Abstract
Objective: Sporadic Alzheimer’s disease (AD) is an oxidative, stress-dependent neurodegenerative disease. We investigated whether the levels of protein-methionine sulfoxide (MetO) in plasma could be a possible marker for AD in individuals with mild cognitive impariment (MCI). Design: We evaluated blood samples from patients with AD or MCI, as well as from normal controls, testing their MetO levels and superoxide dismutase (SOD) specific activity. Results: An increase of MetO levels of a particular protein of human plasma and a decrease of SOD activity were observed only in AD plasma. Conclusion: Monitoring the patterns of these plasma markers in patients with MCI could provide a warning sign for disease progression into AD.
Keywords: Alzheimer’s disease, methionine oxidation, blood-plasma, antioxidants
Alzheimer’s disease (AD) is a neurodegenerative condition that causes memory loss and cognitive decline, eventually leading to death. Most individuals with AD do not develop symptoms until the age of 65 years or older, though signs of early-onset AD can develop as early as 30 to 60 years of age in some individuals.1 AD is caused by aggregations of proteins within the brain (beta amyloid plaques extracellularly and tau tangles intracellularly), causing widespread neuronal death.1 Symptoms of AD first manifest most commonly with memory loss, but patients might also experience disorientation, mood and behavior changes, paranoia, and, eventually, difficulty with basic motor functions, such as speaking, walking, and even swallowing.1 Patients with mild cognitive impairment (MCI) show less severe declines in cognitive abilities, but are considered to be at high risk of developing AD or other more severe forms of dementia.1 Due to symptom overlap, it can be difficult to determine whether a patient with MCI will eventually degrade into a more seriously impaired state, such as AD.
Methionine is a free and protein-bound amino acid. Upon exposure to reactive oxygen species (ROS), methionine oxidizes to methionine sulfoxide (MetO), which can be cellularly reduced to methionine by the methionine sulfoxide reductase (Msr) system.2,3 The cyclic conversion of MetO to Met within the cell produces a scavenging effect of ROS. Superoxide dismutase (SOD) is an enzyme well known for its defensive role against oxidative stress caused by ROS. SOD catalyzes the reaction of changing superoxide into hydrogen peroxide and molecular oxygen. Both Msr and SOD function as cellular antioxidant enzymes, while only the SOD activity is detected extracellularly in plasma.4
Our previous comparative analyses of serum MetO-containing proteins between subjects carrying mutant familial AD (FAD) genes and nonmutation-carrier kin showed a correlation between methionine sulfoxidation of specific serum proteins and the presence of the mutation.4 In the current study, we sought to determine if there is a correlation between plasma MetO levels and AD.
MATERIALS AND METHODS
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study by the executive committee of the KUADC.
Plasma samples were collected from human patients for three months by the University of Kansas Alzheimer’s Disease Center (KUADC). Exclusion criteria were subjects below the age of 70 years. The diagnosis of the patients was performed by clinicians at the KUADC. Patients who did not posses any neurodegenerative disease symptoms were included within the control group. The samples were kept frozen at -80ºC until use. The subjects (N=61) from whom the samples were collected were either healthy controls (n=23) or had been diagnosed with MCI (n=13) or AD (n=25) (Table 1). Once the plasma samples were collected, they were analyzed via standard western blot assay using equal amounts of plasma proteins from each subject and the anti-MetO antibody as the primary antibody.5 Protein concentrations in the plasma samples were determined using the Bradford reagent, according to the manufacture protocol (Bio-Rad, Hercules, California). The 61 total samples were analyzed using eight different Western blots—seven experimental and one control. Each experimental blot contained samples from each group (control, MCI, and AD). The eighth control blot contained pooled samples from each set (all 7 experimental blots) to standardize the results across all blots (account for different exposure times and background signal) and be able to accurately compare the data. A specific protein band was selected for densitometry using the National Institutes of Health (NIH) image-J program. Obtained values were tested for significance via a one-way analysis of variance (ANOVA), followed by a Tukey’s multiple comparisons follow-up test.
TABLE 1.
