Abstract
Background
This pilot study aimed to investigate the anatomical site variation of water content of the stratum corneum (SC) on the body by measuring skin capacitance with the Epsilon, a new generation corneometer with multiple sensors. Secondly, values of the Epsilon were compared to values measured by conventional single sensor corneometers.
Methods
The hydration status of SC was measured in 15 healthy Caucasian volunteers with the Epsilon at five body sites (cheek, lower forearm, mid‐calf, lower back and abdomen). Transepidermal water loss (TEWL) was measured with the Aquaflux to get more insight into the condition of the skin barrier. A literature search was performed to compare Epsilon values with conventional corneometers.
Results
The tested anatomical locations showed significant differences in water content (P < 0.001) with large interindividual variations; highest values were found in the cheek (11.64ε) and lowest values in the mid‐calf (4.43ε). No correlation between water content and TEWL was found. In general, Epsilon values were lower compared to values of conventional corneometers, with a similar trend.
Conclusion
This pilot study showed significant variations in water content at different skin locations measured by the Epsilon. Moreover, the Epsilon measured consistent lower values compared to single sensor corneometers. Further validation of the device is recommended.
Keywords: corneometer, Epsilon, skin barrier, skin capacitance, water content
1. INTRODUCTION
The stratum corneum (SC) plays an important role in skin surface management by protecting the human body against microorganisms and guaranteeing skin barrier function by regulation of moisture grade and temperature.1, 2, 3 SC imbalance can lead to various inflammatory skin diseases, for instance constitutional eczema. The structure and barrier function of the SC can be studied noninvasively with different measurement tools; water content and transepidermal water loss (TEWL) are two commonly evaluated skin variables.4 A corneometer measures the water content by measuring electrical capacitance of the skin surface. Until today, single sensor corneometers are used, showing significant differences in water content between various skin locations.5, 6, 7 Recently, the Epsilon, a multi‐sensor corneometer with 76 800 sensors at one probe was introduced.8 Due to this increase in sensors, multiple measurements take place at once. In addition, options for analysis are integrated in this device and water content based images can be obtained.
To the best of our knowledge, this is the first study to investigate the anatomical site variation of water content in human skin with the Epsilon. Also, measured water content values of the Epsilon were compared to values measured by conventional single sensor corneometers by performing a literature search.
2. MATERIALS AND METHODS
2.1. Participants
Fifteen healthy Caucasian volunteers (nine women and six men; median age 26 years; range 21‐62 years) participated in this explorative study. Informed consent was obtained. The study was approved by the local medical ethics committee and conducted according to the principles of the Declaration of Helsinki. Exclusion criteria were as follows: age <18 years, signs of skin diseases or open wounds at the measurements sites, use of immunosuppressive medication, diagnosed with inflammatory dermatoses. Participants were asked not to use cream or body lotion at the day of measurements.
2.2. Technical device specifications
Water content of the SC was measured with the Epsilon (Epsilon E100, Biox, UK). This corneometer measures calibrated dielectric permittivity (dielectric constant, ε) through the SC and consists of a probe of 76 800 sensors with a sensing area of 12.8 × 15 mm, depth resolution of 20 μm and spacial resolution of 50 μm.8, 9 The hardware and the probe of the Epsilon are shown in Figure 1A‐D. Due to the multiple sensors, skin surface hydration can be mapped, taking skin relief and variable distribution of sweat glands into account (Figure 1E,F). This allows measurement of more average values and exclusion of regions with poor physical contact between sensor and skin.10 Moreover, the Epsilon is the only corneometer with a linearized and calibrated response, allowing consistent quantitative image evaluation.9 In this study, the standardized Burst mode option was used with a 5 seconds delay after first skin contact (to rule out initial variations in occlusion), a frame interval of 1‐second, and a total measurement frame of 30 seconds.
Figure 1.
