Abstract
Introduction
Latinx-Americans are underserved across healthcare contexts, and racial disparities in pain management are pervasive. One potential contributor is racial bias in pain perception – including low-level implicit biases and explicitly held lay-beliefs. Delays in seeking pain treatment may compound these disparities. However, experiments testing these factors in the context of Latinx-American pain are limited, and mechanisms by which Latinx-American group-membership influences pain perception and treatment are not understood.
Methods
Here, Latinx-American and White-American participants read vignettes including a Latinx or White patient’s pain description and numerical pain rating. Participants then rated how much pain they thought each patient was in using the same numerical scale. Participants also reported how much pain they themselves would need to experience to prompt treatment-seeking.
Results
In contrast to prior work identifying lay beliefs that Latinx-Americans feel less pain than White-Americans, participants in the current study revealed a bias in the opposite direction. This was largely driven, however, by Latinx-American participants, who have been under-represented in previous studies of empathy and pain perception. Latinx-Americans ascribed more pain to patients overall – irrespective of patient race – relative to White-Americans. Latinx-American participants also reported that their own pain would need to be significantly more intense before seeing a doctor.
Conclusion
These results suggest that, relative to White-Americans, Latinx-Americans may be more likely to believe people are in more pain than they report – or may be more perceptive of others’ pain – and that they may be in more pain upon presenting to medical settings.
Keywords: disparities, race, ethnicity, empathy
Introduction
As is the case across sociodemographic groups, pain is a major health concern for Latinx-Americans – Americans of Latin American origin or descent. Older Latinx-American adults report that pain significantly interferes with everyday life and mental health.1 Prior research demonstrates that Latinx-Americans bear an enhanced burden of pain, experiencing more severe clinical pain2,3 and greater pain in response to controlled laboratory stimuli4,5 relative to White-Americans. Latinx-Americans also face disproportionate structural barriers to pain care.6 Even after ACA-related decreases in health insurance disparity, Latinx-Americans are still more likely than any other racial or ethnic group to be uninsured.7 Moreover, approximately 20% of Hispanic and Latinx-Americans live below the poverty line, and nearly 45% at or below 200% of the federal poverty line,8 presenting additional barriers to care.9,10
Provider-level factors further compound these disparities.11 Even in the context of seeking and receiving medical care, the pain of Latinx-Americans is underestimated and under-managed by clinicians relative to the pain of White-Americans across contexts and pain conditions (emergency room setting;12 bone fracture;13,14 cancer pain;15 labor pain;16 post-operative pain;17,18 and across contexts19,20, although two studies found no significant differences21,22). This under-estimation of Latinx pain is consistent with cultural lay beliefs that Hispanic/Latinx-Americans are less sensitive to pain than White-Americans.23 Though little is known about the specific mechanisms underlying provider-level contributions to the under-treatment of Latinx-American pain, experimental research probing causal mechanisms of disparities between Black- and White-Americans suggests that racial bias is a central driver of disparities in pain management. Racial bias can engender disparities directly by influencing pain perception, assessment, and treatment decisions – as well as indirectly via damage to the doctor-patient relationship (hindering treatment seeking).24 Lay perceivers demonstrate implicit (below the level of conscious awareness) perceptual biases in pain detection,25 and clinicians and non-clinicians reveal explicit biases in pain assessment and treatment recommendations, such that the pain of Black-Americans is under-perceived26–29(but also see31–33). However, identification of mechanisms of racial bias in the context of Latinx-American pain is needed. Decrements in doctor-patient relationships and prior experience with unequal care may also result in such patients primarily seeking medical treatment when pain is most severe, resulting in greater pain when first seeking medical care. Although some work provides support for this possibility, this has not been well-established in the prior literature.34
Others have suggested that disparities may be partially driven by group-level differences in patient preferences based on findings that Latinx-Americans are less likely to seek medical care for2,9 or use analgesics to treat their pain,6,35 and may be more likely to use alternative forms of care in lieu of going to the doctor, such as seeking social support from family members or prayer to cope with pain.6,36 However, inferring preference or personal choice from these observed patterns critically ignores the context of structural barriers and experiences with inadequate and unequal care that in fact constrain choice. People in general tend to turn toward alternatives to biomedical care in contexts in which symptoms are not adequately addressed by medicine.37 It follows that groups who have experienced disparate care may be more likely, therefore, to seek less medical care and rely more on alternative forms of care and coping. A recent, nationally representative study found that Americans report structural barriers to care (e.g., cost, insurance) and unfavorable prior experiences (most notably provider-level issues related to lack of trust and communication) as the major reasons for not seeking medical care.38 Consistent with this, Latinx-Americans report that expectations of racial bias and fears of discrimination fuel distrust in the medical system and contribute to observed relative under-utilization.9 Moreover, when Latinx-Americans do seek pain treatment, they are more likely to have their pain inadequately treated,39 and report more dissatisfaction with their medical care.40 Therefore, what has previously been interpreted as patients’ “choice,” when viewed in context, points toward structural, systemic, and interpersonal (including unconscious biases and unequal treatment) inequalities as prime drivers of disparities. In this way, uncovering the mechanisms that underlie these interpersonal and extrapersonal drivers in context is imperative.
To date, mechanistic investigations of interpersonal and extrapersonal mechanisms underlying pain disparities have primarily focused on the disparate treatment and perception of Black-American pain, relative to White-American pain. However, due to systematic differences in context due to history, cultural climate, and interpersonal treatment across marginalized sociodemographic groups, specific investigations within groups are necessary. Though disparities in outcomes (i.e., pain management) may appear similar across racial minority groups, mechanisms underlying these disparities are expected to differ due to qualitatively different experiential contexts. Specific social and cultural frameworks and factors relevant to Latinx-Americans may be particularly important to consider for adequately addressing their pain. For example, qualitative research and case studies suggest that Latinx-Americans may define and experience pain as transcending personal physical experiences and including interpersonal dimensions.41,42 Latinx-Americans are also more likely to report cultural values of acceptance of pain as a necessary part of life34,43 (including fatalistic beliefs that one should not attempt to change one’s pain,44 as well as stoicism [e.g., refraining from expressing pain] so as not to burden close others36,41,45).
