Abstract
Objective
The National Comprehensive Cancer Network (NCCN) has established guidelines for treating epithelial ovarian cancer (EOC) which includes cytoreductive surgery and platinum and taxane-based chemotherapy (CT). The objective of this study was to determine the reasons for failure to deliver NCCN-adherent care at an NCCN cancer center serving a diverse racial and socioeconomic population.
Methods
Medical records of women with EOC diagnosed between 2004–2009 were reviewed for demographic, clinical, tumor, treatment, and survival data. Independent reviewers determined if their treatment met criteria for being NCCN-adherent. Progression-free (PFS) and overall survival (OS) was calculated with Kaplan-Meier estimates and compared with the log-rank test.
Results
367 patients were identified. 79 (21.5%) did not receive NCCN-adherent care. Non-adherent CT in 75 patients was the most common reason for failure to receive NCCN-adherent care. 39 patients did not complete CT due to treatment toxicities or disease progression. 12 patients received single agent CT only and 4 received no CT due to comorbidities. 2 patients declined CT. 18 patients died in the postoperative period without receiving CT. 8 patients did not undergo cytoreduction due to disease progression or comorbidities. PFS and OS were improved in the NCCN-adherent cohort (PFS 5.7 vs. 18.3 months, p<.005) (OS 11.4 vs. 49.5 months, p<.005).
Conclusions
The vast majority of patients at an NCCN cancer center received NCCN-adherent treatment. Reasons for failure to receive NCCN-adherent care were variable, but most did not receive chemotherapy in accordance with guidelines due to comorbidities or disease progression.
Keywords: Epithelial ovarian cancer, NCCN-adherent care, Treatment disparities
Background
In order to improve the lives of women with cancer, improving the delivery of quality cancer care is of the utmost importance. National standards for quality care in the treatment of various malignancies, including epithelial ovarian cancer (EOC), has been provided through the National Comprehensive Cancer Network (NCCN) guidelines (1). These guidelines, established by an expert panel after rigorous review of the literature, provide algorithms for the surgical and chemotherapeutic treatment approaches for the management of both primary and recurrent disease. In addition to listing acceptable strategies, these algorithms also grade recommendations based on the data that lead to the determination.
The importance of adherence to national guidelines has been highlighted in population-based studies from the National Cancer Data Base (NCDB), which demonstrate that unfortunately, only 43–53%% of ovarian cancer patients receive NCCN-adherent care nationwide (2, 3). Survival is improved in patients who receive adherent care (2). Age, stage, histology, annual hospital case volume, household income, race, and insurance status are all independently associated with adherence to NCCN care. Although associative, it is unclear how these factors might cause deviation from the receipt of standard of care. Single institution reports have shown improved adherence to guidelines when care is delivered at tertiary referral center (4, 5).
Additional work from Bristow and colleagues utilized the California Cancer Registry and evaluated outcomes in 13,321 consecutive patients over an eight-year period from 1999 to 2006 (6). Although California possesses four of the twenty-three member institutions of the NCCN, still only 37.2% of patients received care that was adherent with NCCN recommendations. Importantly, this recent report demonstrated that both higher volume physicians (> 10 ovarian cancer cases a year), and higher volume hospitals (> 20 ovarian cancer cases annually), were associated with more adherent care. This corroborates with earlier studies that have shown that higher ovarian cancer surgical volume is associated with better surgical and oncologic outcomes (7–10). Nonetheless, one limitation of this work was the absence of physician specialty (gynecologic oncologist versus other) as this information is not collected in the registry.
Accordingly, it is evident based on population-based reports from the state and national level that adherence to NCCN guidelines is not universal (2, 6). Moreover, while patients who receive NCCN-adherent care have improved survival compared to those who do not, several factors associated with this are yet to be fully elucidated. Therefore, it is imperative that we understand why women are not receiving standard of care. The objective of the current study was to examine the reasons that prevented patients from receiving NCCN-adherent care at a large NCCN cancer center serving a diverse racial and socioeconomic population.