Description of the human subjects contributing to the studies.
| DIAGNOSIS | AGE | SEX, n |
|---|---|---|
| No dementia | 76.3±5.3 | Female, 20 Male, 3 |
| MCI | 78.6±7.2 | Female, 2 Male, 11 |
| AD | 79.4±5.6 | Female, 11 Male, 14 |
| AD: Alzheimer’s disease; MCI: mild cognitive impairment | ||
The specific activity of SOD was measured using the EpiQuick Superoxide Dismutase activity/inhibition Assay kit (EpiGentek, Farmingdale, New York). The kit includes a dye that becomes water soluble upon reduction with superoxide anion, which is inhibited by SOD. Hence, SOD specific activity can be measured via absorbance of the dye (i.e. higher SOD yields less dye absorbance). Obtained values were tested for significance via a one-way ANOVA followed by a Tukey’s multiple comparisons follow-up test.
RESULTS
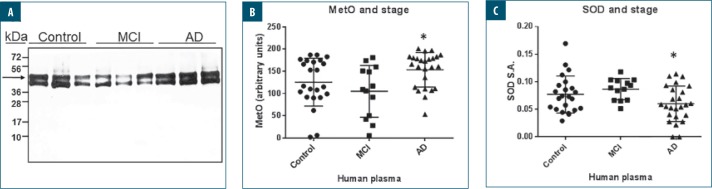
We examined the levels of MetO-protein in healthy controls, patients with AD, and patients with MCI to provide support for our hypothesis that these protein-MetO levels generally increase extracellularly in AD, regardless of the protein/peptide identity. We performed standard western blot analyses using our anti-MetO antibody (as the primary antibody) on plasma extracted from controls (n=23), patients with MCI (n=13), and patients with AD (n=25) who were 70 years of age or older. In addition, we determined SOD activity in these plasma samples to see if there was an inverse correlation between SOD activity and protein-MetO levels as an indication of oxidative stress state (i.e., lower SOD activity and higher protein-MetO level will suggest an enhanced oxidative stress status). The reason for choosing subjects who were 70 years of age or older was because sporadic AD is more associated with this age group. Thus, the disease markers are expected to be better linked to the tested parameters. As shown in Figure 1, in comparison to the MCI and control groups, the average level of a specific MetO-containing protein (Figure 1A) was significantly greater in the AD group (about 45% greater compared to the MCI group, P<0.005), while the SOD specific activity was lower in the AD group (about 42% lower compared to the MCI group, P<0.05). Analysis of the patterns of both of these factors in a patient over time might help determine if the patient will remain at the MCI stage or will decline to an AD state. Note that this study only showed significant results when comparing patients with MCI to those with AD; no significance was found in relation to control patients. No correlations were found between a specific age and protein MetO levels or SOD activities in the three patient groups (data not shown). The effect of sex on the obtained data was not examined, due to the lack of sufficient number of subjects for each sex to satisfy statistical requirements.
FIGURE 1.
Western blot analyses for the detection of methionine sulfoxide (MetO)-proteins in human plasma—A) Equal amounts of plasma proteins taken from control (n=23), mild cognitive impairment (MCI) (n=13), and Alzheimer’s disease (AD) (n=25) subjects were separated on sodium dodecyl sulfate–polyacrylamide (SDS)-gel electrophoresis, followed by western blot analysis using primary rabbit anti-MetO antibody. A typical blot contained samples from the three groups is shown, and all blots (n=7) were developed at the same time to an X-ray film. kDa: kilodaltons. B) The band marked by an arrow was quantified using National Institutes of Health (NIH) Image J program. Statistical analyses were performed using one-way analysis of variance (ANOVA) followed by Tukey’s multiple comparisons test. The asterisk indicates significant statistical differences between the AD and MCI groups (P<0.005). C) Analyses of superoxide dismutase (SOD) activity in human plasma —equal amounts of plasma proteins taken from the same control, MCI, and AD subjects were analyzed for SOD activity using EpiQuick Superoxide Dismutase activity/inhibition Assay kit (Epigentek, Farmingdale, New York). Statistical analyses were performed using one-way ANOVA followed by Tukey’s multiple comparisons test. The asterisk indicates significant statistical differences between the AD and MCI groups (P<0.05). SA: specific activity was calculated as unit/min/mL, according to Assay kit protocol.