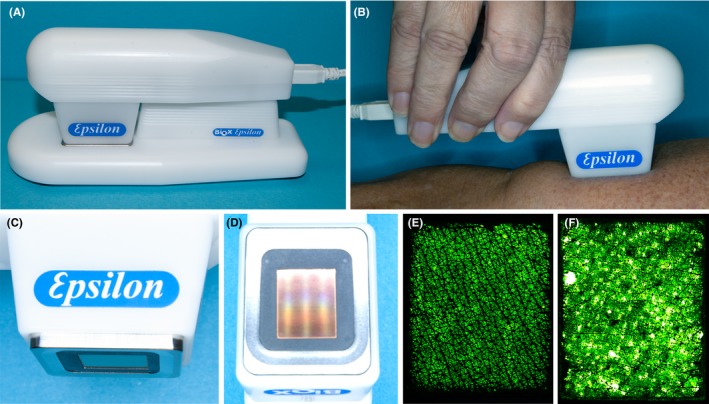
The Epsilon is a novel instrument for measuring near‐surface dielectric permittivity (ε) and contact imaging of the skin. Its proprietary electronics and signal processing algorithms map the sensor's nonlinear signals onto a calibrated scale for measuring properties such as stratum corneum hydration. A, The Epsilon instrument on the parking stand. B, A measurement performed on the inner arm. C, Close‐up of the Epsilon measurement head with the metal bezel. D, The sensor surface embedded in an epoxy frame. E, Typical contact image of the inner forearm skin. F, A contact image of the skin in the face with visible sweat gland activity
To investigate the overall SC barrier function, TEWL was measured with the Aquaflux (AquafluxAF200, Biox, UK). The closed measurement chamber of the Aquaflux contains sensors for relative humidity and temperature.8, 11 After calibration, measurements were performed with standard settings and a maximum measurement time of 80 seconds. The mean TEWL value was based on ten measure points, within a humidity degree of maximum 50%.
2.3. Study procedure
In each participant, water content and TEWL were investigated at five anatomical locations: cheek, first 1/3 of the flexor surface of the lower forearm, mid‐calf, lower back and abdomen (Figure 2). For water content, one Burst mode measurement per body site was performed; for TEWL, the average of three measurements per body site was obtained. Standardized environmental circumstances were created; room temperature was kept constant at 20°C and exposed skin was air‐acclimatized for at least 5 minutes prior to measurements.
Figure 2.
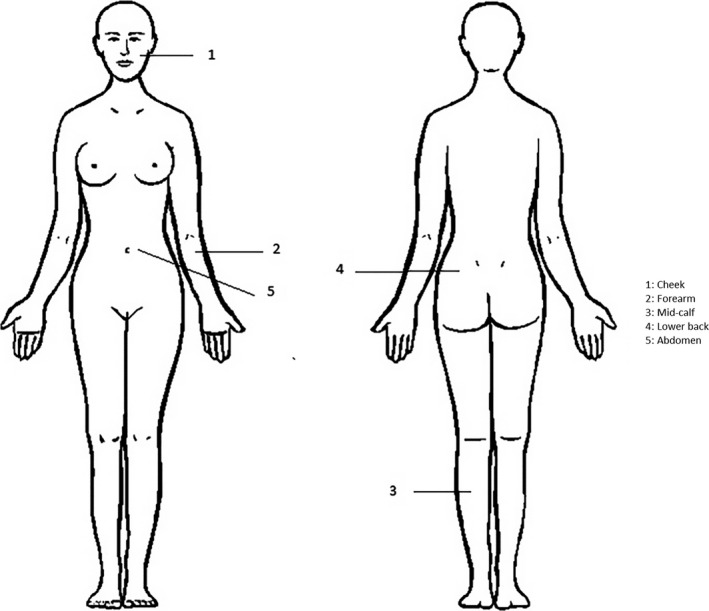
Measurement locations of water content and transepidermal water loss (TEWL)
2.4. Statistics
Burst mode results from the Epsilon from all body sites were used to create regression functions and y‐axis intersections were calculated. Statistical analysis was done with SPSS Statistics 22 (IBM Corporation, Armonk, New York). A Kruskal‐Wallis test with Dunn‐Bonferroni post hoc method was performed to demonstrate possible differences between the water content among the body sites. A relationship between water content and TEWL was investigated using Pearson correlation analysis. Tests were performed at 0.05 significance level.
2.5. Comparison with conventional corneometers
To compare the Epsilon results with conventional corneometer values, a PubMed search was performed. Study inclusion criteria were as follows: in vivo setting, healthy/normal human skin, nonexperimental setting OR use of a baseline control area in case of an intervention with topical therapies. Studied body sites preferably corresponded to the body sites chosen in this pilot study.
