinics and patients' homes. A flow process was composed for viewing the video (Fig. 2).
Fig. 1.
TB educational DVD and DVD player.
Fig. 2.
Flow process model for DVD viewing.
Once a diagnosis of TB was suspected or confirmed in the San Salvador region, each patient would be referred to one of 14 MOH-supported TB clinics. Upon arriving to the TB clinic, patients and accompanying family members would watch the 7 minute educational video. Each patient then met with a physician and/or nurse for an examination and more comprehensive discussion on TB and the treatment plans. The video was designed to be short and not disruptive to a busy outpatient clinic practice.
Upon return evaluations to the TB clinic, patients and family members would again watch the video to reinforce the primary educational points previously made. In some clinics with mounted television monitors in the waiting rooms, the video was also displayed to larger patient and family audiences. As part of the contact investigations, TB nursing outreach workers would travel to many of the patients' homes with a portable DVD player to show the educational video to family members and interested neighbors.
2.5. Evaluation of effectiveness and impact of videography intervention
During and after the patient treatment courses, the participating MOH TB clinics were instructed to ask patients and family members a set of questions listed in Table 3. The questions addressed basic information about TB including transmission, symptoms, medical examination procedures and curative potential. Additional questions were commonly asked by the health providers for other video impact assessments, including viewer impressions of the video, personal feelings of fear and discomfort about TB, the treatment plans outlined and other select issues. Supplemental video-specific impact assessments of patients by the TB health providers were recorded based on their observations and impressions with subsequent patient treatment compliance, contact investigations, and time spent talking with patients during clinic visits. All observational data, including patient and family member responses, was collected by the El Salvador MOH through the participating TB clinics.
Table 3.
Questions asked to patients and family members about tuberculosisa (basic knowledge).
| 1. Is TB contagious? |
| 2. What causes TB? |
| 3. How is TB transmitted? |
| 4. What are the primary symptoms of pulmonary TB? |
| 5. What does a medical examination of a person with TB involve? |
| 6. Is TB curable? |
The questionnaire was provided in Spanish for patients and family members; translated into English for this table.
2.6. Ethics
All patients, former patients, family members and health providers included in the video openly consented before filming commenced, and no patient specific or confidential information was used. Permission to conduct the project was granted through the El Salvador MOH and the 14 participating TB clinics. The project was exempt for review by the Mayo Clinic institutional review board.
3. Results
From January 2013 through January 2014, 1916 patients and family members viewed the TB video. As previously noted, home viewings of the video to family members and neighbors were shown for TB contact investigations and for select patients not able to travel to a local health clinic. The impressions and observations of health providers from the participating TB clinics were compiled by the MOH during the 12 month period and are listed in Table 4. Many of the participating TB clinics reported additional and supplemental patient, family and health provider impressions of the video, although such data collection was not consistent across all clinics.
Table 4.
Three-tiered assessment of the TB educational video impact and corresponding statements by the Ministry of Health compiled from the impressions and observations submitted by the participating TB clinic health providers.
| Tier 1: patient responses and observed changes | |
| Tier 2: family member and community responses | |
| Tier 3: MOH TB provider responses and observationsb |
|
Numbers in parentheses indicate the number of clinics reporting specific outcomes as documented by Ministry of Health. Outcomes without corresponding numbers were those reported directly by multiple TB clinics but could not be accurately quantified by the Ministry of Health.
Includes physicians and nurses working in the MOH-supported TB clinic.
Health providers from ten participating TB clinics observed noticeable improvements in patients' knowledge of TB, including a greater patient understanding of what TB is, how TB infects people and how it is treated. Among patients who described a better understanding of TB after watching the video, health providers observed higher interest in the disease itself and more acceptance of the diagnosis. At least five clinics also experienced improvements in patient adherence to TB therapy, which was attributed to patients having a better understanding of their diagnosis and rationale for taking their therapy. After watching the video, many patients also were observed to have a better understanding why sputum collections were important in both the disease diagnosis and subsequent monitoring of treatment effectiveness.
