Abstract
Environmental pollution of the air, water, and soil comprise an increasingly urgent challenge to global health, well-being, and productivity. The impact of environmental pollution arguably has its greatest impact across the lifespan on children, women of childbearing age, and pregnant women and their unborn children, not only because of their vulnerability during development, but also because of their subsequent longevity. Ulaanbaatar, Mongolia, is a highly instructive, perhaps extreme, example of what happens with recent, rapid urbanization. It is the coldest capital city on Earth, where average ambient temperatures routinely fall below −40°C/F between November and February. During the cold winter period, more than 200,000 “Gers” (traditional felt-lined dwellings) in the “Ger district” burn over 600,000 tons of coal for domestic heating (>3 tons each). Thus, outdoor ambient particulate levels frequently exceed 100 times the WHO-recommended safety level for sustained periods of time, and drive the majority of personal particulate matter exposure. Indoor levels of exposure are somewhat lower in this setting because Gers are equipped with chimneys. Major adverse health impacts that we have documented in the Ger districts include the following: respiratory diseases among those between 1 and 59 years of age and cardiac diseases in those over 60; alarming increases in lung cancer rates in females are also beginning to emerge; and fertility and subsequent successful completion of term pregnancy falls by up to half during the winter pollution season, while early fetal death rises by fourfold. However, the World Bank has intervened with a Ger stove replacement project that has progressively reduced winter pollution by about 30% over the past 5 years, and this has been accompanied by an increase in mean term birth weight of up to 100g. Each incremental decrement in air pollution clearly has beneficial effects on pregnancy, which are likely to have the greatest positive health and macroeconomic impact across the lifespan. However, innovative policies and solutions are clearly needed to eliminate coal heating in Gers and thus further reduce the markedly negative health impact of this practice.
Keywords: air pollution impact, lifespan, Mongolia, mothers and children
Environmental pollution of the air, water, and soil poses an increasingly urgent challenge to global health, well-being, and population productivity (1). The impact of environmental pollution arguably has its greatest impact across the lifespan on women of childbearing age, pregnant women and their unborn children, and young children, not only because of their special vulnerability during human development but also because of impairment of their subsequent well-being, productivity, and longevity (2–9).
Ulaanbaatar, the capital city of Mongolia, represents a highly instructive, yet perhaps somewhat extreme, example of what happens with recent, rapid urbanization. Ulaanbaatar is the coldest capital city on Earth. Its average ambient temperatures routinely fall below −40°C/F between November and February. Ulaanbaatar has a population of approximately 1.5 million and is situated geographically in a river valley (Figure 1). About 60% of the city’s population are relatively impoverished recent immigrants from the countryside and still live in traditional dwellings that are round wool felt-lined tents called Gers (2–5). Gers are actually well adapted to the wintertime rural environment when spaced well apart (Figure 2, upper panel). During the extreme cold of the Mongolian winter, the “Ger district,” with more than 200,000 closely spaced households, burns over 600,000 tons of coal for domestic heating (>3–5 tons per Ger) (6–10). Because individual Ger stoves have chimneys, much of the resulting particulate and gaseous pollution is expelled to the outside via the stove flues (Figure 2, lower panel). Thus, outdoor ambient mean particulate levels frequently significantly exceed 100 times the World Health Organization–recommended safety level of less than 10 μg/m3 particulate matter less than or equal to 2.5 μm in aerodynamic diameter (PM2.5) for sustained periods of time, and thus drive the majority of average personal outdoor particulate matter exposure. On extremely cold windless days with atmospheric inversion, outdoor PM2.5 can occasionally peak as high as 3 mg/m3 (U.S. Embassy, personal communication, December 2017 and January 2018) (UNICEF report [11]), levels that are more usually found at the coal face in underground mining environments. Outdoor PM2.5 levels also vary diurnally as well as by season, being higher in the morning and the evening than during the rest of the day in winter (Figure 3), because this is when coal burning for domestic heating and incidentally for cooking is taking place (2, 3). Indoor levels of exposure in Gers, however, tend to be somewhat lower than outdoors because Gers are equipped with chimneys (Figure 2). Thus, even in Gers, outdoor levels of air pollution usually substantially exceed indoor levels, unless the door is left open or frying is in progress in a big wok on the coal stove (5). Apartment dwellers are generally exposed to somewhat lower levels of indoor pollution because apartments are centrally heated with steam and take up external pollution only if the windows leak and/or are left open for cooling (5). Thus, in certain more salubrious southern parts of Ulaanbaatar, such as the Zaisan district, indoor pollution in apartments is, on average, fourfold (or more) less than in Gers, with the major drivers being cooking and smoking. However, during the morning or evening commute, all commuters are exposed to massive levels of outdoor pollution, with those with a long bus commute likely faring the worst, because buses take on a fresh load of pollution along with the passengers when the doors open at each stop (5).