Taken together, prior research suggests compounding effects that may exacerbate the burden of pain, such that Latinx-Americans face known structural barriers to care, and may experience more pain that is commonly under-treated even when care is sought and accessible. However, mechanisms underlying these disparities are unknown. Furthermore, although our recent work provides evidence that people of color may be more sensitive to others’ pain relative to White-Americans,25,46 few studies have examined the impact of perceiver race – particularly of Latinx identity – on pain perception. Moreover, examinations of specific pain experiences and pain-related biases affecting Latinx-Americans – the second largest racial/ethnic group in the United States – broadly are critically under-represented in the extant literature on pain disparities. Here, we use an experimental approach – manipulating patient race – to determine bias in the perception of Latinx-Americans’ pain relative to White-Americans’ pain. We include White- and Latinx-American perceivers to probe perceiver race and ingroup effects on pain perception. We hypothesized that the pain of Latinx patients would be under-rated relative to that of White patients, and that Latinx-Americans would perceive others to be in more pain than would White-Americans. Finally, to examine a potential driver of intergroup differences in pain perception, we asked about how much pain participants would need to experience before seeking treatment.
Method
Terminology
Though researchers have primarily used the term “Hispanic Americans” in prior literature, we use the term “Latinx-Americans” in this manuscript to be inclusive of people of Latin American descent (Mexico, Central America, and South America), as opposed to “Hispanic Americans”– people from Spanish-speaking nations (e.g., Spain) which excludes people from Brazil. Additionally, we refer to “race” and “racial bias” in the present work, as opposed to “ethnicity” which has been favored by others in prior work. In the current design, we expect any participant biases in perception of the pain of others to be due to race – socially constructed, but meaningful categories of difference upon which differential treatment and opportunity are structured47 – as opposed to the construct of ethnicity which refers to shared culture.
Participants
Our full sample consisted of 261 (188 female, 72 male, 1 “prefer not to say”; 116 Latinx, 103 White, 14 Black, 13 Asian, 11 Multi-racial, 1 Native American, 2 “prefer not to say” and 1 “other”; Mean Age =18.59 years, SD Age =0.85) healthy young volunteers. To limit potential confounds with participant race (e.g., education, acculturation) and boost internal validity in this first mechanistic study, all participants were recruited from a college campus. Participants received course credit for their time, and all interested volunteers were eligible to enroll. However, to test our hypotheses and ensure powered group samples, we only included participants who self-identified as either White-American or Latinx-American in our primary analyses (see Supplementary Results for analyses including pain-free individuals across all races). Because stereotypes about minority and majority groups are culturally constrained, participants were excluded from analysis if they were not born in the United States. We also excluded participants who reported suffering from either current or chronic pain because current pain may influence the perception of others’ pain. This left a final sample of 169 participants (85 White-American [53 female, 32 male] and 84 Latinx-American [66 female, 18 male]). This study was approved by the Texas A&M University institutional review board, and informed consent was obtained electronically from all participants before the experiment.
Stimuli
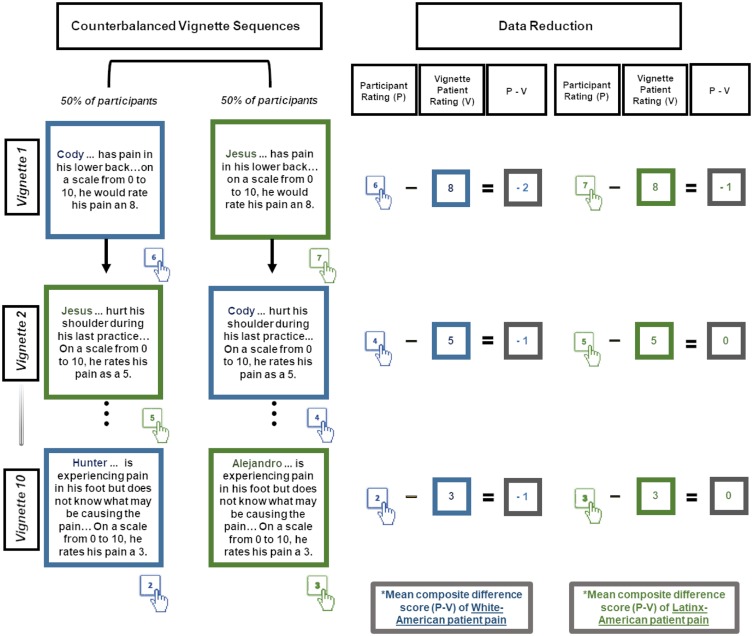
In the primary experimental task, participants were instructed to imagine they were working in the student health clinic as part of a work-study job. In this capacity, they will be pre-screening students who come to the clinic with physical pain. They were then presented with ten short case vignettes that described a male patient in pain (adapted from Mathur and colleagues 2014).25 Consistent with evidence across laboratory and clinical contexts of incongruence between perceiver/clinician and patient pain ratings,25,29,48–50 this particular paradigm has previously been shown to detect perceiver bias in perception – even in the context of explicit pain ratings from the patient in the vignette.25,49 Given prior work suggesting that people may have different assumptions about male and female pain reporting23 and to hold patient reports constant, all case vignettes featured male patients. In each vignette, participants were provided with the patient’s name, location and brief description of pain from the patient’s perspective, and importantly, the patient’s self-reported pain severity on a scale from 0 (no pain) to 10 (worst pain imaginable). The vignette set included patient pain ratings from 2–9, and injury locations of back, shoulder, neck, head, foot, finger, and tooth for realism and to capture a range of pain experiences. However, all participants saw exactly the same vignettes. Counter-balancing was used to control for order effects (Figure 1).
Figure 1.
The vignette patient pain rating was constant, all that varied was whether the patient was Latinx or White. Participants provided ratings of how much pain they thought the patient was experiencing. The figure depicts truncated vignettes. The buttons with the hands indicate hypothetical participant responses.