TB clinic health providers and outreach workers also provided observational assessments on patients' family members who watched the video either in the clinic or at home. Though targeted conversations with family members, health providers from five TB clinics reported a perceived reduction in both the fear and negative family stigma about TB. Indeed, TB outreach workers from these clinics described a corresponding rise in family and local community interest in TB, coupled with an increased willingness of family members to help identify symptomatic relatives for evaluation. In addition, four clinics also reported significant improvements in family support of TB patients, largely attributed to an improved understanding of the ‘curative’ potential and resolution of TB infectiousness conferred by treatment.
Compared to MOH TB clinic operations before implementation of the educational video, health providers from the TB clinics using the video subjectively reported more time-efficient TB clinic evaluations through more targeted discussions with informed patients and less repetition of basic TB-specific information. Through the efforts to show family members the video at the clinic and/or at home, nurses from six clinics reported more efficient contact investigations and more effective assessments of potential secondary TB cases in the home and community. TB outreach workers also subjectively reported improvements in directly observed therapy (DOT)-based delivery and treatment completion rates outside of the clinic setting, but measurements of these metrics were not available. Improved delivery of patient sputum samples for acid-fast bacilli (AFB) staining were also observed, but these also were not formally quantified. In discussions with the TB clinic directors and MOH TB section leadership, the short TB video did not interfere with the high volumes of patient care in any of the participating TB clinics.
To further substantiate the initial observational subjective impact of the educational video intervention among the participating TB clinics, the El Salvador MOH documented the results from the pre- and post-video viewing questionnaire with an additional random 15 patients and family members in 2015 (Table 5). After watching the video, there was an 80% response increase from patients and family members that TB was contagious, a 53% response increase that TB is caused by “a germ”, a 60% response increase that TB is transmitted by people who are sick with active disease (rather than by those with latent infection), a 33% increase in identifying the correct diagnostic testing used for TB, and an 87% response increase (all responders) after watching the video that TB is curable.
Table 5.
Patient and family member answers to MOH questionnaire before and after watching the video over 1-month perioda.
| Pre- and post-video patient/family member questionnaire | Patient and family members responses to questions before watching the video (n = 15): | Patient and family members responses to questions after watching the video (n = 15) | Measured change in response after viewing video |
|---|---|---|---|
| Is TB contagious? |
|
|
|
| What causes TB? |
|
|
|
| How is TB transmitted? |
|
|
|
| What are some symptoms of pulmonary TB? |
|
|
No significant changes. Patients and families were familiar with at least some of the symptoms often through the patient's presentation |
| What does a medical examination of a person with TB involve? |
|
|
33% response increase in identifying diagnostic testing used |
| Is TB curable? |
|
|
87% response increase that TB is curableb |
2015 questionnaire provided by Ministry of Health (MOH).
87% response increase that TB is curable.
Also in 2015, the MOH TB section leadership queried nursing coordinators from seven participating TB clinics that had select baseline information available before the start of this videography project. Using the TB education video for patients and family members over the subsequent two years, the nurses uniformly reported a continued and sustainable observed increase in patient and family member TB knowledge retention and patient adherence to prescribed TB therapy. Conversely, these nurses also reported an approximated 50% decrease in patients subsequently not completing therapy and a perceived sustainable decrease in the negative stigma and discrimination verbalized by patients upon questioning.
Additional observations and commentary reported by patients, family members and health providers are listed in Table 6. Problems encountered with the project were also recorded and primary reflected the equipment used. The DVD players used did not have an overly high auditory volume capacity, making the video difficult to hear for some patients within a noisy bustling clinic. A paucity of electrical outlets in some clinics or lack of replacement batteries occasionally created delays in viewing the video. One of the DVD players also broke down and needed to be replaced. Importantly, information on specific patient numbers was not available that would otherwise allow for direct and more objective comparisons of treatment compliance through DOT and treatment completion rates before and after implementation of the videography project in the 14 TB clinics.