Methods
Subjects
The study was carried out in accordance with the standards of the Institutional Human Subjects Protection Review Board at the University of Alabama at Birmingham (UAB). Eligible subjects included women diagnosed with EOC between 2004–2009 with treatment at our institution. Subjects were identified through the comprehensive cancer center tumor registry, which captures all new cancer diagnoses seen within the UAB health system.
Study Design
Our primary objective was to retrospectively report our rate of NCCN-adherent treatment of ovarian cancer in a large cohort of patients and determine the reasons why there were deviations from the guidelines. Our secondary objective was to compare survival between groups as well as the factors associated with receipt of standard of care.
Patient records were reviewed for demographics (including age, self-identified race, insurance status, distance from the hospital), tumor characteristics (stage, grade, histology), treatment (surgery and chemotherapy), progression-free survival (PFS) and overall survival (OS). NCCN-adherent care was defined as the receipt of a combination of surgical cytoreduction (or surgical staging for early stage disease) and at least 6 cycles of platinum and taxane-based chemotherapy for advanced stage disease (11). Patients whose initial surgery was performed at an outside institution were excluded for analysis. For stage IA and IB, grade 1 or 2 disease, chemotherapy was not necessary to be considered standard of care, although chemotherapy for grade 2 tumors in this group was considered acceptable. Neoadjuvant chemotherapy was considered NCCN-adherent if it was followed by an interval cytoreductive procedure. Indications for failure to receive standard of care was determined through a thorough review of the physician’s documented assessment and plan. Because this was a subjective data point, two independent reviewers abstracted this data from each patient chart and a third reviewer resolved any discrepancies.
PFS was calculated from the time of initiation of chemotherapy until disease recurrence or progression according to clinical assessment, rising CA-125, or radiographic evidence of recurrence. OS was calculated from initiation of chemotherapy until last known follow-up or death from any cause.
Statistical Analysis
Chi-square (χ2) test or Fisher’s exact test for categorical variables and the t-test for continuous variables were used to compare factors between patients who did and did not receive standard of care. Kaplan-Meier survival estimates were performed and differences in survival were compared with the log-rank test. A value of p<0.05 was considered statistically significant and all tests were two-sided. All analyses were performed using SPSS statistical software version 21(IBM, Armonk, NY).
Results
367 patients met inclusion criteria. Overall, 288 patients (78.5%) received NCCN-adherent care, leaving 79 that did not receive adherent care. In terms of the components of adherent care for the entire study population, 359 patients (97.8%) received NCCN-adherent surgery and 293 patients (79.8%) received NCCN-adherent chemotherapy. Four patients (1.1%) received neither adherent surgery nor chemotherapy for their disease. All patients were treated by a gynecologic oncologist. 44 patients (12%) participated in a clinical trial as part of their upfront therapy.
Women who received NCCN-adherent care were younger, with a mean age of 61.9 versus 69.0 years (p=0.009) (Table 1). Stage distribution also varied, with more patients in the NCCN-adherent cohort having stage I or II disease (p=0.04). Specifically, 78 of 87 patients (89.6%) with stage I or II disease had NCCN-adherent care (Table 1). Patients who received NCCN-adherent care were also more likely to have private insurance and less likely to have Medicare or Medicaid only (p=0.001). Overall, 267 patients (72.8%) were optimally cytoreduced to <1 cm of residual disease. Patients who received NCCN-adherent care were more likely to have been optimally cytoreduced (77.8% vs. 54.4%, p<0.001). 13 patients (3.5%) required upper abdominal surgery and 104 patients (28.3%) underwent a small and/or large bowel resection as part of their cytoreductive surgery. Race, BMI, histology, and distance from an NCCN cancer center were not different between groups.