To examine the impact of racial bias, each vignette was paired with a stereotypically Mexican-American name (i.e., Jesus, Juan, Luis, Jose, or Alejandro) for half of the participants, and with a stereotypically White-American name (i.e., Cody, Justin, Dylan, Kyle, or Hunter) for the other half of the sample. The robust effect of experimentally manipulated names to signal racial group membership has been demonstrated and widely replicated by social psychologists.51 To select names, we examined the top male baby names from the social security administration for the years 1996–97 (to correspond to the average age of the population from which our participants were drawn) in the state of Texas (https://www.ssa.gov/cgi-bin/namesbystate.cgi). These names were expected to be familiar to, and perceived as common by, participants in this study. From the top 50 names (which were similar and overlapping for 1996–97), we excluded names that were expected to be popular across ethnicities (e.g., Michael, Jacob, Joshua, David, Daniel), and created a list of 20 names for pilot testing. Seventeen naïve raters drawn from the same population as our sample categorized these names according to perceived race (“Below are a list of names. If you had to guess the race/ethnicity of an American with this name, what would it be?”). Based on these ratings, we picked names most universally perceived to be either Mexican-American (chosen for the Latinx patient vignettes) or White/European-American.
Procedure
This study was conducted in a university laboratory setting. All procedures were completed on a dedicated desktop computer. After providing consent, participants completed the primary task. Participants were assigned to a counterbalanced order to control for order effects (alternating between Latinx-American and White-American patients, Figure 1). All participants read the same ten vignettes (five paired with the selected Latinx-American patient names and five with the White-American patient names) and responded with how much pain they thought the patient was feeling. After reading the case vignettes, participants completed a brief questionnaire that included a manipulation check, demographic questions, a question about pain-treatment seeking, and debriefing information.
Measures
Pain Perception
The primary dependent variable was operationalized as participant perception of patient pain (“How much pain do you think [vignette patient] is in?”). As participants were given the rating for each patient (5 of whom were Latinx-American, and 5 of whom were White-American), the overall composite difference score between the two ratings [Participant Pain Perception – Provided Vignette Patient Rating] for Latinx-American patients and White-American patients served as our measure of perceptual bias.
Manipulation Check
After completing the task, participants were asked questions about the patients they viewed, including information that was provided in the vignettes as well as for the race of the patients, which was not explicitly provided in the vignettes. This was to confirm that participants’ perceptions of patients’ races matched our initial pilot testing. Consistent with predictions, participants generally perceived the patients with Latinx names as being Hispanic/Latinx-American (92.31%; range across the five names: 78.75–96.25%) and White patients as being White-American (84.38%; range across the five names: 78.75–90.00%).
Demographic Questions
Participants self-reported their age, sex, race, place of birth, their mother’s place of birth, their father’s place of birth, and whether or not they had current pain or chronic pain.
Prior Experiences with Pain and Seeking Pain Treatment
Participants were asked to elaborate on their own prior experiences with pain, though this qualitative data is not discussed in the present paper. Participants then answered the following question: “If/When you are in pain, how intense would your pain have to be for you to go see a doctor?” on a 0 (no pain) −10 (worst pain imaginable) scale.
Data Reduction
To operationalize pain perception (the primary dependent variable), we computed a difference score for each vignette [Study Participant Rating – Vignette Patient Rating]. In this way, a negative score would reflect under-perception or underestimation of the vignette patient’s pain, and a positive score would reflect over-perception or overestimation of the patient’s pain. Thus, each difference score takes into account the participants’ pain ratings, as well as the patients’ pain ratings. In other words, this score is the participant response controlling for patient ratings provided in the vignettes. Since participants were explicitly given the vignette patients’ self-reported pain rating, if they simply believed the patient, they would provide an identical pain rating to the patients’ self-reported pain rating, and have a difference score of zero for that vignette. We then computed composite averages of the raw difference scores for all Latinx-American vignettes, and all White-American vignettes, separately. Main effects of vignette patient race represent a conservative measure of patient race-related pain perceptual bias. As vignettes across participants were identical and either paired with a White or Latinx name, any bias based on vignette patient race can only be due to perceived patient race.
Data Analyses
All data analyses were conducted using SPSS (version 25; IBM Corp, Armonk, NY). We conducted a 2 (Participant Race: Latinx-American, White-American) by 2 (Vignette Patient Race: Latinx-American, White-American) repeated measures ANOVA on pain perception ratings (difference scores). We also conducted a one-way ANOVA, with participant race as a between-subjects factor, on the pain intensity necessary to prompt treatment-seeking. Secondary analyses included a separate 2 (Participant Race: Latinx-American, White-American) by 2 (Vignette Patient Race: Latinx-American, White-American) repeated measures ANOVA on only the first two trials to help control for potential influence of socially desirable responding. We considered the possibility that participants may become aware that the study was about the direct comparison of Latinx-American patients and White-American patients as the study progressed. To further clarify observed effects, we employed independent-samples t-tests to examine between-participant group effects and paired-samples t-tests to examine within-participant group effects. We also examined potential effects of participant sex, order and reaction time (Supplementary Results, Figure S1).
Results
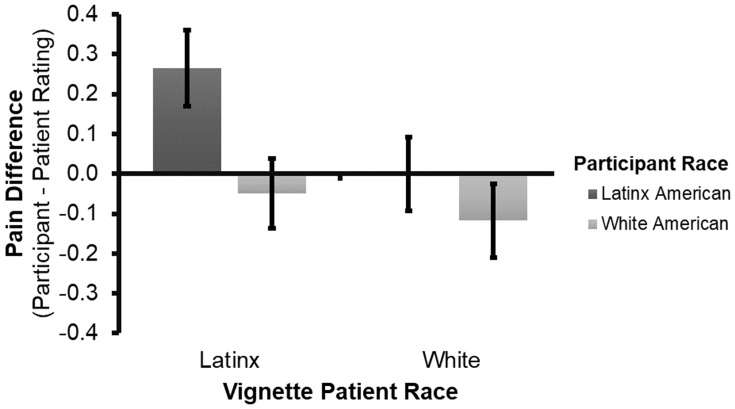
Results revealed a significant main effect of participant race, such that Latinx-American participants perceived patients to be in more pain (M=0.13, SE=0.08), relative to White-American participants (M=−0.08, SE=0.08), F(1,167)=4.02, p=0.047, ηp2=0.023, Figure 2. When examining only the first two trials (when participants would have seen only one vignette of each patient race, and thus may have been less aware that the study was about comparing Latinx-American and White-American patients), the main effect of participant race held, such that Latinx-American participants (M=−0.28, SE=0.10) still perceived more pain in the vignettes relative to White-American participants (M=−0.59, SE=0.10), F(1,167)=4.41, p=0.037, ηp2=0.026.