Table 6.
Additional videography project commentary reported by TB clinic health providers to the MOH.
|
4. Discussion
Wide ranging misconceptions and false beliefs about TB significantly contribute to delays in seeking medical care and compliance with treatment [5], [9]. Social isolation, inner-family ostracism and marital problems are common sequela of TB among the misinformed [22], [23]. Thus, the El Salvador MOH considers optimizing patient and public TB education a high priority within their country-wide TB control efforts.
Overall, the TB videography program resulted in noticeable observed and perceived improvements in patient and family understanding of tuberculosis which correlated with an enhanced patient acceptance of their diagnosis, higher TB treatment adherence and expedited patient sputum sample submissions. Decreasing the fear and common misconceptions of TB through education was a vital step towards increasing family support of many TB patients. By enhancing a basic understanding of TB through videography-based education, health providers and clinic outreach workers could more easily deliver medications via DOT, ensure patient treatment completion and perform contact investigations. Within the participating TB clinics, the Salvadorian health providers felt the project improved both the quality and time-efficiency of their discussions with patients. Thus, videography-based TB education was considered a very helpful and probably effective tool towards optimally managing high patient volumes in busy public health clinics. Since 2014, the El Salvador MOH has subsequently expanded the use and viewing audience of the TB educational video to include patients within the prison health clinics.
For the TB videography educational project to have a positive impact, we felt it was imperative that the content and delivery of information was medically accurate, culturally appropriate and in a format that is readily understandable by patients with differing degrees of health literacy. Showing recognizable national landmarks in the video and using the local Spanish dialogue enhanced the video's capacity to connect with viewers on a more personal level. Incorporating actual Salvadorian health providers and consenting former TB patients added authenticity to the video's educational message. Patient testimonials in the video, including personal experiences with TB and its treatment, resonated well with patients and family members. Such testimonials allowed patients to identify with certain emotional and physical commonalities shared by others with TB and reinforced a central theme that TB affects people of all economic, educational and professional backgrounds.
The battery powered portable DVD players enabled video viewings well outside of the TB clinics and into the homes of families and neighbors. As effective as videography-based health education can be, it should never replace the face-to-face discussions between health providers and their patients.
To address some of the equipment problems identified, new DVD players with a higher auditory volume capacity were subsequently delivered to the clinics. For expanded general public viewing from any computer or mobile device with internet access, the video has been uploaded onto the webpage of the El Salvador Ministry of Health National TB Program (http://www.salud.gob.sv/servicios/descargas/videos/ano-2014/category/947-tuberculosis-lo-que-usted-y-su-familia-deben-saber.html).
The study does have several limitations. Unfortunately, despite MOH involvement and direct communication with the participating TB clinics, not all clinics reported important metrics and outcome data, including rates of compliance to DOT and treatment completion rates. Pre- and post-video patient questionnaires were not uniformly conducted early on during the study period. The absence of a dedicated study coordinator on the ground to both directly administer patient questionnaires during the study period and ensure consistent reporting metrics among the participating TB clinics was a significant limitation to this project and can explain the variability in the observed assessments and limited quantified data.
We also acknowledge that the study observed outcomes, and effectiveness assessment were based on subjective impressions of patients, family members and observations reported by TB Clinic health providers, which in turn, can introduce notable bias and possible underreporting of the effects of this educational intervention. This initial pilot field study was done in a very resource-limited setting with very little financial support to implement more objective and comprehensive measurements of the effectiveness and impact of this educational intervention in the study subjects and overall TB-related health outcomes.
The follow-up survey in 2015 on a subset of patients, family members and TB clinic nurses, however, more objectively shows positive results that align with the overall impact impressions reported earlier during the study intervention. Indeed, patient and family responses had to be documented through discussions with the health providers and outreach workers since illiteracy is prevalent in this population. Patient illiteracy is a problem in many international underserved communities, and health providers within a busy clinic often did not have the time to assist patients with written questionnaires. Nevertheless, this initial study experience is a proof of concept that will be helpful in designing more rigorous prospective field studies with more objective metrics to accurately quantify the effectiveness and impact of this low-cost educational and patient-centered health care intervention.