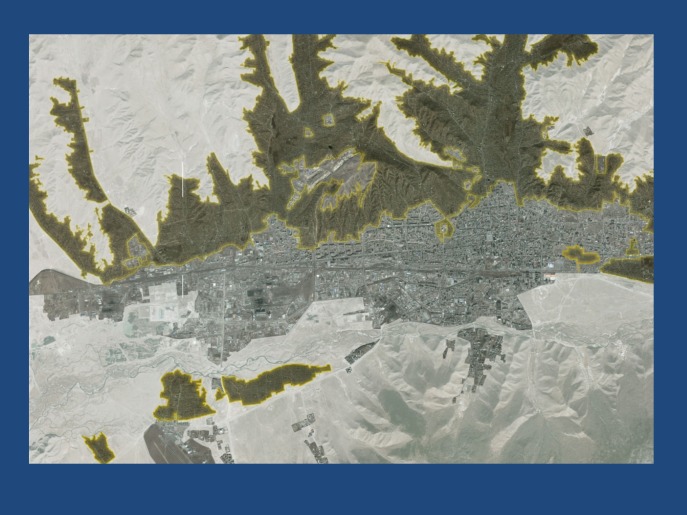
Figure 1.
Distribution of Ger districts, predominantly in the northern suburbs of Ulaanbaatar. Satellite view of greater Ulaanbaatar surrounded by snow (white). The centrally built environment that houses 40% of the total population in apartments is shown in gray. The surrounding dark green areas show the extent of the Ger districts that house the remaining 60% of the total Ulaanbaatar population of 1.5 million. The northern Ger districts contain approximately 200,000 family units, each living in a Ger and/or adjacent wooden shanties.
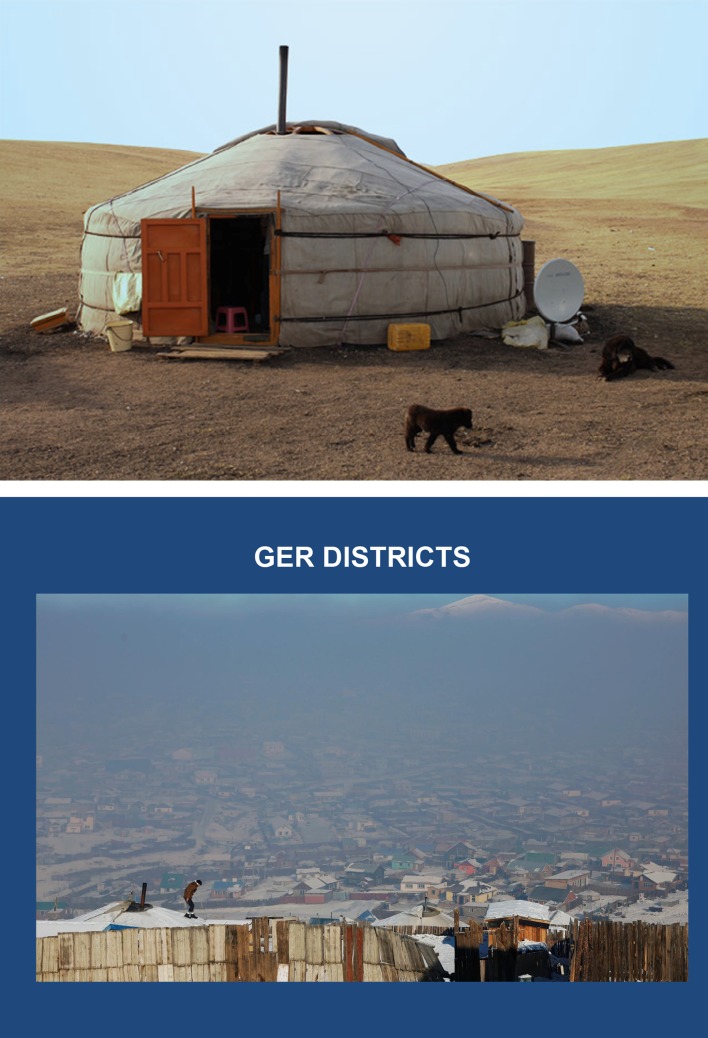
Figure 2.