3. RESULTS
3.1. Anatomical variation in water content
The water content differed significantly between the five body sites (P < 0.001). As Figure 3 shows, the cheek had the highest water content (median 11.64ε), followed by the forearm (9.35ε), abdomen (7.45ε), lower back (7.07ε) and mid‐calf (4.43ε). Post hoc analysis revealed that the water content of the mid‐calf was significantly lower than the water content of the cheek (P < 0.001) and the forearm (P < 0.001). Additionally, a large interindividual variation in water content among the various skin locations was seen. There was no significant correlation between water content (measured by Epsilon) and TEWL (r = 0.194, n = 75, P = 0.095).
Figure 3.
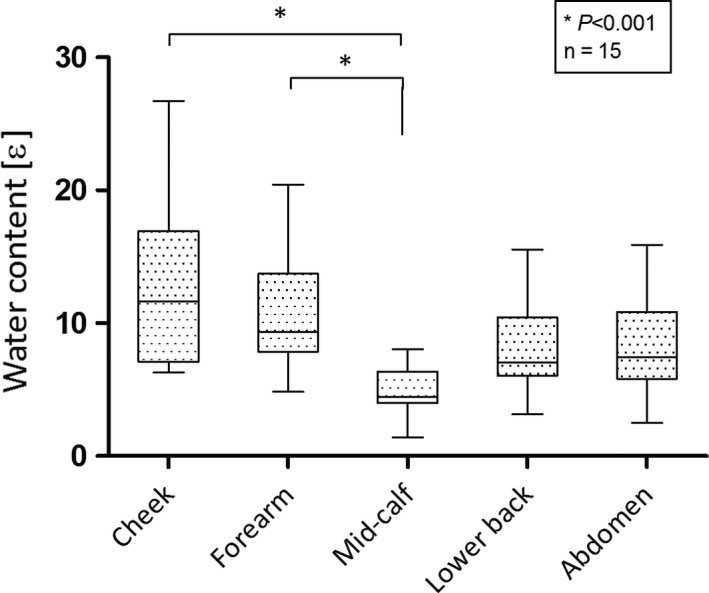
Water content at five body sites measured with the Epsilon. The values are expressed as median with interquartile range and range (minimum‐maximum)
3.2. Comparison with conventional corneometers
Table 1 shows literature‐based reference values of the water content with single sensor corneometers. In general, single sensor corneometers showed higher water content values than the Epsilon. In line with the Epsilon, also conventional corneometers measured lower values of the calf compared to the cheek and forearm.
Table 1.
Overview of water content values measured with single sensor corneometers
| Study | Device | Population | Skin location | |||
|---|---|---|---|---|---|---|
| Forehead (a.u.) | Cheek (a.u.) | Forearm (a.u.) | Calf (a.u.) | |||
| O'goshi et al5 |
Corneometer CM820 Corneometer CM82 Corneometer CM810 |
53 healthy volunteers |
74 (38‐122)a 72 (29‐113)a 78 (41‐131)a |
75 (37‐100) 74 (24‐96) 81 (33‐104) |
65 (43‐115) 65 (50‐100) 71 (52‐113) |
50 (28‐90) 49 (29‐90) 50 (27‐95) |
| Egawa et al17 | Corneometer CM825 | 45 healthy volunteers |
Winter:
36 ± 11b Spring: 37 ± 11b Autumn: 48 ± 9b Summer: 50 ± 11b |
Winter: 37 ± 9 Spring: 37 ± 6 Autumn: 38 ± 10 Summer: 47 ± 8 |
||
| O'goshi et al6 |
Skicon‐100c Skicon‐200EX |
26 healthy volunteers | 73 ± 52 (16‐369)a
151 ± 86 (27‐414)a |
50 ± 27 (11‐123) 80 ± 56 (27‐272) |
26.5 ± 31 (3‐153) 37.5 ± 71 (9‐425) |
|
| Algiert‐Zielińska et al22 | Corneometer CM825 | 10 healthy volunteers |
Left side: 46.67 ± 10 (28.1‐65.35)b Right side: 51.04 ± 12.50 (30‐64.64)b |
Left side: 39.77 ± 13.78 (19.60‐59.52 Right side: 44.2 ± 12.65 (27.18‐66.72) |
||
| Kleesz et al12 | Corneometer CM825 | 125 healthy volunteers | 75 ± 13 b | 72 ± 16 | 62 ± 13 | 58 ± 10 |
| de Farias Pires et al23 | Corneometer CM820 | 1339 healthy volunteers |
Female:
37 (9‐78)a Male: 28 (5‐66)a |
Female: 32 (10‐56) Male: 27 (2‐56) |
||
| Young et al24 | Corneometer CM825 | 21 healthy volunteers | 25 (24.5‐25.5)b | |||
| Marrakchi et al25 | Corneometer CM 420 | 20 healthy volunteers |
24‐34 y: 89.33 ± 12.7b 66‐83 y: 76.90 ± 18.2b |
24‐34 y: 87.40 ± 12.4 66‐83 y: 84.00 ± 16.9 |
24‐34 y: 81.70 ± 11.1 66‐83 y: 95.10 ± 7.1 |
|
| Fluhr et al26 | Corneometer CM825 | Seven healthy volunteers | 46.4 ± 6.5b | |||
| Lodén et al27 | Corneometer CM820 | 17 healthy volunteers | 70 (69‐82)a | |||
| Esposito et al28 | Corneometer CM820 | 10 healthy volunteers | 22 (20‐24)b | |||
| Cheng et al29 | Corneometer CM825 | 30 healthy volunteers | 55 ± 9b | 55 ± 8 | ||
| Hillebrand et al30 | Corneometer 820PC | 602 healthy females |
5‐15 y:
59.90 ± 11.7b 25‐35 y: 76.87 ± 10.0b 45‐54 y: 78.74 ± 10.8b 55‐65 y: 77.48 ± 11.9b |