5. Conclusion
Videography-based health education can be successfully implemented in busy and resource-limited outpatient settings and appears to be an effective and low-cost tool towards increasing patient, family and community education on TB. Whether in the medical clinic or home setting, videography-based education can improve patient satisfaction, treatment compliance, contact investigations, and concurrently help lower the false negative stigma of TB. Additional prospective studies to further evaluation and quantify the effectiveness and sustainable impact of videography-based patient and family TB education are warranted.
Authors' contributions
All listed authors/co-authors have provided substantial contributions to the design of the project, content of the video, interpretation of the data, and the drafting / revisions of the manuscript. All have provided final approval and accountability for this version of the manuscript to be published.
Contributor Information
John W. Wilson, Email: wilson.john@mayo.edu.
Julio Garay Ramos, Email: jgaray@salud.gob.sv.
Francisco Castillo, Email: fcastillo@salud.gob.sv.
Evelyn F. Castellanos, Email: castellanosflores_ob@yahoo.com.
Patricio Escalante, Email: escalante.patricio@mayo.edu.
References
- 1.World Health Organization. Global tuberculosis report 2015. Available from http://apps.who.int/iris/bitstream/10665/191102/1/9789241565059_eng.pdf.
- 2.World Health Organization. Media centre,tuberculosis, key facts. 2014 [updated March 2014; cited 2014 September 19, 2014]; Available from: http://www.who.int/mediacentre/factsheets/fs104/en/.
- 3.Martin LR, Williams S.L., Haskard K.B., Dimatteo M.R. The challenge of patient adherence. Ther Clin Risk Manag. 2005;1(3):189–199. [PMC free article] [PubMed] [Google Scholar]
- 4.Pronyk R.M., Makhubele M.B., Hargreaves J.R., Tollman S.M., Hausler H.P. Assessing health seeking behaviour among tuberculosis patients in rural South Africa. Int J Tuberc Lung Dis. 2001;5(7):619–627. [Research Support, Non-U.S. Gov't] [PubMed] [Google Scholar]
- 5.Eastwood S.V., Hill P.C. A gender-focused qualitative study of barriers to accessing tuberculosis treatment in The Gambia, West Africa. Int J Tuberc Lung Dis. 2004;8(1):70–75. [Comparative Study Research Support, Non-U.S. Gov't] [PubMed] [Google Scholar]
- 6.Kiwuwa M.S., Charles K, Harriet M.K. Patient and health service delay in pulmonary tuberculosis patients attending a referral hospital: a cross-sectional study. BMC Public Health. 2005;5:122. doi: 10.1186/1471-2458-5-122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Viney K.A., Johnson P, Tagaro M, Fanai S, Linh N.N., Kelly P. Tuberculosis patients' knowledge and beliefs about tuberculosis: a mixed methods study from the Pacific Island nation of Vanuatu. BMC Public Health. 2014;14:467. doi: 10.1186/1471-2458-14-467. [Research Support, Non-U.S. Gov't] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tasnim S, Rahman A, Hoque F.M. Patient's knowledge and attitude towards tuberculosis in an urban setting. Pulm Med. 2012;2012 doi: 10.1155/2012/352850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liefooghe R, Baliddawa J.B., Kipruto E.M., Vermeire C, De Munynck A.O. From their own perspective. A Kenyan community's perception of tuberculosis. Trop Med Int Health. 1997;2(8):809–821. doi: 10.1046/j.1365-3156.1997.d01-380.x. [Research Support, Non-U.S. Gov't] [DOI] [PubMed] [Google Scholar]
- 10.Rubel A.J., Garro L.C. Social and cultural factors in the successful control of tuberculosis. Public Health Rep. 1992;107(6):626–636. [Research Support, Non-U.S. Gov't Review] [PMC free article] [PubMed] [Google Scholar]
- 11.Hansel N.N., Wu A.W., Chang B., Diette G.B. Quality of life in tuberculosis: patient and provider perspectives. Qual Life Res. Apr 2004;13(3):639–652. doi: 10.1023/B:QURE.0000021317.12945.f0. [Research Support, Non-U.S. Gov't] [DOI] [PubMed] [Google Scholar]
- 12.World Health Organization. 2013 World Health Organization, Tuberculosis country profile, El Salvador. 2013 [October 26, 2014]; Available from: https://extranet.who.int/sree/Reports?op=Replet&name=%2FWHO_HQ_Reports%2FG2%2FPROD%2FEXT%2FTBCountryProfile&ISO2=SV&LAN=EN&outtype=html.