Figure 2.
Group difference in pain perception, operationalized as a difference score. Error bars represent standard error of the mean (SEM) for each cell.
Results also revealed a significant main effect of vignette patient race F(1,167)=5.13, p=0.025, ηp2=0.030, such that Latinx-American vignette patients were perceived to be in more pain (M=0.11, SE=0.07) relative to White-American patients (M=−0.06, SE=0.07). However, the main effect was not significant when only examining the first two trials, F(1,167)=2.44, p=0.120, ηp2=0.014. Furthermore, though the interaction between participant race and patient race was not significant F(1,167)=1.78, p=0.184, ηp2=0.011, the pattern of results suggests that the main effect of patient race was primarily driven by Latinx-American participants, who ascribed Latinx-American patients with more pain (M=0.26, SE=0.10) than did White-American participants (M=−0.05, SE=0.09), t(167)=2.42, p=0.017, d=0.37.
Finally, results revealed a significant main effect of participant race on treatment seeking, such that Latinx-American participants reported they would have to feel significantly more pain before they would go to see a doctor (M=7.20, SE=0.18), relative to White-American participants (M=6.62, SE=0.18), F(1,167)=5.43, p=0.021, ηp2=0.031, Figure 3.
Figure 3.
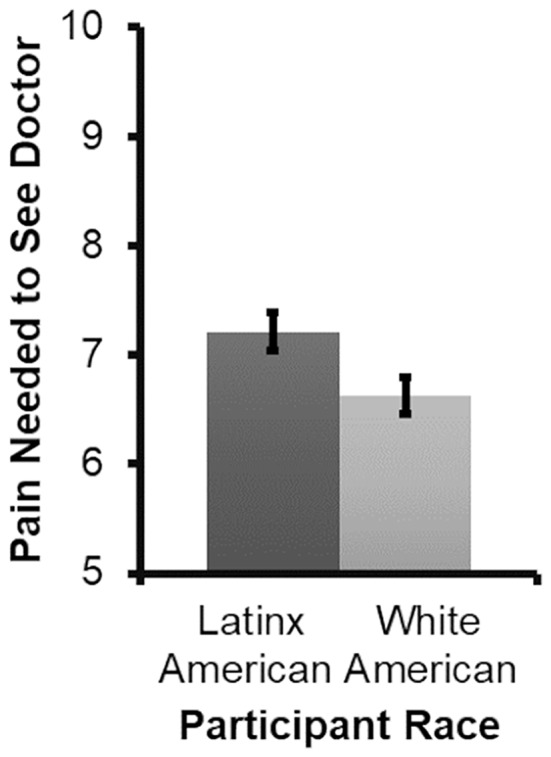
Group differences in pain treatment seeking. Error bars represent standard error of the mean (SEM) for each cell.
Discussion
Latinx-Americans are underserved across healthcare contexts, and their pain is undertreated. Empirical work examining why these pain disparities exist is limited, but prior investigations of disparities among other sociodemographic groups suggests that racial bias may be a primary contributor.50 The present study is one of the first to examine how Latinx identity – from both the perceiver and the patient perspective – may influence the disparate treatment of Latinx-Americans’ pain. To our knowledge, only two prior studies have used experimental methods to examine racial bias in response to the pain of Latinx-Americans.30,22 In contrast to clinical findings, these experimental studies did not find a bias in recommended opioid treatment based on patient race. Both previous studies were limited by inclusion of a small percentage of Latinx-American participants, and thus lacked the ability to examine perceiver race effects. In this way, the recruitment of a sizable sample of both Latinx-American and White-American participants allowed for powered examinations of effects related to perceiver Latinx-identity in the context of responding to the pain of Latinx patients. Further, our examination of pain perception probes an arguably more fundamental cognitive process underlying treatment recommendations, whereas decisions related to opioid recommendations are likely complicated by concerns other than patient pain experience (e.g., concerns about addiction or misuse). Contrary to our hypotheses based on clinical and epidemiological data, but somewhat consistent with limited prior experimental work on opioid recommendations,30,22 we did not find Latinx-American patients were perceived to feel less pain than White-American patients. Rather, participants perceived that Latinx-American patients felt more pain than White-American patients. However, this moderate effect only emerged after presentation of several vignettes and was not present when only looking at the first two trials, when participants may have been less likely to detect the study’s focus on disparities between Latinx- and White-Americans. This effect was also smaller and not statistically significant when perceptual bias was coded as a categorical relative score (Supplementary Results). A prior study found that while people underestimated the pain of Black-American patients when race was presented implicitly, the effect reversed (i.e., participants ascribed more pain to Black-American patients) when race was presented explicitly.25 In the current study, participants read the names of the patients before deciding their response. It is possible that, although the direct comparison between Latinx and White patients in the current study may have started out more implicit, this comparison arguably became more explicit to participants with the presentation of additional vignettes. In other words, as the race comparison may have become more salient with multiple vignettes, participants may have started to respond in more socially desirable ways in an effort to not appear biased52 or in ways that are counter to known societal biases or disparities.
Notably, we also found a moderate sized main effect of participant race, such that Latinx-American participants were more perceptive of patients’ pain in general, irrespective of patient race, relative to White-American participants. Even when explicitly provided with patients’ pain ratings, Latinx-American participants ascribed patients more pain, relative to White-American participants, who tended to perceive patients were in less pain than they reported. Importantly, this effect was robust and held consistent when only examining the first two trials, as well as when pain ratings were coded as a categorical relative score (Supplementary Results). This finding adds to prior work showing that, among clinicians, people of color and women demonstrate less racial bias than majority group members against Black-Americans.53 In previous experimental research, Black-American participants also demonstrated heightened sensitivity to others’ pain.25,46 These findings are contrary to prior work demonstrating that people generally underestimate the pain of others,54 though this prior work is limited by the use of predominantly White-American samples. Therefore, it is possible that certain sociodemographic groups – perhaps those with more experience with discrimination or disparate medical care – may be more perceptive of the pain of other people.