Table 1:
Comparison of patient characteristics between cohorts
| NCCN-adherent care (n=288) | NCCN non-adherent care (n=79) | p-value | |
|---|---|---|---|
| Age (SD) | 61.9 (11.0) | 69.0 (13.2) | 0.009 |
| BMI (SD) | 28.1 (6.3) | 28.2 (6.5) | NS |
| Race | NS | ||
| Black | 37 (12.8%) | 17 (21.5%) | |
| White | 247 (85.8%) | 61 (77.2) | |
| Other | 4 (1.4%) | 1 (1.3%) | |
| Stage | 0.04 | ||
| I | 21 (7.3%) | 2 (2.5%) | |
| II | 57 (19.8%) | 7 (8.9%) | |
| III | 185 (64.2%) | 61 (77.2%) | |
| IV | 25 (8.7%) | 9 (11.4%) | |
| Surgical cytoreduction | <0.001 | ||
| Optimal (<1cm) | 224 (77.8%) | 43 (54.4%) | |
| Sub-Optimal (>1cm) | 64 (22.2%) | 36 (45.6%) | |
| Histology | NS | ||
| Papillary serous | 183 (63.5%) | 58 (73.4%) | |
| Clear cell | 11 (3.8%) | 1 (1.3%) | |
| Endometrioid | 38 (13.2%) | 5 (6.3%) | |
| Mucinous | 8 (2.8%) | 4 (5.1%) | |
| Adenocarcinoma NOS | 7 (2.4%) | 3 (3.8%) | |
| Other (mixed, signet ring) | 41 (14.2%) | 8 (10.1%) | |
| Distance from Cancer Center (miles, SD) | 82.4 (73.4) | 87.5 (76.7) | NS |
| Insurance | 0.001 | ||
| Private only | 123 (42.7%) | 20 (25.3%) | |
| Medicare only | 27 (9.4%) | 21 (26.6%) | |
| Medicare + Supplement | 104 (36.1%) | 28 (35.4%) | |
| Medicaid only | 9 (3.1%) | 3 (3.8%) | |
| No Insurance | 10 (3.5%) | 4 (5.1%) | |
| Unknown | 15 (5.2%) | 3 (3.8%) | |
NS = Non-significant, NCCN = National Comprehensive Cancer Network, SD = Standard Deviation
Reasons for failure to receive adherent care were variable and were divided into surgical and chemotherapeutic reasons (Table 2). Of the 8 patients who did not receive adherent surgery, 6 received neoadjuvant chemotherapy and never underwent surgery due to comorbidities (n=4) or disease progression (n=2). Two patients had evidence of a bowel perforation on presentation and underwent a diverting intestinal procedure and never had an attempt at cytoreductive surgery.
Table 2:
Reasons for NCCN non-adherence (N= 79)
| Non-adherent surgical treatment (N=8)* | No (% of all pts) |
| Neoadjuvant CT without surgery due to disease progression | 2 (2.5%) |
| Neoadjuvant CT without surgery due to patient comorbidities | 4 (5.1%) |
| Diverting bowel surgery only, no CT or debulking surgery performed | 2 (2.5%) |
| Non-adherent CT treatment (N=75) | No (% of all pts) |
| Postoperative death | 18 (22.8%) |
| Patient declined adjuvant CT | 2 (2.5%) |
| Started CT, but did not receive all 6 cycles due to poor tolerance of CT | 29 (36.7%) |
| Started CT, but did not receive all 6 cycles due to disease progression | 10 (12.7%) |
| Single agent CT only due to patient comorbidities | 12 (15.2%) |
| No CT ever given due to comorbidities | 4 (5.1%) |
Total of non-adherence is greater than 79 as 4 patients with non-adherent surgery also had non-adherent CT
CT = chemotherapy
Of the 75 patients who did not receive NCCN-adherent chemotherapy, 51 received some chemotherapy but were either given single agent chemotherapy secondary to medical comorbidities (n=12) or were unable to complete their course due to poor tolerance (n=29) or disease progression (n=10). 24 patients never received chemotherapy and the reasons were variable. 18 patients had a postoperative death prior to initiation of chemotherapy, 2 patients declined treatment, and 4 patients were never given chemotherapy due to comorbidities.