5‐15 y: 48.43 ± 4.30 25‐35 y: 54.82 ± 6.0 45‐54 y: 57.59 ± 6.7 55‐65 y: 60.03 ± 6.2 |
||
| Agache et al31 | Corneometer CM820 | 20 healthy volunteers | 55.45 ± 2b | |||
| Richters et al20 | Corneometer CM825 | 30 volunteers with nonsensitive skin | 37.9 (9.0‐62.3)a | 31.7 (19.4‐55.6) | ||
a.u., arbitrary units.
Words in italic describe specific conditions/subgroups studied.
Median ± SD (range).
Mean ± SD (range).
Measures skin conductance; close correlation to skin capacitance.16
4. DISCUSSION
This pilot study is the first to measure water content of the SC in different body sites with the Epsilon. Our findings showed significant differences among the body sites, in correspondence with previous studies that also showed this trend.5, 6, 7, 12, 13 Many factors could influence these regional differences, for example, variations in the presence of sebaceous glands and lipids, natural moisturizing factor (NMF), size of corneocytes, exogenous compounds on skin surface and occlusion.4, 12, 14 Also, SC thickness variation could play a role; the smallest SC cell number is found in genital skin, followed by the face, neck, scalp, trunk, extremities and palmoplantar region.4, 14, 15 Moreover, skin surface hydration gradually increases in deeper layers of the SC, reaching a certain high level in the fully hydrated epidermis.16, 17 It is therefore more likely to measure water content in deeper and more hydrated layers of skin with thinner SC (eg, cheek), resulting in higher values.
Another important finding was that water content values of the Epsilon were lower compared to values of conventional corneometers. First, it is important to bear in mind that Epsilon measurement units are displayed using a calibrated dielectric permittivity scale (ε) rather than an arbitrary scale (a.u.) as used in conventional corneometers. As both instrument types use the same capacitance measurement principle, they should correlate well; this was already shown by one‐to‐one testing of both devices on the volar forearm of healthy volunteers.18 With the multisensory character of the Epsilon, the sensing depth will probably be more superficial compared to conventional corneometers, which make one big electrical loop through the skin. This increases the chance that Epsilon measurements are confined to the relatively “dry” SC only. Another advantage of the Epsilon is the Burst mode setting, correcting for time‐dependent skin occlusion differences, while conventional corneometers perform single time point measurements. Thirdly, due to the “skin mapping” character of the Epsilon, the number of values in one measurement can be averaged. All of the above could potentially lead to more accurate water content values.
The large interindividual variation of water content among the different skin locations could be influenced by individual parameters, for example, age, gender and lifestyle.4, 5, 13, 19 This was not studied in more detail because of the explorative character of this pilot.
Interestingly, no correlation was found between water content and TEWL. One would expect that TEWL increases in a disrupted skin barrier, resulting in lower water content, and vice versa. However, also previous studies showed no or only weak correlations between these two measurements.20, 21 As mentioned earlier, other factors besides from TEWL and water content seem to be responsible for alterations of skin barrier function.