An alternative plausible explanation of the main effect of participant race is that while Latinx-American participants were more skeptical of patients’ pain ratings, White-American participants may have been more “accurate,” since their ratings differed less from the neutral point of 0. However, this interpretation assumes that the absolute value of score deviation is more problematic than the direction of this deviation. The different directions of pain ascription (under-estimation of pain, versus over-estimation) yield different ramifications, and are not equal. The pain of people of color is under-treated,12 therefore under-estimation of their pain serves to further compound pain disparities. On the other hand, perceiving that patients are in more pain than they report may counteract the direction of disparity and may also reflect perceptions of social cognitive processes involved in providing a pain rating to a doctor (e.g., belief that you won’t be believed if you rate high pain).
The present work also documents an additional potential source of disparities: Latinx-Americans report that their pain needs to be more intense before seeking medical attention, relative to White-Americans. This finding provides added context for interpretation of previous work that has shown that Latinx-Americans are less likely to seek medical treatment for pain, relative to White-Americans,2,9 indicating that delay is not due to less pain experience – and perhaps quite the contrary. It necessarily follows that if one needs to be in more pain before seeking medical treatment for pain, one would be in more pain when first presenting in clinical contexts. While others have suggested that Latinx-Americans may delay treatment seeking preferring alternative forms of care for their pain (not involving a formal medical setting, such as home remedies or spiritual support),6 such an interpretation does not consider larger societal contexts and inequities in clinical contexts. For example, Latinx-Americans may only seek medical care for more severe pain due to structural factors such as access to care (e.g., costs8 or issues with insurance coverage),7 as well as social and cultural factors, such as negative prior experiences with their physicians,40 fear of discrimination or mistrust in the medical system.9,55 Future work is needed to explore the relative contributions of these mechanisms in relevant contexts to the behavior of reserving treatment seeking for high severity pain. The role of these mechanisms in the production and maintenance of pain disparities also needs to be further explored.
The cultural awareness that others may be in more pain than they appear upon presenting to medical settings may represent a mechanism underlying both of the significant main effects observed in the present work – Latinx-Americans’ heightened sensitivity to others’ pain, as well as the higher pain threshold needed before seeking medical attention. Prior work suggests that socially constructed cultural norms and values may influence the reporting and perception of pain. For example, a few researchers have posited that women may under-report their pain – contrary to stereotypes about women being more expressive of pain – due to fears of seeming overly emotional or overexaggerating their pain, perhaps contributing to pervasive gender disparities in the treatment of pain.56 As Latinx-American participants reported that their pain would need to be more intense before seeking medical attention, they may have been more attuned to patients (and particularly other Latinx-American patients) potentially being in more pain than they report. However, pain perception was not correlated with the treatment seeking variable in the present study (Supplementary Results).
Another potential driver of the main effects of participant race may be experiences of discrimination, or threats to belonging more generally. Prior work suggests that experiences of social exclusion enhance perceptual sensitivity to others’ social cues,57 as well as the ability to manage others’ emotions.58 To the extent that Latinx-Americans frequently contend with discrimination, stigma, and social exclusion, this too may explain Latinx-American participants perceiving more pain in all patients, relative to White-American participants. Future work is needed to probe the role of these mechanisms, as well as other social contextual factors, in giving rise to pain disparities.59,60
Strengths of the current study include implementation of a controlled experimental approach and recruitment and equal representation of Latinx-American participants. The experimental design using identical vignettes differing only by implied race allowed for rigorous and conservative probing of biases in the perception of Latinx vs White pain. Thus, by maximizing internal validity, we control for numerous factors other than race that may influence response to pain reports in clinical settings. Equal representation of Latinx-Americans allowed us to probe perceiver race and inter-group effects. Representation is critically important in disparities research. Basing strategies to eliminate pain disparities on work conducted among predominantly majority group members will likely be ineffective; and specific mechanisms underlying disparities are expected to differ based on groups’ unique histories, current sociopolitical climates, and systematic differences in interpersonal experiences. Future pain disparities research will need to consider these nuanced factors.
Though the primary task had numerous advantages (capitalizing on internal validity and mundane realism), the task was also quite conservative. Participants were asked how much pain they perceived in patients after being explicitly presented with patients’ pain ratings –these ratings may have served as an anchor and made it harder to detect effects. However, this conservative design, while increasing the possibility that no effects would be detected, bolsters confidence in the observed significant results. Indeed, clinician consideration of explicit patient pain ratings in addition to clinical descriptions has been shown to decrease pain evaluation biases.49 Furthermore, this design has ecological validity in that an explicit patient self-reported pain rating is almost always provided in clinical contexts – yet, disparities in pain treatment persist. Another limitation of the current study is that all participants were young healthy volunteers. On the one hand, this minimized variability between Latinx-American and White-American participants, as all participants were highly educated and acculturated within a similar context. However, this also means that this Latinx-American sample is somewhat homogeneous (young, educated, geographically constrained), and therefore does not fully represent the broader Latinx-American population. Therefore, future studies are needed to capture diversity and boost the generalizability of the present findings. Finally, although similar patterns are expected among practitioner samples as previous research has shown that clinicians and laypeople are similarly susceptible to racial bias,50,61 replication of these effects among practitioner samples is warranted.
The current results extend prior work in several novel directions, and have a number of relevant clinical implications. Specifically, these results may be informative for clinicians in drawing attention to the influence of social and cultural factors on pain perception and reporting. For example, the result that Latinx-Americans may be in more pain when first seeking care suggests that the influence of widely-held cultural beliefs that Latinx-Americans are less sensitive to pain23 in clinical contexts may be especially harmful. To the extent that Latinx-Americans were more sensitive to the pain of others in the current work, irrespective of race, these results may also potentially suggest that increasing diversity and representation in the medical field could be a fruitful avenue for addressing pain disparities, particularly for patients of color.62 Indeed, a recent study found that Latinx-American nurses were more perceptive of the pain of Latinx-American patients than White patients,63 and others have shown that perceptions of similarity and patients’ levels of identification with their healthcare providers are related to improved health outcomes.64 This also adds to similar calls for increased representation based on prior literature on racial concordance, which suggests that having a healthcare provider of the same race may also improve patient experience via increased interaction with their healthcare provider65 and patient satisfaction.66
Taken together, the results from the present study suggest that mechanisms underlying pain disparities are complex, and that contributing factors need to be examined across diverse sociodemographic groups and relevant contexts. More research is needed on how variability in cultural norms, expectations, and experiences between and within groups may influence pain experience, treatment seeking behavior, and the conceptualization and understanding of the pain (and pain reports) of others.