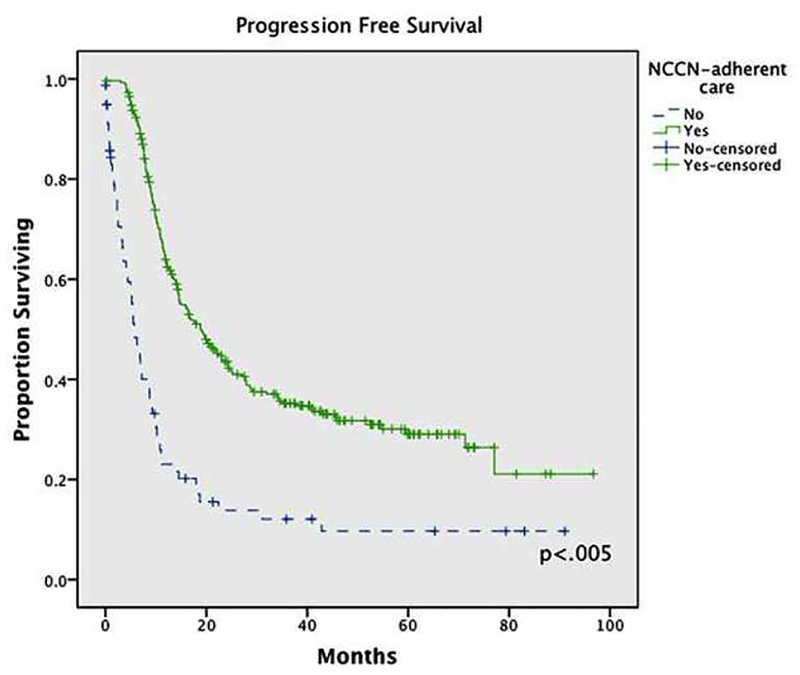
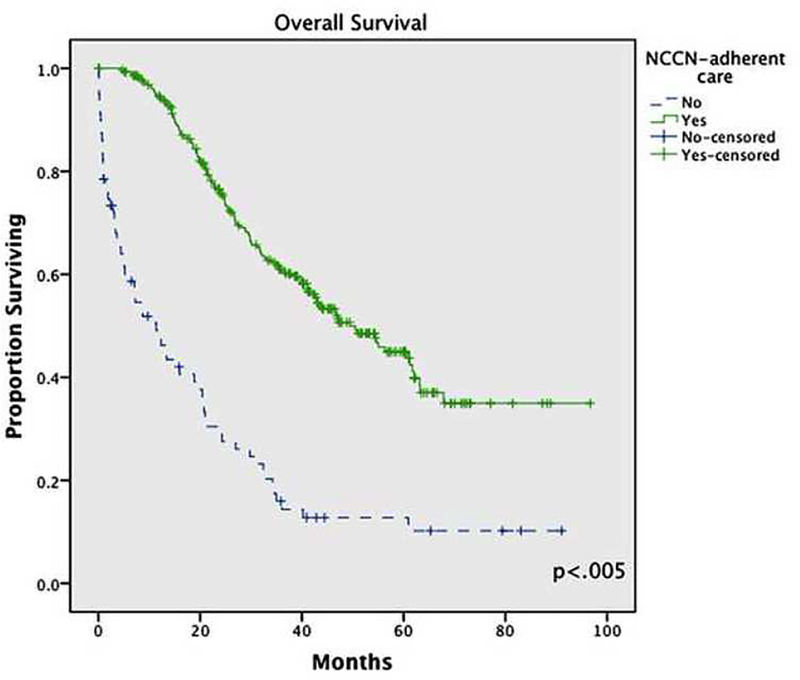
PFS and OS were significantly improved in the cohort of patients who received NCCN-adherent care. Specifically, PFS was 18.8 vs. 5.7 months (p<0.005) and OS was 49.5 vs. 11.4 months (p<0.005) (Figure 1).
Figure 1:
Progression-free survival based on receipt of NCCN-adherent care
Conclusions
In this retrospective cohort study, we investigated the administration and receipt of the standard of care for EOC, as defined by the NCCN guidelines. In cases where non-adherent care was rendered, we investigated the rationale for treatment decisions. Importantly, we found that 78.5% of our patients underwent cytoreductive surgery and received 6 cycles of platinum and taxane-based chemotherapy in accordance with the NCCN guidelines. The most common reason women did not receive NCCN-adherent care was failure to complete chemotherapy due to comorbidities or disease progression.