A single Ger out on the steppe in summer (top), as compared with a small section of the northern Ger district in Ulaanbaatar in winter (bottom). Note how closely packed the round Gers are in the foreground. Also note the thick pall of coal smog hanging over the Ger district and bounded to the north by snowcapped mountains.
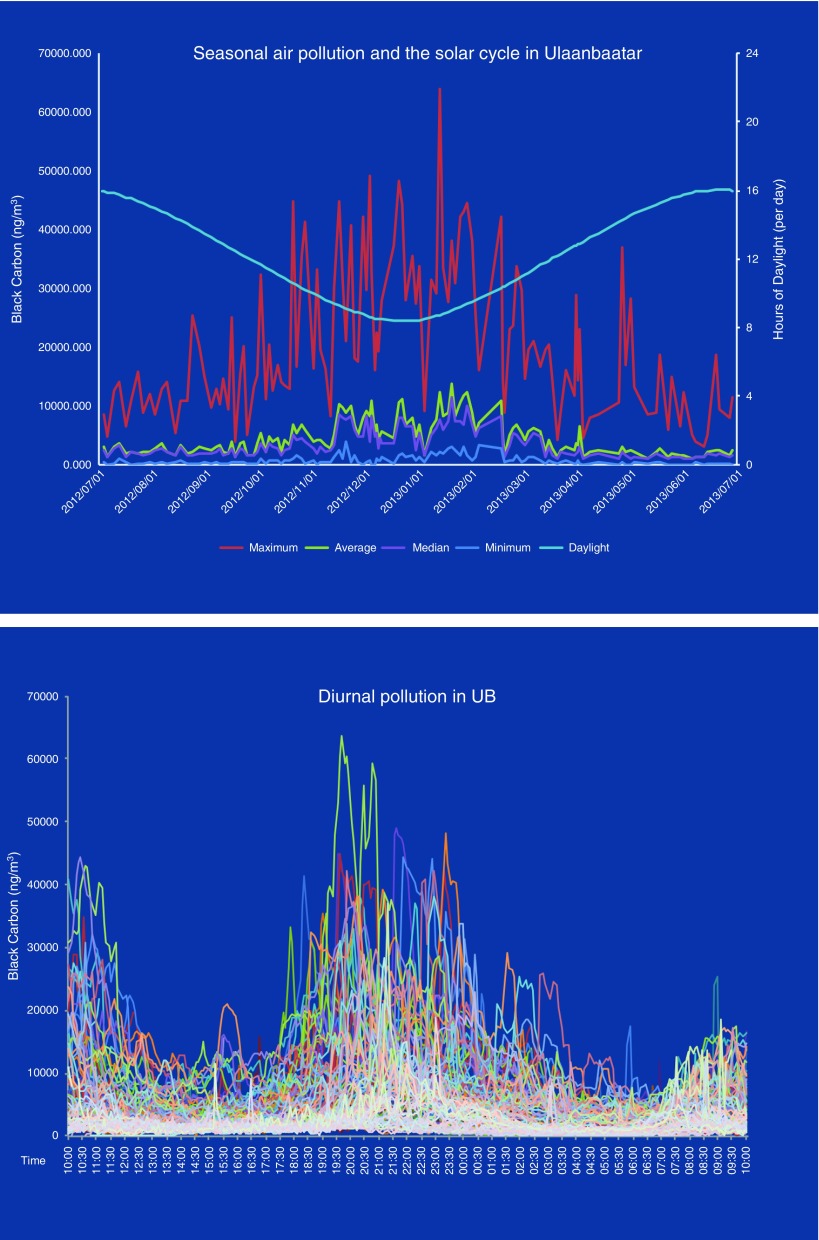
Figure 3.
Top: Annual seasonal air pollution. The relative black carbon particulate matter concentrations in central Ulaanbaatar (UB) are depicted as maximum (red), minimum (dark blue), mean (green), and median (mauve). Hours of daylight is depicted in light blue. Black carbon units are expressed as nanograms per cubic meter. Bottom: Intradiurnal black carbon pollution levels. Each curve represents one individual day. Days were recorded over the course of one year and are superimposed to display patterns of diurnal variation over the course of one year. The bimodal distribution of black carbon pollution with separate peaks in the morning and evening is well illustrated. Data in the upper and lower panels are used by generous and gracious permission of Christa Hassenkopf and were recorded in the climate laboratory of Prof. Sereeter Lodoysamba at the National University of Mongolia. The figure was prepared by Nicole Warburton using these data.