Acknowledgments
We acknowledge the contributions of the many undergraduate research assistants who contributed to this work. Specifically, we thank Matt Cline for his contributions to data collection and interpretation of the results, Lane Bannwart, Jennifer Van Horn, and Jordan Hayes for their assistance with data collection, Sarah Peoples for support in study design and implementation, Humza Ahmed and Magdalena Banda for assistance with experimental programming, and Meredith Gary, Hannah Hutchins Lewer, and Sanya Varma for their assistance with data cleaning. We also thank Brandon Boring for his helpful feedback on the manuscript, and two anonymous reviewers for constructive feedback on an earlier version of this paper. This work was supported by the Department of Psychological and Brain Sciences at Texas A&M University. N.N. was supported by the NSF Graduate Research Fellowship Program. The open access publishing fees for this article have been covered by the Texas A&M University Open Access to Knowledge Fund (OAKFund), supported by the University Libraries and the Office of the Vice President for Research. Portions of this research were presented in a poster form at the Scientific Summit of the American Pain Society and at the annual meeting of the Society for Personality and Social Psychology.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Weaver GD, Kuo YF, Raji MA, et al. Pain and disability in older Mexican-American adults. J Am Geriatr Soc. 2009;57(6):992–999. doi: 10.1111/j.1532-5415.2009.02263.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Portenoy RK, Ugarte C, Fuller I, Haas G. Population-based survey of pain in the United States: differences among white, African American, and Hispanic subjects. J Pain. 2004;5(6):317–328. doi: 10.1016/j.jpain.2004.05.005 [DOI] [PubMed] [Google Scholar]
- 3.Reyes-Gibby CC, Aday LA, Todd KH, Cleeland CS, Anderson KO. Pain in aging community-dwelling adults in the United States: non-Hispanic whites, non-Hispanic blacks, and Hispanics. J Pain. 2007;8(1):75–84. doi: 10.1016/j.jpain.2006.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim HJ, Yang GS, Greenspan JD, et al. Racial and ethnic differences in experimental pain sensitivity: systematic review and meta-analysis. Pain. 2017;158(2):194–211. doi: 10.1097/j.pain.0000000000000731 [DOI] [PubMed] [Google Scholar]
- 5.Rahim-Williams B, Riley JL, Williams AK, Fillingim RB. A quantitative review of ethnic group differences in experimental pain response: do biology, psychology, and culture matter?. Pain Med. 2012;13(4):522–540. doi: 10.1111/j.1526-4637.2012.01336.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hollingshead NA, Ashburn-Nardo L, Stewart JC, Hirsh AT. The pain experience of Hispanic Americans: a critical literature review and conceptual model. J Pain. 2016;17(5):513–528. doi: 10.1016/j.jpain.2015.10.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Berchick ER, Hood E, Barnett JC. Health Insurance Coverage in the United States: 2017.Current Population Reports. United States Census Bureau. U.S. Department of Commerce, Economics and Statistics Administration; 2018. [Google Scholar]
- 8.Fontenot K, Semega J, Kollar M. Income and Poverty in the United States : 2017. United States Census Bureau. U.S. Department of Commerce, Economics and Statistics Administration; 2018. [Google Scholar]
- 9.Nguyen M, Ugarte C, Fuller I, Haas G, Portenoy RK. Access to care for chronic pain: racial and ethnic differences. J Pain. 2005;6(5):301–314. doi: 10.1016/j.jpain.2004.12.008 [DOI] [PubMed] [Google Scholar]
- 10.Langellier BA, Chen J, Vargas-Bustamante A, Inkelas M, Ortega AN. Understanding health-care access and utilization disparities among Latino children in the United States. J Child Health Care. 2016;20(2):133–144. doi: 10.1177/1367493514555587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Burgess DJ, van Ryn M, Crowley-Matoka M, Malat J. Understanding the provider contribution to race/ethnicity disparities in pain treatment: insights from dual process models of stereotyping. Pain Med. 2006;7(2):119–134. doi: 10.1111/j.1526-4637.2006.00105.x [DOI] [PubMed] [Google Scholar]
- 12.Pletcher MJ, Kertesz SG, Kohn MA, Gonzales R. Trends in opioid prescribing by race/ethnicity for patients seeking care in US emergency departments. JAMA. 2008;299(1):70–78. doi: 10.1001/jama.2007.64 [DOI] [PubMed] [Google Scholar]
- 13.Todd KH, Lee T, Hoffman JR. The effect of ethnicity on physician estimates of pain severity in patients with isolated extremity trauma. JAMA. 1994;271(12):925–928. doi: 10.1001/jama.1994.03510360051035 [DOI] [PubMed] [Google Scholar]
- 14.Todd KH, Samaroo N, Hoffman JR. Ethnicity as a risk factor for inadequate emergency department analgesia. Am J Emerg Med. 1996;14(2):157–160. doi: 10.1016/S0735-6757(96)90123-0 [DOI] [PubMed] [Google Scholar]
- 15.Cleeland C, Gonin R, Baez L, Loehrer P, Pandya K. Pain and treatment of pain in minority patients with cancer:the Eastern Cooperative Oncology Group Minority Outpatient Pain Study. Ann Intern Med. 1997;127(9):813–816. doi: 10.7326/0003-4819-127-9-199711010-00006 [DOI] [PubMed] [Google Scholar]
- 16.Rust G, Nembhard WN, Nichols M, et al. Racial and ethnic disparities in the provision of epidural analgesia to Georgia Medicaid beneficiaries during labor and delivery. Am J Obstet Gynecol. 2004;191(2):456–462. doi: 10.1016/j.ajog.2004.03.005 [DOI] [PubMed] [Google Scholar]
- 17.Ng B, Dimsdale JE, Rollnik JD, Shapiro H. The effect of ethnicity on prescriptions for patient-controlled analgesia for post-operative pain. Pain. 1996;66(1):9–12. doi: 10.1016/0304-3959(96)02955-7 [DOI] [PubMed] [Google Scholar]