Bristow and colleagues have reported NCCN compliance rates around 40% both from a large state cancer registry as well as from a national cancer registry (2, 6). Although their studies are potentially limited by lack of information regarding treatment details such as provider specialty and use of second line therapies, the results are concerning. While all patients may not be able to receive NCCN-adherent care because of underlying medical conditions, factors such as race, socioeconomic status, or distance from a large volume center are unacceptable reasons for lack of adherence. These population-based studies that highlight the low national rates of NCCN-adherent care suggest that we are failing at a national level to administer the highest evidence based treatment to the majority of women with epithelial ovarian cancer. One major conclusion from a variety of studies examining the effects of institutional and provider surgical volume suggest that more comprehensive surgical care is rendered at higher volume referral centers (8, 9, 12). However, we have demonstrated in this study that even at high volume NCCN-cancer centers, not all women receive NCCN adherent care. Notably, in our report, we required completion of six cycles of chemotherapy to be considered adherent. In the previously mentioned population-based studies, care was considered to be adherent if the patient received at least one cycle of chemotherapy. If we had included receipt of one cycle of chemotherapy, our rate of adherence would be even higher at 85%.
As the delivery of health care continues to evolve, we will often be held to standard of care as defined by a single objective metric. Results from our study demonstrate it is not practical to administer guideline-based treatment for all patients with EOC. Advanced stage of disease, patient comorbidities, postoperative morbidity and mortality, and poor chemotherapy tolerance all affect delivery of care and adherence. This would suggest that the optimal metric for receipt of adherent care might be between 75–85% rather than100%.
Compared to prior work in ovarian cancer that has evaluated the topic of the delivery of NCCN-adherent care, the current study has several strengths. First, at our NCCN Center, all care was provided by fellowship trained gynecologic oncologists, potentially eliminating this source of bias as physician specialty has not previous been reported. Second, we evaluated specific reasons why patients did not receive care that was adherent with recommendations from the NCCN. Third, standardized definitions of adherence were utilized and confirmed by at least two independent reviewers.
Potential limitations for this retrospective study must always be considered including unmeasured confounding and other sources of potential bias. Although UAB is the only NCCN institution in the state of Alabama, we do not provide care to all patients with EOC in the state and thus the exclusion of these patients may have impacted our results.. Second, the requirement for patients to have received at least six cycles of platinum and taxane-based chemotherapy may be viewed as a weakness in the study design. Finally, secondary to the single institution nature of the study, widespread generalization of our findings may not be appropriate. Importantly, we were unable to assess from our operative reports how many patients were cytoreduced to no visible disease. Finally, although the reported enrollment in clinic trials during the study period is low, the upfront cooperative group trials in this era (GOG protocol 218 and 252) included regimens with prolonged treatment schedules which, secondary to travel limitations was prohibitive for many of our patients who lived far from the cancer center.
Recently at UAB we have initiated a quality improvement (QI) initiative based on a review of previous data in advanced stage EOC patients. The purpose of this QI project has several objectives including: (1) an increase in the optimal cytoreduction rates; (2) an increase in the use of intraperitoneal chemotherapy; (3) judicious use of neoadjuvant chemotherapy in patients thought to have a low likelihood of a primary optimal cytoreduction; (4) prospective collection of operative morbidity, and (5) prospective tracking of both eligibility and enrollment on a clinical trial. In order to accomplish these goals, a comprehensive review of available clinical information including: assessment of performance status, physical examination findings, laboratory values, and radiographic images are incorporated into a pre-operative prediction by the attending physician on the performance of an optimal cytoreduction. Importantly, this standardized approach should allow both a prospective determination of NCCN adherence as well as an improvement in the same metric.
In conclusion, at our NCCN Comprehensive Cancer Center compliance with NCCN care was 78.5%. The most common reason for non-adherence were deviations in administration of platinum and taxane-based chemotherapy. The prospective determination of the actual NCCN-adherent care is vital to have a metric with which further improvement can be refined. A multi-institutional study that incorporates a similar approach at all 23 NCCN cancer centers should be considered.
Figure 2:
Overall survival based on receipt of NCCN-adherent care
Highlights.