Despite the relatively small number of volunteers, these pilot results are promising. Larger populations of healthy volunteers and patients should be investigated for further validation of the Epsilon. This could elucidate the potential of this device for diagnosis and/or therapeutic monitoring of subjects having skin diseases with decreased barrier function, for example, inflammatory dermatoses. It would also be interesting to study possible interactions between water content and other noninvasive skin barrier measurements (eg, NMF and sebum levels16, 20) and the possible impact of inter‐seasonal fluctuation on skin condition.
In conclusion, we found significant regional differences in water content in human skin measured by the Epsilon. Moreover, the Epsilon measures lower water content values compared to conventional single sensor corneometers and these values show an equal trend in differences of water content among different body sites. It is recommended to investigate these findings in a larger population for further validation of the Epsilon and to determine if this device can be implemented into the clinical setting.
CONFLICT OF INTEREST
None declared.
Logger JGM, Münchhoff CU, Olydam JI, Peppelman M, Van Erp PEJ. Anatomical site variation of water content in human skin measured by the Epsilon: A pilot study. Skin Res Technol. 2019;25:333–338. 10.1111/srt.12653
Logger, Münchhoff, Peppelman and Van Erp contributed equally to this work.
REFERENCES
- 1. Yousef H, Sharma S. Anatomy, Skin (Integument), Epidermis. Treasure Island, FL: StatPearls Publishing; 2017. [PubMed] [Google Scholar]
- 2. Gruber R, Schmuth M. [The barrier function of normal skin. Morphologic and functional aspects of the skin barrier]. Hautarzt. 2014;65(3):234‐240. [DOI] [PubMed] [Google Scholar]
- 3. van Logtestijn MD, Dominguez‐Huttinger E, Stamatas GN, Tanaka RJ. Resistance to water diffusion in the stratum corneum is depth‐dependent. PLoS One. 2015;10(2):e0117292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Tagami H. Location‐related differences in structure and function of the stratum corneum with special emphasis on those of the facial skin. Int J Cosmet Sci. 2008;30(6):413‐434. [DOI] [PubMed] [Google Scholar]
- 5. O'Goshi K, Serup J. Inter‐instrumental variation of skin capacitance measured with the Corneometer. Skin Res Technol. 2005;11(2):107‐109. [DOI] [PubMed] [Google Scholar]
- 6. O'Goshi K, Serup J. Skin conductance; validation of Skicon‐200EX compared to the original model, Skicon‐100. Skin Res Technol. 2007;13(1):13‐18. [DOI] [PubMed] [Google Scholar]
- 7. Mayrovitz HN, Bernal M, Brlit F, Desfor R. Biophysical measures of skin tissue water: variations within and among anatomical sites and correlations between measures. Skin Res Technol. 2013;19(1):47‐54. [DOI] [PubMed] [Google Scholar]
- 8. Imhof B. Stratum corneum hydration measurement using capacitance contact imaging. [Poster]. In press; 2017. [Google Scholar]
- 9. Ltd. BS . Epsilon E 100 prduct description [website]. [Available from: http://www.biox.biz/Products/Epsilon/E100ProductDescription.php. Accessed August 14, 2018.
- 10. Berardesca E, Loden M, Serup J, Masson P, Rodrigues LM. The revised EEMCO guidance for the in vivo measurement of water in the skin. Skin Res Technol. 2018;24(3):351‐358. [DOI] [PubMed] [Google Scholar]
- 11. Imhof B, Xiao P, Angelova‐Fischer I. TEWL, closed‐chamber methods: AquaFlux and VapoMeter In: Berardesca E, Maibach HI, Wilhelm K‐P, eds. Non Invasive Diagnostic Techniques in Clinical Dermatology. Berlin, Heidelberg: Springer Berlin Heidelberg; 2014. 345‐352. [Google Scholar]
- 12. Kleesz P, Darlenski R, Fluhr JW. Full‐body skin mapping for six biophysical parameters: baseline values at 16 anatomical sites in 125 human subjects. Skin Pharmacol Physiol. 2012;25(1):25‐33. [DOI] [PubMed] [Google Scholar]