- 18.Ng B, Dimsdale JE, Shragg GP, Deutsch R. Ethnic differences in analgesic consumption for postoperative pain. Psychosom Med. 1996;58(2):125–129. doi: 10.1097/00006842-199603000-00005 [DOI] [PubMed] [Google Scholar]
- 19.Anderson KO, Mendoza TR, Valero V, et al. Minority cancer patients and their providers: pain management attitudes and practice. Cancer. 2000;88(8):1929–1938. doi: [DOI] [PubMed] [Google Scholar]
- 20.Campbell C, Edwards R. Ethnic differences in pain and pain management. Pain Manag. 2012;3(2):219–230. doi: 10.2217/pmt.12.7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Karpman RR, Del Mar N, Bay C. Analgesia for emergency centers orthopaedic patients: does an ethnic bias exist? Clin Orthop Relat Res. 1997;334:270–275. doi: 10.1097/00003086-199701000-00035 [DOI] [PubMed] [Google Scholar]
- 22.Tamayo-Sarver JH, Dawson NV, Hinze SW, et al. The effect of race/ethnicity and desirable social characteristics on physicians’ decisions to prescribe opioid analgesics. Acad Emerg Med. 2003;10(11):1239–1248. doi: 10.1197/S1069-6563(03)00494-9 [DOI] [PubMed] [Google Scholar]
- 23.Wandner LD, Scipio CD, Hirsh AT, Torres CA, Robinson ME. The perception of pain in others: how gender, race, and age influence pain expectations. J Pain. 2012;13(3):220–227. doi: 10.1016/j.jpain.2011.10.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Penner LA, Hagiwara N, Eggly S, Gaertner SL, Albrecht TL, Dovidio JF. Racial healthcare disparities: a social psychological analysis. Eur Rev Soc Psychol. 2013;24(1):70–122. doi: 10.1080/10463283.2013.840973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mathur VA, Richeson JA, Paice JA, Muzyka M, Chiao JY. Racial bias in pain perception and response: experimental examination of automatic and deliberate processes. J Pain. 2014;15(5):476–484. doi: 10.1016/j.jpain.2014.01.488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hoffman KM, Trawalter S. Assumptions about life hardship and pain perception. Gr Process Intergr Relat. 2016;19(4):493–508. doi: 10.1177/1368430215625781 [DOI] [Google Scholar]
- 27.Trawalter S, Hoffman KM, Waytz A. Racial bias in perceptions of others’ pain. PLoS One. 2012;7(11):1–8. doi: 10.1371/journal.pone.0048546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Waytz A, Hoffman KM, Trawalter S. A superhumanization bias in whites’ perceptions of blacks. Soc Psychol Personal Sci. 2015;6(3):352–359. doi: 10.1177/1948550614553642 [DOI] [Google Scholar]
- 29.Hirsh AT, George SZ, Robinson ME. Pain assessment and treatment disparities: a virtual human technology investigation. Pain. 2009;143(1–2):106–113. doi: 10.1016/j.pain.2009.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hollingshead NA. Examining the influence of Hispanic ethnicity and ethnic bias on medical students’ pain decisions. [dissertation]. Accra:Purdue University, 2016. [Google Scholar]
- 31.Hirsh AT, Hollingshead NA, Ashburn-Nardo L, Kroenke K. The interaction of patient race, provider bias, and clinical ambiguity on pain management decisions. J Pain. 2015;16(6):558–568. doi: 10.1016/j.jpain.2015.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wandner LD, Heft MW, Lok BC, et al. The impact of patients’ gender, race, and age on health care professionals’ pain management decisions: an online survey using virtual human technology. Int J Nurs Stud. 2014;51(5):726–733. doi: 10.1016/j.ijnurstu.2013.09.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hirsh AT, Alqudah AF, Stutts LA, Robinson ME. Virtual human technology: capturing sex, race, and age influences in individual pain decision policies. Pain. 2008;140(1):231–238. doi: 10.1016/j.pain.2008.09.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Larkey LK, Hecht ML, Miller K, Alatorre C. Hispanic cultural norms for health-seeking behaviors in the face of symptoms. Health Educ Behav. 2001;28(1):65–80. doi: 10.1177/109019810102800107 [DOI] [PubMed] [Google Scholar]
- 35.Hollingshead NA, Vrany EA, Stewart JC, Hirsh AT. Differences in Mexican Americans’ prevalence of chronic pain and co-occurring analgesic medication and substance use relative to non-Hispanic White and Black Americans: Results from NHANES1999–2004. Pain Med. 2016;17(6):1001–1009. doi: 10.1093/pm/pnv003 [DOI] [PubMed] [Google Scholar]
- 36.Campbell LC, Andrews N, Scipio C, Flores B, Feliu MH, Keefe FJ. Pain coping in Latino populations. J Pain. 2009;10(10):1012–1019. doi: 10.1016/j.jpain.2009.03.004 [DOI] [PubMed] [Google Scholar]
- 37.Thorne S, Paterson B, Russell C, Schultz A. Complementary/alternative medicine in chronic illness as informed self-care decision making. Int J Nurs Stud. 2002;39(7):671–683. doi: 10.1016/S0020-7489(02)00005-6 [DOI] [PubMed] [Google Scholar]
- 38.Taber JM, Leyva B, Persoskie A. Why do people avoid medical care? A qualitative study using national data. J Gen Intern Med. 2015;30(3):290–297. doi: 10.1007/s11606-014-3089-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cleeland CS, Gonin R, Hatfield AK, et al. Pain and its treatment in outpatients with metastatic cancer. N Engl J Med. 1994;330(9):592–596. doi: 10.1056/NEJM199403033300902 [DOI] [PubMed] [Google Scholar]
- 40.Blair IV, Steiner JF, Fairclough DL, et al. Clinicians’ implicit ethnic/racial bias and perceptions of care among Black and Latino patients. Ann Fam Med. 2013;11(1):43–52. doi: 10.1370/afm.1442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Villarruel A. Mexican-American cultural meanings, expressions, self-care and dependent-care actions associated with experiences of pain. Res Nurs Health. 1995;18(5):427–436. doi: 10.1002/(ISSN)1098-240X [DOI] [PubMed] [Google Scholar]