Delgerzul and coworkers have documented major adverse seasonal wintertime health impacts in the Ger-district clinics, including major increases in all International Classification of Diseases, 10th Revision–coded respiratory diseases in individuals between 1 and 59 years of age and cardiac diseases in the over-60 age group, as compared with the much less polluted summer months (personal communication, 2017). Cox regression yielded significantly increased odds ratios for each of these occurrences per 100 μg/m3 increase of PM2.5. Allen and coworkers have also published data on the mortality attributable to air pollution in Ulaanbaatar (6).
Over the most recent decade, alarming increases in lung cancer rates specifically in females have begun to emerge, whereas the lung cancer rate is stable in males. According to our preliminary studies with Jargalsaikhan and coworkers in 10,000 families reporting for obstetric delivery at the Urguu First Maternity Hospital, about 40% of the males (fathers) smoked, whereas in females (mothers), the rate was less than 10% (unpublished results, B.J.). However, all persons are exposed equally to coal smoke air pollution when outside in the winter, morning, and evening (5). The World Health Organization recently declared air pollution to be carcinogenic (12). We postulate that the lung cancer rate among males is driven primarily by firsthand tobacco smoke exposure with a minimal contribution from air pollution, whereas in females the primary driver is air pollution. The increased burden of coal smoke inhalation could therefore account for the steadily increasing lung cancer rates in females versus the stable lung cancer rate in males (O.C. and B.J., personal communication, July 2017). However, other causes, such as secondhand smoke, may also be important. Three years ago, indoor smoking was banned in Mongolia, and this has resulted in clearly observable much cleaner air in restaurants and public spaces (13). Also, men tell us that they are now more likely to smoke outside their homes and not in front of their spouse and family, even when it is very cold outside (personal observation).
Pregnancy and complications thereof are not included in the Global Burden of Disease report (14, 15); yet, we are finding that air pollution has a major impact on fertility and successful completion of pregnancy. Fertility and subsequent successful completion of term pregnancy fall by up to half during the winter pollution season (unpublished results, D.W. and B.J.), and early fetal death rises by fourfold in the same season of the year (3). Moreover, we have found by ultrasound that fetal growth is also adversely affected, depending on the date of conception, with head circumference and leg length as seen on ultrasound being significantly adversely affected pollution targets (unpublished results, H. Ong, S. Hunter, and D.W.).
On the more positive intervention side, over the recent past, the World Bank, with its Millennium Challenge Fund, has intervened with a Ger-stove replacement project that has distributed about 200,000 Turkish stoves virtually free of charge. The coal-burning efficiency of Turkish stoves was measured by Lodoysamba and colleagues at a Mongolian national stove laboratory (unpublished results, S.L. and D.W.), and these stoves are indeed significantly more efficient in energy output and emit about 30% less pollution. The uptake of these stoves by the public has been associated with progressively reduced winter pollution by as much as 30% over the past 5 years, and this in turn appears to correlate with a progressive increase in mean term birth weight of up to 100 g at Urguu First Maternity Hospital (unpublished results, B.J. and D.W.). Thus, even modest decrements in air pollution clearly can have incremental beneficial effects on the outcomes of pregnancy, which are likely overall to have a great positive effect on health and macroeconomic impact across the lifespan.
However, the traditional Ger stove has not actually been discarded, because it is preferred for the quick, intense heat required for cooking traditional meat soups and pastries (buuz), so Ger dwellers often “stack” heat sources with a traditional Mongolian/Russian box stove plus a new replacement heating Turkish stove as well as a small, natural gas camping-style stove (14). Clearly, more innovative policies and solutions are needed to eliminate and replace coal-based heating in Gers and thus further reduce the markedly negative health impact of this practice on health across the lifespan in Ulaanbaatar.