- 13. Manuskiatti W, Schwindt DA, Maibach HI. Influence of age, anatomic site and race on skin roughness and scaliness. Dermatology. 1998;196(4):401‐407. [DOI] [PubMed] [Google Scholar]
- 14. Ya‐Xian Z, Suetake T, Tagami H. Number of cell layers of the stratum corneum in normal skin ‐ relationship to the anatomical location on the body, age, sex and physical parameters. Arch Dermatol Res. 1999;291(10):555‐559. [DOI] [PubMed] [Google Scholar]
- 15. Egawa M, Hirao T, Takahashi M. In vivo estimation of stratum corneum thickness from water concentration profiles obtained with Raman spectroscopy. Acta Derm Venereol. 2007;87(1):4‐8. [DOI] [PubMed] [Google Scholar]
- 16. Tagami H. Electrical measurement of the hydration state of the skin surface in vivo. Br J Dermatol. 2014;171(Suppl 3):29‐33. [DOI] [PubMed] [Google Scholar]
- 17. Egawa M, Tagami H. Comparison of the depth profiles of water and water‐binding substances in the stratum corneum determined in vivo by Raman spectroscopy between the cheek and volar forearm skin: effects of age, seasonal changes and artificial forced hydration. Br J Dermatol. 2008;158(2):251‐260. [DOI] [PubMed] [Google Scholar]
- 18. Xiao P. Capacitive contact imaging for skin measurements. JPRCP. 2016;6(1):2231‐4237. [Google Scholar]
- 19. Leroy T, Geveaux C, Crucq J, Douven LF, Neste DV. The face and neck: regional variation in skin barrier function and reactivity. Skin Res Technol. 1998;4(4):205‐212. [DOI] [PubMed] [Google Scholar]
- 20. Richters RJ, Falcone D, Uzunbajakava NE, et al. Sensitive Skin: assessment of the Skin Barrier Using Confocal Raman Microspectroscopy. Skin Pharmacol Physiol. 2017;30(1):333‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Chilcott RP, Dalton CH, Emmanuel AJ, Allen CE, Bradley ST. Transepidermal water loss does not correlate with skin barrier function in vitro. J Invest Dermatol. 2002;118(5):871‐875. [DOI] [PubMed] [Google Scholar]
- 22. Algiert‐Zielinska B, Mucha P, Rotsztejn H. Comparative evaluation of skin moisture after topical application of 10% and 30% lactobionic acid. J Cosmet Dermatol. 2018;17:1096‐1100. [DOI] [PubMed] [Google Scholar]
- 23. de Farias Pires T, Azambuja AP, Horimoto AR, et al. A population‐based study of the stratum corneum moisture. Clin Cosmet Investig Dermatol. 2016;9:79‐87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Young DL, Chakravarthy D. A controlled laboratory comparison of 4 topical skin creams moisturizing capability on human subjects. J Wound Ostomy Continence Nurs. 2014;41(2):168‐174. [DOI] [PubMed] [Google Scholar]
- 25. Marrakchi S, Maibach HI. Biophysical parameters of skin: map of human face, regional, and age‐related differences. Contact Dermatitis. 2007;57(1):28‐34. [DOI] [PubMed] [Google Scholar]
- 26. Fluhr JW, Sassning S, Lademann O, et al. In vivo skin treatment with tissue‐tolerable plasma influences skin physiology and antioxidant profile in human stratum corneum. Exp Dermatol. 2012;21(2):130‐134. [DOI] [PubMed] [Google Scholar]
- 27. Loden M, Wessman W. The influence of a cream containing 20% glycerin and its vehicle on skin barrier properties. Int J Cosmet Sci. 2001;23(2):115‐119. [DOI] [PubMed] [Google Scholar]
- 28. Esposito E, Drechsler M, Mariani P, et al. Nanosystems for skin hydration: a comparative study. Int J Cosmet Sci. 2007;29(1):39‐47. [DOI] [PubMed] [Google Scholar]
- 29. Cheng Y, Dong Y, Dong M, et al. Moisturizing and antisebum effect of cosmetic application on facial skin. J Cosmet Dermatol. 2007;6(3):172‐177. [DOI] [PubMed] [Google Scholar]
- 30. Hillebrand GG, Miyamoto K, Schnell B, Ichihashi M, Shinkura R, Akiba S. Quantitative evaluation of skin condition in an epidemiological survey of females living in northern versus southern Japan. J Dermatol Sci. 2001;27(Suppl 1):S42‐S52. [DOI] [PubMed] [Google Scholar]
- 31. Agache P, Mary S, Muret P, Matta AM, Humbert P. Assessment of the water content of the stratum corneum using a sorption‐desorption test. Dermatology. 2001;202(4):308‐313. [DOI] [PubMed] [Google Scholar]