- 42.Cervantes JM, Lechuga DM. The meaning of pain: a key to working with Spanish-speaking patients with work-related injuries. Prof Psychol Res Pr. 2004;35(1):27–35. doi: 10.1037/0735-7028.35.1.27 [DOI] [Google Scholar]
- 43.Torres CA, Thorn BE, Kapoor S, DeMonte C. An examination of cultural values and pain management in foreign-born Spanish-speaking Hispanics seeking care at a federally qualified health center. Pain Med. 2017;18(11):2058–2069. doi: 10.1093/pm/pnw315 [DOI] [PubMed] [Google Scholar]
- 44.Jun J, Oh KM. Asian and Hispanic Americans' fatalism and colon cancer screening. Am J Health Behav. 2013;37(2):145–154. [DOI] [PubMed] [Google Scholar]
- 45.Juarez G, Ferrell B, Borneman T. Influence of culture on cancer pain management in Hispanic patients. Cancer Pract. 1998;6(5):262–269. doi: 10.1046/j.1523-5394.1998.00020.x [DOI] [PubMed] [Google Scholar]
- 46.Mathur V, Paice J. Racial differences in neural response to the acute pain of other people. J Pain. 2013;14(4):S48. doi: 10.1016/j.jpain.2013.01.530 [DOI] [Google Scholar]
- 47.Smedley A, Smedley BD. Race as biology is fiction, racism as a social problem is real: anthropological and historical perspectives on the social construction of race. Am Psychol. 2005;60(1):16–26. doi: 10.1037/0003-066X.60.1.16 [DOI] [PubMed] [Google Scholar]
- 48.Solomon P. Congruence between health professionals’ and patients’ pain ratings: a review of the literature. Scand J Caring Sci. 2001;15(2):174–180. doi: 10.1046/j.1471-6712.2001.00027.x [DOI] [PubMed] [Google Scholar]
- 49.Riva P, Rusconi P, Montali L, Cherubini P. The influence of anchoring on pain judgment. J Pain Symptom Manage. 2011;42(2):265–277. doi: 10.1016/j.jpainsymman.2010.10.264 [DOI] [PubMed] [Google Scholar]
- 50.Hoffman KM, Trawalter S, Axt JR, Oliver MN. Racial bias in pain assessment and treatment recommendations, and false beliefs about biological differences between blacks and whites. PNAS. 2016;113:4296–4301. doi: 10.1073/pnas.1516047113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Okonofua JA, Eberhardt JL. Two strikes: race and the disciplining of young students. Psychol Sci. 2015;26(5):617–624. doi: 10.1177/0956797615570365 [DOI] [PubMed] [Google Scholar]
- 52.Dunton BC, Fazio RH. An individual difference measure of motivation to control prejudiced reactions. Pers Soc Psychol Bull. 1997;23(3):316–326. doi: 10.1177/0146167297233009 [DOI] [Google Scholar]
- 53.Sabin J, Nosek B, Greenwald A, Rivara F. Physicians’ implicit and explicit attitudes about race by MD race, ethnicity, and gender. J Health Care Poor Underserved. 2009;20(3):896–913. doi: 10.1353/hpu.0.0185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Robinson ME, Wise EA. Gender bias in the observation of experimental pain. Pain. 2003;104(1–2):259–264. doi: 10.1016/S0304-3959(03)00014-9 [DOI] [PubMed] [Google Scholar]
- 55.Casagrande SS, Gary TL, Laveist TA, Gaskin DJ, Cooper LA. Perceived discrimination and adherence to medical care in a racially integrated community. J Gen Intern Med. 2007;22(3):389–395. doi: 10.1007/s11606-006-0057-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hoffmann D, Tarzian A. The girl who cried pain: a bias against women in the treatment of pain. J Law, Med Ethics. 2001;28:13–27. doi: 10.1111/j.1748-720X.2001.tb00037.x [DOI] [PubMed] [Google Scholar]
- 57.Pickett CL, Gardner WL, Knowles M. Getting a cue: the need to belong and enhanced sensitivity to social cues. Pers Soc Psychol Bull. 2004;30(9):1095–1107. doi: 10.1177/0146167203262085 [DOI] [PubMed] [Google Scholar]
- 58.Cheung EO, Gardner WL. The way I make you feel: social exclusion enhances the ability to manage others’ emotions. J Exp Soc Psychol. 2015;60:59–75. doi: 10.1016/j.jesp.2015.05.003 [DOI] [Google Scholar]
- 59.Dovidio JF, Fiske ST. Under the radar: how unexamined biases in decision-making processes in clinical interactions can contribute to health care disparities. Am J Public Health. 2012;102(5):945–952. doi: 10.2105/AJPH.2011.300601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Penner LA, Blair IV, Albrecht TL, Dovidio JF. Reducing racial health care disparities: a social psychological analysis. Policy Insights Behav Brain Sci. 2014;1(1):204–212. doi: 10.1177/2372732214548430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Blair IV, Havranek EP, Price DW, et al. Assessment of biases against Latinos and African Americans among primary care providers and community members. Am J Public Health. 2013;103(1):92–98. doi: 10.2105/AJPH.2012.300812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ferguson WJ, Candib LM. Culture, language, and the doctor-patient relationship. Fam Med. 2002;34(5):353–361. [PubMed] [Google Scholar]
- 63.Bloch C. Hispanic nurses’ knowledge of and approach to pain assessment and management. J Transcult Nurs. 2017;28(3):251–258. doi: 10.1177/1043659616639102 [DOI] [PubMed] [Google Scholar]
- 64.Losin EAR, Anderson SR, Wager TD. Feelings of clinician-patient similarity and trust influence pain: evidence from simulated clinical interactions. J Pain. 2017;18(7):787–799. doi: 10.1016/j.jpain.2017.02.428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hagiwara N, Penner LA, Gonzalez R, et al. Racial attitudes, physician-patient talk time ratio, and adherence in racially discordant medical interactions. Soc Sci Med. 2013;87:123–131. doi: 10.1016/j.socscimed.2013.03.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.LaViest TA, Nuru-Jeter A. Is doctor-patient race concordance associated with greater satisfaction with care? J Health Soc Behav. 2018;43(3):296–306. doi: 10.2307/3090205 [DOI] [PubMed] [Google Scholar]