- 13.Alami N.N., Yuen C.M., Miramontes R., Pratt R., Price S.F., Navin T.R. Trends in tuberculosis—United States, 2013. MMWR morbidity and mortality weekly report. Atlanta, GA. 2014;63(11):229–233. [PMC free article] [PubMed] [Google Scholar]
- 14.Scott C., Kirking H.L., Jeffries C., Price S.F., Pratt R. Tuberculosis trends–United States, 2014. MMWR morbidity and mortality weekly report. Atlanta, GA. 2015;64(10):265–269. [PMC free article] [PubMed] [Google Scholar]
- 15.Centers for Disease Prevention and Control. Reported tuberculosis in the United States, 2014; Atlanta, GA: U.S. Department of Health and Human Services, CDC, October 2015.: Available from: http://www.cdc.gov/tb/statistics/reports/2014/pdfs/tb-surveillance-2014-report.pdf.
- 16.Wieland M.L., Nelson J., Palmer T., O'Hara C., Weis J.A., Nigon J.A. Evaluation of a tuberculosis education video among immigrants and refugees at an adult education center: a community-based participatory approach. J Health Commun. 2013;18(3):343–353. doi: 10.1080/10810730.2012.727952. [Evaluation Studies] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chavez V., Israel B., Allen A.J., 3rd, DeCarlo M.F., Lichtenstein R., Schulz A. A bridge between communities: video-making using principles of community-based participatory research. Health Promot Pract. 2004;5(4):395–403. doi: 10.1177/1524839903258067. [DOI] [PubMed] [Google Scholar]
- 18.Barber J.H., McEwan C., Yates B.D. 'Video, health education and the general practitioner contract'. Health Bull. 1995;53(5):326–333. [Research Support, Non-U.S. Gov't] [PubMed] [Google Scholar]
- 19.Wang D.S., Jani A.B., Sesay M., Tai C.G., Lee D.K., Echt K.V. Video‐based educational tool improves patient comprehension of common prostate health terminology. Cancer. 2015;121(5):733–740. doi: 10.1002/cncr.29101. [DOI] [PubMed] [Google Scholar]
- 20.Ata A. Guía para el control de la tuberculosis en poblaciones privadas de libertad de América Latina y el Caribe: OPS; 2008.
- 21.World Health Organization . Treatment of tuberculosis: guidelines. 4th ed. World Health Organization; Geneva: 2010. Stop TB initiative (World Health Organization) [Google Scholar]
- 22.Liefooghe R, Michiels N, Habib S, Moran MB, De Muynck A. Perception and social consequences of tuberculosis: a focus group study of tuberculosis patients in Sialkot, Pakistan. Soc Sci Med. 1995;41(12):1685–1692. doi: 10.1016/0277-9536(95)00129-u. [Research Support, Non-U.S. Gov't] [DOI] [PubMed] [Google Scholar]
- 23.Diwan VK, Thorson A. Sex, gender, and tuberculosis. Lancet. 1999;353(9157):1000–1001. doi: 10.1016/S0140-6736(99)01318-5. [DOI] [PubMed] [Google Scholar]