DISCUSSION
Several blood and cerebrospinal fluid (CSF) markers have been proposed as early or confirmatory detection of AD.6 The results of our study suggest that a unique combination of plasma markers based on an oxidative posttranslational modification of protein (MetO) and reflects antioxidant enzyme in blood (SOD) might be a useful marker for earlier detection of AD in patients with MCI. The rationale for this approach was based on the knowledge that oxidative stress burden increases with advancing age, fostering MetO modification to proteins due to a reduction of antioxidant defense (e.g., SOD reduced activity). SOD is a cytosolic protein, and its origin in the plasma of the population studied here is not clear. The inverse correlation found might indicate that SOD secretion into the plasma is a result of either a compensatory response to oxidative stress or reflects an elevated enzyme release due to enhanced cell death. However, it is suggested that although the plasma levels of SOD might be greater under these circumstances,4 the actual specific activity of the enzyme drops due to its inactivation by elevated levels of ROS in blood (Figure 1). An age-associated increase of oxidative stress increases ROS production that, in turn, might oxidize and denature proteins, like plasma SOD, causing a drop in their specific activity. Thus, the inverse correlation between the specific MetO-protein levels and SOD activities in the AD group compared to the MCI group is intriguing and might reflect the redox status of the tested subject. Specifically, this dual assay could be used as a diagnostic tool to monitor worsening AD symptoms as a function of age following the first MCI-observed symptoms. Accordingly, the presented analyses might only be applicable to patients already displaying some level of cognitive impairment. Consequently, this study could be extended in a variety of ways. Ideally, these results could be directly replicated in a longitudinal study. For example, plasma samples from patients (controls, MCI, and AD) may be taken and analyzed periodically (e.g., every 6 months) to track the potential progression of MCI toward an AD state and further support the patterns identified by our initial sampling and comparative analysis.
Follow-up studies are currently underway to identify the detected MetO-containing protein from the western blot analysis and to expand the study to a larger population. Once identified, more studies will be conducted to analyze the particular role of this protein within the framework of AD.
Limitations. The total number of the tested subjects is relatively small. Thus, the data may vary following the application of the presented analyses on a larger group of patients.
CONCLUSION
MetO protein levels and SOD activities could serve as biomarkers for AD in patients with MCI. Additional research with a larger patient sample over a longer period of time is needed to support our findings.
REFERENCES
- 1.Scheltens P, Blennow K, Breteler MM, et al. Alzheimer’s disease. Lancet. 2016;388:505–517. doi: 10.1016/S0140-6736(15)01124-1. [DOI] [PubMed] [Google Scholar]
- 2.Oien DB, Moskovitz J. Substrates of the methionine sulfoxide reductase system and their physiological relevance. Curr Top Dev Biol. 2008;80:93–133. doi: 10.1016/S0070-2153(07)80003-2. [DOI] [PubMed] [Google Scholar]
- 3.Oien DB, Moskovitz J. The functions of the mammalian methionine sulfoxide reductase system and related diseases. Antioxidants (Basel). 2018;7(9):pii:E122. doi: 10.3390/antiox7090122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ringman JM, Fithian AT, Gylys K, et al. Plasma methionine sulfoxide in persons with familial Alzheimer’s disease mutations. Dement Geriatr Cogn Disord. 2012;33:219–225. doi: 10.1159/000338546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Oien DB, Canello T, Gabizon R, et al. Detection of oxidized methionine in selected proteins, cellular extracts and blood serums by novel anti-methionine sulfoxide antibodies. Arch Biochem Biophys. 2009;485:35–40. doi: 10.1016/j.abb.2009.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Olsson B, Lautner R, Andreasson U, et al. CSF and blood biomarkers for the diagnosis of Alzheimer’s disease: a systematic review and meta-analysis. Lancet Neurol. 2016;15:673–684. doi: 10.1016/S1474-4422(16)00070-3. [DOI] [PubMed] [Google Scholar]