Mask-wearing outdoors and indoor air filtration are two relatively low-cost interventions that are being evaluated. Allen and coworkers have delivered high-efficiency particulate air filtration devices to a sample of pregnant women living in apartments in Ulaanbaatar, an experiment that reportedly resulted in a significant increase in average birth weight of their newborn infants (R. Allen, personal communication, January 2016). Wigfall and Mandukhai recently published the results of the first phase of their evaluation of attitudes toward mask-wearing among women of childbearing age in Ulaanbaatar and reported that this safety behavior is not popular (16, 17). The expense of good masks is a major concern, as is not being convinced of the efficacy of masks, as well as “we don’t want to smudge our makeup,” which is expensive and an important item of business attire among female professionals in Ulaanbaatar.
A stated preference survey conducted in winter 2010 in Ulaanbaatar revealed a willingness to pay for mortality risk reductions, with results implying a value of statistical life of approximately $500,000 for a 5-in-10,000 annual risk reduction (16). This is a remarkable sum, given that the per capita gross domestic product (GDP) in Mongolia was still less than $4,500 in 2017 and that Mongolia remains a low- to middle-income country. The ultimate answer, as it was for the great smog in London in 1952 and the 1948 Donora smog in Pittsburgh, will be completely stopping the burning of coal for domestic heating in Ulaanbaatar. The cost of doing this will be substantial, however, because it will involve the installation of very significant and as yet nonexistent infrastructure for gas, oil, or solar heating systems. Yet, we propose that the cost of not doing so will also be significant. The costs of health disparities are normally reckoned as disability-adjusted life-years as a measure of increased life expectancy. However, disability-adjusted life-years were not designed to reckon the opportunity cost of lost pregnancies. We propose a novel model in which the revenue opportunity cost of the children that fail to be born owing to air pollution can be calculated as the number of such “nonchildren” multiplied by the GDP per capita ($4,500), multiplied by life expectancy, multiplied by a reasonable lifetime inflation factor (amounting to approximately >$1.6 × 109 compounding per annum). The Mongolian government has further calculated that the cost of pollution-related care and lost work and school productivity in affected children and adults accounts for as much as one-fourth of GDP in Ulaanbaatar in winter (another approximately $1.6 billion).
Currently, each Ger family burns, on average, 3 tons of brown coal per winter, which should produce about 600,000 kWh equivalents of heat energy per stove. We therefore roughly calculate that installing a solar plant at today’s US prices sufficient to replace the thermal output of 200,000 coal stoves in Ulaanbaatar at $5,000 per kWh comes to the astronomical sum of $6 × 1014. However, in Mongolia, the cost per kilowatt hour for solar conversion might be less than estimated on the basis of current U.S. prices if land could be donated by the city government and if China were used as a neighboring discount manufacturer and supplier. In addition, because sunshine is free, the annual cost of coal would ultimately be eliminated with conversion to solar. However, in Mongolia, a low- to middle-income country that recently had to negotiate to borrow $5 billion to refinance its Chinggis Bond debt burden, shouldering the cost of immediately eliminating coal-based pollution and replacing heat generation with solar energy would present a major political and financial challenge. We argue, however, that considering the cumulative annual dollar cost of the adverse health effects of coal smoke air pollution, the amortized dollar cost of decisive and informed action to eliminate coal smoke pollution should be viewed in a more positive light (11).
Supplementary Material
Footnotes
Supported by National Institutes of Health grant 1D43ES02286201.
Author Contributions: D.W. wrote the paper; N.W. assisted S.L. and D.W. in the field and did the data analysis in Figure 3; C.W. provided data on mask-wearing and assisted D.W. in the field; O.C. is a senior Mongolian collaborator; D.L. provided health data and commentary on health clinics; S.L. collected pollution data, provided commentary and guidance on the Ger stove situation, and corrected the manuscript; and B.J. collected data on maternal health and birth outcomes, and read and corrected the manuscript.