The vast majority of patients at an NCCN cancer center received treatment for epithelial ovarian cancer in accordance with NCCN standards (78.5%).
The most common reason women did not receive NCCN-adherent care was failure to complete chemotherapy due to either comorbidities or disease progression.
Women who received NCCN-adherent care were more likely to be younger, have early stage disease, and have private insurance.
Footnotes
Disclosure: The authors declare there are no conflicts of interests.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Morgan RJ Jr., Alvarez RD, Armstrong DK, Burger RA, Chen LM, Copeland L, et al. Ovarian cancer, version 2.2013. Journal of the National Comprehensive Cancer Network : JNCCN. 2013. October 1;11(10):1199–209. [DOI] [PubMed] [Google Scholar]
- 2.Bristow RE, Powell MA, Al-Hammadi N, Chen L, Miller JP, Roland PY, et al. Disparities in ovarian cancer care quality and survival according to race and socioeconomic status. Journal of the National Cancer Institute. 2013. June 5;105(11):823–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chase DM, Fedewa S, Chou TS, Chen A, Ward E, Brewster WR. Disparities in the allocation of treatment in advanced ovarian cancer: are there certain patient characteristics associated with nonstandard therapy? Obstetrics and gynecology. 2012. January;119(1):68–77. [DOI] [PubMed] [Google Scholar]
- 4.Bristow RE, Ueda S, Gerardi MA, Ajiboye OB, Ibeanu OA. Analysis of racial disparities in stage IIIC epithelial ovarian cancer care and outcomes in a tertiary gynecologic oncology referral center. Gynecol Oncol. 2011. August;122(2):319–23. [DOI] [PubMed] [Google Scholar]
- 5.Phippen NT, Barnett JC, Lowery WJ, Miller CR, Leath CA 3rd. Surgical outcomes and national comprehensive cancer network compliance in advanced ovarian cancer surgery in a low volume military treatment facility. Gynecol Oncol. 2013. July 16. [DOI] [PubMed] [Google Scholar]
- 6.Bristow RE, Chang J, Ziogas A, Anton-Culver H. Adherence to treatment guidelines for ovarian cancer as a measure of quality care. Obstetrics and gynecology. 2013. June;121(6):1226–34. [DOI] [PubMed] [Google Scholar]
- 7.Bristow RE, Palis BE, Chi DS, Cliby WA. The National Cancer Database report on advanced-stage epithelial ovarian cancer: impact of hospital surgical case volume on overall survival and surgical treatment paradigm. Gynecol Oncol. 2010. September;118(3):262–7. [DOI] [PubMed] [Google Scholar]
- 8.Mercado C, Zingmond D, Karlan BY, Sekaris E, Gross J, Maggard-Gibbons M, et al. Quality of care in advanced ovarian cancer: the importance of provider specialty. Gynecol Oncol. 2010. April;117(1):18–22. [DOI] [PubMed] [Google Scholar]
- 9.Goff BA, Matthews BJ, Larson EH, Andrilla CH, Wynn M, Lishner DM, et al. Predictors of comprehensive surgical treatment in patients with ovarian cancer. Cancer. 2007. May 15;109(10):2031–42. [DOI] [PubMed] [Google Scholar]
- 10.Goff BA, Matthews BJ, Wynn M, Muntz HG, Lishner DM, Baldwin LM. Ovarian cancer: patterns of surgical care across the United States. Gynecol Oncol. 2006. November;103(2):383–90. [DOI] [PubMed] [Google Scholar]
- 11.Morgan RJ Jr., Alvarez RD, Armstrong DK, Chen LM, Copeland L, Fiorica J, et al. Ovarian cancer clinical practice guidelines. Journal of the National Comprehensive Cancer Network : JNCCN. 2004. November;2(6):526–47. [DOI] [PubMed] [Google Scholar]
- 12.Bristow RE, Puri I, Diaz-Montes TP, Giuntoli RL, Armstrong DK. Analysis of contemporary trends in access to high-volume ovarian cancer surgical care. Annals of surgical oncology. 2009. December;16(12):3422–30. PubMed PMID: 19711131. [DOI] [PubMed] [Google Scholar]