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Austen K.Environmental science: pollution patrol Nature 2015517136–138.[Published erratum appears in Nature 2015;517:257.] [DOI] [PubMed] [Google Scholar]
- 2.Warburton D, Gilliland F, Dashdendev B. Environmental pollution in Mongolia: effects across the lifespan. Environ Res. 2013;124:65–66. doi: 10.1016/j.envres.2013.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Enkhmaa D, Warburton N, Javzandulam B, Uyanga J, Khishigsuren Y, Lodoysamba S, et al. Seasonal ambient air pollution correlates strongly with spontaneous abortion in Mongolia. BMC Pregnancy Childbirth. 2014;14:146. doi: 10.1186/1471-2393-14-146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dashdendev B, Fukushima LK, Woo MS, Ganbaatar E, Warburton D. Carbon monoxide pollution and lung function in urban compared with rural Mongolian children. Respirology. 2011;16:653–658. doi: 10.1111/j.1440-1843.2011.01958.x. [DOI] [PubMed] [Google Scholar]
- 5.Dashnyam U, Warburton N, Brugha R, Tserenkh I, Davaasambuu E, Enkhtur S, et al. Personal exposure to fine-particle black carbon air pollution among schoolchildren living in Ulaanbaatar, Mongolia. Cent Asian J Med Sci. 2016;2:107. [Google Scholar]
- 6.Allen RW, Gombojav E, Barkhasragchaa B, Byambaa T, Lkhasuren O, Amram O, et al. An assessment of air pollution and its attributable mortality in Ulaanbaatar, Mongolia. Air Qual Atmos Health. 2013;6:137–150. doi: 10.1007/s11869-011-0154-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Huang YK, Luvsan ME, Gombojav E, Ochir C, Bulgan J, Chan CC. Land use patterns and SO2 and NO2 pollution in Ulaanbaatar, Mongolia. Environ Res. 2013;124:1–6. doi: 10.1016/j.envres.2013.02.006. [DOI] [PubMed] [Google Scholar]
- 8.Chen YT, Huang YK, Luvsan ME, Gombojav E, Ochir C, Bulgan J, et al. The influence of season and living environment on children’s urinary 1-hydroxypyrene levels in Ulaanbaatar, Mongolia. Environ Res. 2015;137:170–175. doi: 10.1016/j.envres.2014.11.022. [DOI] [PubMed] [Google Scholar]
- 9.Sonomjamts M, Dashdemberel S, Logii N, Nakae K, Chigusa Y, Ohhira S, et al. Prevalence of asthma and allergic rhinitis among adult population in Ulaanbaatar, Mongolia. Asia Pac Allergy. 2014;4:25–31. doi: 10.5415/apallergy.2014.4.1.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Batmunkh T, Kim YJ, Jung JS, Park K, Tumendemberel B. Chemical characteristics of fine particulate matters measured during severe winter haze events in Ulaanbaatar, Mongolia. J Air Waste Manag Assoc. 2013;63:659–670. doi: 10.1080/10962247.2013.776997. [DOI] [PubMed] [Google Scholar]
- 11.Gheorghe A, Ankhbayar B, van Nieuwenhuyzen H, de Sa R National Center for Public Health and UNICEF Mongolia. Mongolia’s air pollution crisis: a call to action to protect children’s health. Ulanbataar, Mongolia: UNICEF Mongolia; February 2018 [accessed 2018 Mar 28]. https://www.unicef.org/mongolia/Mongolia_air_pollution_crisis_ENG.pdf.
- 12.Straif K, Cohen A, Samet J, editors. Air pollution and cancer. International Agency for Research on Cancer Scientific Publication No. 161. Geneva: World Health Organization; 2013. [Google Scholar]
- 13.Chang SH, Delgermaa V, Mungun-Ulzii K, Erdenekhuu N, Odkhuu E, Huang SL. Support for smoke-free policy among restaurant owners and managers in Ulaanbaatar, Mongolia. Tob Control. 2009;18:479–484. doi: 10.1136/tc.2009.030486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Murray CJ, Ezzati M, Flaxman AD, Lim S, Lozano R, Michaud C, et al. GBD 2010: design, definitions and metrics. Lancet. 2012;380:2063–2066. doi: 10.1016/S0140-6736(12)61899-6. [DOI] [PubMed] [Google Scholar]
- 15.Gordon JK, Emmel ND, Manaseki S, Chambers J. Perceptions of the health effects of stoves in Mongolia. J Health Organ Manag. 2007;21:580–587. doi: 10.1108/14777260710834364. [DOI] [PubMed] [Google Scholar]
- 16.Wigfall C, Mandukhai G, Jargalsaikhan B, Warburton D, Crano WD. Implementing attitudes measurement to influence winter air pollution mask wearing by pregnant women in Ulaanbaatar: a pilot study. Cent Asian J Med Sci. 2017;3:269–281. [Google Scholar]
- 17.Hoffmann S, Qin P, Krupnik A, Badrach B, Batbaatar S, Altangerel E, et al. The willingness to pay for mortality reductions in Mongolia. Resour Energy Econ. 2012;34:493–513. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.